Introduction
Aberrant lymphoma epigenome is the result of a combinatorial contribution of changes in DNA methylation, histone modifications, and noncoding RNA (ncRNA) expression in lymphoma cells. All of the components of epigenome have been the focus of intense studies in various subtypes of lymphoma, which resulted in the deeper understanding of novel mechanisms of lymphomagenesis and revealed novel therapeutic targets. Some of the changes are common to all lymphomas and even other types of cancers, whereas others are subtype specific. In this review, we attempt to summarize the current state of knowledge in the field of lymphoma epigenomics with particular emphasis on subtype-specific changes, differences between adult and pediatric lymphomas, and novel epigenetic therapies.
DNA methylation
DNA methylation patterning and the role of DNA methyltransferases in normal B-cell development and lymphomagenesis
DNA methylation is part of epigenetic programming that is required for normal B-cell development and is disrupted during lymphomagenesis.1 To understand how aberrant methylation contributes to lymphomagenesis, it is important to understand the patterns of methylation in normal B cells. Deaton et al2 showed that not only differentially methylated regions (DMRs) around transcriptional start sites are of significance, but also methylation patterns in the intergenic areas have cell and tissue specificity. The dynamic nature of methylome during hematopoietic development was studied by Ji et al in mouse multipotent progenitors using comprehensive high-throughput array-based relative methylation analysis, which examined 4.6 million CpGs in the genome.3 This study demonstrated DMRs and revealed that lymphoid lineage commitment requires more DNA methylation than myeloid lineage. Challen et al demonstrated that DNMT3a expression is higher in primitive long-term hematopoietic stem cells than in progenitors and differentiated cells.4 Importantly, the same group demonstrated that loss of DNMT3a in mice resulted in significant expansion of HSCs because of their reduced differentiation ability and was associated with broad changes in the distribution of methylated CpGs. Shaknovich et al addressed changes in epigenome during germinal center (GC) transit and revealed that transition from naïve B cells (NB) to centroblasts (CB) is associated with predominant loss of methylation in 235 differentially methylated genes that affect NF-κB and mitogen-activated protein kinase pathways.5 These studies set the stage for interpretation of epigenetic changes in pre-GC and GC-derived lymphomas.
The key factors responsible for DNA methylation are members of the DNA methyltransferase (DNMT) family: DNMT1, DNMT3a, and DNMT3b, which have complex patterns of expression in peripheral B cells and during GC transit.5,6 DNMT expression is highly compartmentalized within the GC, with DNMT1 and DNMT3b being the most highly expressed within GC B cells, but not in NB cells. GC formation is dependent on the amount of DNMT1 with significant diminution of GCs in Dnmt1 hypomorphic mice.5 The important role of DNMTs in lymphomagenesis is underscored by the evidence from Amara et al7 that DNMT1, DNMT3a, and DNMT3b are overexpressed in 48%, 13%, and 45% of 81 de novo diffuse large B-cell lymphomas (DLBCLs) and correlate with advanced clinical stages. Importantly, concomitant expression of DNMT1 and DNMT3b correlated with resistance to treatment, whereas DNMT3b overexpression correlated with shorter overall and progression-free survival. Somatic mutations in DNMTs may contribute to chromosomal instability, as supported by the observation of increased mutation rates in patients with germline mutations in DNMT3b.8 Mutational analysis of DNMT3a by Kim et al in 401 hematologic malignancies identified that mutations do occur infrequently in pre–B-acute lymphocytic leukemia (ALL), but allelic loss is more frequent (48.1%) in lymphomas.9 Van Vlierberghe et al identified DNMT3a mutations in 2 of 57 patients with adult immature T-ALL.10 It appears that DNMT mutations in precursor B and T neoplasms, albeit infrequent, result in aberrant pathogenic function, whereas the overall DNMT expression levels play a role in more mature lymphoid malignancies. These findings suggest that the development of specific DNMT inhibitors is warranted for the treatment of lymphomas.
Aberrant DNA methylation patterning in B-cell lymphomas
DNA methylation in DLBCLs.
DLBCL is the most common aggressive lymphoma in adults, and many studies so far focused on the changes in DLBCL epigenome elucidating the patterns of aberrant methylation.
Two key changes in DNA methylation seem to be at play in DLBCLs and possibly in follicular lymphoma (FL): (a) site-directed changes affecting specific oncogenes or tumor suppressor genes and (b) increasing epigenomic instability and heterogeneity. Hypermethylation of gene regulatory regions can lead to transcriptional silencing, in part because of recruitment of methylation-dependent repressor proteins, whereas hypomethylation can lead to increased gene expression, and genomic instability when affecting large regions of the genome.1 P16 (INK4A) is an example of a known tumor suppressor gene hypermethylated in lymphomas. Even though P16 methylation in lymphomas has been thought to impart a worse prognosis, Zainuddin et al studied 113 cases of primary DLBCL using pyrosequencing and showed no association with worse outcome.11 KLF4 is another example of a tumor suppressor gene reported to be aberrantly hypermethylated in many subtypes of lymphoma, including FL, DLBCL, Burkitt’s lymphoma (BL) and classical Hodgkin lymphoma (HL) by Guan et al, suggesting common subtype-independent mechanisms of lymphomagenesis.12
Recent reports suggest that regulation of gene expression by DNA methylation patterning is complex and is not a simple “on” or “off” switch for gene expression. For example, hypermethylation of a CpG-rich region within the first intron of BCL6 was reported to induce higher levels of BCL6 expression, at least in part by blocking binding of CCCTC-binding factor.13 Accordingly, BCL6 levels were decreased in lymphoma cell lines exposed to the DNMT inhibitor decitabine.13 These findings illustrate the need for more comprehensive studies characterizing the mechanisms of epigenetic regulation.
Additional insight into the pathobiology of lymphomas came from the study of 83 mature aggressive B-cell non-HL by Martin-Subero et al that revealed 56 genes de novo methylated in all lymphoma subtypes and 22 genes with a subtype-specific pattern of methylation.14 Remarkably, de novo methylated genes were enriched for Polycomb (PcG) targets in embryonic stem cells, highlighting the complex epigenetic mechanisms of lymphomagenesis. Velichutina et al demonstrated that in normal GC B cells, DNA methylation and H3K27me3 mark created by the PcG family protein EZH2 were mutually exclusive, whereas this epigenetic segregation was disrupted in DLBCLs.15 These aberrant epigenetic events may be caused by mutations in the SET domain of EZH2 that have been detected in as much as 12% of FLs and 9.7% of DLBCLs.16,17 The effect of SET domain mutations on the physical interaction between EZH2 and DNMTs is not known but might contribute to aberrant overlap of gene silencing marks, as stated before.18 EZH2 inhibitors promise to be effective therapeutic options for patients with mutated EZH2. Knutson et al reported the discovery of EPZ005687, a potent inhibitor of EZH2 with Tyr641 or Ala677 mutations.19,20 Treatment of DLBCL cell lines with mutant EZH2 with this novel inhibitor induced apoptosis and eventually cell death.
In addition to individual genes that are aberrantly methylated in lymphomas, a new concept of epigenetic instability has emerged as contributing to the pathogenesis of some lymphoma subtypes. De et al clearly demonstrated that increased variance in DNA methylation, as compared with normal B cells, correlated with worse overall and progression-free survival in DLBCLs and in FLs.21,22 The intrasample and intersample heterogeneity reflect possible clonal heterogeneity within lymphoma and heterogeneity between individuals respectively. Normal B cells appear to have bimodal distribution of methylation, whereas lymphomas have much greater variance of methylation at each individual CpG, and this variance is increasing from low grade to high grade FLs and further to GCB-like DLBCLs and ABC-like DLBCLs, resulting in unimodal distribution. The source of such growing epigenetic instability is not entirely clear but has been linked to the events in the GC. Shaknovich et al demonstrated that GC B cells have higher epigenetic heterogeneity than NB cells and that this phenomenon may be dependent on activation-induced cytidine deaminase (AID).5 It appears that AID may contribute to epigenetic instability in lymphomas through its role as a demethylase, similar to its contribution to genomic instability through its role in somatic hypermutation (SHM).23-27 Another potential contributor to epigenetic instability is CCCTC-binding factor—an insulator protein that may prevent the spread of aberrant methylation in lymphomas.28
DNA methylation in FL.
The first truly genome-wide methylome analysis in FL was performed by Choi et al, interrogating 726 003 CpGs in FL cell line RL and 1.3 million CpGs in CD19+ B cells using 454 sequencing technology.29 Comparison of the methylation maps between CD19+ B cells and FL cell line revealed the overall differences in the distribution of CpG methylation: in normal B cells, methylation was predominantly associated with inter- and intragenic regions enriched for repetitive sequences, whereas in FL there was increased methylation in promoter regions and decreased methylation of intra- and intergenic regions. This finding supports the idea of increased chromosomal fragility in lymphomas as a result of hypomethylation and aberrant methylation of tumor suppressor genes. Significant differences were observed in methylation in HOX genes as well as SOX and FRIZZLED gene families. Earlier studies by O’Riain et al and Benett et al30 discovered that, similarly to DLBCLs, there is hypermethylation of PRC2 targets in FL.31 Hypermethylation of EZH2 targets along with EZH2 mutations in 7.2% of FLs16 opens the possibility for effective epigenetic treatments with EZH2 inhibitors in combination with demethylating agents.
DNA methylation of MCL.
Methylation profiling of mantle cell lymphoma (MCL) by Enjuanes et al revealed 252 hypermethylated genes. Five genes (SOX9, HOXA9, AHR, NR2F2, and ROBO1) correlated with higher proliferation, increased number of chromosomal abnormalities, and shorter survival of the patients.32 Methylation of HOX genes was also reported in MCL.33 Leschenko et al performed DNA methylation profiling using the HELP assay and NimblegenRoche methylation arrays and revealed differences in methylation between 22 primary MCLs and 10 purified fractions of IgD+ B-cell controls, which are the putative normal precursors to MCL.34 The study revealed several aberrantly methylated genes, of which CD37 was confirmed to be aberrantly overexpressed in MCL and served as a novel therapeutic target for small modular immunotherapeutic (CD37-SMIP), resulting in significant loss of viability in cell lines and in synergism with epigenetic therapy with decitabine.
DNA methylation in CLL.
Chronic lymphocytic leukemia (CLL) displays concomitant genome-wide loss of methylation and site-specific gain of methylation. Hypomethylation of the genome has been demonstrated using a variety of techniques from high-performance liquid chromatography35 to whole-genome bisulphate sequencing.36 Kulis et al identified DMRs between unmutated CLL and mutated CLL and their putative normal B-cell precursors NB cells and memory B cells and confirmed that although majority of CpGs were hypomethylated and centered in gene bodies, hypermethylated CpGs were enriched in 5′ regulatory regions, CpG islands, and 5′ regions of introns.36 Aberrantly hypermethylated genes in CLL that serve as biomarkers and shed light into disease biology include CDKN2A and CDKN2B, ZAP70, DAPK1, and ID4 among others.37-40 Another significant epigenetic event in CLL is silencing of Wnt pathway inhibitors such as CDH1, DKK1, DKK2, DKK3, SFRP1, SFRP2, SFRP3, SFRP4, SFRP5, and WIF1 genes, which leads to activation of the pathway and overexpression of WNT family members and its receptor Frizzled (Fzd).41,42
Recent study by Kulis et al36 revealed that 3 epigenetic subtypes of CLL have different clinical course and time to first treatment, underscoring the importance of epigenome in the pathogenesis of the disease and promising novel disease biomarkers and therapeutic targets.
DNA methylation in pediatric lymphoid neoplasms.
The most common pediatric malignancy is pre–B-cell ALL, and, consequently, most of the relevant studies in pediatric lymphomas/leukemias come from this diagnostic category. The biology of childhood ALL is different from adult ALL with different characteristic leukemogenic events.43 There are limited data suggesting that epigenetic lesions may be similar in the 2 categories.43 Garcia-Manero et al studied promoter-associated CpG islands in MDR1 (multidrug resistance gene 1), P15, C-ABL, CD10, P16, and P73 in 16 pediatric patients and concluded that there was no difference in the methylation levels of those genes between pediatric and adult patients.44 Wong et al identified a common methylation signature for all genetic subtypes of pediatric ALL that could differentiate disease-free bone marrow specimens from malignant specimens.43 Davidsson et al profiled the 2 most common genetic subgroups of B-ALL: hyperdiploid and t(12;21)(p13;q22) or EVT6/RUNX1 fusion–associated cases and detected subtype-specific methylation differences.45 Methylation hotspots were associated with chromosomal bands containing imprinted genes. Hyperdiploid ALL had more hypermethylated genes (7650 vs 3983), and the top candidates were enriched for genes from cell signaling, transcription regulation, and apoptosis gene ontology (GO) categories. There is already emerging molecular evidence that epigenetic treatments can be effective in pediatric leukemia: histone deacetylase (HDAC) inhibitors may reverse aberrant hypomethylation of MYC, SET, RUNX1, and RAN, as well as the MLL-AF4 fusion product in t(4;11)-positive primary infant ALL cells, leading to cell death.45
Histone modifications
Histone code in normal lymphoid development
A major part of the epigenetic regulation is conveyed through “the histone code,” which serves as a platform for the assembly of the appropriate transcription regulatory machinery.46,47 Cells use a large army of histone-modifying enzymes—“writers,” “erasers,” and chromatin “remodelers”—to edit the histone code,48,49 and then they use another set of enzymes (“readers”), which contain specific domains that recognize different modifications, to interpret this code and initiate additional chromatin modification and/or relevant biological processes.49,50 This tightly-woven network plays an essential role in lymphoid development, and genetic abnormalities involving readers, writers, erasers, and remodelers have been implicated in many lymphoid malignancies. For example, PAX5, a transcription factor (TF) that is required for B-cell identity commitment and maintenance,51 was shown to activate its target genes by binding to promoters and putative enhancers that were enriched in active histone marks, such as H3K9ac, H3K4me2, and H3K4me352,53 in mice pro–B cells. However, Pax5−/− pro–B cells lost those epigenetic marks at these promoters and enhancers. Recently, it was demonstrated that PAX5 can recruit histone modifiers, such as the histone acetyltransferase (HAT) CREBBP, the subunit RbBP5 of the MLL-containing methyltransferase complex and the chromatin-remodeling BAF complex to its activated genes, and the HDAC3-containing NCOR corepressor complex to its repressed genes in pro–B cells.53 The recruitment of these enzymes by PAX5 may establish the epigenetic signature required for B-cell commitment. Interestingly, somatic mutations in these enzymes, including CREBBP and ARID1A (encodes BAF250a), have been discovered in different subtypes of lymphomas, suggesting that deregulation of this epigenetic circuit is crucial for lymphomagenesis.54-59
Mutations in histone-modifying enzymes
Owing to the advances in next-generation sequencing technology, including RNA-seq, exome-seq, and whole-genome-seq, recent years brought about the discovery of many novel mutations in cancers. Next we summarize recent findings of novel mutations within histone modifying enzymes in lymphoid malignancies and discuss the potential implications of these mutations for lymphomagenesis (Table 1).13
Chromatin modifying enzymes deregulated in lymphoid neoplasms
| Genes . | Activity . | Genetic Deregulation . | Disease . | Implications . |
|---|---|---|---|---|
| EZH2 | H3K27 methyltransferase (PRC2 complex) | Mutation | FL | Increasing H3K27me3 level (FL, DLBCL, PMBL); Loss-of-function (T-ALL) |
| GCB-DLBCL | ||||
| PMBL | ||||
| T-ALL | ||||
| MLL2 | H3K4 methyltransferase | Mutation | FL | May result in reduced H3K4me3 level |
| Frame-shift | DLBCL | |||
| KDM2B | H3K36 methyltransferase | Mutation | DLBCL | Not known |
| UTX | H3K27 demethylase | Mutation | MM | Slowing of proliferation |
| MMSET | Histone methyltransferase | Activating translocation | MM | Affecting H3K27me3 and H3K36me2/3 levels |
| JMJD2C | H3K9 demethylase | Amplification | PMBL | Not known |
| HL | ||||
| MLL1 | H3K4 methyltransferase | Translocation | ALL | Not known |
| EED | PRC2 complex | Mutation | T-ALL | Loss-of-function, may result in reduced H3K27me3 |
| SUZ12 | PRC2 complex | Mutation | T-ALL | Loss-of-function, may result in reduced H3K27me3 |
| CREBBP | Histone acetyltransferase | Mutation | FL | Disrupting acetyltransferase and transcription co-activation activities |
| Deletion | DLBCL | |||
| ALL | ||||
| EP300 | Histone acetyltransferase | Mutation | FL | Disrupting acetyltransferase and transcription coactivation activities |
| Deletion | DLBCL | |||
| ARID1A | Chromatin remodeling SWI/SNF complex | Mutation | Pediatric-BL | May give malignant B-cell growth advantages |
| CLL | ||||
| CHD2 | Chromatin remodeling CHD family member | Mutation | CLL | Deregulation of histone variant H3.3 deposition |
| Genes . | Activity . | Genetic Deregulation . | Disease . | Implications . |
|---|---|---|---|---|
| EZH2 | H3K27 methyltransferase (PRC2 complex) | Mutation | FL | Increasing H3K27me3 level (FL, DLBCL, PMBL); Loss-of-function (T-ALL) |
| GCB-DLBCL | ||||
| PMBL | ||||
| T-ALL | ||||
| MLL2 | H3K4 methyltransferase | Mutation | FL | May result in reduced H3K4me3 level |
| Frame-shift | DLBCL | |||
| KDM2B | H3K36 methyltransferase | Mutation | DLBCL | Not known |
| UTX | H3K27 demethylase | Mutation | MM | Slowing of proliferation |
| MMSET | Histone methyltransferase | Activating translocation | MM | Affecting H3K27me3 and H3K36me2/3 levels |
| JMJD2C | H3K9 demethylase | Amplification | PMBL | Not known |
| HL | ||||
| MLL1 | H3K4 methyltransferase | Translocation | ALL | Not known |
| EED | PRC2 complex | Mutation | T-ALL | Loss-of-function, may result in reduced H3K27me3 |
| SUZ12 | PRC2 complex | Mutation | T-ALL | Loss-of-function, may result in reduced H3K27me3 |
| CREBBP | Histone acetyltransferase | Mutation | FL | Disrupting acetyltransferase and transcription co-activation activities |
| Deletion | DLBCL | |||
| ALL | ||||
| EP300 | Histone acetyltransferase | Mutation | FL | Disrupting acetyltransferase and transcription coactivation activities |
| Deletion | DLBCL | |||
| ARID1A | Chromatin remodeling SWI/SNF complex | Mutation | Pediatric-BL | May give malignant B-cell growth advantages |
| CLL | ||||
| CHD2 | Chromatin remodeling CHD family member | Mutation | CLL | Deregulation of histone variant H3.3 deposition |
Mutations affecting histone methylation marks.
Much focus has been given to H3K4 methylation and H3K27 methylation as they pose opposite effects (H3K4 and H3K27 methylation are associated with transcriptional activation and repression, respectively), yet they coexist at the promoters of genes controlling lineage differentiation in embryonic stem cells (bivalent genes).60,61 H3K36 and H3K79 methylation at gene bodies also reflects active transcription.61 In lymphomas, genetic abnormalities observed in enzymes that “write” or “erase” methylation of these lysines could potentially destroy the balance between the active and repressive histone marks.
For example, several studies discovered mutations that could affect the H3K4 and H3K27 methylation balance in FL and DLBCL.16,17,54,55,62 Morin et al first identified a heterozygous point mutation within EZH2, a PRC2 complex component that methylates H3K27.54 This mutation occurs within the SET domain, which has methyltransferase activity.17,55,62 Interestingly, in the very same cohorts, these investigators also discovered missense, nonsense, and frame-shift mutations within MLL2 gene that encodes a histone H3K4 methyltransferase.16,55,62 The frequencies of MLL2 mutations were 23% to 32%55,63 in the 3 cohorts of DLBCLs16 and was 89% in FLs.16 EZH2 plays an important role in B-cell development. It is required for VDJ recombination in pro–B cells.63 In GC B cells, which may give rise to GCB-DLBCLs and FLs, EZH2 epigenetically silences expression of genes involved in cell growth and proliferation, such as CDKN1A, CDKN1B, and CDKN2A.15 Although wide-type EZH2 preferentially methylates unmethylated H3K27 to produce H3K27me1, biochemical experiments revealed that PRC2 complexes containing mutant forms of EZH2 preferentially methylates H3K27me1 and H3K27me2, resulting in elevated H3K27me2 and H3K27me3 levels.64-66 Given this shift of enzymatic activity, one can imagine that there might be an increased level of the repressive H3K27me3 mark in lymphoma cells that harbor this gain-of-function mutation. On the other hand, the MLL2 mutations discovered in FL and DLBCL are all predicted to disrupt the methyltransferase SET domain of the MLL2 protein and cause reduced levels of H3K4me3. Therefore, it appears that both EZH2 and MLL2 mutations would establish an aberrant histone methylation code to further repress gene expression in FL and DLBCL. However, the existence of this aberrant histone methylation code and its consequence to FL and DLBCL development are still not clear. Modeling these mutations in B cells is crucial to address these questions. In addition to EZH2 and MLL2, Pasqualucci et al also discovered KDM2B (H3K36 demethylase) mutations in 7.4% of the DLBCLs, suggesting there might be an altered H3K36me3 pattern in these lymphomas.62
The key epigenetic changes in multiple myeloma (MM) involve H3K36me3 and H3K27me3. Van Haaften et al identified inactivating mutations in UTX, a histone H3K27 demethylase, in 10% of MM cases.67 Interestingly, UTX mutation is mutually exclusive with MMSET-activating translocation t(4;14),67 another hallmark of MM. MMSET is a SET domain–containing histone methyltransferase. About 15% to 20% of MM patients carry t(4;14) translocation that places MMSET and FGFR3 genes under the control of IGH enhancers.68 However, only MMSET overexpression is thought to be important for MM pathogenesis.69,70 Martinez-Garcia et al showed that overexpression of MMSET correlated with an increase in H3K36me3 and a decrease in H3K27me3.71 On the contrary, Kuo et al only observed reduction of H3K36me2 after MMSET knock down in a MM cell line (KMS11), suggesting MMSET is primarily an H3K36me2 methyltransferase.72 Furthermore, they demonstrated that overexpression of MMSET could disrupt the physiological genomic distribution of H3K36me2.72 Although the enzymatic function of MMSET needs to be further clarified, it is obvious that deregulation of MMSET affects H3K36 methylation. Therefore, the disrupted balance between H3K27me3 and H3K36me2/3 may play an important role in the molecular pathogenesis of MM. To further complicate the situation, UTX is also shown to be associated with MLL2/3 complexes,73 raising the possibility that UTX mutations may also tip the balance between H3K27me3 and H3K4me3. In addition, mutations in MLL family members have also been identified in several MM patients.74 However, no correlation between the change in global H3K27me3 and H3K4me3 levels was observed in Utx null cells compared with wide-type cells.67
In addition to FL, DLBCL, and MM, genetic alterations of factors affecting histone methylation have been found in other lymphoid malignancies. For example, H3K9 demethylase JMJD2C was amplified along with JAK2 in primary mediastinal B-cell lymphoma (PMBL) and HL.75 It is proposed that JAK2 and JMJD2 cooperatively remodel the PMBL and HL epigenome to deregulate oncogenes such as MYC.75 MLL1 translocations are seen in 8% to 10% of ALL, and more rarely in T-ALL, all of which result in a loss of its histone methyltransferase SET domain.76 More interestingly, 2 groups have recently discovered loss-of-function mutations of PRC2 complex genes EZH2, EED, and SUZ12 in T-ALL. Zhang et al reported that 42% of the ETP ALL (early T-cell precursor ALL) cases and 12% of non-ETP T-ALL cases harbored a deletion and/or mutation in these genes.77 Similarily, Ntziachristos et al reported 25% of T-ALL had loss-of-function mutations and deletions of the EZH2 and SUZ12 genes.78 By using a NOTCH1-dependent mouse model of T-ALL, they further suggested a dynamic interplay between oncogenic NOTCH1 and tumor-suppressing PRC2 function for gene expression regulation and malignant transformation.78 It is intriguing that genetic profiling revealed 2 opposite roles of EZH2 in lymphoid malignancies. It is hoped that further mechanistic studies of the PRC2 complex in normal and malignant B cells will shed some light on this paradox.
Mutations affecting histone acetylation marks.
Histone acetylation is often associated with a more “open” chromatin conformation that facilitates transcription, translation, and DNA repair. It is distributed at actively transcribed promoters and their nearby enhancers.79,80 In particular, acetylation of H3K27 (opposing mark to H3K27me3 on the same lysine that is trimethylated by PRC2 complex) is dynamically regulated at enhancers of genes involved in development and differentiation and can predict developmental state.81 Histone acetylation is written by HATs and erased by HDACs. In addition, it can be read by proteins containing bromodomains and/or PHD fingers.
Recurrent mutations in HATs, such as CREBBP and/or EP300, have been identified in 16% to 39% of DLBCLs and 41% to 62% of FLs.54-56,82 In addition, focal deletion and mutations involving CREBBP were found in 18% of relapsed ALL.57 Mutations in CREBBP and EP300 are often heterozygous and may disrupt their acetyltransferase activity, affecting the cellular acetylome and promoting the oncogenic phenotype. Indeed, mutations affecting the HAT activity of CREBBP and EP300 promote the activation of BCL6 and HSP90 while destabilizing P53.56,82 Therefore, loss of BCL6 acetylation in CREBBPHAT or EP300HAT mutant cells may exacerbate the oncogenic activity of BCL6 and HSP90 in these lymphomas. Although the balance between HAT and HDACs can be pharmacologically manipulated by using HDAC inhibitors (HDACi), DLBCL with CREBBPHAT and/or EP300HAT mutations tend to be resistant to this strategy.82 The combination of HDACi with molecules that inactivate EP300 substrate proteins such as HSP90 and BCL6 may offer a way to circumvent this problem.82 Interestingly, BCL6 itself can repress EP300 in DLBCLs, and treatment with RI-BPI, a BCL6 peptide inhibitor, can induce EP300 expression, which is required for killing of DLBCL cells by RI-BPI,82 providing an alternative way to restore the HAT/HDAC balance in lymphomas with wild-type enzymes. Currently, it is important to establish a mechanistic link between CREBBP/EP300 mutations, aberrant histone acetylation, impaired target regulation, and lymphomagenesis to design a targeted therapy specific for lymphomas with CREBBP/EP300 mutations.
Mutations affecting chromatin remodeling.
In addition to histone modifications, remodeling of chromatin can also epigenetically regulate transcription, replication, and DNA repair. Chromatin remodelers use the energy from ATP hydrolysis to change the location of nucleosomes, or to deposit histone variants, resulting in change of chromatin conformation and composition.83 Based on the difference of the core adenosine triphosphatase subunits, chromatin remodelers can be divided into the SWI/SNF (SWItch/Sucrose NonFermentable), ISWI (Imitation of SWItch), CHD (Chromodomain Helicase DNA-binding), and INO (INOsitol) families.
Mutations in ARID1A, which encodes BAF250a, a subunit of the SWI/SNF chromatin remodeling complex, has been found in 17% of pediatric BL58 and 2 of 105 CLL patients.59 ARID1A was shown to have tumor suppressor functions in gastric adenocarcinoma by slowing down cell proliferation through repressing expression of EF1 and CCND1.84 Other ARID1A targets include cell cycle regulator CDKN1A85 and ES cell self-renewal factors SOX2 and OCT4.86 Although the role of ARID1A mutations in lymphomagenesis has not been explored, it is possible that mutant ARID1A may give malignant B cells growth advantages.
CHD2 mutations were also identified in 4.8% of CLL cases.59 CHD2 belongs to the CHD family of chromatin remodelers. Chd2-deficient mice showed defects in erythrocyte differentiation and developed lymphomas, probably because of the deregulation of activated T cells.87 Recently, Harada et al demonstrated that CHD2 can deposit histone variant H3.3 at genes important for differentiation.88 Histone H3.3 has been shown to localize at promoters of actively transcribed genes as well as some silent genes presumably poised to be expressed. In addition, H3.3 has been proposed to take part in the epigenetic transmission of active chromatin states.89 Therefore, it will be interesting to see whether CHD2 mutants could induce an aberrant gene transcription programming by deregulating H3.3 deposition in malignant B cells.
Although the discovery of mutations within histone-modifying enzymes led us one step closer to the understanding of molecular pathogenesis of lymphoid malignancies, the lack of the knowledge about how these mutations lead to disease development still hinders us from developing effective targeted therapies. To date, it is still unclear whether these mutations are “driver” mutations that initiate malignant transformation, “facilitator” mutations that promote disease progression, or just merely “passenger” mutations that have no effect on disease pathogenesis. Recently, Green et al established a hierarchy model of FL somatic evolution by comparing and contrasting the exome mutational profiles of FL in subpopulations at diagnosis and relapse, based on CD20 expression levels.90 Their model suggested that CREBBP mutations were early “drivers” of FL disease evolution, and because these mutations were found in the CD20 subpopulations of FLs at both diagnosis and relapse, MLL2 mutations were likely later “accelerators” because MLL2 mutations were only found in one of the subpopulations. Although the observation was interesting, the case number was limited. Moreover, the mechanistic explanations of the CREBBP driving effects and MLL2 accelerating effects on lymphomagenesis are still missing. We will not be able to offer rationalized and targeted therapies until we fill in these blanks.
MicroRNAs and ncRNAs in lymphoid malignancies
Shortly after the discovery of human microRNAs (miRNAs) in 2000,91 the first studies emerged linking miRNA genes and disease. The finding that miR-15 and miR-16-1 were frequently deleted or repressed in CLL92 was the first of several studies to uncover the critical role of deregulation of miRNA and ncRNA expression in the pathogenesis of several tumors, including leukemia and lymphoma. It gradually became clear that aberrant gene expression of both precursor and mature miRNAs occurred as a result of genomic alterations, deregulated processing machinery, or epigenetic mechanisms, with deregulated miRNAs functioning as oncogenes (oncomiRs) or tumor suppressors (Table 2). The miR-17-92 cluster and miR-155 were the first oncomiRs discovered, and their role in the pathogenesis of hematologic malignancies was validated using gain- and loss-of-function mouse models.93,94 He et al showed that overexpression of miR-17-92 accelerated C-MYC–induced tumorigenesis in a B-cell lymphoma model.93 Overexpression of the miR17-92 cluster is observed in several lymphoid malignancies95 and its oncogenic role is a result of the miRNAs within the cluster targeting critical genes (including PTEN, BIM, CDKN1A, and E2F) inducing lack of differentiation and increased proliferation and angiogenesis.95-98 Furthermore, deregulation of miR-17-92 either because of amplification or aberrant targeting by MLL proteins has been associated with MLL-rearranged ALL.29 Another notable oncomiR, miR-155, is amplified in several tumors,99,100 and specific overexpression in B cells leads to an expansion of the pre–B-cell compartment followed by the development of leukemia or high-grade lymphoma in transgenic mice.95-101 Other oncomiRs include miR-125a and miR-125b, which aberrantly target TNFAIP3, leading to constitutive NF-κB activation.102
Deregulated miRNAs in lymphoid neoplasms
| miRNA . | Disease . | Target Genes . | Genetic/Epigenetic deregulation . |
|---|---|---|---|
| miR-17-92 cluster (includes miR-17, miR-18a, miR-19a, miR-20a, miR-19b, and miR-92a) | DLBCL, MCL, Burkitt, FL, ALL | PTEN, BIM, CDKN1A, E2F TFs | Amplification upregulated by MLL |
| miR-155 | CLL, HD, pediatric Burkitt, DLBCL | Amplification | |
| miR-125a/miR-125b | DLBCL | TNFAIP3 | Amplification Upregulation |
| p15AS | AML, ALL | p15 | Upregulation |
| Tumor supressor miRNAs | |||
| miR-15a/miR-16-1 | CLL, NHL | BCL2, MCL-1 | Deleted Repressed by HDACs |
| miR-26a | Burkitt | EZH2 | Repressed by MYC |
| miR-29/miR-29b | CLL, MCL,DLBCL, Burkitt | CDK6,IGF-1R | Repressed by MYC |
| miR-31 | ATL | NIK | Repressed by PRC2 |
| miR-203 | MALT, ALL, CLL, MM | ABL1 | Promoter hypermethylation |
| miR-124 | ALL, NHL | CDK6 | Promoter hypermethylation |
| miRNA . | Disease . | Target Genes . | Genetic/Epigenetic deregulation . |
|---|---|---|---|
| miR-17-92 cluster (includes miR-17, miR-18a, miR-19a, miR-20a, miR-19b, and miR-92a) | DLBCL, MCL, Burkitt, FL, ALL | PTEN, BIM, CDKN1A, E2F TFs | Amplification upregulated by MLL |
| miR-155 | CLL, HD, pediatric Burkitt, DLBCL | Amplification | |
| miR-125a/miR-125b | DLBCL | TNFAIP3 | Amplification Upregulation |
| p15AS | AML, ALL | p15 | Upregulation |
| Tumor supressor miRNAs | |||
| miR-15a/miR-16-1 | CLL, NHL | BCL2, MCL-1 | Deleted Repressed by HDACs |
| miR-26a | Burkitt | EZH2 | Repressed by MYC |
| miR-29/miR-29b | CLL, MCL,DLBCL, Burkitt | CDK6,IGF-1R | Repressed by MYC |
| miR-31 | ATL | NIK | Repressed by PRC2 |
| miR-203 | MALT, ALL, CLL, MM | ABL1 | Promoter hypermethylation |
| miR-124 | ALL, NHL | CDK6 | Promoter hypermethylation |
ATL, adult T-cell leukemia.
On the contrary, several key miRNAs that target antiapoptotic genes are downregulated or deleted in lymphoid tumors. For example, miR-15a/16-1 acts as a tumor suppressor in CLL by targeting BCL2.103 More recently, epigenetic silencing of several miRNAs resulting from aberrant DNA methylation and altered histone modification patterns has been associated with the pathogenesis of lymphomas and leukemias. HDAC complexes mediate repression of miR-15a, miR-16, and miR-29b in CLL and in NHL.104,105 Treatment with HDACi induced the expression of these miRNAs, antagonizing survival protein MCL-1 and triggering cell death.104 Deregulated PRC2 complexes repress miR-31 in adult T-cell leukemia and lead to activation of NF-κB, triggering oncogenic signaling.106 DNA hypermethylation led to miR-124 and miR-203 silencing in several lymphoid malignancies, providing a basis for therapeutic targeting with demethylating agents.107-112 Moreover, genome-wide miRNA profiling studies in ALL further revealed an EZH2 targeted and aberrantly methylated miRNA signature, suggesting that these cases might benefit from EZH2 inhibition.107-111,113 Along the same lines, miR-26a and miR-29 are repressed by MYC during lymphomagenesis.114,115 EZH2 targeting by miR-26a might lead to global deregulation of gene expression, whereas MYC recruits HDAC3 and EZH2 complexes to aberrantly repress miR-29. Combined pharmacologic inhibition of HDAC and PRC2 complexes restored miR-29 levels, suppressing lymphoma growth. Alternatively, the ncRNA p15AS was shown to induce heterochromatin formation to epigenetically silence its target P15, a cyclin-dependent kinase inhibitor, in acute leukemia.116 Finally, leukemogenesis has also been associated with deregulation of some highly-conserved ncRNAs, namely transcribed ultraconserved regions, with unclear functions in CLL.117 As genome-wide ncRNA and epigenetic profiles of both normal and malignant cells become available, the integration of these datasets will further uncover the underlying mechanisms of epigenetic deregulation of miRNAs and facilitate the design of targeted therapeutic approaches in leukemia and lymphoma.
Future challenges
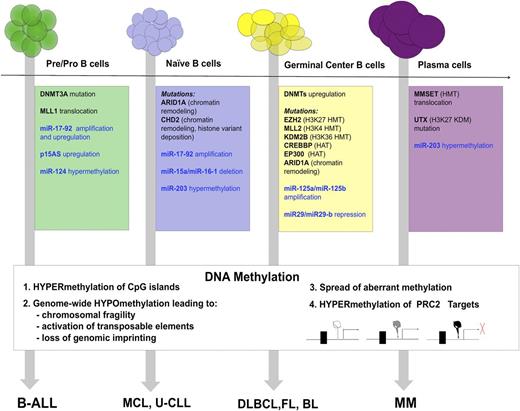
Complete understanding of the role epigenome plays in lymphomagenesis will require systematic study of a large number of cases using high-resolution techniques. Because the genome of each subtype of lymphoma proved to be unique, the epigenome similarly is emerging as a dynamic set of marks that is deregulated in a unique fashion in each lymphoid malignancy (Figure 1). In addition, a causal link is still missing between the deregulated epigenome and the development of the diseases. Moreover, given the increasing scale of the genome-wide genetic and epigenetic studies, a new generation of computer-savvy biologists is needed to provide solutions to the challenging data analysis. Until then, we only have small glimpses into the nature of epigenomic regulation.
Summary of epigenetic abnormalities that contribute to neoplastic transformation of normal B-cell precursors (on the top) to specific lymphoma subtypes (on the bottom). Abnormalities in histone- and DNA-modifying enzymes are within colored boxes in black, abnormalities in miRNAs are within colored boxes in blue. DNA methylation changes are summarized in the white box.
Summary of epigenetic abnormalities that contribute to neoplastic transformation of normal B-cell precursors (on the top) to specific lymphoma subtypes (on the bottom). Abnormalities in histone- and DNA-modifying enzymes are within colored boxes in black, abnormalities in miRNAs are within colored boxes in blue. DNA methylation changes are summarized in the white box.
The study of DNA methylation in lymphoid malignancies led to the accumulation of a large body of correlative studies linking changes in patterns and expression levels of methylation machinery to the disease. However, thus far, the amount of direct evidence linking changes in DNA methylation or its machinery to lymphomagenesis is insufficient. Further functional evidence including animal models is necessary to establish the cause and effect among deregulated DNA methylation machinery, aberrant DNA methylation pattern, and malignant transformation.
The challenge in solving the “malignant histone code” lies in the diverse nature of histone marks and their complex combinatorial effect that is difficult to interrogate. Moreover, careful functional characterization of newly discovered mutations within histone-modifying enzymes to identify true “driver” and/or “facilitator” mutations is in urgent need. The interplay between the aberrant DNA methylation pattern and the “malignant histone code” is yet another complicated question waiting to be addressed.
Finally, the ultimate goal is to integrate the genomic and epigenomic data to identify new therapeutic targets. High-throughput screening of therapeutic molecules promises to deliver many new candidate therapies. Their preclinical and clinical testing will require an increasing agility from regulatory agencies.
Acknowledgments
The authors thank Dr L. Cerchietti for editing the manuscript and Dr N. Weinhold for help with the figure design and graphics.
This work was supported by grants from the National Institutes of Health (K08 CA127353) and The Leukemia & Lymphoma Society (LLS 6304-11) (R.S.) and by an ASH Scholar Award (Y.J.).
Authorship
Contribution: Y.J., K.H., and R.S. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Rita Shaknovich, Department of Medicine, Weill Cornell Medical College, Building C Room 620C, 1300 York Ave, New York, NY 10065; e-mail: ris9004@med.cornell.edu.