Abstract
Abstract 3118
Hematopoietic stem cell (HSC)-targeted gene therapy is potentially curative for the hemoglobin disorders; however, highly efficient, lineage specific globin expression remains elusive, and large animal models thus remain important for further development toward clinical application.
We previously constructed a chimeric HIV1 vector (χHIV vector) system to circumvent a species specific restriction to HIV1-based vectors wherein the HIV1 vector genome is packaged in the context of the simian immunodeficiency virus (SIV) capsid for efficient transduction of rhesus CD34+ cells in vitro (J Virol. 2009) and in vivo (ASH 2009). In this study, we sought to evaluate transduction efficiency and vector integration pattern among long-term repopulating cells in the rhesus HSC transplantation model.
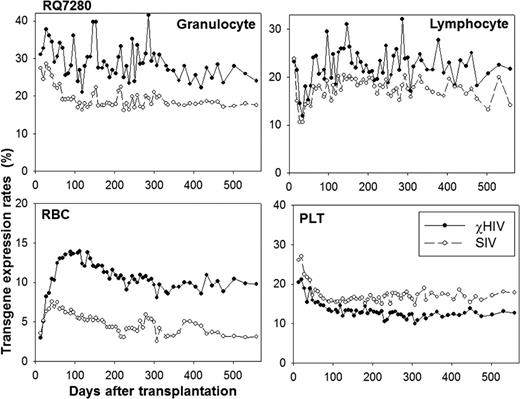
We followed up transgene expression rates among peripheral blood cells of three animals for 1.5–2 years. For two animals (RQ7307 and RQ7280), half of the CD34+ cells were transduced with a standard SIV vector and the other half with the χHIV vector using the same protocol. Transduced cells were transplanted into lethally irradiated rhesus macaques, as previously described (J Virol. 2009). The transgene expression rates in peripheral blood cells plateaued 3–4 months after transplantation and similar transgene expression rates continued in all cell lineages for at least 1.5 years (Figure). The χHIV vector demonstrated that 2–3 fold higher transgene expression rates were seen in granulocytes (RQ7307: 8.6±0.2% vs. 3.1±0.1%, RQ7280: 27.9±0.7% vs. 18.4±0.2%) and RBCs (RQ7307: 3.3±0.1% vs. 0.9±0.0%, RQ7280: 10.0±0.1% vs. 4.0±0.1%), and equivalent transgene expression rates in lymphocytes (RQ7307: 7.8±0.2% vs. 4.5±0.1%, RQ7280: 22.4±0.5% vs. 17.6±0.3%) and platelets (RQ7307: 3.1±0.1% vs. 2.7±0.1%, RQ7280: 12.3±0.2% vs. 16.8±0.2%), compared to the SIV vector. The average vector copy numbers in transduced cells were 4.6–5.7 for the χHIV vector and 1.5–2.0 for the SIV vector in both transplanted animals, evaluated by Southern blot analysis.
We then performed transplantation of rhesus CD34+ cells which were transduced with the χHIV vector alone to evaluate transgene expression and vector integration pattern. Transgene expression rates among peripheral blood cells in this animal (RQ7387) plateaued 1–3 months after transplantation, with stable high transgene expression rates of 51.7±1.2% in granulocytes, 54.7±0.1% in lymphocytes, 22.1±0.2% in RBCs, and 19.1±0.1% platelets for 2 years after transplantation. Multi-lineage marking was observed by flow cytometric analysis.
We then evaluated integration sites for the χHIV vector in the recipient of χHIV vector alone transduced cells by linear amplification mediated-PCR, using peripheral blood cells of RQ7387 in 0.5–1.5 years after transplantation. We found a total of 344 integration sites for the χHIV vector, and our data demonstrated that the χHIV vector integrated into gene regions, especially introns, when compared to the integration pattern of computer-generated random controls (p<0.001). On the other hand, our data revealed fewer integrations of the χHIV vector into ≤30kb upstream of genes (p<0.001) and into the upstream regions of transcription start sites. Most of the integration sites had low gene density (0–10 genes within 1 Mb upstream or downstream of integration sites, p<0.01), compared to that of random controls. No specific trend was noted for the number of integration sites around CpG islands and the number of CISs around integration sites. These data suggest that the χHIV vector has integration patterns comparable to HIV1 and SIV vectors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal