Abstract
Human T-cell leukemia virus type 1–associated adult T-cell leukemia/lymphoma (ATL) typically has survivals measured in months with chemotherapy. One prior published series (1983-1991) assessed local radiotherapy for ATL. Ten consecutive patients with pathologically confirmed ATL treated with radiotherapy were reviewed. Subtypes included acute (n = 7), smoldering (n = 2), and lymphomatous (n = 1). Patients received an average of 2.5 systemic therapy regimens before radiotherapy. Twenty lesions (cutaneous = 10, nodal = 8, extranodal = 2) were treated to a mean of 35.4 Gy/2-3 Gy (range, 12-60 Gy). At 9.0-month mean follow-up (range, 0.1-42.0 months), all lesions symptomatically and radiographically responded, with in-field complete responses in 40.0% (nodal 37.5% vs cutaneous 50.0%; P = .62). No patient experienced in-field progression. Nine patients developed new/progressive out-of-field disease. Median survival was 17.0 months (3-year survival, 30.0%). No Radiation Therapy Oncology Group acute grade ≥ 3 or any late toxicity was noted. This report is the first to use modern radiotherapy techniques and finds effective local control across ATL subtypes. Radiotherapy should be considered for symptomatic local progression of ATL.
Introduction
Adult T-cell leukemia/lymphoma (ATL) is a rare peripheral T-lymphoma characterized by blood and bone marrow involvement, hepatosplenomegaly, hypercalcemia, and cutaneous and lytic bone lesions.1 ATL is most prevalent in Southwestern Japan, the Caribbean basin, intertropical Africa, the Middle East, and in African American populations in the Southeastern United States. ATL develops in ≤ 6% of persons infected with human T-cell leukemia virus type 1 (HTLV-1) 20-60 years after infection.1-6
Acute (60% of cases) and lymphomatous (20%) ATL typically have aggressive disease courses with shortened median survivals and are characterized by large tumor burdens, multiorgan failure, hypercalcemia, and infectious complications.2,7 The median survival of aggressive ATL subtypes ranges from < 1 month untreated8 to 4-6 (acute) and 9-10 (lymphomatous) months with intensive therapy.1,6,9-11 Chronic (15%) and smoldering (5%) ATL are more indolent, with median survivals of 17-24 and 34 to ≥ 60 months, respectively.1,6,9-11 Transformation into aggressive subtypes is common.12 Across subtypes, the 5-year overall survival is 14%.13 The 2- and 4-year survival rates, respectively, are 16.7% and 5.0% for acute, 21.3% and 5.7% for lymphomatous, 52.4% and 26.9% for chronic, and 77.7% and 62.8% for smoldering ATL.9,10,14
ATL treatment is based on subclassification, pretreatment prognostic factors, and response to initial therapy.7 Intensive multidrug chemotherapy regimens are often used for aggressive subtypes. However, disease progression occurs in ≤ 80% of patients, and complete responses are infrequent.15
The role for radiotherapy in ATL is not well defined, even for symptom palliation. No large study or randomized trial exists, which assesses the role of radiotherapy for ATL. Only 1 prior case series of patients with ATL treated over 20 years ago used localized external beam radiotherapy.16,17 We report a patient series treated with modern radiotherapy techniques to assess the role of external beam radiotherapy for ATL. We evaluated symptomatic response and local control in these patients.
Methods
This retrospective analysis reviewed 10 consecutive patients with pathologically confirmed ATL treated with radiotherapy at the National Institutes of Health (NIH) between 1997 and 2010. The diagnosis was based on pathologic confirmation of T-cell lymphoma/leukemia, a clinical picture consistent with ATL, and serologic evidence of HTLV-1 infection. This research was approved by the relevant institutional review boards.
Patients were referred for radiotherapy for local disease control, palliation of symptomatic lesions, or sterilization of a single site of disease. Patients underwent weekly evaluations during radiotherapy and 1 month after the completion of radiotherapy or just before their departure from NIH.
Uniform surveillance after treatment was not possible because of geographic constraints (patients residing in the Caribbean). During subsequent patient visits to NIH for assessment or treatment of disease progression, comprehensive skin assessments and lymph node evaluations were performed. Computerized tomography (CT) was obtained to assess radiotherapy response and for systemic disease assessment. Study follow-up was determined from (1) the last CT, magnetic resonance imaging, or positron emission tomography scan after radiotherapy completion for patients with visceral/nodal disease; (2) last comprehensive skin examination for patients with cutaneous disease; or (3) patient death.
Treatment response was assessed with the Japan Clinical Oncology Group criteria for ATL modified according to International Consensus Meeting recommendations.7 Complete response was defined as disappearance of all clinical/radiographic evidence of disease within the treatment field and no new in-field lesions, with all lymph nodes regressed to normal size (≤ 1.5 cm in greatest transverse diameter, or ≤ 1.0 cm in previously involved nodes that were ≤ 1.5 cm). Partial response was defined as ≥ 50% reduction in the sum of the products of the perpendicular diameters of all measurable disease lesions without new in-field lesions. Absolute percentage of residual abnormal lymphocytes and bone marrow analysis were not used to define response.
Local failure was defined as any identifiable disease on examination or radiographic assessment, which remained within the treatment field measured at 30 days after radiotherapy or last follow-up. Patients with partial responses or reappearance of tumor after complete responses were defined to have local failures. Locoregional failure was any new identifiable disease adjacent to the radiation field, including regional lymph nodes or satellite cutaneous lesions. Distant failure was the development of new distant cutaneous, nodal, visceral, or systemic disease.
Statistical analysis was performed with Excel for Windows (Microsoft Office 2003). χ2 statistic and Fisher exact test for discrete variables were used to compare proportions, and Student t test was used for continuous variables. Statistical significance was defined as P < .05.
Results and discussion
Patients
All 10 patients were of African descent from the Caribbean (Jamaica n = 9, Haiti n = 1; Table 1). Most were women (n = 9) and had a mean age of 48.0 years (range, 30-65 years). They had acute (n = 7), smoldering (n = 2), or stage IV lymphomatous (n = 1) ATL. Before radiotherapy, in addition to systemic corticosteroids, patients received an average of 2.5 chemotherapy regimens (range, 1-4). Patients received radiotherapy at a mean of 12.3 months (range, 5-24 months) after their diagnosis.
Treatment responses to radiation therapy according to ATL lesion type
| Patient . | ATL subtype . | Prior systemic therapy . | RT site . | Lesion type . | RT source . | RT energy . | Total dose, Gy . | Frac-tion dose, Gy . | Initial local response . | In-field relapse . | Out-of-field relapse . | Additional therapy after RT . | Time from RT to last evaluation, mo . | Disease at last evaluation . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Acute | CHOP | Lt neck, Bl supraclav | Nodal | Photon | 6/15 MV | 30 | 3 | PR | No | Yes | Fludarabine/ cyclophosphamide/ LMB-2 | 2.4 | Local* + distant |
| 2 | Lymphomatous | Alemtuzumab | Rt groin | Nodal | Electron | 6 MeV | 24 | 2 | CR | No | Yes† | CHOP/denileukin diftitox | 16.7 | Distant* |
| 3 | Smoldering | Daclizumab, alemtuzumab | Rt scapula | Cutaneous | Electron | 9 MeV | 36 | 3 | PR | No | Yes† | Alemtuzumab, etoposide | 42.0 | Local + distant |
| 4 | Acute | CHOP, fludarabine/ cyclophosphamide/LMB-2, denileukin diftitox | Lt pelvic mass | Nodal | Photon | 15 MV | 20 | 2 | CR | No | Yes† | EPOCH/fludarabine, allo-transplant, intrathecal methotrexate, EPOCH/fludarabine | 10.0 | Local + distant |
| 5 | Acute | EPOCH/alemtuzumab, intrathecal methotrexate, fludarabine/cyclophosphamide/LMB-2 | Rt groin | Cutaneous | Photon | 6 MV | 30 | 3 | PR | No | Yes | No | 1.6 | Local* + distant |
| Rt ankle | Cutaneous | Photon | 6 MV | 30 | 3 | PR | No | |||||||
| Lt orbit | Extra-nodal | Photon | 6 MV | 15 | 3 | PR | No | |||||||
| 6 | Smoldering | EPOCH/rituximab/siplizumab, 7-hydroxystaurosporine, denileukin diftitox, nelfinavir/ alemtuzumab | Forehead | Cutaneous | Electron | 6 MeV | 50 | 2 | CR | No | Yes† | No | 15.8 | Local + distant |
| Lt lower extremity | Cutaneous | Electron | 6 MeV | 50 | 2 | CR | No | |||||||
| Rt lower extremity | Cutaneous | Photon | 6 MV | 50 | 2 | PR | No | |||||||
| Lt ankle | Cutaneous | Photon | 6 MV | 60 | 2 | CR | No | |||||||
| Lt nares, malar eminence | Cutaneous | Electron | 9 MeV | 60 | 2 | PR | No | |||||||
| Submental chin | Cutaneous | Electron | 6 MeV | 50 | 2 | CR | No | |||||||
| Rt Achilles heel | Cutaneous | Photon | 6 MV | 50 | 2 | CR | No | |||||||
| 7‡ | Acute | CHOP, denileukin diftitox | Bl neck | Nodal | Photon | 6/15 MV | 50 | 2 | PR | No | No | No | 0.3 | Local |
| 8 | Acute | EPOCH/rituximab, denileukin diftitox, alemtuzumab | Lt neck, supraclav | Nodal | Photon | 6 MV | 12 | 3 | PR | No | Yes | No | 0.1 | Local* + distant |
| Rt head/neck | Nodal | Electron | 9 MeV | 12 | 3 | CR | No | |||||||
| 9 | Acute | CHOP, alemtuzumab/ deoxycoformycin, intrathecal methotrexate | Whole brain | Lepto-meningeal | Photon | 6 MV | 30 | 3 | PR | No | Yes | No | 0.4 | Local* + distant |
| 10 | Acute | CHOP, EPOCH, yttrium-90 daclizumab | T-spine | Nodal | Photon | 15 MV | 24 | 2 | PR | No | Yes | No | 0.3 | Local* + distant |
| C-spine | Nodal | Photon | 6 MV | 24 | 2 | PR | No |
| Patient . | ATL subtype . | Prior systemic therapy . | RT site . | Lesion type . | RT source . | RT energy . | Total dose, Gy . | Frac-tion dose, Gy . | Initial local response . | In-field relapse . | Out-of-field relapse . | Additional therapy after RT . | Time from RT to last evaluation, mo . | Disease at last evaluation . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Acute | CHOP | Lt neck, Bl supraclav | Nodal | Photon | 6/15 MV | 30 | 3 | PR | No | Yes | Fludarabine/ cyclophosphamide/ LMB-2 | 2.4 | Local* + distant |
| 2 | Lymphomatous | Alemtuzumab | Rt groin | Nodal | Electron | 6 MeV | 24 | 2 | CR | No | Yes† | CHOP/denileukin diftitox | 16.7 | Distant* |
| 3 | Smoldering | Daclizumab, alemtuzumab | Rt scapula | Cutaneous | Electron | 9 MeV | 36 | 3 | PR | No | Yes† | Alemtuzumab, etoposide | 42.0 | Local + distant |
| 4 | Acute | CHOP, fludarabine/ cyclophosphamide/LMB-2, denileukin diftitox | Lt pelvic mass | Nodal | Photon | 15 MV | 20 | 2 | CR | No | Yes† | EPOCH/fludarabine, allo-transplant, intrathecal methotrexate, EPOCH/fludarabine | 10.0 | Local + distant |
| 5 | Acute | EPOCH/alemtuzumab, intrathecal methotrexate, fludarabine/cyclophosphamide/LMB-2 | Rt groin | Cutaneous | Photon | 6 MV | 30 | 3 | PR | No | Yes | No | 1.6 | Local* + distant |
| Rt ankle | Cutaneous | Photon | 6 MV | 30 | 3 | PR | No | |||||||
| Lt orbit | Extra-nodal | Photon | 6 MV | 15 | 3 | PR | No | |||||||
| 6 | Smoldering | EPOCH/rituximab/siplizumab, 7-hydroxystaurosporine, denileukin diftitox, nelfinavir/ alemtuzumab | Forehead | Cutaneous | Electron | 6 MeV | 50 | 2 | CR | No | Yes† | No | 15.8 | Local + distant |
| Lt lower extremity | Cutaneous | Electron | 6 MeV | 50 | 2 | CR | No | |||||||
| Rt lower extremity | Cutaneous | Photon | 6 MV | 50 | 2 | PR | No | |||||||
| Lt ankle | Cutaneous | Photon | 6 MV | 60 | 2 | CR | No | |||||||
| Lt nares, malar eminence | Cutaneous | Electron | 9 MeV | 60 | 2 | PR | No | |||||||
| Submental chin | Cutaneous | Electron | 6 MeV | 50 | 2 | CR | No | |||||||
| Rt Achilles heel | Cutaneous | Photon | 6 MV | 50 | 2 | CR | No | |||||||
| 7‡ | Acute | CHOP, denileukin diftitox | Bl neck | Nodal | Photon | 6/15 MV | 50 | 2 | PR | No | No | No | 0.3 | Local |
| 8 | Acute | EPOCH/rituximab, denileukin diftitox, alemtuzumab | Lt neck, supraclav | Nodal | Photon | 6 MV | 12 | 3 | PR | No | Yes | No | 0.1 | Local* + distant |
| Rt head/neck | Nodal | Electron | 9 MeV | 12 | 3 | CR | No | |||||||
| 9 | Acute | CHOP, alemtuzumab/ deoxycoformycin, intrathecal methotrexate | Whole brain | Lepto-meningeal | Photon | 6 MV | 30 | 3 | PR | No | Yes | No | 0.4 | Local* + distant |
| 10 | Acute | CHOP, EPOCH, yttrium-90 daclizumab | T-spine | Nodal | Photon | 15 MV | 24 | 2 | PR | No | Yes | No | 0.3 | Local* + distant |
| C-spine | Nodal | Photon | 6 MV | 24 | 2 | PR | No |
RT indicates radiation therapy; CHOP, cyclophosphamide, doxorubicin, vincristine, prednisolone; Lt, left; Bl, bilateral; PR, partial response; Rt, right; CR, complete response; and EPOCH, etoposide, doxorubicin, vincristine, cyclophosphamide, prednisone.
Disease status at the time of patient mortality.
Patients with new out-of-field disease, as opposed to patients with out-of-field progression of disease that was evident before starting radiation therapy. The times from the completion of radiation therapy to the identification of new out-of field disease in these patients were as follows: patient 2, 9.7 mo; patient 3, 13.8 mo; patient 4, 0.9 mo; and patient 6, 1.9 mo (mean, 6.6 mo).
This male patient was from Haiti. The remaining 9 patients were women from Jamaica.
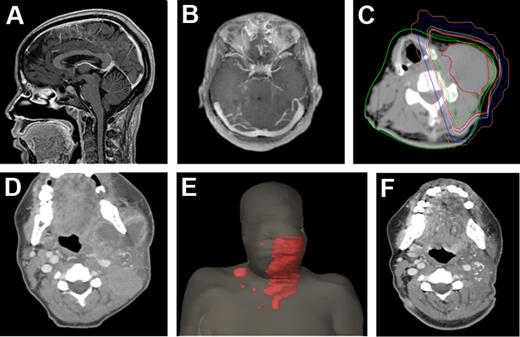
All 20 disease sites treated were symptomatic before irradiation. Patients received radiotherapy to lymph nodes (n = 8; Figure 1), cutaneous lesions (n = 10), whole brain for leptomeningeal disease (n = 1), and a unilateral orbit (n = 1).
Extent of disease among the ATL patient cohort. CT slices in the sagittal (A) and axial (B) planes of a patient with leptomeningeal disease. (C) CT slice in the axial plane of a patient with extensive cervical neck lymphadenopathy. The patient was treated with a right anterior oblique and left posterior oblique photon beam arrangement to gross adenopathy, contoured in red, with radiation isodose lines also depicted (green indicates 102% of the prescribed dose; red, 100%; yellow, 99%; lavender, 98%; cyan, 95%; dark blue, 50%; and pink, 20%). (D) Disease extent in another patient with bilateral, left greater than right, cervical and supraclavicular lymphadenopathy depicted in the axial plan and (E) as a 3-dimensional body reconstruction image with gross tumor contoured in red. (F) Treatment response of the same patient depicted in panels D and E, shown in the axial plane at 7 weeks after photon radiation therapy to the left neck only. A strong partial response to radiation therapy was obtained in this patient.
Extent of disease among the ATL patient cohort. CT slices in the sagittal (A) and axial (B) planes of a patient with leptomeningeal disease. (C) CT slice in the axial plane of a patient with extensive cervical neck lymphadenopathy. The patient was treated with a right anterior oblique and left posterior oblique photon beam arrangement to gross adenopathy, contoured in red, with radiation isodose lines also depicted (green indicates 102% of the prescribed dose; red, 100%; yellow, 99%; lavender, 98%; cyan, 95%; dark blue, 50%; and pink, 20%). (D) Disease extent in another patient with bilateral, left greater than right, cervical and supraclavicular lymphadenopathy depicted in the axial plan and (E) as a 3-dimensional body reconstruction image with gross tumor contoured in red. (F) Treatment response of the same patient depicted in panels D and E, shown in the axial plane at 7 weeks after photon radiation therapy to the left neck only. A strong partial response to radiation therapy was obtained in this patient.
Radiotherapy
Lesions were treated with photons (n = 13; all 2-field; 6-15 MV) or electrons (n = 7; single en face field; 6-9 MeV). Bolus (0.5-1.0 cm) was used for 75% of lesions. Patients were treated to a mean dose of 35.4 Gy (range, 12-60 Gy) in 2-Gy (n = 12) or 3-Gy (n = 8) fractions over a mean of 16 fractions (range, 4-30 fractions).
Radiotherapy response
All patients reported symptomatic improvement after radiotherapy, including decreased/resolved pain, pruritus, ulcerations, headaches, paresthesias, trismus, brachial plexopathy, difficulty with ambulation, or B symptoms.
At a mean of 9.0 months (range, 0.1-42.0 months) after radiotherapy, radiographic and/or clinical response was achieved in all 20 lesions. Partial responses were observed at 60.0% of sites. Complete responses were achieved in 40.0%, with similar complete response rates for nodal and cutaneous lesions (37.5% vs 50.0%; P = .62). Throughout the follow-up period, no in-field progression occurred for any irradiated site (0 of 20 lesions). Five patients experienced out-of-field progression of disease that was evident before radiotherapy. Four patients developed new distant disease. With a partial response indicative of residual local disease, at last evaluation, 8 patients had local and distant disease, 1 had distant-only disease, and 1 had local-only disease. Because of distant disease progression, 4 patients received multidrug chemotherapy initiated at a mean of 8.9 months (range, 0.4-14.4 months) after radiotherapy.
Six patients died of progressive disease, with 3 deaths occurring within 1 month of radiotherapy completion. The 5 patients with acute ATL who died in this cohort did so at a mean of 1.0 month (range, 0.1-2.4 months) after radiotherapy and 10.6 months after diagnosis (range, 5.3-17.9 months). The remaining death occurred in a lymphomatous patient 16.6 months after radiotherapy (31.4 months after diagnosis).
The median survival for the group was 17.0 months (1.4 years). Patients lived a mean of 2.0 years (range, 0.4-4.5 years) from diagnosis to last evaluation/death, with a 2.9-year mean survival (range, 0.7-4.5 years) to date among the 4 patients alive at last evaluation. Both patients with nonaggressive subtypes are alive at a mean of 4.0 years (range, 3.4-4.5 years) from diagnosis and 2.4 years (range, 1.3-3.5 years) after radiotherapy. The 1-, 2-, and 3-year survivals for the entire cohort after diagnosis were 70.0%, 40.0%, and 30.0%, respectively.
Toxicity
Acute toxicity was grade 1 in 2 patients (4 lesions) and grade 2 in 2 patients (5 lesions). Acute toxicities were cutaneous/skin (grade 1 in 3 lesions, grade 2 in 3 lesions), odynophagia/mucositis (grade 1 in 1 patient, grade 2 in 1 patient), and ocular (grade 2 in 1 patient). No patient had any acute grade ≥ 3 toxicity. No patient experienced any Radiation Therapy Oncology Group late toxicity.
This is one of the largest studies to assess radiotherapy for the treatment of HTLV-1–associated ATL and is the first to use modern radiotherapy techniques. This study found that radiotherapy can achieve excellent local control and symptomatic improvement across a variety of lesion types and ATL subtypes, with both symptomatic improvement and clinical/radiographic disease response in all 20 lesions treated, and no in-field disease progression throughout the follow-up period. This study also found the complete response rate did not differ by lesion type or ATL subtype. However, despite excellent local control, 9 of 10 patients developed new or progressive distant disease.
Radiotherapy was well tolerated. Despite doses up to 60 Gy for cutaneous lesions and 50 Gy for nodal disease, acute toxicities were mild and resolved spontaneously. No late toxicity was observed.
The 40.0% 2-year and 30.0% 3-year survival in this series is longer than that of other reports, particularly because 70.0% of our patients had acute ATL that is associated with a historical 16.7% 2-year survival.9,10,14 Although this report assessed 10 consecutive patients who received radiotherapy, the lengthy survival observed may be attributable to fewer referrals of patients with high systemic disease burdens or poor performance statuses.
The only prior reported patient series of localized radiotherapy for ATL was conducted by investigators at Kumamoto University Hospital. In their 5-patient series, total clinical resolution of nodal disease occurred with 30 Gy.16 In their subsequent report of 30 patients treated with radiotherapy from 1983 to 1991, patients received high-energy x-rays, cobalt-60 γ rays, or electrons to 10.8-40.0 Gy in 1.5- to 2.0-Gy daily fractions to nodal lesions (n = 17 patients), 30.0 Gy in 3-Gy fractions administered 3 times weekly to focal cutaneous lesions (n = 6), or 30.0 Gy in 1.5-Gy fractions with alternating fields treated twice weekly to the total skin (n = 7). Cutaneous patients all achieved partial or complete responses and had a 37.7-month mean survival. Nodal patients were less likely to respond (69%) and had a 5.4-month mean survival.17 Unlike with that cohort, the present study used modern radiotherapy treatment planning strategies to treat all fields each treatment day, administering daily fractions, using more standard fraction sizes of 2-3 Gy, and using all linear accelerator-based therapy rather than older cobalt-60 equipment.
Radiotherapy is well tolerated and can achieve excellent local control and universal symptomatic improvement in patients with ATL. Radiotherapy should be considered for palliation for patients with ATL with symptomatic local disease progression and may currently be underused, particularly among patients with good performance statuses. Distant progression remains common. Radiotherapy should be integrated into multimodality therapy for patients with ATL.
Poster presented, in part, at the 53rd annual meeting of the American Society for Radiation Oncology, Miami, FL, October 3, 2011.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study is supported, in part, by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Center for Cancer Research.
National Institutes of Health
Authorship
Contribution: C.B.S. and A.K. contributed to study concept and design; C.B.S., J.C.M., D.M.S., N.E.U., J.E.J., R.J.K., E.L., K.C., G.W., T.A.W., and A.K. performed data collection and analysis; C.B.S. and A.K. performed statistical analysis; C.B.S. and A.K. drafted the manuscript and created the figure and table; C.B.S., J.C.M., D.M.S., N.E.U., J.E.J., R.J.K., E.L., K.C., G.W., T.A.W., and A.K. critically reviewed the manuscript and read and approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Aradhana Kaushal, National Institutes of Health, National Cancer Institute, Radiation Oncology Branch, Building 10, CRC Rm B2-3561, 10 Center Dr, MSC 1682, Bethesda, MD 20892-1682; e-mail: kaushala@mail.nih.gov.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal