In this issue of Blood, Gudbrandsdottir et al from Denmark report that in the largest multicenter cohort to date comprising newly diagnosed adults with primary immune thrombocytopenia (ITP), addition of rituximab (RTX) to high-dose dexamethasone (DEX) as first-line therapy yields higher sustained response rates.
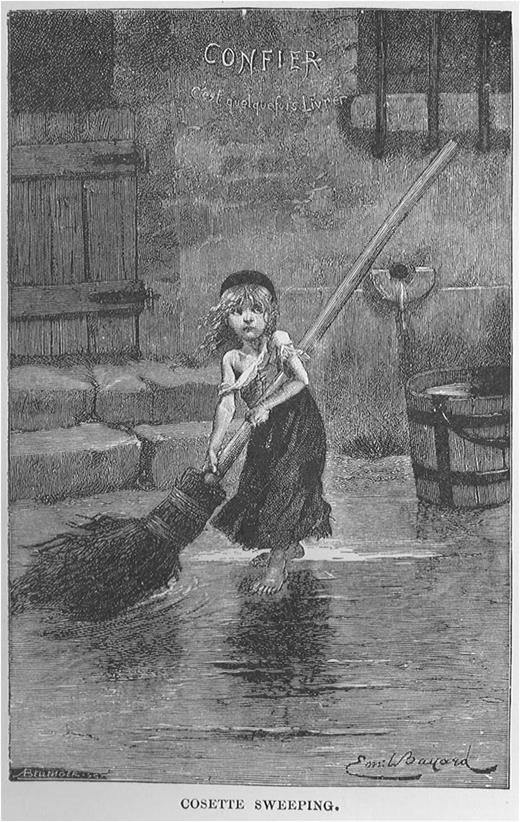
Cosette as depicted in a painting on the cover of the novel Les Misérables11
Cosette as depicted in a painting on the cover of the novel Les Misérables11
If all the ailments covered under hematology were characters in Victor Hugo’s novel Les Misérables, ITP might rank as someone like Cosette, who is considered by some literary critics as an inconsequential character that adorns the cover while serving as a mere prop for imbibing parental and romantic love with changing fortunes (see figure). After recalling orphaned Cosette’s rescue by Jean Valjean from wily innkeeper Thenardier and their tumultuous journey through the course of the novel with its historical backdrop of revolutionary 19th-century France, one should ponder the plight of a patient with ITP today.
German physician and poet Paul Gottlieb Werlhof originally described ITP in a 16-year-old girl in 1735, more than 100 years before Victor Hugo published his novel in 1862. Others have astutely summarized the intriguing history of ITP consisting of fascinating observations and game-changing discoveries, an approximate incidence of 6 per 100 000, and good paradigms for its treatment following the licensing of thrombopoietin mimetic agents.1,2
However, any patient with leukemias—including chronic myeloid leukemia or even the rarer acute promyelocytic leukemia—presenting to hematology clinics in the developed world today is likely to be offered a more definitive and targeted treatment as part of a randomized clinical trial in a cooperative group than if he or she has newly diagnosed ITP. There are no collaborative clinical groups or registries for prospectively diagnosing, observing (as spontaneous remissions though rare in adults often occur in children), and treating newly diagnosed ITP patients as part of a clinical trial. Corticosteroids and intravenous immunoglobulin introduced in 1951 and 1981, respectively, are the mainstays of immediate intervention. Splenectomy, in use for almost 100 years, is the only therapy with a curative potential.3,4
Despite its widespread use for more than a decade, because of lack of data from randomized trials that can satisfy the US Food and Drug Administration, rituximab use in ITP has remained off-label in North America.5 Evidence-based guidelines offer a grade 2C recommendation for its use as a reasonable second-line option.6 The premise of using B-cell depletion therapy in ITP with no consistent antibody to follow as a surrogate marker of disease activity poses challenges. Although the majority of B cells reside in bone marrow and lymphoid tissue, RTX mostly depletes circulating peripheral blood B cells.7 Current regimens of RTX borrowed from the lymphoma clinics may not be optimal in depleting B cells from lymphoid tissues in nonmalignant conditions. Long-lived plasma cells, the source of most autoantibodies, do not express CD20 and are not depleted by RTX.
Gudbrandsdottir and colleagues from 9 hospitals in Denmark report the largest prospective, randomized cohort study to date of newly diagnosed primary ITP patients with a 4-year follow-up.8 Their study compares concurrent use of RTX and high-dose DEX (n = 49) with DEX alone (n = 52) as first-line therapy, with a median follow-up of 921 and 922 days, respectively. At 12-month follow-up, sustained partial or complete response was achieved in 53% in the RTX+DEX group and 33% in DEX monotherapy group (P < .05). By combining high-dose DEX with RTX, this study avoided immediate RTX “failures”—a result of responses lagging by 6 to 8 weeks when RTX is used as a single agent, often requiring concurrent rescue medications. Based on their study, the authors propose instead to use RTX early in the course of the treatment of ITP, even before splenectomy.
Similar studies to determine the feasibility of recruitment, protocol adherence, and blinding of a larger trial of RTX vs placebo to evaluate role of adjuvant RTX in nonsplenectomized adults with ITP saw no difference in the outcome with or without RTX. After recruiting 60 patients over 46 months, this study from Canada closed because of insufficient accrual. Rate of refusal was high (42%) because of patients’ unwillingness to be randomized to the placebo arm.9
One of the secondary end points of the study by Gudbrandsdottir et al was time to rescue treatment. Significant difference was noted between the 2 groups, favoring those receiving RTX+DEX. More serious adverse events (n = 16 vs 9) and infections (n = 11 vs 9) were noted in the RTX+DEX cohort than DEX single-agent cohort. Serum immunoglobulin-G and -A levels were decreased in all that could be tested, but were still within the normal range, similar to what was observed by others.9 However, there are publications cautioning against persistent hypogammaglobulinemia following rituximab exposure in patients that received rituximab for autoimmune and autoinflammatory conditions.10
Designing appropriate trials addressing rituximab dosage and scheduling in ITP is imperative and using it concurrently with corticosteroids might actually confer some benefit by minimizing infusion reactions. Using this Danish design as a template, future clinical trials in newly diagnosed ITP patients should study its natural history, pathophysiology, and T- and B-cell dysfunction that can lead to identification and validation of appropriate biomarkers of ITP as the disease evolves in an individual patient. This would allow us to move forward from the prevailing empiricism in ITP therapeutics to effective targeting and appropriate risk-benefit assessment with different classes of medications while being wary of the cost structure for all of them (Table 1).
Prices of all currently available medications used for ITP
| Commonly used ITP drugs . | Unit . | Suggested warehouse price per unit (US $) . | Price for 1 month or a single-course treatment in an adult (US $) . |
|---|---|---|---|
| Prednisone | 20 mg (100 tablets) | $8 from Costco Pharmacy | $16 |
| Dexamethasone | 4 mg (40 tablets) | $13.20 from Costco Pharmacy | $52.80 |
| IVIG (Gamunex 10%) | 40 g | $4824 | $9648 |
| WinRho | 5000 IU | $1351.72 | $1351.72 |
| Rituximab | 500 mg | $3899.16 | $15 596.64 |
| Romiplostim | 250 μg SDV 0.5 mL | $1433.10 | $5732.40 |
| Eltrombopag | 50 mg (30 tablets) | $5934.54 | $5934.54 |
| Commonly used ITP drugs . | Unit . | Suggested warehouse price per unit (US $) . | Price for 1 month or a single-course treatment in an adult (US $) . |
|---|---|---|---|
| Prednisone | 20 mg (100 tablets) | $8 from Costco Pharmacy | $16 |
| Dexamethasone | 4 mg (40 tablets) | $13.20 from Costco Pharmacy | $52.80 |
| IVIG (Gamunex 10%) | 40 g | $4824 | $9648 |
| WinRho | 5000 IU | $1351.72 | $1351.72 |
| Rituximab | 500 mg | $3899.16 | $15 596.64 |
| Romiplostim | 250 μg SDV 0.5 mL | $1433.10 | $5732.40 |
| Eltrombopag | 50 mg (30 tablets) | $5934.54 | $5934.54 |
The splenectomy procedure itself costs approximately US $20 000.2
Findings reported in the current issue of Blood do underscore that a multicenter clinical trial in adult ITP with long-term follow-up is feasible.8 The time has come for clinicians that care for patients with newly diagnosed ITP to enroll them in controlled trials to investigate the role of immunosuppression in relation to newer agents such as thrombopoietin agonists. After all, despite insipid characterization by Victor Hugo, Cosette’s fortunes do change during the course of Les Misérables—from an abused and orphaned urchin to a millionaire heiress of Jean Valjean’s wealth and she lives happily ever after married to Marius.11 Let us hope for a comparable outcome for all the new patients with ITP, a relatively common medical condition benevolently neglected by clinical trialists until now.
Acknowledgment
Drug prices were researched and provided by Dr Timothy Jancel, Pharmacy Department, National Institutes of Health Clinical Center. The author is grateful to Dr Michael Sneller for reviewing the manuscript and providing valuable comments.
This research was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
National Institutes of Health
Conflict-of-interest disclosure: The author declares no competing financial interests.