In this issue of Blood, Leleu and colleagues1 and Richardson and colleagues2 publish two different trials using pomalidomide and dexamethasone in patients with relapsed and refractory multiple myeloma (MM).
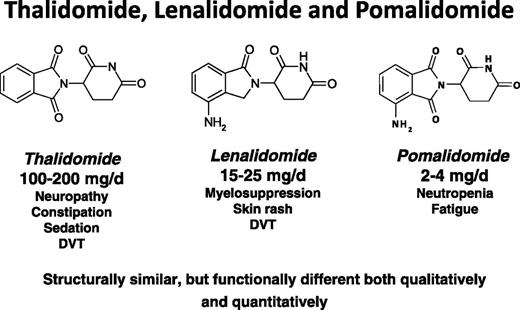
Structure, dose range, and common side effects of the three immunomodulatory drugs.
Structure, dose range, and common side effects of the three immunomodulatory drugs.
The introduction of immunomodulatory drugs (IMiDs), proteasome inhibitors, and other novel agents has dramatically improved the prognosis for patients with MM.3 However, once patients are no longer responsive to IMiDs and bortezomib, the prognosis is grave4 and new agents are needed. Pomalidomide is the newest IMiD. Evidence is mounting that suggests at least incomplete cross-resistance among thalidomide, lenalidomide, and pomalidomide,5-8 which have very similar chemical structures but differ markedly in their potency and side effects. Their mechanism of resistance to IMiDs is not known but recent studies suggest that a threshold level of cereblon expression is required for response to IMiD therapy.9
In this issue, Richardson and colleagues report their phase 1 dose-escalation study to determine the maximum tolerated dose (MTD) of pomalidomide given for 21 of 28 days per cycle in patients with relapsed and refractory MM.2 The population of patients was heavily pretreated with a median of six prior regimens that included bortezomib and lenalidomide. Dexamethasone was added in 22 patients for suboptimal responses. Among the 38 patients, treated responses of partial remission (PR) or better were seen in 21% and minor response or better in 42%. There were four dose-limiting toxicities (grade 4 neutropenia) at 5 mg/day, thus the MTD was 4 mg/day. Toxicity was manageable and side effects consisted primarily of neutropenia, anemia, thrombocytopenia, and fatigue. Also in this issue, Leleu and colleagues1 describe their randomized phase 2 study comparing different dosing schedules of pomalidomide and low-dose dexamethasone in dual refractory MM patients. Eighty-four patients with relapsed MM who were refractory to both bortezomib and lenalidomide were randomized to receive pomalidomide 4 mg for 21 of 28 days or 4 mg continuously with weekly dexamethasone. Overall response rates did not appear to be dose dependent (35% and 34%, respectively). They also found little difference in toxicity between the two dose schedules. The major toxicity was myelosuppression, with grade 3 or 4 neutropenia seen in 65% (21/28) and 58% (28/28) of patients. Pneumonia was seen more frequently in the continuous dose group. These two trials confirm the impressive results seen in other studies of pomalidomide in MM.
The dose of pomalidomide that should be used is a recurring question. Initial phase 1 trials established an MTD dose of 2 mg daily10 or 5 mg every other day.11 A series of phase 2 studies conducted at the Mayo Clinic5-7 used doses of 2 mg and 4 mg continuously for 28 days with dexamethasone 40 mg once weekly. In the first Mayo Clinic trial, responses of PR or better were seen in 63%6 of patients treated with 2 mg daily. This group of patients was less heavily pretreated than subsequent cohorts. A follow-up trial in lenalidomide refractory patients7 using pomalidomide 2 mg daily showed responses of PR or better in 32%. Among patients refractory to both lenalidomide and bortezomib,5 responses of PR or better were seen in 26% of the patients treated with 2 mg daily and 29% of those treated with 4 mg daily. Toxicity in all these trials was manageable and similar to what is reported by Richardson and colleagues in this issue and consisted primarily of neutropenia and fatigue.
At least one study suggests that the addition of clarithromycin may enhance antimyeloma activity of pomalidomide and dexamethasone. Mark and colleagues12 reported a phase 2 study that used clarithromycin 500 mg twice daily, pomalidomide 4 mg for days 1 to 21 of a 28-day cycle, and dexamethasone 40 mg weekly in 97 relapsed patients, many of whom were refractory to lenalidomide or both lenalidomide and bortezomib. They reported responses of PR or better in 53%.
How does one interpret this data in aggregate? It is important to look not only at MTD but at minimum effective dose as well. An analysis of 345 patients enrolled in the Mayo Clinic studies suggested the strongest predictors of response and survival were the number and type of prior regimens.13 The same appears to be true of the all other studies using pomalidomide for relapsed MM, with the best response rates reported in the patients who were the least heavily pretreated. Although Richardson and colleagues suggest that the data in the current study show a dose response in favor of the higher dose of pomalidomide, it should be noted that there were only 6 patients treated at the 2-mg dose level. In aggregate, the Mayo Clinic trials treated 129 patients with the 2 mg/day schedule. The only difference in outcomes we have observed between the 2-mg and 4-mg dose levels is a slightly higher rate of neutropenia in patients receiving the higher doses. Current data suggest that either 2 mg/day continuously or 4 mg for 21 of 28 days is effective and well tolerated.
How does pomalidomide differ from the other IMiDs? Like thalidomide and lenalidomide, pomalidomide is taken orally and responses occur rapidly. Pomalidomide induces less asthenia and neuropathy than thalidomide. Pomalidomide is more likely to induce neutropenia than thalidomide, but this side effect is generally easily managed with a dose reduction. Although lenalidomide is less myelosuppressive than many chemotherapeutic agents, there is a subset of MM patients who are sensitive to the myelosuppressive effects of lenalidomide and have trouble tolerating even very low doses. These patients often do well with pomalidomide, suggesting there are fewer myelosuppressive effects with pomalidomide. Finally, skin rash is commonly seen with lenalidomide but is rarely seen with pomalidomide.
Although the introduction of new agents has significantly improved the prognosis for patients with MM, new therapies are needed. Pomalidomide is effective and well tolerated in patients with advanced, refractory disease and provides an “ideal” treatment option for the management of relapsed MM.
Conflict-of-interest disclosure: M.Q.L. received research funding for clinical trials from Celgene.