Abstract
It is unclear whether karyotype aberrations that occur in regions uncovered by the standard fluorescence in situ hybridization (FISH) panel have prognostic relevance in chronic lymphocytic leukemia (CLL). We evaluated the significance of karyotypic aberrations in a learning cohort (LC; n = 64) and a validation cohort (VC; n = 84) of patients with chronic lymphocytic leukemia with “normal” FISH. An abnormal karyotype was found in 21.5% and 35.7% of cases in the LC and VC, respectively, and was associated with a lower immunophenotypic score (P = .030 in the LC, P = .035 in the VC), advanced stage (P = .040 in the VC), and need for treatment (P = .002 in the LC, P = < .0001 in the VC). The abnormal karyotype correlated with shorter time to first treatment and shorter survival in both the LC and the VC, representing the strongest prognostic parameter. In patients with chronic lymphocytic leukemia with normal FISH, karyotypic aberrations by conventional cytogenetics with novel mitogens identify a subset of cases with adverse prognostic features.
Introduction
Chronic lymphocytic leukemia (CLL) is a clinically heterogeneous disease.1-3 Adverse prognostic parameters include stage,4 CD38 and the unmutated configuration of the variable region of the immunoglobulin heavy chain gene (IGHV),5 ZAP-70,6 and chromosome aberrations.7,8
According to fluorescence in situ hybridization (FISH) analysis to detect trisomy 12 and deletions at 13q14, 11q22-23/ATM, and 17p13/p53, 60%-80% of cases carry an abnormality.9 Patients without FISH aberrations (here referred to as “normal” FISH) have a relatively favorable outcome.9
In vitro stimulation with CpG-oligonucleotide DSP30 plus IL-2 (DSP30/IL2) improves the proliferation of CLL cells, yielding assessable metaphases in most patients.10 By this method, chromosomal aberrations are detected in 80% of CLL patients, with some patients showing aberrations in regions not covered by the classic 4-probe panel.11
The present study was designed to assess whether karyotypic aberrations in CLL cases with normal FISH correlate with established clinical and prognostic parameters. The clinical and prognostic significance of karyotypic aberrations in normal FISH CLL was first evaluated in a retrospective single-center series of patients (learning cohort [LC]) diagnosed between 1998 and 2006 and then validated prospectively in a multicenter series of cases (validation cohort [VC]) diagnosed and analyzed for karyotype with DSP30/IL2 stimulation between 2007 and 2011.
Methods
The LC consisted of 65 of 70 unselected normal FISH CLL patients for whom a successful cytogenetic analysis was available. These patents were derived from a series of 218 consecutive CLL patients diagnosed between 1998 and 2006 at the Hematology Section of the University of Ferrara. The VC consisted of 85 of 85 normal FISH patients with successful cytogenetic analysis derived from a series of 274 consecutive CLL patients diagnosed according to National Cancer Institute criteria12 at 4 GIMEMA (Gruppo Italiano Malattie EMatologiche dell'Adulto) CLL group centers between 2007 and 2011. The Matutes immunophenotypic score13 was calculated, giving 1 point each to CD5 positivity, CD23 positivity, CD22 weak positivity, sIg (surface immunoglobulins) weak positivity, and FMC7 negativity. Only patients with a score ≥ 3 (ie, typical CLL) were included. The expression of CD38 (since 2000) and ZAP-70 (since 2003) was tested on fresh peripheral blood cells with a 20% cutoff for positivity, as described previously.14 This study was approved by the University of Ferrara ethics committee. Indications for treatment included increased white blood cell count with < 6-month lymphocyte doubling time, anemia or thrombocytopenia because of bone marrow infiltration or autoimmune phenomena not responding to steroids, and disease progression in the Binet staging system. Fludarabine-containing regimens were used as first-line treatment; chlorambucil was used in some elderly and unfit patients.
In the LC, cytogenetic analysis was performed with traditional mitogens, as reported previously.8 In the VC, cytogenetic analysis was centralized in the Ferrara center and performed with CpG-oligonucleotide DSP30 (2 μM; TIB MolBiol) plus IL-2 (100 U/mL; StemCell Technologies) as described previously.10,15 In all cases, cytogenetic analysis was conducted on the same samples used for FISH studies. Interphase FISH was performed on peripheral blood samples obtained at diagnosis or before therapy with probes for the following regions: 13q14, 12q13, 11q22/ATM, and 17p13/TP53 (Vysis/Abbott Co) as described previously.16 IGHV genes were amplified from genomic DNA and sequenced according to standard methods; the cutoff of 98% homology to the germline sequence was chosen to discriminate between mutated (< 98% homology) and unmutated (≥ 98% homology) cases, as reported previously.14 TP53 mutational analysis was performed as described elsewhere.17
The Mann-Whitney test and the Fisher exact test were applied for quantitative and categorical variables, respectively. Time to first treatment (TFT) was calculated as the interval between diagnosis and the start of first-line treatment. Overall survival was calculated from the date of diagnosis until death of any cause or until the last patient follow-up. Survival curves were compared by log-rank test. Proportional hazards regression analysis was used to identify the significant independent prognostic variables on TFT. Statistical analysis was performed with Stata 8.0 (Stata Corp) and GraphPad Prism 4.00 for Windows software.
Results and discussion
The present data show that a significant proportion of CLL cases with normal FISH carry chromosome aberrations in regions not covered by the 4-probe FISH panel used in most clinical trials.3,9 An abnormal karyotype was observed in 14 (21.5%) of 65 and 30 (35.7%) of 84 patients in the LC and VC, respectively (P = NS). This novel cytogenetic category (ie, abnormal karyotype with normal FISH) accounted for 6.4% and 10.9% of the cases in the LC and VC, respectively, and for 8.9% in the pooled series of 492 patients in the present study, thus representing the fourth most common cytogenetic group, after deletions at 13q and 11q and trisomy 12.
Recurring aberrations were as follows (supplemental Tables 1 and 2, available on the Blood Web site; see the Supplemental Materials link at the top of the online article): 14q deletions in 8 cases (1 in the LC, 7 in the VC); 7q deletions in 5 cases (1 in the LC, 4 in the VC); 6q deletions in 5 cases (4 in the LC, 1 in the VC); 14q32 translocations in 4 cases (2 in the LC, 2 in the VC); and 3q deletions, distal to the q14 band, in 3 cases (all in the VC). A complex karyotype (≥ 3 aberrations) was found in 14 patients, 12 of whom were in the VC.
The present study confirms previous observations that in CLL patients, stimulation with DSP30/IL2 improves the rate of metaphase generation (65/70 versus 85/85 cases in the LC and VC, respectively; P = .017).10
The correlations between karyotype and clinicobiologic parameters are reported in Table 1. Interestingly, the abnormal karyotype did not correlate with known molecular prognostic parameters, including CD38 and ZAP-70 positivity (in both the LC and VC) and IGHV mutational status in the VC.
Clinical correlations according to karyotype
| Parameter . | Learning cohort . | Validation cohort . | ||||
|---|---|---|---|---|---|---|
| Normal karyotype (51 cases) . | Abnormal karyotype (14 cases) . | P . | Normal karyotype (54 cases) . | Abnormal karyotype (30 cases) . | P . | |
| Mean age, y (range) | 64 (31-84) | 69 (50-87) | NS | 63 (41-90) | 63 (32-84) | NS |
| M/F | 31/20 | 8/6 | NS | 34/20 | 23/7 | NS |
| Matutes score, 3/4/5 | 3/25/23 | 4/3/7 | .030 | 4/24/25 | 7/6/12 | .035 |
| Binet stage, A/B/C | 47/3/1 | 10/3/1 | .089 | 45/9/0 | 20/7/3 | .040 |
| CD38 positive/negative | 21/29 | 8/6 | NS | 11/41 | 12/18 | .079 |
| ZAP-70 positive/negative | 15/6 | 5/4 | NS | 16/31 | 15/11 | .083 |
| IGVH unmutated/mutated | ND | ND | 11/38 | 10/17 | .191 | |
| Therapy, yes/no | 16/35 | 11/3 | .002 | 6/48 | 19/11 | < .0001 |
| Parameter . | Learning cohort . | Validation cohort . | ||||
|---|---|---|---|---|---|---|
| Normal karyotype (51 cases) . | Abnormal karyotype (14 cases) . | P . | Normal karyotype (54 cases) . | Abnormal karyotype (30 cases) . | P . | |
| Mean age, y (range) | 64 (31-84) | 69 (50-87) | NS | 63 (41-90) | 63 (32-84) | NS |
| M/F | 31/20 | 8/6 | NS | 34/20 | 23/7 | NS |
| Matutes score, 3/4/5 | 3/25/23 | 4/3/7 | .030 | 4/24/25 | 7/6/12 | .035 |
| Binet stage, A/B/C | 47/3/1 | 10/3/1 | .089 | 45/9/0 | 20/7/3 | .040 |
| CD38 positive/negative | 21/29 | 8/6 | NS | 11/41 | 12/18 | .079 |
| ZAP-70 positive/negative | 15/6 | 5/4 | NS | 16/31 | 15/11 | .083 |
| IGVH unmutated/mutated | ND | ND | 11/38 | 10/17 | .191 | |
| Therapy, yes/no | 16/35 | 11/3 | .002 | 6/48 | 19/11 | < .0001 |
M/F indicates male/female; NS, not significant; and ND, not done.
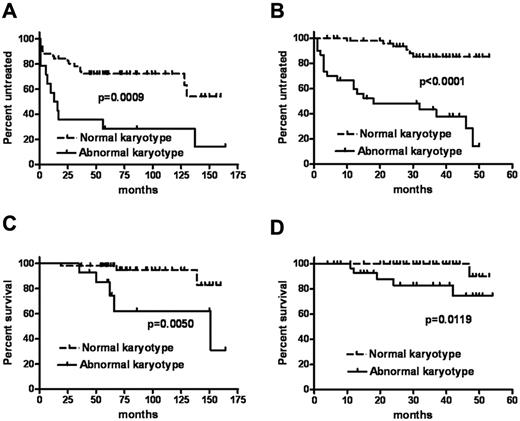
Most importantly, we demonstrated for the first time that among CLL patients with normal FISH, the abnormal karyotype correlated significantly with a shorter TFT in univariate analysis in both the LC and the VC (Table 2; Figure 1). On multivariate analysis, the factors independently predictive of shorter TFT were as follows: In the LC, CD38 positivity (hazard ratio [HR] 2.82, 95% CI 1.19-6.69, P = .018) and abnormal karyotype (HR 2.54, 95% CI 1.07-6.07, P = .034); in the VC, advanced Binet stage (HR 2.77, 95% CI 1.05-7.29, P = .039) and abnormal karyotype (HR 6.39, 95% CI 2.44-16.86, P < .001).
Analysis of factors affecting time to first treatment
| Parameter . | Learning cohort . | Validation cohort . | ||||
|---|---|---|---|---|---|---|
| No. of cases . | HR (95% CI) . | P . | No. of cases . | HR (95% CI) . | P . | |
| Karyotype, abnormal vs normal | 14 vs 51 | 3.33 (2.03-15.66) | .0009 | 34 vs 50 | 7.80 (4.36-25.12) | < .0001 |
| Binet stage, B-C vs A | 8 vs 57 | 4.56 (4.43-89.97) | < .0001 | 19 vs 65 | 3.66 (2.47-26.83) | .0006 |
| CD38 positive vs negative | 29 vs 35 | 3.26 (1.60-7.78) | .0018 | 23 vs 59 | 2.00 (0.91-5.73) | .0786 |
| ZAP-70 positive vs negative | 10 vs 20 | 2.31 (0.81-5.78) | NS | 32 vs 41 | 1.52 (0.70-3.41) | NS |
| IGHV unmutated vs mutated | ND | ND | ND | 21 vs 55 | 2.40 (1.11-7.64) | .0297 |
| Parameter . | Learning cohort . | Validation cohort . | ||||
|---|---|---|---|---|---|---|
| No. of cases . | HR (95% CI) . | P . | No. of cases . | HR (95% CI) . | P . | |
| Karyotype, abnormal vs normal | 14 vs 51 | 3.33 (2.03-15.66) | .0009 | 34 vs 50 | 7.80 (4.36-25.12) | < .0001 |
| Binet stage, B-C vs A | 8 vs 57 | 4.56 (4.43-89.97) | < .0001 | 19 vs 65 | 3.66 (2.47-26.83) | .0006 |
| CD38 positive vs negative | 29 vs 35 | 3.26 (1.60-7.78) | .0018 | 23 vs 59 | 2.00 (0.91-5.73) | .0786 |
| ZAP-70 positive vs negative | 10 vs 20 | 2.31 (0.81-5.78) | NS | 32 vs 41 | 1.52 (0.70-3.41) | NS |
| IGHV unmutated vs mutated | ND | ND | ND | 21 vs 55 | 2.40 (1.11-7.64) | .0297 |
NS indicates not significant; and ND, not done.
TFT and overall survival. TFT and overall survival, respectively, in the learning (A,C) and the validation (B,D) cohorts.
TFT and overall survival. TFT and overall survival, respectively, in the learning (A,C) and the validation (B,D) cohorts.
Recently, it was demonstrated that TP53 mutations18,19 represent a strong prognostic marker in CLL. By mutational analysis, we observed no TP53 mutations in the VC (0 of 23 patients with abnormal karyotype). This finding is not surprising if we consider that patients with 17p− were excluded from the present analysis and that among untreated CLL patients without 17p−, the incidence of TP53 mutations is approximately 3%.17-19
The abnormal karyotype also correlated on univariate analysis with overall survival in both the LC and the VC (HR 5.87, 95% CI 2.08-62.68, P = .005, and HR 9.41, 95% CI 1.61-47.35, P = .0119, respectively; Figure 1). This observation needs to be validated in clinical trials with homogeneous treatment for larger series of patients.
In conclusion, conventional karyotyping with DSP30/IL2 stimulation is an effective method for the detection of chromosome aberrations in approximately one third of CLL patients with normal FISH on a conventional 4-probe panel. This set of data also showed that in CLL patients with normal FISH, conventional cytogenetic analysis identifies a subset of cases with adverse clinical and prognostic features that should be considered for the design of risk-adapted treatment strategies.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The study was supported by FAR 2009 and 2010 of the University of Ferrara (G.M.R. and A.C.), Programma Ricerca Regione Università 2007-2009 University of Ferrara (G.M.R. and A.C.), AIL Ferrara, PRIN 2008 (A.C.), AIRC (G.P.), and Fondazioni CARIVERONA and CARIPARO (an integrated approach to Chronic Lymphoproliferative disorders: B-CLL and virus-related disorders; G.P.).
Authorship
Contribution: G.M.R., G.P., R.F., P.G., and A.C. created and designed the study; G.M.R., F. Cibien, F. Cavazzini, M.C., I.N., F.Z., A.D., F.M., and N.T. provided study materials or patients; E.T. and A.B. performed the cytogenetic analysis; L.R., E.S., and M.N. performed the molecular studies; G.M.R., F. Cibien, S.M., L.F., F. Cavazzini, I.N., F.Z., and N.T. collected and assembled data; and all authors assisted in the analysis and/or interpretation of the data and critically revised and gave final approval of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Gian Matteo Rigolin, MD, PhD, Hematology Section, Azienda Ospedaliero-Universitaria Arcispedale S. Anna, University of Ferrara, Corso Giovecca, 203, 44100, Ferrara, Italy; e-mail: rglgmt@unife.it.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal