Abstract
A subset of patients with the Philadelphia-chromosome negative myeloproliferative neoplasms (MPNs) transform to AML, and the prognosis of post-MPN AML patients is very poor. As such, new genomic insights are needed to define the mechanisms that govern transformation from MPN to AML, and to identify new therapeutic targets for clinical intervention in this poor-risk myeloid neoplasm. Importantly, patients with JAK2V617F mutant chronic-phase disease transform to JAK2 wildtype AMLs in approximately half of cases, indicating that diverse genomic paths lead to transformation.
To characterize the genomic alterations, including point mutations, short indels, translocations, and copy number alterations, in 33 post-MPN AML samples.
Genomic DNA and total RNA was isolated from formalin fixed paraffin embedded (FFPE) tissue, blood and bone marrow aspirates. Adaptor ligated sequencing libraries were captured by solution hybridization using two custom baitsets targeting 374 cancer-related genes and 24 genes frequently rearranged for DNA-seq, and 272 genes frequently rearranged for RNA-seq. All captured libraries were sequenced to high depth (Illumina HiSeq), averaging >590X for DNA and >20,000,000 total pairs for RNA, to enable the sensitive and specific detection of genomic alterations. We achieved a mean coverage depth of 511x (range 405-645).
The most common genomic alterations identified in post-MPN AML samples were mutations in JAK2 (51.5%), ASXL1 (48.5%), and IDH2 (30.3%). Mutually exclusive mutations in the genes of spliceosome components SRSF2, U2AF1, and SF3B1 were identified in 39% of patients in this cohort, suggesting that somatic mutations in splicing factors are a common genomic event in transformation from MPN to AML. These data were in contrast to de-novo AML, in which mutations in FLT3, NPM1, and DNMT3A are the most common disease alleles (NEJM 2013; 368: 2059), suggesting that the spectrum of genomic alteration in post-MPN AML differs from that in de novo AML.
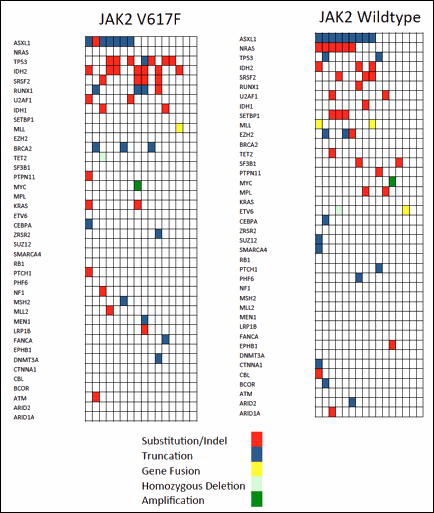
Within our cohort of post–MPN AML samples, 52% of the patients had JAK2V617F positive AML and 48% of our cohort presented with JAK2 wildtype AML. Notably, the two subsets of post-MPN AML had distinct mutational patterns. In the JAK2V617F mutant subgroup, we identified frequent mutations in ASXL1 (41.2%), TP53 (41.2%), and IDH2 (41.2%). In JAK2-wildtype AML subgroup we identified frequent ASXL1 mutations (56.3%) and NRAS point mutations (37.5%). NRAS mutations were exclusive of JAK2 mutations in the entire cohort, consistent with alternate disease alleles which activate signaling in JAK2V617F positive AML and in JAK2 wildtype AML. SETBP1 mutations were found in 19% of patients with JAK2 wildtype post-MPN AML but not in any patients with JAK2V617F-positive post-MPN AML.
Several alterations not previously described in post-MPN AML, to the best of our knowledge, were identified in this cohort including MLL-PTD, which was observed in both JAK2V617F and wildtype JAK2 patients. Copy number analysis of our high-depth sequencing data allowed us to identify homozygous deletions of TET2 and ETV6 and MYC amplifications in post-MPN AML. Univariate analysis demonstrated TP53 mutations were associated with significantly impaired overall survival (p<0.001). IDH2 mutations were associated with higher peripheral blood blast count (p=0.017).
The spectrum of genomic alterations in post-MPN AML is strikingly distinct from de novo AML. Furthermore, capture-based sequencing allowed us to show there are important differences in the mutational profile of JAK2V617F and JAK2 wildtype post-MPN AML. NRAS mutations may represent driver mutations in JAK2V617F negative post-MPN AML and further biologic evaluation of these mutations is needed. Most importantly, the identification of NRAS, IDH2, and MLL-PTD mutations in post-MPN AML suggest specific therapies including MAPK inhibition, IDH2 inhibition and dot1L/BRD4 inhibition may be of value in genotypically defined subsets of post-MPN AML. These finding help to further define the biology of leukemic transformation, as well as offer new therapeutic avenues for the treatment of post-MPN AML.
Spectrum of genomic alterations found in JAK2V617F and JAK2 wildtype post-MPN AML.
Spectrum of genomic alterations found in JAK2V617F and JAK2 wildtype post-MPN AML.
Rampal:Foundation Medicine: Consultancy. Verstovsek:Incyte Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal