Abstract
Rapid laboratory assessment of heparin-induced thrombocytopenia (HIT) is important for disease recognition and management. The utility of contemporary immunoassays to detect antiplatelet factor 4 (PF4)/heparin antibodies is hindered by detection of antibodies unassociated with disease. To begin to distinguish properties of pathogenic anti-PF4/heparin antibodies, we compared isotype-matched monoclonal antibodies that bind to different epitopes: KKO causes thrombocytopenia in an in vivo model of HIT, whereas RTO does not. KKO binding to PF4 and heparin is specifically inhibited by human HIT antibodies that activate platelets, whereas inhibition of RTO binding is not differentially affected. Heparin increased the avidity of KKO binding to PF4 without affecting RTO, but it did not increase total binding or binding to nontetrameric PF4K50E. Single-molecule forced unbinding demonstrated KKO was 8-fold more reactive toward PF4 tetramers and formed stronger complexes than RTO, but not to PF4K50E dimers. KKO, but not RTO, promoted oligomerization of PF4 but not PF4K50E. This study reveals differences in the properties of anti-PF4 antibodies that cause thrombocytopenia not revealed by ELISA that correlate with oligomerization of PF4 and sustained high-avidity interactions that may simulate transient antibody-antigen interactions in vivo. These differences suggest the potential importance of epitope specificity in the pathogenesis of HIT.
Introduction
Heparin-induced thrombocytopenia (HIT) is a thrombotic complication of heparin therapy mediated by antibodies to complexes between platelet factor 4 (PF4) and heparin or glycosaminoglycans (GAGs).1-3 However, antibodies to PF4/heparin are detected by ELISA far more frequently than antibodies that activate platelets or than clinical disease.4-6 For example, anti-PF4/heparin antibodies are detected in 25% to 60% of patients who receive unfractionated heparin after cardiopulmonary bypass surgery and a high proportion of hospitalized patients in other medical settings,4,7-9 an incidence that far exceeds the prevalence of HIT.1,10 The reason why only a fraction of patients with anti-PF4 antibodies detected by ELISA develop HIT is unclear and is only partially explained by antibody titer and IgG isotype.5,9,11-14
One clue to the differences in the pathogenic potential of anti-PF4/heparin antibodies may begin with the finding that heparin and PF4 form complexes of diverse size that depend on the molar ratio of the reactants.15-17 HIT antibodies and the HIT-like monoclonal antibody KKO bind and activate platelets and monocytes and promote thrombosis in an animal model over a narrow molar ratio of reactants.18,19 At these molar ratios, ultralarge complexes (ULCs) form in solution between heparin and multiple PF4 tetramers capable of binding multiple antibody molecules16 that in the case of platelets may lead to sustained engagement of FcRγIIA, which initiates aggregation.20-22
Molecular replacement studies reveal a track of amino acids on the surface of the PF4 tetramer required for binding of a HIT-like pathogenic monoclonal antibody KKO.23,24 Heparin approximates PF4 tetramers as assessed by atomic force microscopy25 and in doing so may expose this region or other neoepitopes recognized by pathogenic, but not by nonpathogenic antibodies, or reorganization may promote antibody avidity.
To begin to understand the structural basis for the binding of pathogenic antibodies, we compared the effect of heparin on the binding of KKO and platelet-activating anti-PF4/heparin antibodies and anti-PF4/heparin antibodies not associated with platelet activation from patients suspected of HIT. The data presented here suggest there is a fundamental difference between the binding properties of pathogenic and nonpathogenic anti-PF4 antibodies that is not evident by ELISA, and they suggest potential new approaches toward identifying clinically relevant HIT antibodies in the future.
Methods
Generation of human PF4 in Schnieder 2 insect cells
cDNAs encoding human wild-type (WT) PF4 and PF4K50E were cloned into the plasmid pMT/BiP/V5-His (Invitrogen) for expression in Drosophila Expression System (Invitrogen). Cloning was performed using BglII and AgeI cloning sites. A hexanucleotide encoding the BglII site was then eliminated by site-directed mutagenesis so that the expressed protein contained full-length WT PF4 or PF4K50E with an identical sequence as their counterparts expressed in Escherichia coli.26 PF4 expression was induced by adding copper sulfate (0.5mM), and the protein was collected in serum-free medium Insect-Xpress (Lonza Walkersville) for 3 to 5 days; sodium azide (0.02% final concentration) and EDTA (2.5mM final concentration) were added, and the medium was filtered through Express Plus 0.22-mm filter (Millipore). PF4 was purified from the media on a heparin HiTrap column (GE Healthcare) on an ATKA Prime FPLC (GE Healthcare) at 4°C using a 10mM Tris and 1mM EDTA, pH 8, buffer system. Medium was loaded in buffer containing 0.5M NaCl and PF4 eluted at 1.8M NaCl using a linear gradient. Fractions containing purified PF4 detected by silver staining of 12% polyacrylamide gels (SDS-PAGE) were pooled and then concentrated, and buffer was exchanged into 50mM HEPES and 0.5M NaCl, pH ∼ 7.2, using an Amicon Ultra filter (3000 molecular weight cut-off; Millipore). Protein was quantified using a bicinchoninic acid assay (Thermo Fisher Scientific). PF4K50E was purified in the same way as WT PF4, with several modifications: the buffer system used was 50mM MES, 1mM EDTA, pH 6.5; medium was loaded in buffer containing 0.3M NaCl, and the protein was eluted at 1.3M NaCl using a linear gradient.
Anti–human PF4 monoclonal antibodies to PF4
KKO and RTO hybridoma cells were generated and characterized as described previously.27 In brief, KKO and RTO are IgG2bκ monoclonal anti–human PF4 antibodies generated concurrently in mice injected with complexes of human PF4 and unfractionated heparin at an equimolar ratio. The IgG fractions were purified from conditioned PFHM-II media (Invitrogen) using protein A agarose (Invitrogen) as recommended by the manufacturer. IgG purity was demonstrated by SDS-PAGE on NuPAGE 4%-12% Bis-Tris Gel (Invitrogen).
Effect of KKO and RTO on platelet counts in vivo
FcγRIIA/hPF4+ mice, generated and characterized as described previously,19,21 were injected intraperitoneally with KKO (10 or 20 mg/kg) or RTO (10 or 100 mg/kg), and the platelet count was measured daily over the next 4 days. All studies involving animal were approved by the institutional animal care committee at the Children's Hospital of Philadelphia.
Binding of KKO and RTO to PF4: ELISA
Immulon 4 HBX plates (Thermo Fisher Scientific) were coated overnight at room temperature (RT) with PF4 or PF4K50E (50 μL/well; 5 μg/mL)27 in PBS, in the absence or presence of 0.1 U/mL heparin (Hospira). For stoichiometric calculations, we used previously published estimates of specific activity of 140 U/mg16,28 and a mean molecular mass of 15 kDa. The plates were washed 4 times with 180 μL of PBS, and nonreactive sites were blocked with 1% BSA in PBS (150 μL/well) for 1 hour at RT. Serial dilutions of KKO or RTO IgGs were added in 1% BSA/PBS (100 μL/well) for 1 hour at RT. The plates were washed 6 times with 180 μL PBS and 0.1% Tween 20. HRP-conjugated goat anti–mouse IgG-Fc (Bethyl Laboratories) diluted 1:3000 in 1% BSA-PBS was added (100 μL/well) for 1 hour at RT and washed 6 times with 180 μL PBS and 0.1% Tween 20. HRP substrate ABTS (Roche Diagnostics) dissolved in ABTS buffer as recommended by the manufacturer was added (100 μL/well) at RT. Color development over time was read on a SpectraMax 340 microplate reader (Molecular Devices) at 405 nm and 490 nm.
Inhibition of KKO and RTO binding: ELISA
Plates were coated with PF4 complexed to heparin (PF4:H) and blocked with 1% BSA as described in the preceding section. Human plasma (1:50 dilution) was added in 1% BSA-PBS (50 μL/well) for 30 minutes at 37°C, followed by KKO or RTO (0.02 μg/mL) ± plasma (50 μL/well) for 5 minutes at 37°C. Plates were washed 5 times with 180 μL of PBS and 0.1% Tween 20. HRP-conjugated goat anti–mouse IgG-Fc (Jackson ImmunoResearch Laboratories) diluted 1:5000 in 1% BSA-PBS was added (50 μL/well) for 30 minutes at 37°C and washed 5 times with 180 μL of PBS and0.1% Tween 20. The assay was performed, and color development over time was measured as described in the preceeding section.
Binding of human HIT antibodies to PF4: ELISA
Citrated plasma samples from 15 patients referred to the Coagulation Laboratory at the Hospital of University of Pennsylvania for evaluation of HIT were selected for analysis based on serologic profile. All patients experienced a greater than 30% fall in platelet count in appropriate temporal relationship to heparin exposure to raise concern for HIT. Samples from 8 patients produced a positive polyspecific ELISA result (Gen-Probe GTI Diagnostics) and a positive in-house serotonin release assay (SRA) result; 7 patients had a positive ELISA and a negative SRA. The mean optical density result in both groups was greater than 1.0 optical density unit (strong positive). ELISAs were performed as described for monoclonal antibodies using wells precoated with PF4 ± heparin. Plasma was tested at 1:50 dilution. The investigator performing these assays was blinded to clinical history and serologic profile. Studies were performed in accordance with approval of the Institutional Review Board at the University of Pennsylvania.
Oligomerization of PF4 assessed by autoradiography
Radiolabeling of PF4 was performed with Na125I (PerkinElmer Life and Analytical Sciences) with immobilized chloramine T (Iodo-Beads; Thermo Fisher Scientific) according to the manufacturer's instructions. Equimolar solutions of 125I-labeled PF416 (10 μg/mL) and KKO or RTO (46.5 μg/mL) were incubated for 30 minutes at RT in a volume of 30 μL of PBS. The cross-linker bis-sulfosuccinimidyl suberate (Thermo Fisher Scientific; final concentration 0.2mM) or PBS was added for an additional 30 minutes at RT. Oligomerization of PF4 was examined by SDS-PAGE (3%-8% Tris-acetate gradient gel). The relative amounts of PF4 migrating as tetramers or at higher molecular masses was quantified by densitometry using the Gel Logic 100 imaging system with Kodak molecular imaging software (Version 4.5.1; Carestream Health).
Binding of KKO and RTO to PF4: optical trap-based force spectroscopy
To measure the binding of KKO and RTO to PF4 at the single-molecule level while minimizing effects of avidity and other auxiliary intermolecular interactions, we used optical trap-based force spectroscopy that we developed (supplemental Methods, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).29 In optical trap-based force spectroscopy, the tension produced on the receptor-attached ligand-coated latex bead causes a beam deflection that is sensed by a photodetector and displayed as a voltage signal, reflecting the strength of ligand-receptor binding (supplemental Figures 1-2). Because of the stochastic nature and variability, rupture forces after contact are displayed as force histograms. In these experiments, a KKO- or RTO-coated 2-μm latex bead was trapped by the focused laser light and brought to a distance of a few micrometers from a PF4-coated 5-μm spherical silica pedestal (supplemental Figure 1). After oscillating the bead at 10 Hz with a 0.8-μm peak-to-peak amplitude (2000 pN/s loading rate), the bead was brought into intermittent contact with the pedestal by micromanipulation using a keyboard-controlled piezoelectric stage (supplemental Figure 2). Rupture force signals after repeated contacts between the pedestal and the bead were collected for periods of up to 1 minute and were displayed as normalized force histograms for each experimental condition.
To ensure the comparability of the binding probability determined for KKO versus RTO with PF4, we used identical coating protocols for both antibodies, including the same initial concentration in the binding mixture with the same freshly activated beads under identical experimental conditions. From many previous experiments with other proteins,30-34 we know that the immobilization protocol is robust and highly reproducible in terms of surface density and reactivity of proteins. To maximize single-molecule interactions while decreasing the likelihood of multiple interactions, the surface densities of reacting proteins were deliberately decreased so that the fraction of specific interactions between antibody and PF4 was ∼ 10% of bead-pedestal contacts or less (see supplemental Methods for details). Because only a small percentage of contact-detachment cycles resulted in effective antigen-antibody binding and unbinding, data from at least 10 experiments, representing 103 to 104 individual measurements were combined. Individual forces measured during each contact-detachment cycle were collected into 5-pN-wide force ranges (bins). The number of events in each bin was plotted against the average force for that bin after normalizing for the total number of interaction cycles. The percentage of events in a particular bin represents the probability density of rupture events at that tension. Importantly, to minimize potential weaker signals because of noncovalent PF4-PF4 interactions (revealed in control experiments as a noisy background), the surface-bound WT PF4 tetramers were covalently cross-linked with 0.5% glutaraldehyde before interaction with an antibody-coated bead. Glutaraldehyde was chosen for these initial studies because it generated homogeneous, irreversible complexes (as opposed to heparin) that preserved binding of both mouse monoclonal antibodies and human antibodies to PF4 (data not shown). The efficacy of cross-linking was confirmed as described in the preceding section using SDS-PAGE.16
Results
Identification of pathogenic and nonpathogenic antibody
Our goal was to begin to understand the molecular basis of the difference between anti-PF4 antibodies associated with platelet activation, a central feature of HIT, and those that are not. To do so, we took advantage of 2 extensively characterized murine monoclonal anti–human PF4 IgG2bκ antibodies, designated KKO and RTO.27 Consistent with our previous work,18,19 injection of KKO into FcγRIIA/hPF4+-expressing transgenic mice caused a transient reduction in the platelet count by ∼ 70%, whereas the same amount of RTO had no effect (Figure 1). To take into account unknown pharmacokinetic interactions that could affect antibody availability, a 10-fold higher dose of RTO was injected. Again, RTO did not cause a significant fall in the platelet count.
Effect of KKO and RTO on platelet counts in vivo. Platelet counts after intraperitoneal injection of KKO or RTO in the FcγRIIA/hPF4+ mice are shown. Platelet counts were measured before (basal = time 0) and 4, 24, 48, and 96 hours after antibody injection. Data are mean ± 1 SEM of 5 animals for each condition.
Effect of KKO and RTO on platelet counts in vivo. Platelet counts after intraperitoneal injection of KKO or RTO in the FcγRIIA/hPF4+ mice are shown. Platelet counts were measured before (basal = time 0) and 4, 24, 48, and 96 hours after antibody injection. Data are mean ± 1 SEM of 5 animals for each condition.
Comparison of KKO and RTO binding by ELISA
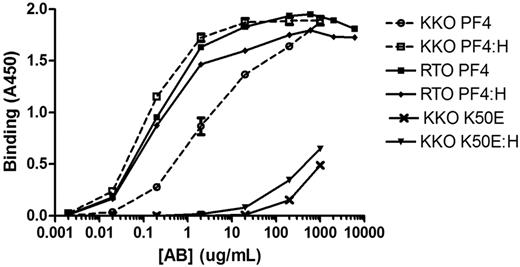
We next measured the binding properties of these 2 antibodies to PF4 and PF4:H by ELISA (Figure 2). Although KKO and RTO completely inhibited binding of their biotinylated counterparts, neither inhibited the binding of the other (data not shown), suggesting they recognize distinct binding sites. RTO bound more tightly to PF4 than KKO in the absence of heparin (EC50 = 0.19 ± 0.05 and 6.13 ± 0.01 μg/mL, respectively). Binding of RTO was unaffected by heparin (EC50 = 0.19 ± 0.04). In contrast, binding of KKO to PF4:H was 32-fold higher than to PF4 alone (EC50 = 0.19 ± 0.01 and 6.13 ± 0.01 μg/mL, respectively) and comparable with binding of RTO to PF4:H. Of note, maximal binding of both antibodies to PF4 was virtually identical in the presence of heparin under conditions where secondary antibody and substrate were not limiting.
Binding of KKO and RTO measured by ELISA. PF4 alone, PF4:H, PF4K50E alone, and PF4K50E:H. Data are the mean ± SEM of at least 3 independent experiments performed in triplicate.
Binding of KKO and RTO measured by ELISA. PF4 alone, PF4:H, PF4K50E alone, and PF4K50E:H. Data are the mean ± SEM of at least 3 independent experiments performed in triplicate.
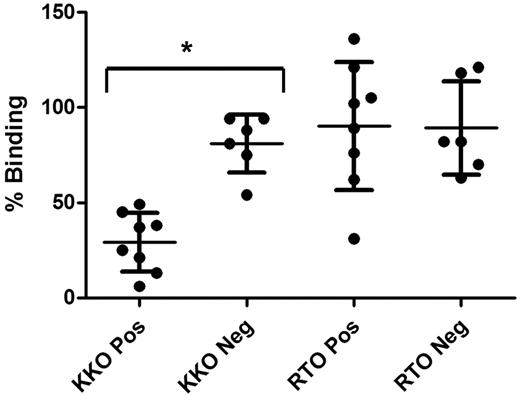
Relationship between binding of monoclonal and human anti-PF4 antibodies
Based on these results, we asked whether anti-PF4 antibodies that activate platelets (positive SRA) from patients suspected of HIT compete for KKO binding to PF4:heparin, whereas anti-PF4 antibodies that fail to activate platelets do not. Plasma from 8 ELISA+/SRA+ patients suspected of HIT inhibited KKO binding by a mean of 80% compared with 30% by ELISA+/SRA− samples (P < .0001), whereas no discrimination was evident based on inhibition of RTO binding (90% vs 89%, P = .96; Figure 3). These data are consistent with the concept that platelet-activating antibodies from patients suspected of having HIT recognize an epitope that overlaps with KKO that is less prevalent in plasma from patients without platelet-activating antibodies.
Inhibition of KKO and RTO by human HIT antibodies. Scattergram showing inhibition of model antibody (KKO or RTO) binding to PF4:H by human plasma containing anti-PF4 antibodies (ELISA positive). Pos denotes competition with antibodies from SRA-positive patients, and Neg denotes competition with antibodies from SRA-negative patients. Means ± SDs are shown (*P < .0001).
Inhibition of KKO and RTO by human HIT antibodies. Scattergram showing inhibition of model antibody (KKO or RTO) binding to PF4:H by human plasma containing anti-PF4 antibodies (ELISA positive). Pos denotes competition with antibodies from SRA-positive patients, and Neg denotes competition with antibodies from SRA-negative patients. Means ± SDs are shown (*P < .0001).
Dynamic bimolecular interactions between surface-bound antibody and PF4
We next tested the hypothesis that the discordance between measurements of antibody binding by ELISA and their effect in vivo is because of the complications of avidity and other intermolecular interactions that are intrinsic to bulk equilibrium assays such as ELISAs. To explore the possibility that KKO and RTO bind PF4 differently at the single-molecule level, we measured the binding interactions of these antibodies with PF4 using an original biophysical methodology named optical trap-based force spectroscopy (supplemental Methods).29,34 This approach enabled us to measure the probability and strength of binding among bimolecular partners in a nonequilibrium state over a wide range of rupture forces capable of dissociating noncovalent single-molecule protein-protein complexes.35 Through a series of control experiments with tetrameric WT PF4 and either KKO or RTO, we identified a set of lower binding strength interactions arising from PF4-PF4 bonds (data not shown), which partially overlapped with antibody-PF4 interactions. To study antibody-PF4 binding specifically, we prevented rupture of PF4-PF4 bonds by covalently cross-linking the PF4 tetramers with glutaraldehyde. The specificity of rupture forces generated by the surface-bound cross-linked PF4 and surface attached KKO or RTO was confirmed by competitive inhibition experiments in the presence of free antibodies (supplemental Figure 3) or PF4 (data not shown). The force histogram revealed that KKO-PF4 interactions occurred with about an 8-fold higher probability than RTO-PF4 interactions at the same surface densities, reflecting a much higher reactivity of KKO to PF4 (Figure 4A inset). KKO-PF4 interactions were also slightly stronger, as reflected by the position of the peak at higher rupture forces (Figure 4A). In contrast to the WT PF4, KKO and RTO showed lower and similar binding probabilities to glutaraldehyde-treated PF4K50E, which forms few tetramers or higher ordered complexes (Figure 4B).
Rupture force histograms for KKO and RTO binding to PF4. (A) Frequency of events in each 5-pN bin was plotted against the average force for that bin after normalizing for the total number of interaction cycles. PF4 tetramers were attached covalently to pedestals and cross-linked with glutaraldehyde, and Ab was covalently attached to latex beads in the absence of heparin. Each curve represents ∼ 10 000 contact cycles of bead to pedestal. The probability of KKO binding to PF4 is much greater than for RTO, and the binding strength is slightly higher. Inset shows the cumulative binding probability for KKO and RTO. (B) Similar analysis of KKO and RTO interactions with the glutaraldehyde-treated PF4K50E mutant that does not form tetramers. In this case, the probability of binding of KKO is lower and comparable with that of RTO.
Rupture force histograms for KKO and RTO binding to PF4. (A) Frequency of events in each 5-pN bin was plotted against the average force for that bin after normalizing for the total number of interaction cycles. PF4 tetramers were attached covalently to pedestals and cross-linked with glutaraldehyde, and Ab was covalently attached to latex beads in the absence of heparin. Each curve represents ∼ 10 000 contact cycles of bead to pedestal. The probability of KKO binding to PF4 is much greater than for RTO, and the binding strength is slightly higher. Inset shows the cumulative binding probability for KKO and RTO. (B) Similar analysis of KKO and RTO interactions with the glutaraldehyde-treated PF4K50E mutant that does not form tetramers. In this case, the probability of binding of KKO is lower and comparable with that of RTO.
Role of PF4 oligomerization in antibody binding
In view of these differences, we next examined the impact of these 2 antibodies on oligomerization of PF4, which is induced by heparin. PF4K50E has a single amino-acid mutation at the interface between dimer surfaces.16 This sharply curtails tetramer formation that we have shown is a prerequisite for heparin-induced oligomerization and binding of HIT antibodies.16 Binding of both KKO and RTO to PF4K50E was weak and insensitive to heparin, confirming the importance of PF4 tetramerization (Figure 4B). We then hypothesized that KKO, like heparin, may approximate PF4 tetramers, increasing its avidity in the ELISA and in vivo, whereas RTO does not. To explore this possibility, we examined whether KKO, RTO, or both clustered PF4. Incubation of PF4 with KKO, but not RTO, generated larger molecular mass structures (Figure 5). Because both antibodies bind PF4 in the presence of heparin with almost identical EC50 values and maximal capacity by ELISA, this suggests that KKO, unlike RTO, promotes PF4 clustering of complexes (120-200 kDa) like heparin, although to a lesser extent than heparin alone (> 700 kDa).16 Because the linking arm of bis-sulfosuccinimidyl suberate used in these experiments is only 11.4 Å and cross-links primary amines on the side chains of lysine residues and amino termini, these data may demonstrate only a subset of such complexes that are formed.
Autoradiogram of 125I-PF4 after incubation with KKO or RTO. Molecular mass markers are to the left of each panel correspond to 55, 71, 117, and 268 kDa. Lanes 1 and 4 show PF4 complexes with KKO (1) or RTO (4) that were subsequently cross-linked with bis-sulfosuccinimidyl suberate. Lanes 2 and 5 show PF4 cross-linked with bis-sulfosuccinimidyl suberate, and lanes 3 and 6 show PF4 alone (uncross-linked). Higher molecular mass PF4 complexes in the presence of the KKO comprise ∼ 60% of the total PF4 tetramers versus ∼ 2% with RTO. Data are representative of 3 such experiments.
Autoradiogram of 125I-PF4 after incubation with KKO or RTO. Molecular mass markers are to the left of each panel correspond to 55, 71, 117, and 268 kDa. Lanes 1 and 4 show PF4 complexes with KKO (1) or RTO (4) that were subsequently cross-linked with bis-sulfosuccinimidyl suberate. Lanes 2 and 5 show PF4 cross-linked with bis-sulfosuccinimidyl suberate, and lanes 3 and 6 show PF4 alone (uncross-linked). Higher molecular mass PF4 complexes in the presence of the KKO comprise ∼ 60% of the total PF4 tetramers versus ∼ 2% with RTO. Data are representative of 3 such experiments.
Discussion
The initial diagnosis of HIT relies on clinical impression that may or may not receive support from subsequent laboratory evaluation. In most settings, serologic assessment of HIT is confined to measurement of anti-PF4/heparin antibodies by ELISA, because more specific assays based on platelet activation are not available in real-time. HIT is uncommon even in patients receiving heparin who develop thrombocytopenia and the ELISAs most commonly used are better suited to exclude a diagnosis of HIT than to affirm it, especially in complex medical settings where the need for a test with a high positive predictive value is most pressing.10,36 High titers of IgG antibodies correlate with platelet activation and probability of disease in experienced hands,5,11,12 but the outcome of predicating clinical decisions on laboratory outcomes has not been formally tested in general practice.
The finding that the prevalence of anti-PF4/heparin antibodies vastly exceeds clinical disease in settings such as cardiopulmonary bypass surgery, among others, raises the question of why only a subset of antibodies detected by ELISA is associated with the risk of developing thrombocytopenia and thrombosis. We hypothesize that part of the explanation involves heterogeneity in the distribution of PF4 bound to heparin or heparin-like compounds15,16 in ELISA wells compared with ULCs formed in solution or on cell surfaces. It is likely that ULC formation in the ELISA plate may be partly constrained (by steric effects, electrostatic effects, or both), limiting the formation (or accessibility) of critical binding epitopes needed to optimize binding of HIT antibodies. In addition, the ELISA format yields a measurement of total antibody binding at equilibrium, which contrasts with the situation in vivo where the opportunity for antibody-antigen interactions with cell surface GAGs are probably brief and subject to hemodilution and disruption by flow.
To begin to address these possibilities, we compared the binding of 2 isotype-matched monoclonal IgG anti–human PF4 antibodies: KKO that causes thrombocytopenia (and thrombosis18 ) in vivo, and RTO that does not. The epitopes recognized by the antibodies differed based on cross-competition experiments and greater inhibition of KKO by SRA-positive but not SRA-negative human plasma, in contrast to RTO for which no specific pattern of inhibition by human antibody was seen. Importantly both antibodies bound comparably to PF4:H-coated wells as measured using a standard ELISA used clinically but adapted to measure mouse antibody, eliminating the question of titer or isotype from consideration. Of note, when present at high concentrations, KKO binds to immobilized PF4. We attribute this to a low level of oligomerization on the well surface, although additional experimentation is needed to state this with certainty.
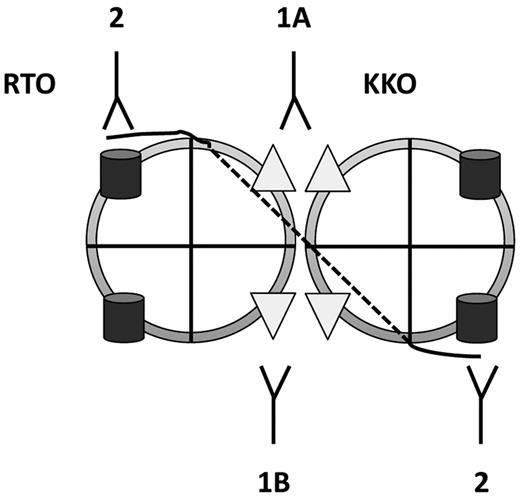
These 2 antibodies differed in several important characteristics. KKO induced oligomerization of PF4, as does heparin, whereas RTO did not, and heparin enhanced the avidity of KKO but had no effect on RTO. We hypothesize that the binding avidity of KKO, and possibly HIT antibodies with which it competes, is enhanced when heparin or cellular GAGs promote organization of PF4 tetramers into higher ordered complexes in vitro or in vivo. These complexes are in turn stabilized by KKO (Figure 6). In contrast, high titers of nonpathogenic anti-PF4 antibodies may show comparable behavior at equilibrium, but their binding is not enhanced by heparin-induced oligomerization and they bind to sites that do not reinforce oligomer stability (Figure 6).
Schematic of pathogenic versus nonpathogenic antibody binding. Simplest model showing distinction between effects of heparin on binding of pathogenic (KKO) and nonpathogenic (RTO) anti-PF4 antibodies. Heparin (black line) binds to a circumferential band of cationic residues on the surface of each PF4 tetramer; the interrupted line represents binding to the distal side of the tetramer. Heparin neutralizes cationic charge repulsion among PF4 tetramers forming oligomeric complexes (shown here as a dimer for simplicity), which approximates the binding sites for KKO. Epitope approximation increases the avidity of KKO through increased proximity to more than 1 binding site on PF4 (1A). Some KKO antibodies may bind to epitopes on neighboring tetramers stabilizing ULCs induced by heparin (1B). In contrast, heparin has no such effect or may partially inhibit exposure of the epitope recognized by RTO (2).
Schematic of pathogenic versus nonpathogenic antibody binding. Simplest model showing distinction between effects of heparin on binding of pathogenic (KKO) and nonpathogenic (RTO) anti-PF4 antibodies. Heparin (black line) binds to a circumferential band of cationic residues on the surface of each PF4 tetramer; the interrupted line represents binding to the distal side of the tetramer. Heparin neutralizes cationic charge repulsion among PF4 tetramers forming oligomeric complexes (shown here as a dimer for simplicity), which approximates the binding sites for KKO. Epitope approximation increases the avidity of KKO through increased proximity to more than 1 binding site on PF4 (1A). Some KKO antibodies may bind to epitopes on neighboring tetramers stabilizing ULCs induced by heparin (1B). In contrast, heparin has no such effect or may partially inhibit exposure of the epitope recognized by RTO (2).
In furtherance of this concept, measurement of antibody-PF4 binding at the single-molecule level (using rupture force spectroscopy) rather than in bulk (by ELISA) reveals that the probability of KKO binding to PF4 was ∼ 8-fold greater than RTO binding and that higher tensile forces, such as may occur with shear in vivo, were required to dissociate KKO. This increase was most apparent when PF4 was oligomerized and was not seen when a nonoligomerizing PF4 variant, recognized by both antibodies, was studied.
Although studying PF4-antibody interactions at the single-molecule level is somewhat artificial in terms of surface density, steric limitations because of surface confinement, and relative orientation, and may or may not reflect antibody behavior in vivo, this approach provides important information on the fundamental nature of these interactions that correlates with the in vivo activity of these antibodies that was not apparent by ELISA. In 2-dimensional kinetics, the binding probability at a given contact duration and surface densities of interacting molecules reflects the rate of association and is governed by the on-rate constant, whereas the peak of rupture forces (binding strength) depends on the height of the dissociation energy barrier and reflects the forced dissociation rate.37,38 Therefore, the data indicate that at least under 2-dimensional nonequilibrium conditions, KKO has higher affinity for PF4 tetramers than RTO irrespective of avidity and other effects of heparin- or antibody-induced, higher order polymerization of PF4. In combination with the ability of KKO to promote “super-oligomerization” of the PF4 tetramers, these data suggest an amplification reaction, in which KKO, unlike RTO, binds preferentially to PF4 tetramers (with or without heparin), further enhances their polymerization, and binding becomes more avid as the antigenic complexes grow in size (Figure 6). Whatever mechanisms are operative, we hypothesize that the single-molecule rupture force measurements, which summarize thousands of ongoing individual antigen-antibody interactions, simulate more closely the transient interactions that vascular and hematopoietic cells are subjected to in the circulation because of hemodilution and shear forces, which might affect antibody binding in ways not reflected in the ELISA platform.
In summary, our study affirms and extends results described previously using atomic force microscopy25 by showing the importance of epitope specificity, probability, and strength of antibody binding in real time and the differences in the effect of approximation of epitopes by heparin on the binding of platelet-activating versus nonactivating antibodies. Together, these results begin to reveal potentially important biologic differences in the behavior of anti-PF4 antibodies not reflected in ELISAs or similar in vitro detection systems. They suggest that epitope specificity may be an important parameter in assessing clinical risk, in part because oligomerization of the antigen by heparin or GAGs affects antibody binding and its downstream consequences. In turn, cell-activating antibodies may stabilize oligomer formation. Based on these principles, it may be possible to develop assays that more closely simulate the in vivo setting and provide greater discrimination between the binding characteristics of pathogenic antibodies and those less likely to cause HIT, thereby improving clinical diagnosis and management.
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by the National Institutes of Health grants HL078726, HL078726-S1 (B.S.S.), HL099973, HL090774 (J.W.), and HL084006 (D.B.C., M.P., L.R.).
National Institutes of Health
Authorship
Contribution: B.S.S., R.I.L., S.V.Y., L.R., A.H.R., J.W.W., and D.B.C. designed experiments; R.I.L., S.V.Y., L.R., and J.L.H. performed experiments; B.S.S., R.I.L., S.V.Y., L.R., J.L.H., A.H.R., G.M.A., M.P., A.C., J.W.W., and D.B.C. analyzed and interpreted data; and B.S.S., R.I.L., S.V.Y., L.R., J.L.H., A.H.R., G.M.A., M.P., A.C., J.W.W., and D.B.C. wrote and edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bruce Sachais, Department of Pathology and Laboratory Medicine, Division of Transfusion Medicine and Therapeutic Pathology, University of Pennsylvania, 605A Stellar-Chance Labs, 422 Curie Blvd, Philadelphia, PA 19104; e-mail: sachais@mail.med.upenn.edu.
References
Author notes
B.S.S. and R.I.L. contributed equally to this work.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal