Abstract
Hematopoietic stem cells (HSCs) interact with osteoblastic, stromal, and vascular components of the BM hematopoietic microenvironment (HM) that are required for the maintenance of long-term self-renewal in vivo. Osteoblasts have been reported to be a critical cell type making up the HSC niche in vivo. Rac1 GTPase has been implicated in adhesion, spreading, and differentiation of osteoblast cell lines and is critical for HSC engraftment and retention. Recent data suggest a differential role of GTPases in endosteal/osteoblastic versus perivascular niche function. However, whether Rac signaling pathways are also necessary in the cell-extrinsic control of HSC function within the HM has not been examined. In the present study, genetic and inducible models of Rac deletion were used to demonstrate that Rac depletion causes impaired proliferation and induction of apoptosis in the OP9 cell line and in primary BM stromal cells. Deletion of Rac proteins caused reduced trabecular and cortical long bone growth in vivo. Surprisingly, HSC function and maintenance of hematopoiesis in vivo was preserved despite these substantial cell-extrinsic changes. These data have implications for therapeutic strategies to target Rac signaling in HSC mobilization and in the treatment of leukemia and provide clarification to our evolving concepts of HSC-HM interactions.
Introduction
Hematopoietic stem cells (HSCs) give rise to all lineages of mature blood cells and maintain hematopoiesis in vivo through a balance of self-renewal and differentiation. To maintain this balance, HSCs are supported within a complex milieu known as the hematopoietic microenvironment (HM) or HSC niche.1,2 This HM includes cellular components (osteoblastic cells,3,4 perivascular cells,5 and sympathetic neurons6 ), bone mineral matrix,7 and ionic gradients.8 Trabecular bone appears to be particularly important in HSC biology3,9,10 ; however, there is ongoing controversy regarding the existence or identity of one predominant cell type that is necessary and sufficient for HSC survival in vivo. Apparently conflicting results have identified osteoblastic cells,3,11-13 perivascular cells,5 and a nestin-positive common precursor cell type with the ability to differentiate into either lineage as key cells within the HSC niche. Irrespective of this controversy, it has been firmly established that key ligand/receptor signaling interactions are responsible for HSC engraftment and mobilization from the HM. These include the interactions between CXCL12 (also known as SDF1) and CXCR4,14,15 between the cKit receptor and SCF,16 and between fibronectin and β1-integrins.17,18
The Rac family of Rho GTPases (encompassing Rac1, Rac2, and Rac3) integrates a critical downstream common pathway of the aforementioned signaling pathways. Through this, Rac proteins regulate the homing, engraftment, mobilization, and survival of HSCs in vivo (for a recent, comprehensive review, see Cancelas and Williams19 ). Deletion of Rac1 in HSCs causes failed HSC engraftment and reduced HSC proliferation in vivo.20 Deletion of Rac2 alone has modest but significant effects on HSC mobilization and engraftment21 and leads to reduced HSC survival through impaired growth factor signaling and increased apoptosis.20 Combined deletion of Rac1 and Rac2 causes a massive egress of HSCs from the HM and profoundly impaired engraftment.20,22 Vav1, a hematopoietic-specific guanine exchange factor for Rac, differentially regulates endosteal/osteoblast and perivascular retention and subsequent engraftment.23 Moreover, Rac1 and Rac2 were shown to be important for the survival of leukemia stem cells in a murine model of chronic myeloid leukemia.24 These findings were reinforced by the development and preclinical testing of NSC23766, a small-molecule inhibitor of Rac signaling that has substantial in vivo effects including HSC mobilization22 and antileukemic efficacy.24 Whereas Rac3 is widely expressed with high levels of expression in the CNS25 and Rac3-deficient mice show no obvious hematopoietic phenotype, we have previously shown functional redundancy of Rac3 in leukemic cells expressing p210-BCR-ABL.24
Interestingly, despite the breadth of knowledge regarding the cell-intrinsic requirements for Rac signaling in HSC function, little is known about the function of Rac within HM components and therefore about cell-extrinsic Rac signaling within the HM. Data from in vitro experiments would support the role of Rac signaling within the HM. For example, Rac signaling is important for fibroblast survival26 and the inhibition of Rac signaling causes impaired in vitro osteoblastic migration.27 Rac1 has been shown to be critical in osteoblastic cell line adhesion, spreading, and proliferation,28 retinoblastoma-induced adherens junction formation in osteoblasts,29 and inhibition of mesenchymal stem cell (MSC) differentiation into chondrocytes.30 Finally, Rac1 activity is critical for β-catenin translocation into the nucleus, and thus Wnt signaling in adherent cells.31 Therefore, there are significant in vitro data suggesting that Rac signaling may be critical for osteoblast cell function. By understanding the specific cellular context and requirements of Rac signaling that control HSC function, a more precise definition and understanding of the HM may be obtained. In addition, a complete understanding of Rac within the HM is of critical importance to understanding the effects of Rac inhibitors in HSC mobilization and for therapeutic antileukemia trials in the future.
In the present study, we used a series of genetic and inducible models of Rac deletion to specifically delete Rac within BM stromal cells and osteoblastic cells. Using these models, we sought to examine the effects of Rac signaling in BM stromal cells. Finally, we examined the cell-extrinsic effects of Rac signaling on HSC function in vivo.
Methods
Cell culture
The murine calvarium stromal cell line OP9 was obtained through ATCC and maintained in αMEM supplemented with penicillin/streptomycin, 20% FCS, and 1% L-glutamine. Primary MSC cultures were obtained by harvesting femurs, pelvises, and vertebrae from 8- to 12-week-old mice and homogenized with a sterile mortar and pestle. The resulting supernatant was treated with RBC lysis buffer (BD Pharmlyse) and then resuspended in αMEM supplemented with 20% FCS (α MEM/20%). Adherent cells were enriched by washing and passage on tissue culture–treated flasks. Osteoblastic differentiation was performed by adding β-glycerol phosphate (2.16 mg/mL), dexamethasone (10nM), and ascorbic acid (0.05 mg/mL) to the culture medium for 5-14 days. Colony formation assays were assessed by plating 2000-5000 cells per well in a 6-well plate and culturing in osteoblast differentiation medium for 14 days. CFU-F were stained with methylene blue (Sigma-Aldrich). Alkaline phosphatase staining was performed with NBT/BCIP reagent according to the manufacturer's instructions (Sigma-Aldrich). For Alizarin Red S staining (Sigma-Aldrich), adherent cells were washed with PBS, fixed with 4% formalin, washed twice with deionized water, and stained with 2.0% Alizarin Red in water at pH 4.0 for 3 minutes. Cells were subsequently washed with water 3 times and visualized. Images were obtained with a Nikon Eclipse TS100 microscope and a Nikon Digital Sight System camera.
Lentivirus shRNA knockdown and CreER retrovirus
shRNAs targeting Rac1 were obtained in the pLKO.1 backbone (Open Biosystems) and validated to determine effective gene silencing (coded 88 and 92). OP9 cells were infected with shRNAs targeting Rac1 or scrambled (nontargeting) control vector and selected for 5 days using puromycin (2 μg/mL). 4-Hydroxytamoxifen (4OHT)–inducible Cre expression was obtained by infected cells with the MSCV-CreER-puro retrovirus (a gift from Dr D. Kalaitzidis, Harvard Medical School) and Cre expression was induced with 200-400nM 4OHT (Sigma-Aldrich).
Genetic mouse models
Rac1fl/fl, Rac2−/−, and Rac3−/− mice have been described previously.22,24,32 Osterix-Cre:GFP mice were obtained from Dr D. Scadden (Harvard Medical School) and have also been described previously.33,34 Mouse blood parameters were measured by retro-orbital blood sampling and a Hemavet 950 (Drew Scientific).
Flow cytometry assays
BM was harvested from the long bones of 8- to 10-week-old mice and flushed with sterile PBS containing 2% FCS, treated with RBC lysis buffer (BD Pharmlyse), and resuspended in PBS/2% FCS. For osteoblastic progenitor cell assays, bones were crushed in a mortar and pestle and filtered through a 70-μm strainer. The bone chips were retained and treated for 90 minutes with collagenase solution (StemCell Technologies) while vortexing regularly. The solution was then washed with PBS/2% FCS and passed through a 70-μm strainer to obtain the digested cells, which were then stained with secondary Abs. Annexin V staining and bromodeoxyuridine incorporation (both BD Biosciences) were performed according to the manufacturer's instructions. For stem cell enumeration, samples were incubated in the presence of a lineage cocktail containing biotinylated Abs directed against CD3 (clone 145-2C11), CD5 (53-7.3), Ter119 (Ter119), B220 (RA3-6B2), Gr-1 (RB6-8C5), and Mac1 (M1/70). Samples were washed and stained with streptavidin-APC/Cy7 and directly conjugated Abs against CD34 (Ram34), Sca-1 (D7), cKit (2B8), CD150 (TC15-12F12.2), CD48 (HM48-1), and Flk2 (BV10A4H2). CD45.2 (104) and CD45.1 (A20) Abs were used for chimerism studies. Mac1 (M1/70), B220 (RA3-6B2), and TCR (H57-597) Abs were used for lineage determination. The gating strategy is illustrated in Figure 4E. For osteoblastic assays, Abs to ALCAM (3A6) and biotinylated Abs directed against CD45 (30-F11) and CD31 (390) were also used (all eBioscience). A FACSAria was used for cell sorting and a FACS LSR II flow cytometer for lineage determination (both BD Biosciences).
Micro-CT
For microcomputed tomography (micro-CT), a high-resolution desktop microtomographic imaging system (μCT40; Scanco Medical) was used to assess trabecular bone microarchitecture in the distal femoral metaphysis, and cortical bone morphology was assessed at the femoral midshaft following recommended guidelines.35 Scans were acquired using a 12-μm3 isotropic voxel size, 70 kVP, and 114 mAs, and were subjected to Gaussian filtration and segmentation. For the distal femur, transverse CT slices were evaluated in a region that's location and size was based on the average femur length for each sample group. The region of evaluation must vary based on femur length to consistently analyze the same anatomical region of bone. Based on the average femur lengths by group, a region starting 180 μm proximal to the growth plate and extending 1440 μm proximally was used for the wild-type (WT), OsxCreWT, and Rac1fl/flRac2−/−Rac3−/− groups, whereas a region starting 120 μm proximal to the growth plate and extending 1200 μm proximally was used for the OsxCreRac1fl/flRac2−/−Rac3−/− group. The trabecular bone region was identified by semimanually tracing the region of interest with the assistance of an auto-thresholding software algorithm. Images were thresholded using an adaptive-iterative algorithm and morphometric variables were computed from the binarized images using direct, 3D techniques that do not rely on any prior assumptions about the underlying structure. For trabecular bone regions, the bone volume fraction (as a percentage), trabecular thickness (in micrometers), and trabecular number (per millimeter) were assessed. A single outlier biologic replicate (OsxCreRac1fl/flRac2−/−Rac3−/− group) was excluded from analysis because it was 3 standard deviations from the mean of that group. The exclusion of this value did not affect the statistical significance of WT versus OsxCreWT or Rac1fl/flRac2−/−Rac3−/− versus OsxCreRac1fl/flRac2−/−Rac3−/− comparisons.
To assess cortical bone parameters, 50 transverse μCT slices were obtained at the femoral mid-diaphysis using a 12-μm isotropic voxel size. Images were subjected to Gaussian filtration and segmented using a fixed threshold. The following variables were computed: total cross-sectional area (bone + medullary area; in square millimeters), cortical thickness (in micrometers), and polar moments of inertia (in mm4), which describes the shape/distribution of cortical bone (larger values indicate a higher torsional strength).
Immunohistochemistry
Hind limbs were fixed overnight in 10% phosphate buffered formalin and decalcified for 2 weeks in 14% EDTA, pH 7.2. Once decalcified, all specimens were processed for paraffin embedding using a Shandon Pathcenter Processor (Thermo Electron). Sections were deparaffinized, rehydrated, and immunohistochemistry was performed using the immunoperoxidase method with diaminobenzidine (DakoCytomation). Ag retrieval was performed using 0.37% Carezyme trypsin (Biocare Medical) for 10 minutes at room temperature. Sections were incubated for 60 minutes in serum block (10% FCS [Invitrogen] plus 10% normal goat serum [Vector Laboratories]), followed by incubation for 60 minutes with rabbit anti–mouse osteocalcin Ab (Alexis Biochemicals) or normal rabbit IgG (Santa Cruz Biotechnology) isotype control. All other incubations were for 30 minutes, including blocking for endogenous peroxidase using 3% H2O2, incubation with a goat anti–rabbit biotinylated F(ab′)2 secondary Ab (Santa Cruz Biotechnology), followed by HRP-conjugated streptavidin (Jackson ImmunoResearch Laboratories). All sections were counterstained using Mayer hematoxylin (Sigma-Aldrich) and mounted using permanent mounting medium (Thermo Fisher Scientific). Slides were viewed at a 20× magnification using a Nikon Eclipse 80i microscope with a Nikon D5-Ri1 camera and NIS Elements Version 2BR imaging software.
PCR and primers
For validation of excision, genomic DNA was obtained from FACS-purified cells and in vitro cultures (DNA Mini Kit; QIAGEN). PCR was performed using the following primers: Rac1fl/fl 5′-GATGCTTCTAGGGGTGAGCC-3′; Rac1−/− 5′-CAGAGCTCGAATCCAGAAACTAGTA-3′; and Rac1common 5′-TCCAATCTGTGCTGCCCATC-3′.
For RT-PCR reactions, RNA was isolated from FACS-purified cells (RNeasy Micro Kit; QIAGEN). Complementary DNA was synthesized (Taqman reagents; Applied Biosystems) and analyzed by PCR. The following primers were used: Rac1 (f) 5′-ATAGGCCCAGATTCACTGGTT-3′; (r) 5′-GAGACGGAGCTGTTGGTAAAA-3′; β-actin (f) 5′-GGCTGTATTCCCCTCCATCG-3′; and (r) 5′-CCAGTTGGTAACAATGCCATGT-3′.
In vivo transplantation assays
Cells were obtained as described in the flow cytometry assay section. For all transplantation assays, congenic recipient mice were irradiated with 11 Gy in split doses at least 3 hours apart. For noncompetitive transplantation assays, 2 × 106 cells per recipient were injected. For competitive transplantation assays, 1 × 106 donor cells (CD45.2) were mixed with 1 × 106 competitor (CD45.1, CD45.2 double-positive) and injected into congenic, CD45.1-expressing recipient mice. For chimerism studies, retro-orbital sampling was used to obtain blood samples at 4 weekly intervals after transplantation. FACS analysis was used to determine chimerism.
Results
Rac1 depletion induces apoptosis and impairs proliferation in OP9 MSC lines
The OP9 cell line was used to determine whether Rac signaling influenced the growth of BM MSCs. OP9 cells have been demonstrated previously to possess adipocytic, chondrogenic, and osteogenic potential, identifying these cells as a bona fide MSC line.36 Rac1 depletion was induced by lentivirus infection with shRNA targeting Rac1 (sh88 and sh92) or nontargeting scrambled (SCR) controls. Efficient gene silencing with sh88 and sh92 was demonstrated by Western blot analysis for Rac1 protein compared with SCR control (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Rac1 knockdown induced morphologic changes including cytoplasmic retraction and cytoskeletal elongation (Figure 1A-B). Rac1 knockdown resulted in impaired growth, and apoptosis and proliferation assays were performed to determine the mechanism underlying this observation. Rac1 depletion induced apoptosis compared with SCR controls (Figure 1C). Furthermore, Rac1 depletion impaired bromodeoxyuridine incorporation, demonstrating a reduction in actively cycling cells (Figure 1D-F). These data demonstrate that Rac1 is essential for the survival and proliferation of murine stromal cells in vitro.
Rac1 knock-down impairs growth and induces apoptosis in the osteoblast cell line OP9. Photomicrograph of OP9 cells infected with nontargeting virus pLKO.1 (SCR; A) or infected with Rac1-shRNA 88 (pLKO.1 vector) demonstrating cytoskeletal elongation (B arrowheads). (C) Apoptosis (annexin V+ cells by flow cytometry) was induced by Rac1shRNA (88 and 92: apoptosis, 24.4% ± 2.6% and 17.4% ± 3.3%, respectively), but not with nontargeting hairpin (SCR, apoptosis 11.7% ± 0.2%, P < .01 vs sh88, P = .05 vs sh92). (D) Reduction in S-phase cell determined by bromodeoxyuridine incorporation caused by Rac1shRNA (88 and 92: S-phase 1.1% ± 0.9% and 1.9% ± 2.0%, respectively), but not nontargeting (SCR: S-phase 9.6% ± 4.0%, P < .05 for comparison with 88 and 92) control. (E) Representative image of bromodeoxyuridine incorporation in OP9 infected with nontargeting (SCR) control hairpin compared with Rac1shRNA 88 (F). All values are means ± SD. n = 3 per condition for each experiment.
Rac1 knock-down impairs growth and induces apoptosis in the osteoblast cell line OP9. Photomicrograph of OP9 cells infected with nontargeting virus pLKO.1 (SCR; A) or infected with Rac1-shRNA 88 (pLKO.1 vector) demonstrating cytoskeletal elongation (B arrowheads). (C) Apoptosis (annexin V+ cells by flow cytometry) was induced by Rac1shRNA (88 and 92: apoptosis, 24.4% ± 2.6% and 17.4% ± 3.3%, respectively), but not with nontargeting hairpin (SCR, apoptosis 11.7% ± 0.2%, P < .01 vs sh88, P = .05 vs sh92). (D) Reduction in S-phase cell determined by bromodeoxyuridine incorporation caused by Rac1shRNA (88 and 92: S-phase 1.1% ± 0.9% and 1.9% ± 2.0%, respectively), but not nontargeting (SCR: S-phase 9.6% ± 4.0%, P < .05 for comparison with 88 and 92) control. (E) Representative image of bromodeoxyuridine incorporation in OP9 infected with nontargeting (SCR) control hairpin compared with Rac1shRNA 88 (F). All values are means ± SD. n = 3 per condition for each experiment.
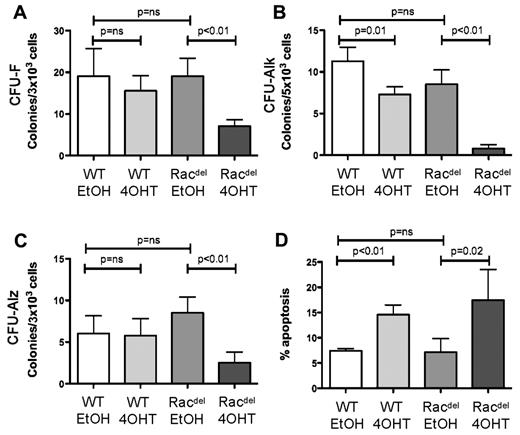
Primary murine MSCs require Rac for growth and osteoblastic differentiation
To validate these cell line experiments in a genetically defined model in which all Rac proteins are absent, primary MSC cultures were generated from mice expressing a conditional allele for Rac1 and deficient for Rac2 and Rac3 (Rac1fl/flRac2−/−Rac3−/−, hereafter referred to as Racdel mice) or WT controls. Racdel or WT MSCs were infected with a tamoxifen-inducible CreER containing retrovirus so that administration of 4OHT would induce the expression of Cre recombinase. Efficient genomic DNA deletion of Rac1 was determined with PCR analysis (supplemental Figure 2A). MSCs were directed into osteoblastic differentiation with 2-glycerol-phosphate, ascorbic acid, and dexamethasone. Induction of Cre expression with 4OHT impaired MSC colony formation (CFU-F) in Racdel MSCs but not in WT controls (Figure 2A and supplemental Figure 2B). CFU-Alk and CFU-Alz (measuring in vitro alkaline phosphatase production and calcification staining with Alizarin Red, respectively) were measured to determine osteoblastic differentiation. 4OHT-induced Cre expression impaired CFU-Alk and CFU-Alz in Racdel MSCs (Figure 2B-C and supplemental Figure 2B). A reduction in CFU-Alk was also observed in WT MSC cultures after 4OHT treatment, however, this effect was less than that observed in Racdel MSC cultures. There was increased apoptosis in 4OHT-treated MSC in Racdel and WT MSC cultures (Figure 2D), which is consistent with toxicity from the sustained expression of Cre recombinase. However, this increase in apoptosis in WT cells did not appear to substantially affect MSC growth or differentiation in vitro. These data demonstrate that Rac proteins are required for the growth and osteoblastic differentiation of primary MSCs in vitro.
Rac deletion impairs osteoblast growth and differentiation in vitro. Primary osteoblast cultures were transduced with an inducible Cre-expressing retrovirus (MSCV-CreER-puro) and treated with 4OHT or with EtOH as a control. (A) CFU-Fs were significantly reduced in Rac-deleted osteoblast cultures after induction of Cre expression by 4OHT (CFU-F Racdel 19 ± 4.4 EtOH vs 7.0 ± 1.6 4OHT), but not in WT controls. (B) CFU-Alk was reduced in Rac-deleted osteoblast cultures after 4OHT treatment (CFU-Alk Racdel 8.5 ± 1.7 EtOH vs 0.8 ± 0.5 4OHT). A modest reduction in CFU-Alk was observed with 4OHT treatment in WT osteoblast controls. (C) CFU-Alz was reduced in Rac-deleted osteoblast cultures after 4OHT treatment (CFU-Alz Racdel 8.5 ± 1.9 EtOH vs 2.5 ± 1.3 4OHT). (D) Apoptosis (annexin V+ cells by flow cytometry) was increased in WT and Rac-deficient osteoblast cultures after 4OHT treatment (Racdel 7.1% ± 2.7% EtOH vs 17.4% ± 6.1% 4OHT; WT 7.4% ± 0.5% EtOH vs 14.5% ± 2.0% 4OHT). All values are means ± SD. n = 3 per condition for each experiment.
Rac deletion impairs osteoblast growth and differentiation in vitro. Primary osteoblast cultures were transduced with an inducible Cre-expressing retrovirus (MSCV-CreER-puro) and treated with 4OHT or with EtOH as a control. (A) CFU-Fs were significantly reduced in Rac-deleted osteoblast cultures after induction of Cre expression by 4OHT (CFU-F Racdel 19 ± 4.4 EtOH vs 7.0 ± 1.6 4OHT), but not in WT controls. (B) CFU-Alk was reduced in Rac-deleted osteoblast cultures after 4OHT treatment (CFU-Alk Racdel 8.5 ± 1.7 EtOH vs 0.8 ± 0.5 4OHT). A modest reduction in CFU-Alk was observed with 4OHT treatment in WT osteoblast controls. (C) CFU-Alz was reduced in Rac-deleted osteoblast cultures after 4OHT treatment (CFU-Alz Racdel 8.5 ± 1.9 EtOH vs 2.5 ± 1.3 4OHT). (D) Apoptosis (annexin V+ cells by flow cytometry) was increased in WT and Rac-deficient osteoblast cultures after 4OHT treatment (Racdel 7.1% ± 2.7% EtOH vs 17.4% ± 6.1% 4OHT; WT 7.4% ± 0.5% EtOH vs 14.5% ± 2.0% 4OHT). All values are means ± SD. n = 3 per condition for each experiment.
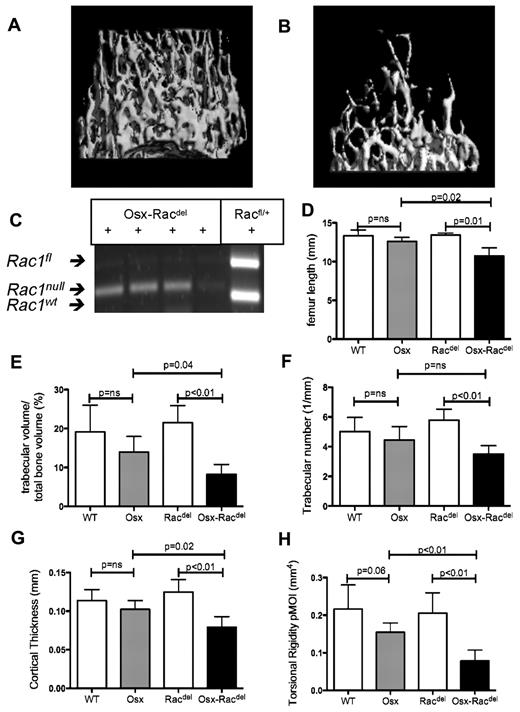
Rac proteins are required for normal bone development in vivo
To validate the in vitro findings in a genetically defined in vivo system and to define the role of osteoblast-restricted Rac expression in HSC function, all 3 known Rac proteins were selectively deleted in osteoblasts using the Osterix-Cre:GFP (Osx) transgenic mouse model crossed with Rac1fl/fl mice in a Rac2−/−Rac3−/− germline-deleted model. Osx-Racdel mice showed runted growth compared with Cre− controls. To measure bone formation in vivo, high-resolution micro-CT was performed on femora from Osx-Racdel mice and Cre− controls. There was a marked effect on long bone size and bone architecture. Osx-Racdel animals demonstrated a striking reduction in trabecular bone formation compared with Cre− controls (Figure 3A-B). To confirm that Rac deletion was achieved in Osx-Racdel osteoblasts, GFP+CD45− osteoblast progenitors were isolated by FACS (see supplemental Figure 4B for gating strategy). Complete deletion of the targeted Rac1 allele was observed in FACS-purified osteoblast progenitor cells (Figure 3C). Furthermore, RNA expression of Rac1 was not detected in osteoblast progenitor cells from Osx-Racdel compared with Osx controls (supplemental Figure 4C). To quantify the reduction in bone formation with Rac deletion, statistical analysis was performed on the micro-CT images. Osteoblast progenitor restricted Rac deletion in vivo caused a reduction in total femur length (Figure 3D), reduced trabecular bone volume fraction, and reduced trabecular number (Figure 3E-F). Similarly, Osx-Racdel mice had reduced cortical bone thickness and reduced cortical bone strength, as estimated by the polar moment of inertia (Figure 3G-H). No macroscopic abnormalities in bone growth were observed when the Osterix-Cre:GFP transgene was suppressed with tetracycline administration, demonstrating that the effects were specific to Cre recombinase–mediated deletion of Rac in vivo.
Osteoblast-restricted Rac deletion leads to defective bone acquisition in vivo. Micro-CT images of distal femoral trabecular bone architecture demonstrating normal bone structure in Racdel mice (Cre− controls; A) and marked reduction of trabecular bone volume and abnormal architecture in Osx-Racdel mice (B). (C) Validation of complete excision of Rac alleles in osteoblasts isolated by flow cytometry in OsxRacdel mice but not Osx-WT controls. (D) Bone length was reduced in Osx-Racdel mice (10.7 ± 1.1 mm) compared with Cre− controls (13.4 ± 0.3 mm, P = .01). No difference was observed between Osx and WT controls (12.6 ± 0.5 mm vs 13.3 ± 0.8 mm, respectively, P = .14; n = 3-5 biologic replicates for each genotype). (E) Trabecular bone volume was reduced in Osx-Racdel mice (8.2% ± 2.6%) compared with Cre− controls (21.5% ± 4.4%, P < .01). No difference was observed between Osx and WT controls (13.9% ± 4.1% vs 19.1% ± 6.9%, respectively, P = .15; n = 4-6 biologic replicates for each genotype; F) Trabecular number was reduced in Osx-Racdel mice (3.5 ± 0.6/mm) compared with Cre− controls (5.7 ± 0.8/mm, P < .01). No difference was observed between Osx and WT controls (4.4 ± 0.9/mm vs 5.0 ± 1.0/mm, respectively, P = .15; n = 4-6 biologic replicates for each genotype; G) Cortical bone thickness was reduced in Osx-Racdel mice (0.078 ± 0.014 mm) compared with Cre− controls (0.124 ± 0.016 mm, P < .01). No difference was observed between Osx and WT controls (0.102 ± 0.012 mm vs 0.113 ± 0.014 mm, respectively, P = .18). (n = 4-6 biologic replicates for each genotype; H.) Estimated cortical bone strength (as measured by the polar moment of inertia) was reduced in Osx-Racdel mice compared with Cre− controls (0.08 ± 0.03 mm4 vs 0.20 ± 0.05 mm4, P < .01). A trend to reduced cortical bone strength was observed in Osx transgenic controls compared with WT controls (0.15 ± 0.03 mm4 vs 0.22 ± 0.06 mm4, respectively, P = .06). (n = 4-6 biologic replicates for each genotype.) All values are means ± SD.
Osteoblast-restricted Rac deletion leads to defective bone acquisition in vivo. Micro-CT images of distal femoral trabecular bone architecture demonstrating normal bone structure in Racdel mice (Cre− controls; A) and marked reduction of trabecular bone volume and abnormal architecture in Osx-Racdel mice (B). (C) Validation of complete excision of Rac alleles in osteoblasts isolated by flow cytometry in OsxRacdel mice but not Osx-WT controls. (D) Bone length was reduced in Osx-Racdel mice (10.7 ± 1.1 mm) compared with Cre− controls (13.4 ± 0.3 mm, P = .01). No difference was observed between Osx and WT controls (12.6 ± 0.5 mm vs 13.3 ± 0.8 mm, respectively, P = .14; n = 3-5 biologic replicates for each genotype). (E) Trabecular bone volume was reduced in Osx-Racdel mice (8.2% ± 2.6%) compared with Cre− controls (21.5% ± 4.4%, P < .01). No difference was observed between Osx and WT controls (13.9% ± 4.1% vs 19.1% ± 6.9%, respectively, P = .15; n = 4-6 biologic replicates for each genotype; F) Trabecular number was reduced in Osx-Racdel mice (3.5 ± 0.6/mm) compared with Cre− controls (5.7 ± 0.8/mm, P < .01). No difference was observed between Osx and WT controls (4.4 ± 0.9/mm vs 5.0 ± 1.0/mm, respectively, P = .15; n = 4-6 biologic replicates for each genotype; G) Cortical bone thickness was reduced in Osx-Racdel mice (0.078 ± 0.014 mm) compared with Cre− controls (0.124 ± 0.016 mm, P < .01). No difference was observed between Osx and WT controls (0.102 ± 0.012 mm vs 0.113 ± 0.014 mm, respectively, P = .18). (n = 4-6 biologic replicates for each genotype; H.) Estimated cortical bone strength (as measured by the polar moment of inertia) was reduced in Osx-Racdel mice compared with Cre− controls (0.08 ± 0.03 mm4 vs 0.20 ± 0.05 mm4, P < .01). A trend to reduced cortical bone strength was observed in Osx transgenic controls compared with WT controls (0.15 ± 0.03 mm4 vs 0.22 ± 0.06 mm4, respectively, P = .06). (n = 4-6 biologic replicates for each genotype.) All values are means ± SD.
To determine whether deletion of Rac proteins impaired osteoblastic maturation, immunohistochemistry was performed on WT, Racdel, and Osx-Racdel mice. In WT and Racdel mice, trabecular bone was lined by layers of osteoblastic cells, which strongly expressed osteocalcin; however, osteocalcin staining was markedly reduced in OsxCre+Racdel mice (supplemental Figure 3). These findings demonstrate that Rac signaling is required for bone growth, development, and osteoblastic maturation.
Differentiation within the osteoblastic progenitor compartment may be examined by analyzing nonhematopoietic and nonvascular (ie, CD45, CD31, and Ter119 negative) cells in the BM for ALCAM−Sca1+ (immature mesenchymal cells) or ALCAM+Sca1− (osteoblast-enriched cells).37,38 We performed flow cytometry analysis on BM from Racdel (n = 4) or Osx-Racdel (n = 2) mice to examine whether the effects of Rac deletion had any effect on the differentiation into these different components of the hematopoietic microenvironment. No differences were observed in CD45−CD31−Ter119−ALCAM+Sca1− or CD45−CD31−Ter119−Sca1+ALCAM− cell populations (supplemental Figure 4A).
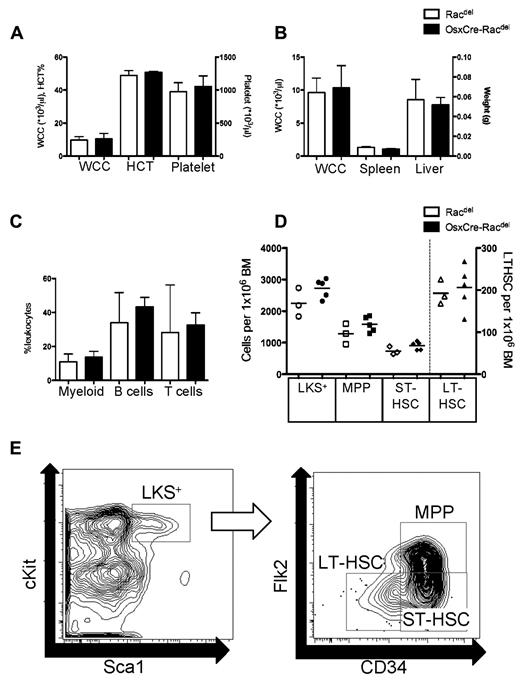
Osteoblastic cell Rac signaling is dispensable for steady-state hematopoiesis
HSCs reside within specialized areas of the BM HM, including endosteal and perivascular zones. Trabecular bone has been specifically implicated in HSC function.3 Because we had observed a significant reduction in bone formation from the deletion of Rac in osteoblast progenitor cells, we hypothesized that this would affect HSC function and consequently hematopoiesis. Mice were examined at between 6 and 10 weeks of age to coincide with the most marked changes in bone phenotype. However, the peripheral blood counts were similar between Racdel and Osx-Racdel mice (Figure 4A). There were no changes in the BM white cell count or size of the extramedullary organs of hematopoiesis (liver and spleen; Figure 4B). The leukocyte immunophenotype was similar between Racdel and Osx-Racdel mice (Figure 4C). Finally, immunophenotyping of BM was performed to determine whether osteoblast-restricted Rac deletion had an effect on HSC-enriched populations. No differences were observed in HSC-enriched LKS+ cells or in LKS+ subpopulations, multipotent progenitors, short-term HSCs, or long-term HSCs (Figure 4D; for FACS gating strategy, see Figure 4E). Long-term (6 months) follow-up did not reveal any differences between Racdel and Osx-Racdel (supplemental Figure 5A-B) of mice. In all cases, the relative proportions of stem cell populations was preserved; however, we sometimes observed reduced total cellularity in the BM that was proportional to the overall reduction in bone size. Therefore, total absolute stem cell numbers (per femur) was reduced in proportion to the total cellularity. These data demonstrate that cell-extrinsic Rac signaling from osteoblastic cells is dispensable for normal hematopoiesis.
Deletion of Rac in osteoblasts does not affect hematopoiesis. (A) Peripheral blood counts were similar between Racdel and Osx-Racdel mice for white blood cell count (WCC, 9.6 ± 2.2 × 103/μL vs 10.3 ± 3.4 × 103/μL, respectively, P = ns), hematocrit (HCT, 48.8% ± 3% vs 50.6% ± 0.8% respectively, P = ns) and platelet counts (973 ± 140 × 103/μL vs 1052 ± 164 × 103/μL, respectively, P = ns; n = 3-6 biologic replicates). (B) No difference in BM cellularity from Racdel and Osx-Racdel mice (9.6 ± 2.2 × 103/μL vs 10.3 ± 3.4 × 103/μL per 1 femur, respectively, P = ns), liver weight (1.3 ± 0.2 g vs 1.0 ± 0.1 g, respectively, P = ns), or spleen weight (0.06 ± 0.02 g vs 0.05 ± 0.01 g, respectively, P = ns; n = 3-6 biologic replicates). (C) Peripheral blood immunophenotype was similar between Racdel and Osx-Racdel for myeloid (10.8% ± 4.7% vs 13.5% ± 3.6%, respectively, P = ns), B cells (33.9% ± 17.8% vs 43.2 ± 5.6%, respectively, P = ns), and T cells (28.1% ± 28.1% vs 32.5% ± 7.3%, respectively, P = ns; n = 3-6 biologic replicates). (D) HSC and progenitor cell populations were similar between Racdel and Osx-Racdel mice; LKS+ 2248 ± 456 vs 2730 ± 303; multipotent progenitors (MPP), 1280 ± 323 vs 1580 ± 244; short-term HSCs (ST-HSC), 736 ± 127 vs 906 ± 131; and long-term HSCs (LT-HSC), 193 ± 29 vs 206 ± 52; P = ns for all, expressed per 1 × 106 BM cells, each dot represents individual biologic replicate. (E) Representative flow cytometry data plot demonstrating gating strategy for LKS+, MPP, ST-HSC, and LT-HSC. All values are means ± SD. Open boxes, Racdel; shaded boxes, Osx-Racdel.
Deletion of Rac in osteoblasts does not affect hematopoiesis. (A) Peripheral blood counts were similar between Racdel and Osx-Racdel mice for white blood cell count (WCC, 9.6 ± 2.2 × 103/μL vs 10.3 ± 3.4 × 103/μL, respectively, P = ns), hematocrit (HCT, 48.8% ± 3% vs 50.6% ± 0.8% respectively, P = ns) and platelet counts (973 ± 140 × 103/μL vs 1052 ± 164 × 103/μL, respectively, P = ns; n = 3-6 biologic replicates). (B) No difference in BM cellularity from Racdel and Osx-Racdel mice (9.6 ± 2.2 × 103/μL vs 10.3 ± 3.4 × 103/μL per 1 femur, respectively, P = ns), liver weight (1.3 ± 0.2 g vs 1.0 ± 0.1 g, respectively, P = ns), or spleen weight (0.06 ± 0.02 g vs 0.05 ± 0.01 g, respectively, P = ns; n = 3-6 biologic replicates). (C) Peripheral blood immunophenotype was similar between Racdel and Osx-Racdel for myeloid (10.8% ± 4.7% vs 13.5% ± 3.6%, respectively, P = ns), B cells (33.9% ± 17.8% vs 43.2 ± 5.6%, respectively, P = ns), and T cells (28.1% ± 28.1% vs 32.5% ± 7.3%, respectively, P = ns; n = 3-6 biologic replicates). (D) HSC and progenitor cell populations were similar between Racdel and Osx-Racdel mice; LKS+ 2248 ± 456 vs 2730 ± 303; multipotent progenitors (MPP), 1280 ± 323 vs 1580 ± 244; short-term HSCs (ST-HSC), 736 ± 127 vs 906 ± 131; and long-term HSCs (LT-HSC), 193 ± 29 vs 206 ± 52; P = ns for all, expressed per 1 × 106 BM cells, each dot represents individual biologic replicate. (E) Representative flow cytometry data plot demonstrating gating strategy for LKS+, MPP, ST-HSC, and LT-HSC. All values are means ± SD. Open boxes, Racdel; shaded boxes, Osx-Racdel.
Rac signaling from osteoblastic cells is not required for HSC function
Because HSC numbers by immunophenotype were unaffected by cell-extrinsic Rac deletion in the osteoblastic niche, the effect of this deletion on HSC function was next determined. To determine the ability of HSCs from Osx-Racdel mice to support hematopoiesis in a transplantation model, lethally irradiated recipient mice were injected with 2 × 106 BM cells from Osx-Racdel mice. Flow cytometric analysis demonstrated predominant donor chimerism for all recipients (16-week donor chimerism was > 95% for all recipients). Peripheral blood white cell count, hematocrit, and platelet counts were normal 16 weeks after transplantation (Figure 5A). To determine the long-term repopulating ability of HSCs from Osx-Racdel mice, BM cells were harvested from recipient mice and transplanted into lethally irradiated secondary recipient mice. After a further 16 weeks, there was predominant donor chimerism in recipient mice (donor chimerism, 81% ± 18%); associated with this were normal peripheral blood white cell counts, hematocrit, and platelet counts (Figure 5B). Finally, competitive transplantation was performed using equal numbers of BM cells from Osx-Racdel mice (expressing CD45.2) and WT mice (expressing CD45.1 and CD45.2) injected into lethally irradiated recipient mice (expressing CD45.1 only). No difference was observed in recipient chimerism between Osx-Racdel mice and Cre− controls (Figure 5C), although a gradual reduction in chimerism compared with WT mice was noted over time in both groups (Figure 5D).
HSCs isolated from Osx-Racdel mice have normal function. (A) Osx-Racdel donor BM transplantation is able to sustain normal blood counts in lethally irradiated recipient mice (white blood cell count [WCC], 19.1 ± 7.9 × 103/μL; hematocrit [HCT], 47.6% ± 4.6%; platelet count, 616 ± 238 × 103/μL). n = 10 recipient mice. (B) Normal blood counts in lethally irradiated secondary recipient mice (WCC, 9.1 ± 2.0 × 103/μL; HCT, 46.6 ± 3.9%; platelet count, 880 ± 130 × 103/μL). (C) Similar BM competitive repopulation between Osx-Racdel and Cre− controls (donor chimerism, 37.4% ± 3.4% vs 35.1% ± 8.6% 16-week chimerism, P = ns; n = 6-7 recipients per condition). (D) Donor chimerism over time of BM derived from Osx-Racdel and Cre− controls (P = ns all time points). All values are means ± SD.
HSCs isolated from Osx-Racdel mice have normal function. (A) Osx-Racdel donor BM transplantation is able to sustain normal blood counts in lethally irradiated recipient mice (white blood cell count [WCC], 19.1 ± 7.9 × 103/μL; hematocrit [HCT], 47.6% ± 4.6%; platelet count, 616 ± 238 × 103/μL). n = 10 recipient mice. (B) Normal blood counts in lethally irradiated secondary recipient mice (WCC, 9.1 ± 2.0 × 103/μL; HCT, 46.6 ± 3.9%; platelet count, 880 ± 130 × 103/μL). (C) Similar BM competitive repopulation between Osx-Racdel and Cre− controls (donor chimerism, 37.4% ± 3.4% vs 35.1% ± 8.6% 16-week chimerism, P = ns; n = 6-7 recipients per condition). (D) Donor chimerism over time of BM derived from Osx-Racdel and Cre− controls (P = ns all time points). All values are means ± SD.
Because both Osx-Racdel and Cre− control mice had germline deletion of Rac2 and Rac3, a competitive repopulation transplantation was performed using WT, Rac2−/−, or Rac2−/−Rac3−/− BM to determine whether this loss of chimerism was because of cell-intrinsic deletion of Rac2, Rac3, or both. Consistent with our previously reported data,20 Rac2−/− BM demonstrated reduced repopulation potential 16 weeks after transplantation (supplemental Figure 6A-B). No difference was observed between Rac2−/− and Rac2−/−Rac3−/− BM, suggesting that Rac3 has nonessential or redundant roles in HSC function. To ensure that this effect was not caused by cell-extrinsic factors, normal BM was transplanted into Rac2−/−Rac3−/− recipients. No differences in white cell count, hematocrit, platelet count, or HSC numbers were observed between WT or Rac2−/−Rac3−/− recipients (supplemental Figure 7A-B). These data demonstrate that Rac2 deletion or combined Rac2 and Rac3 deletion causes cell-intrinsic reduced HSC function. These data demonstrate that loss of Rac signaling from osteoblastic cells is dispensable for HSC function in vivo.
Discussion
The Rac family of Rho GTPases are responsible for integrating cell-extrinsic signals in HSC and other blood lineages. Through these signaling pathways, Rac proteins control critical functions of HSCs, including mobilization, engraftment, survival, and proliferation. These pathways are highly relevant to clinical applications such as HSC transplantation, expansion, regenerative medicine, and treatment of leukemia. The data reported here provide new information regarding the effects of Rac on osteoblastic cells and their progenitors, an important component of the HM, thereby detailing the effects of HSC-extrinsic Rac signaling on HSC function.
Our data demonstrate that Rac signaling is necessary for osteoblast growth and survival. Because germline Rac1-knockout mice are lethal at early embryonic time points, data on the effects of Rac deletion in osteoblastic progenitor cells on bone formation have been lacking. Deletion of Rac family members caused impaired proliferation and induced apoptosis of osteoblastic progenitors in vivo and was associated with cytoskeletal abnormalities. Rac deletion was also associated with impaired terminal osteoblast differentiation in vitro. Deletion of Rac in osteoblastic cells caused runting and impaired bone formation in vivo. These in vivo data are consistent with multiple reports implicating Rac1 in osteoblast cell line adhesion, spreading, and differentiation28 and Rb-induced regulation of several genes involved in adherens junction function, including Rac1.29 Previous studies have not used cells or animals genetically deficient in all 3 mammalian Rac proteins as was done in the present study. This approach eliminates functional redundancy between these highly related GTPases. Whereas Rac1 has been implicated in human osteoblast differentiation,39 germline mutations in Rac leading to bone abnormalities have not been described in humans. It is likely that such mutations would be strongly selected against through the predicted deleterious effects on embryonic development and organogenesis.
Based on the existing literature, such effects on osteoblast function and survival would be predicted to have profound effects on HSC function.33,40,41 However, somewhat surprisingly, Osx-Racdel mice had normal hematopoietic parameters, normal HSC numbers, and normal function in transplantation experiments. These results were unexpected because of the perceived importance of osteoblasts within the HM. However, these results are consistent with observations from other models such as biglycan-deficient mice, which have reduced osteoblast number but normal HSC function,42 and, conversely, strontium-treated mice, which have increased osteoblastic cells and thickened bone trabeculae but normal HSC numbers.43 Furthermore, deletion of β-catenin in the HM impairs osteoblast function without impairing HSC function in vivo.44 These data further strengthen the hypothesis that osteoblastic cells require additional supportive structures to comprise the HSC niche. Furthermore, perturbations in osteoblasts that lead to HSC dysfunction are specific and are not merely related to a quantitative change in osteoblast number or trabecular bone formation. The relative preservation of osteoblastic progenitor cells, despite changes in mature osteoblastic cells and impaired bone formation, may explain the relative preservation in HSC function of Osx-Racdel mice.
In addition to the marked changes in bone formation seen in Osx-Racdel mice, there was a consistent trend toward reduced parameters of bone formation in the Osx control mice compared with WT controls, suggesting that the prolonged expression of Cre recombinase in osteoblast progenitor cells may be toxic to osteoblast development in vivo. In support of this observation, we observed increased apoptosis in WT osteoblast cultures on constitutive retrovirus-induced expression of Cre. To our knowledge, the effects of sustained Cre expression have not been described in osteoblastic cells, however, adverse effects of sustained systemic Cre expression on hematopoietic cells45 and other tissues such as lung epithelium46 have been reported. These findings reinforce the importance of considering Cre-expressing WT controls in addition to Cre− transgenic controls in experimental design and data analysis.
Finally, these data serve to clarify the primarily cell-intrinsic role of Rac signaling in the regulation of HSC function in vivo. Although previous studies have demonstrated the requirements for HSC-intrinsic Rac signaling through transplantation experiments,22 phenotypic differences were noted between primary animals and transplant recipients, raising the possibility that cell-extrinsic factors contributed to the reported findings. The results of the present study demonstrate that HSC-extrinsic Rac signaling, at least as mediated through osteoblastic cells, is dispensable for normal hematopoiesis and HSC function. This is particularly reassuring for the use of Rac inhibitors such as NSC23766 to aid HSC mobilization or leukemia therapy. In these situations, the potential benefit of new agents must be weighed against potential damage or toxicity to the patient.
In summary, Rac signaling is required for the survival and normal development of osteoblastic cells. However, these perturbations in Rac signaling within the HM do not affect hematopoiesis or HSC function in vivo.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Patrick Smits, Dr Siddhartha Mukherjee, and Prof Matthew Warman (Harvard Medical School) for technical advice and comments; Dr D. Kalaitzidis for the MSCV-CreER-puro plasmid and helpful discussions; members of the Williams, Ebert, and Armstrong laboratories for insightful comments; and Meaghan McGuinness, Chad Harris, and Megan Bariteau for expert animal husbandry and support.
S.W.L. has received funding support from the National Health and Medical Research Council of Australia. D.A.W. has received funding support from the US National Institutes of Health (grant DK62757).
National Institutes of Health
Authorship
Contribution: S.W.L. designed and performed the experiments, interpreted the data, and wrote the manuscript; S.D.V., A.P., R.K., M.D.M., and A.M.D. performed the experiments; L.L., K.A.A., and M.L.B. performed the experiments and interpreted the data; and D.A.W. designed the experiments, reviewed the manuscript, and provided supervision.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: David A. Williams, MD, Chief of the Division of Hematology/Oncology, Director of Translational Research for Children's Hospital Boston, Leland Fikes Professor of Pediatrics, Harvard Medical School, Children's Hospital Boston, 300 Longwood Ave, Karp 08125.3, Boston, MA 02115; e-mail: dawilliams@childrens.harvard.edu.


![Figure 5. HSCs isolated from Osx-Racdel mice have normal function. (A) Osx-Racdel donor BM transplantation is able to sustain normal blood counts in lethally irradiated recipient mice (white blood cell count [WCC], 19.1 ± 7.9 × 103/μL; hematocrit [HCT], 47.6% ± 4.6%; platelet count, 616 ± 238 × 103/μL). n = 10 recipient mice. (B) Normal blood counts in lethally irradiated secondary recipient mice (WCC, 9.1 ± 2.0 × 103/μL; HCT, 46.6 ± 3.9%; platelet count, 880 ± 130 × 103/μL). (C) Similar BM competitive repopulation between Osx-Racdel and Cre− controls (donor chimerism, 37.4% ± 3.4% vs 35.1% ± 8.6% 16-week chimerism, P = ns; n = 6-7 recipients per condition). (D) Donor chimerism over time of BM derived from Osx-Racdel and Cre− controls (P = ns all time points). All values are means ± SD.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/3/10.1182_blood-2011-07-368753/5/m_zh89991184780005.jpeg?Expires=1764986284&Signature=pzslStrEK8Ctj17oKnCnQxSYt6lHpAUBk0BO3yU55VIJ0uGnIbLHzT-6EuwiwHle~kVAtymZDu3p-dhoLKxs-ZO~VJGtbmkpHHZDAe11rdPV0OYYMbpTs0~B0DHBG-OMXyHzxNMsa0KdxJPZxVQ0ep2VTSISdrcSp57hDD~wDbfzMstrgGjOi8LZ8ynyzj7Lo~6F9wbcKDCixhsM0-hmlCTQ8vsFRVrv06KR~9Qjjx~cRJ7hrLeo2Zdb4m~W8j0R5hkF4NjfmF~URJKa~fEytVnDIpUKpneS-tktVrZSB39EzPZKRNu-GvuEcbAriDSgOYudstpy99s5x8FMzP51nA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal