In this issue of Blood, Pulsipher et al identify key differences in adverse events related to donation for hematopoietic cell transplantation (HCT) from a prospective cohort of nearly 9500 unrelated allogeneic donors recruited through the National Marrow Donor Program.1 Although the rates of life-threatening complications were very low overall (<0.3%) for donors of both peripheral blood and bone marrow, those donating bone marrow had a 4-fold increased risk of experiencing a serious adverse event. Most adverse events were acute in nature, resolving within a matter of days to weeks, and importantly, no deaths as a result of donation procedures occurred. This prospective study, with more than 20 000 donor-years of follow-up after granulocyte colony-stimulating factor administration, also showed no increased risk for hematologic or other cancers, autoimmune diseases, or thrombosis associated with growth factor mobilization. In fact, donors in this cohort had a significantly lower incidence of cancer compared with the general population, regardless of granulocyte colony-stimulating factor exposure.
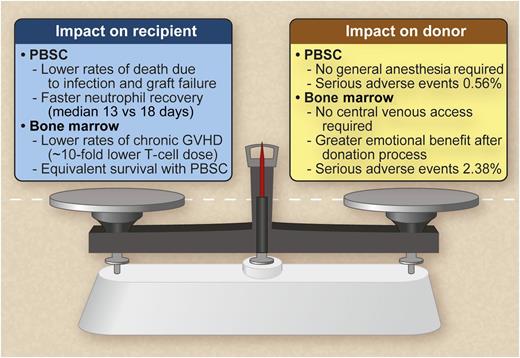
Weighing the benefits of PBSC vs marrow donation. Professional illustration by Debra T. Dartez.
Weighing the benefits of PBSC vs marrow donation. Professional illustration by Debra T. Dartez.
Will these results affect the rates of peripheral blood stem cell (PBSC) vs marrow harvest for our current and future donors? Several potential risks and benefits are inherent with each allograft source (see figure). PBSC grafts may be viewed as more convenient and not requiring general anesthesia or recovery from an invasive surgical procedure, yet they may require several days of filgrastim and 1 to 3 days of apheresis. However, central venous access is not needed during marrow harvesting, sparing the rare but serious complications of central venous access, including pneumothorax, thrombosis, and infections. Donor safety and the preferred product for the intended recipient must both be considered in any debate of an optimal stem cell source.2 The report by Pulsipher et al demonstrates that donor safety has improved over time, and it is indeed reasonable to consider both stem cell donation methods very safe. Interestingly, a recent study of donor quality of life revealed a greater sense of meaning and emotional benefit from bone marrow over peripheral blood stem cell donation.3
Another issue is the optimal source of hematopoietic cells for the recipient. This subject has been a matter of ongoing debate since the development and refinement of apheresis procedures for the harvesting of PBSC in the 1980s and 1990s.4 Differences in hematopoietic and immune reconstitution, rates of acute and chronic graft-versus-host disease (GVHD), relapse risk, and cost have led to a marked increase in the use of PBSC over marrow.5,6 Rates of PBSC donation (approximately 75% of collections) dominated over marrow donation (approximately 15% of collections) for adult recipients of HCT from 2002 to 2011, with cord blood HCT making up the remainder.7 The preferred graft source for the recently growing experience in haploidentical grafting is even less certain. Thus, it remains unclear whether recipient outcomes manifest mostly as greater risks for chronic GVHD with PBSC grafts8 vs the ease of collection, or whether these small but recognized differences in donor safety will alter this trend, at least for unrelated donor transplantation. Bone marrow is generally preferred for most nonmalignant diseases and for children in whom any extra risks for chronic GVHD are unwarranted. The growing experience with cord blood transplants as an acceptable hematopoietic stem cell source raises new options that pose no risk to the donor, in contrast to the risks inherent in a marrow harvest or apheresis. However, a suitable graft, collectable in many ways, may not be the ideal graft for any cohort of recipients. The cellular composition varies substantially with different hematopoietic stem cell sources, and as such, the optimal cellular content of T cells, myeloid cells, and other subsets that result in the best outcomes, reproducible across the different graft sources, remains to be defined.9
Because it is unlikely that unrelated donor HCT is going to become outmoded in the near future, how can we best serve our unrelated donors, who make possible thousands of potentially life-saving HCT procedures each year? Continued studies on donor safety10 and quality of life3 should remain a priority, but novel methods of hematopoietic allograft engineering and improved pharmacologic approaches to stem cell mobilization, such as the upcoming Center for International Blood and Marrow Transplant Research–sponsored study of plerixafor for related donor HCT, should also be a priority. Such new techniques could one day obviate the need for surgical procedures or prolonged cytokine administration, thus avoiding the present dilemma of marrow vs PBSC donation for future donors.
Conflict-of-interest disclosure: The authors declare no competing financial interests.