Abstract
Abstract 4573
Clostridium difficile, a gram-positive sprore-forming anaerobic bacillus, associated diarrhea (CDAD) is a major cause of nosocomial antibiotic-associated diarrhea. Hematopoietic stem cell transplant (HSCT) recipients are at increased risk of developing CDAD during the early posttransplant period due to prolonged exposure to broad-spectrum antibiotics and immunosuppressive agents. The incidence of CDAD has been increasing up to as high as 20% in allogeneic bone marrow (BMT) and peripheral blood stem cell transplantation (PBSCT). Although cord blood transplant (CBT) recipients are subjected to delayed immune constitution and high incidence of infectious complications to be risk factors for CDAD, the frequency of CDAD after CBT is unclear. We therefore retrospectively investigated the incidence and clinical features of CDAD in patients receiving CBT.
During the 2-yr retrospective period (2007–2008), 201 allogeneic HSCT were performed at the Department of Hematology of Toranomon Hospital: 135 CBT, 39 BMT and 27 PBSCT. The median age of the patients was 56 yr (range, 19–82 yr). All patients with diarrhea had a minimum of one diarrheal stool sample evaluated for the presence of toxin A. A patient found to have toxigenic Clostridium difficile by ELISA was diagnosed as CDAD. The cumulative incidence of CDAD was calculated using the Gray method considering death without CDAD as a competing risk. Overall survival (OS) was estimated by the Kaplan-Meier method. The time-dependent Fine and Gray proportional hazards model was used for multivariate analysis.
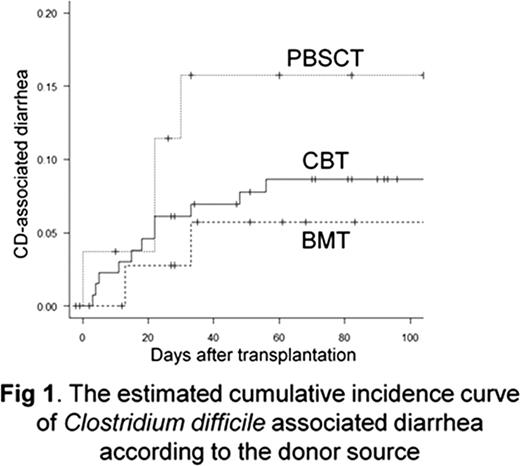
CDAD developed within 100 days in 11 out of 135 CBT recipients at a median onset of day 18 (range, 3–56 days). The cumulative incidence of CDAD after CBT was 9% at day 100 (Fig 1), which was similar to that after BMT (6%, P= 0.55) and to that after PBSCT (16%, P=0.27). All 17 patients who developed CDAD were successfully treated with using oral metronidazole or oral vancomysin. Of the 17 patients with CDAD, 7 (41%) died within 100 days after transplant, and the direct cause of death was irrelevant to CDAD in the 7 patients. The 1-yr survival after diagnosis of CDAD was 58%, which was comparable to that in patients without developing CDAD (59%, P=0.98). The univariate analysis failed to identify any significant risk factors for CDAD as well as the multivariate analysis.
The current study showed that CDAD developed early after CBT at the incidence similar to BMT or PBSCT, and that prompt treatment for CDAD may work in improving its prognosis. It is therefore essential to recognize CDAD as one of the differential diagnosis of diarrhea because it is treatable complication after HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal