Abstract
Anaplastic lymphoma kinase (ALK)–positive anaplastic large cell lymphoma (ALCL) constitutes an ideal model disease to study tumor-specific immune responses. All the tumor cells express oncogenic ALK resulting from a chromosomal translocation involved in lymphomagenesis. Although antibodies and T-cell responses to ALK have previously been detected in ALK-positive ALCL patients, their prognostic significance is unknown. We investigated a large cohort of uniformly treated ALK-positive pediatric ALCL patients to ascertain whether the titers of preexisting ALK autoantibodies correlated with clinical and histologic characteristics, tumor dissemination, and patient outcome. ALK autoantibodies were analyzed in pretherapeutic serum samples from 95 patients enrolled into 2 therapy studies between 1996 and 2007. ALK autoantibodies were detected in 87/95 patients. The titers inversely correlated with stage and amount of circulating tumor cells. High antibody titers correlated with significantly lower cumulative incidence of relapses (CI-R): titers ≥ 1/60 750, n = 29, CI-R 11% ± 6%; titers 1/2025-< 1/60 750, n = 39, CI-R 31% ± 8%; and titers 0-≤ 1/750, n = 27, CI-R of 63% ± 10% (P < .001). Our results provide the first clinical evidence that a robust preexisting immune response to an oncoantigen resulting from an oncogenic chromosomal translocation inhibits lymphoma dissemination and decreases the risk of relapse.
Introduction
There is increasing evidence of the importance of the immune system in cancer development and control.1,2 Anaplastic lymphoma kinase (ALK)-positive anaplastic large cell lymphoma (ALCL) in children and adolescents represents an ideal tumor model to study the existence and impact of a tumor-specific immune response. First, all tumor cells express high levels of ALK in the form of ALK fusion proteins resulting from oncogenic chromosomal translocations. In contrast to many other tumor-associated antigens (TAAs), ALK fusion proteins exert an essential role in lymphomagenesis and the survival of the tumor cells, therefore representing real oncoantigens.3 The most common ALK fusion protein is nucleophosmin (NPM)–ALK resulting from the t(2;5)(p23;q35) translocation occurring in 90% of ALK-positive ALCLs.4 Second, the normal tissue distribution of ALK is restricted to a few scattered neurons in the central nervous system,5 thus permitting specific targeting of ALK while minimizing problems with autoimmunity. Third, immunity to ALK may be implicated in the control of ALK-positive ALCLs. Antibodies against ALK and cytotoxic T-cell and CD4 T-helper responses to ALK have been detected in patients with ALK-positive ALCLs both at the time of diagnosis and during remission.6-10 Furthermore, murine studies have identified ALK as an ideal tumor antigen for vaccination-based therapies.11
The current study was therefore performed in a large cohort of uniformly treated children and adolescents with ALK-positive ALCLs to investigate (1) the prevalence of a preexisting antibody response to ALK and (2) whether the strength of the antibody response correlates with parameters of tumor dissemination and the risk of relapse.
Methods
Patients
A total of 236 patients from the Berlin-Frankfurt-Muenster group study NHL-BFM95 study with a diagnosis of ALCL and German patients enrolled in the European inter-group trial ALCL99 between April 1996 and November 2007 were eligible for this study. Both studies were approved by the institutional Ethics committee of the primary investigator of the BFM group (A.R.) at Justus-Liebig-University. NPM-ALK positivity of the ALCL was confirmed by at least one of the following: presence of NPM-ALK mRNA, positive 2-color fluorescence in situ hybridization for the t(2;5)(p23;q35) NPM-ALK translocation, and/or immunolabeling studies to show the presence of nuclear and cytoplasmic ALK in the tumor cells.
The treatment strategy was based on protocol NHL-BFM90, as described previously.12,13 Patients were stratified according to stage (St Jude system) and the involvement of at-risk organs.14 Staging procedures included bone marrow (BM) aspiration cytology and a spinal tap. Detection and quantification of submicroscopic amounts of circulating tumor cells in BM or blood at diagnosis were carried out by quantitative real-time polymerase chain reaction (PCR) for NPM-ALK transcripts as previously described.15
Serum and/or plasma samples were obtained at the time of diagnosis from 95 patients. BM or peripheral blood (PB) was obtained before the start of therapy and sent to the NHL-BFM study center within 24 hours. Details of some of these patients are included in previous studies by Damm-Welk et al.15,16
The median age of the 95 study patients at diagnosis was 11.9 years (range, 0.3-17.9 years). The clinical details of the patients are summarized in Table 1. Comparison of the clinical characteristics of the 95 patients analyzed in the current study with those from the 141 German ALCL patients not included in this study showed that increased numbers of patients in the group used in this study had mediastinal (53.7% vs 36.1%, P = .01) or BM (14.7% vs 5.7%, P = .02) involvement resulting in a higher clinical staging for the patients in the current study (stage 3 or 4: 75.9% vs 63.8%, P = .04). Details are provided in supplemental Table 1 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). There was, however, no significant difference with regard to sex, age, or involvement of the skin, visceral organs (lung, liver, and spleen), or central nervous system.
Association of rising antibody titers against ALK with clinical features of the ALCL patients
| Category . | No. of patients (%) . | ALK antibody titer patients, no. (%) . | P . | ||
|---|---|---|---|---|---|
| 0-≤ 1/750 . | 1/2025-< 1/20 250 . | ≥ 1/60 750 . | |||
| All patients | 95 | 27 | 39 | 29 | |
| Age, y | .50 | ||||
| Less than 1 | 1 (1) | 1 (4) | |||
| 1-9 | 33 (35) | 10 (37) | 15 (39) | 8 (28) | |
| 10-18 | 61 (64) | 16 (59) | 24 (61) | 21 (72) | |
| Sex | .02 | ||||
| Female | 35 (37) | 7 (26) | 11 (28) | 17 (41) | |
| Male | 60 (63) | 20 (74) | 28 (72) | 12 (59) | |
| Skin | .22 | ||||
| No | 74 (78) | 18 (67) | 31 (80) | 25 (86) | |
| Yes | 21 (22) | 9 (33) | 8 (20) | 4 (14) | |
| Mediastinum | .01 | ||||
| No | 44 (46) | 8 (30) | 16 (41) | 20 (69) | |
| Yes | 51 (54) | 19 (70) | 23 (59) | 9 (31) | |
| Visceral organs* | .01 | ||||
| No | 62 (65) | 16 (59) | 21 (54) | 25 (86) | |
| Yes | 33 (35) | 11 (41) | 18 (46) | 4 (14) | |
| CNS | .32 | ||||
| No | 90 (95) | 25 (93) | 36 (92) | 29 (100) | |
| Yes | 5 (5) | 2 (7) | 3 (8) | ||
| BM | .11 | ||||
| Negative | 81 (85) | 22 (82) | 31 (80) | 28 (97) | |
| Positive | 14 (15) | 5 (19) | 8 (20) | 1 (3) | |
| Stage† | .004 | ||||
| I | 9 (9) | 2 (7) | 7 (24) | ||
| II | 14 (15) | 2 (7) | 6 (15) | 6 (21) | |
| III | 54 (57) | 17 (63) | 22 (57) | 15 (52) | |
| IV | 18 (19) | 6 (22) | 11 (28) | 1 (3) | |
| Histologic subtype | .15 | ||||
| Common type | 47 (49) | 12 (44) | 17 (44) | 18 (62) | |
| Small cell, lymphohistiocytic, mixed, giant, not further classified | 42 (44) | 14 (52) | 20 (51) | 8 (28) | |
| NA | 6 (6) | 1 (4) | 2 (5) | 3 (10) | |
| Category . | No. of patients (%) . | ALK antibody titer patients, no. (%) . | P . | ||
|---|---|---|---|---|---|
| 0-≤ 1/750 . | 1/2025-< 1/20 250 . | ≥ 1/60 750 . | |||
| All patients | 95 | 27 | 39 | 29 | |
| Age, y | .50 | ||||
| Less than 1 | 1 (1) | 1 (4) | |||
| 1-9 | 33 (35) | 10 (37) | 15 (39) | 8 (28) | |
| 10-18 | 61 (64) | 16 (59) | 24 (61) | 21 (72) | |
| Sex | .02 | ||||
| Female | 35 (37) | 7 (26) | 11 (28) | 17 (41) | |
| Male | 60 (63) | 20 (74) | 28 (72) | 12 (59) | |
| Skin | .22 | ||||
| No | 74 (78) | 18 (67) | 31 (80) | 25 (86) | |
| Yes | 21 (22) | 9 (33) | 8 (20) | 4 (14) | |
| Mediastinum | .01 | ||||
| No | 44 (46) | 8 (30) | 16 (41) | 20 (69) | |
| Yes | 51 (54) | 19 (70) | 23 (59) | 9 (31) | |
| Visceral organs* | .01 | ||||
| No | 62 (65) | 16 (59) | 21 (54) | 25 (86) | |
| Yes | 33 (35) | 11 (41) | 18 (46) | 4 (14) | |
| CNS | .32 | ||||
| No | 90 (95) | 25 (93) | 36 (92) | 29 (100) | |
| Yes | 5 (5) | 2 (7) | 3 (8) | ||
| BM | .11 | ||||
| Negative | 81 (85) | 22 (82) | 31 (80) | 28 (97) | |
| Positive | 14 (15) | 5 (19) | 8 (20) | 1 (3) | |
| Stage† | .004 | ||||
| I | 9 (9) | 2 (7) | 7 (24) | ||
| II | 14 (15) | 2 (7) | 6 (15) | 6 (21) | |
| III | 54 (57) | 17 (63) | 22 (57) | 15 (52) | |
| IV | 18 (19) | 6 (22) | 11 (28) | 1 (3) | |
| Histologic subtype | .15 | ||||
| Common type | 47 (49) | 12 (44) | 17 (44) | 18 (62) | |
| Small cell, lymphohistiocytic, mixed, giant, not further classified | 42 (44) | 14 (52) | 20 (51) | 8 (28) | |
| NA | 6 (6) | 1 (4) | 2 (5) | 3 (10) | |
CNS indicates central nervous system; and NA, not available.
Liver, spleen, and lung.
St Jude staging system.
Sera were also collected from adult patients with ALK-negative ALCL (n = 19), diffuse large B-cell lymphoma (DLBCL, n = 10), Hodgkin lymphoma (n = 10), and follicular lymphoma (n = 10) who were attending the Departments of Hematology, John Radcliffe Hospital, Oxford and Stoke Mandeville Hospital, Stoke Mandeville, United Kingdom, the Internal Medicine Hospital Merkur, Zagreb, Croatia, and the First Department of Medicine, Pecs, Hungary and normal subjects (n = 30). Serum samples were also obtained from 20 age- and sex-matched pediatric patients diagnosed between 2006 and 2009 with lymphoma other than ALK-positive ALCL (10 Burkitt lymphoma, 4 DLBCL, 5 lymphoblastic lymphoma, and 1 T cell–rich B-cell lymphoma). The median age of the 12 boys and 8 girls was 11.6 years (range, 1.4-17.9 years). Informed ethical consent was obtained from all patients and their parents (where relevant) in accordance with the Declaration of Helsinki and local ethical approval.
Detection of the antibody response to ALK
Cytocentrifuge preparations of COS cells transiently transfected with cDNA encoding NPM-ALK or pcDNA3 vector only were prepared and stained with the patient's serum in an indirect immunoperoxidase technique as previously described.6 NPM-ALK transfectants enabled the detection of autoantibodies recognizing epitopes present in the intracytoplasmic region of ALK (present in all ALK fusion proteins) and over the NPM-ALK fusion junction. The highest dilution of the serum/plasma samples at which staining of the NPM-ALK transfectants was still observed was taken as the titer of the antibody. Three groups of patients were identified: antibody dilutions 0-≤ 1/750, 1/2025-< 1/60 750, and ≥ 1/60 750.
Statistical analysis
Differences between subgroups were examined using the χ2 test or Fisher exact test. Analysis of event-free survival (EFS) and overall survival (OS) was performed using the Kaplan-Meier method with differences compared by the log-rank test. Cumulative incidence functions for relapse (CI-R) were constructed following the method of Kalbfleisch and Prentice and compared using Gray test. All analyses were performed using the SAS package (Version 9.1; SAS Institute).
Results
Incidence of anti-ALK antibody titers among patients with NPM-ALK-positive ALCL
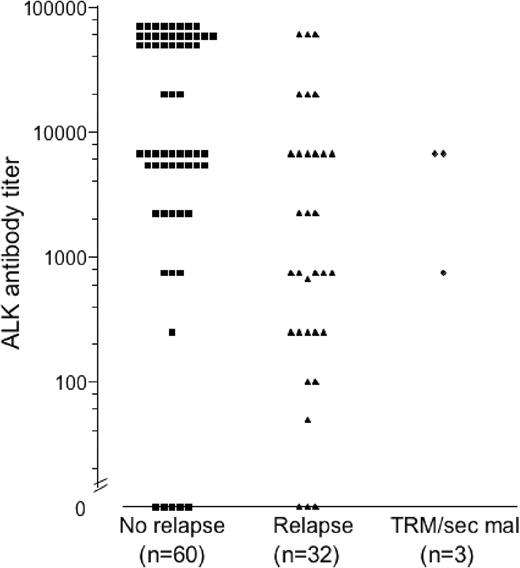
An antibody response to ALK at the time of diagnosis was detected in the serum from 87 (92%) of the 95 ALK-positive ALCL patients studied. Twenty-nine patients (31%) mounted high antibody titers against ALK (≥ 1/60 750), 39 patients (41%) intermediate titers (1/2025-< 1/60 750), and 27 patients (28%) low titers or no antibodies (0-≤ 1/750; Figure 1). With the exception of one boy with DLBCL, no antibodies to ALK were identified in serum from any of the 99 patients with ALK-negative hematologic malignancies or normal subjects. Given the immunogenicity of ALK, it is of interest to follow the clinical course of the 13.5-year-old boy with DLBCL and low antibody titer (< 1/250) to ascertain whether there is any underlying ALK-positive condition.
Anti-ALK antibody titers according to the outcome of the ALCL patients. TRM indicates treatment-related mortality; and sec mal, secondary malignancy.
Anti-ALK antibody titers according to the outcome of the ALCL patients. TRM indicates treatment-related mortality; and sec mal, secondary malignancy.
Correlation between anti-ALK antibody titers and characteristics of patients
A significant correlation was observed between the clinical stage and antibody titers. Forty-five percent of patients with high titers had stage 1 or 2 disease compared with 15% of patients with intermediate or low titers (P = .004, Table 1). In keeping with this result, low antibody titers were significantly associated with advanced stage. There also was a significant association between low antibody titers and the known clinical risk features of mediastinal and visceral organ involvement (P = .01, Table 1).
High antibody titers (≥ 1/60 750) were detected more often in those patients with common subtype (18 of 47 patients, 38%) as opposed to those with lymphohistiocytic, small cell, or other histologic subtypes of ALCL (8 of 42 patients, 19%, P = .06). It was of interest that girls had significantly higher titers of antibodies than boys (P = .02).
Correlation between anti-ALK antibody titers and numbers of circulating tumor cells in BM or blood
Antibody titers and qualitative PCR results for NPM-ALK in BM and PB were available from 76 and 59 patients, respectively. There was a significant inverse correlation between the titers of antibodies to ALK and the presence of NPM-ALK transcripts in BM or PB (P < .001 and P = .004, respectively, Table 2). The inverse correlation between antibody titers and the number of circulating tumor cells was even more pronounced using quantitative PCR and the previously defined prognostic cutoff of 10 copies of NPM-ALK/104 copies ABL in BM (n = 70) or PB (n = 59; Table 2).15 No patient exhibiting high antibody titers (≥ 1/60 750) had more than 10 copies of NPM-ALK/104 copies ABL detectable in either BM or PB (Table 2; P = .001), respectively.
Association of antibody titers against ALK with the presence and amount of circulating tumor cells
| . | All . | ALK-antibody titer patients (%) . | P . | ||
|---|---|---|---|---|---|
| 0-≤ 1/750 . | 1/2025-< 1/20 250 . | ≥ 1/60 750 . | |||
| BM-PCR* | < .001 | ||||
| Negative | 40 | 9 (43) | 10 (33) | 21 (84) | |
| Positive | 36 | 12 (57) | 20 (67) | 4 (16) | |
| PB-PCR* | .004 | ||||
| Negative | 26 | 6 (37) | 6 (25) | 14 (74) | |
| Positive | 33 | 10 (63) | 18 (75) | 5 (26) | |
| BM-quant† | .001 | ||||
| ≤ 10 NCN | 55 | 11 (61) | 19 (70) | 25 (100) | |
| > 10 NCN | 15 | 7 (39) | 8 (30) | 0 (0) | |
| PB-quant† | < .001 | ||||
| ≤ 10 NCN | 42 | 8 (50) | 15 (63) | 19 (100) | |
| > 10 NCN | 17 | 8 (50) | 9 (37) | 0 (0) | |
| . | All . | ALK-antibody titer patients (%) . | P . | ||
|---|---|---|---|---|---|
| 0-≤ 1/750 . | 1/2025-< 1/20 250 . | ≥ 1/60 750 . | |||
| BM-PCR* | < .001 | ||||
| Negative | 40 | 9 (43) | 10 (33) | 21 (84) | |
| Positive | 36 | 12 (57) | 20 (67) | 4 (16) | |
| PB-PCR* | .004 | ||||
| Negative | 26 | 6 (37) | 6 (25) | 14 (74) | |
| Positive | 33 | 10 (63) | 18 (75) | 5 (26) | |
| BM-quant† | .001 | ||||
| ≤ 10 NCN | 55 | 11 (61) | 19 (70) | 25 (100) | |
| > 10 NCN | 15 | 7 (39) | 8 (30) | 0 (0) | |
| PB-quant† | < .001 | ||||
| ≤ 10 NCN | 42 | 8 (50) | 15 (63) | 19 (100) | |
| > 10 NCN | 17 | 8 (50) | 9 (37) | 0 (0) | |
BM indicates bone marrow; and PB, peripheral blood.
Antibody titers against ALK and amount of circulating tumor cells in BM (76 patients) or PB (59 patients) measured by qualitative PCR for NPM-ALK.
Antibody titers and presence of circulating tumor cells in BM (70 patients) or PB (59 patients) measured by quantitative PCR for NPM-ALK.
Prognostic impact of the anti-ALK antibody titer
With a median follow-up of 4.6 years (range, 0.6-10.3 years), the 5-year EFS and OS for the whole group of 95 patients analyzed for an antibody response to ALK were 61% plus or minus 5% and 83% plus or minus 4%, respectively. The CI-R was 34% plus or minus 5%. A total of 32 patients relapsed, 2 died of treatment related toxicity, and one had a second malignancy. A comparison of the outcome data obtained from the NHL-BFM 95 and ALCL99 trials patients not entered into this study is shown in supplemental Table 1.
Of the 32 patients who had a relapse, a high antibody titer (≥ 1/60 750) was detected in 3 (9%), an intermediate titer (1/2025-< 1/60 750) in 12 (37%), and low titers or no detectable antibodies (0-≤ 1/750) in 17 patients (53%). Among the 60 patients who stayed in long-term remission, 26 (43%) showed high titers, 25 (42%) intermediate titers, and 9 (15%) low titers or no antibodies (Figure 1).
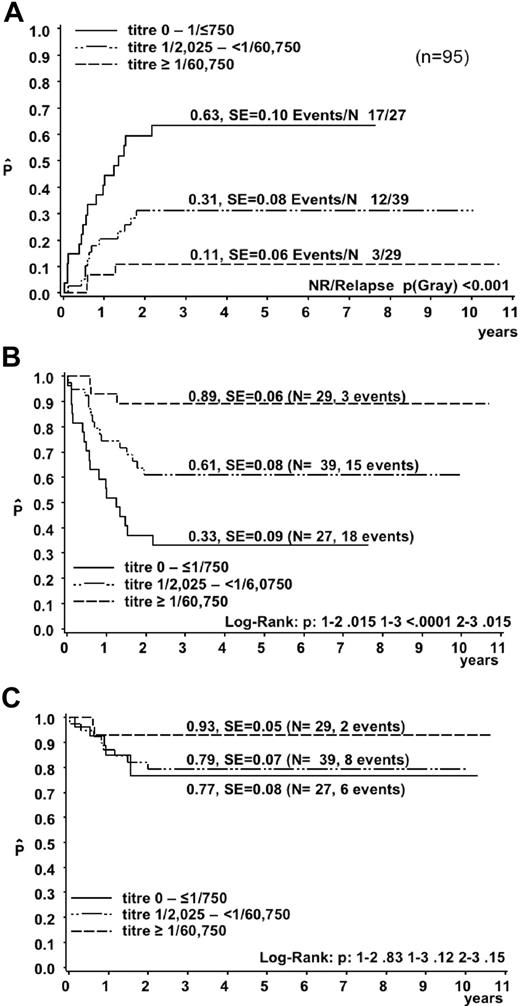
Increasing antibody titers were associated with a decreasing risk of relapse and increasing EFS (Figure 2A-B). Three of the 29 patients with a high antibody titer (≥ 1/60 750) relapsed (CI-R, 11% ± 6%) compared with 12 of 39 patients with intermediate titers (CI-R, 31% ± 8%) and 17 of 27 patients with low titers or no detectable antibodies (CI-R, 63% ± 10%; P < .001). The OS, however, was not significantly different between the 3 groups (Figure 2C), suggesting that rescue therapy for relapsed patients was effective also for patients with low antibody titers. Seventeen of the 32 patients who relapsed were treated by allogeneic hematopoietic stem cell transplantation (HSCT) in their second or later remission. Only 2 of these patients relapsed again after HSCT. For comparison, 13 of 15 relapsed patients treated without allogeneic HSCT relapsed again and died.
Outcome of the 95 ALCL patients according to the magnitude of the antibody response against ALK. (A) Cumulative incidence of relapses. Kaplan-Meier estimates of EFS (B) and OS (C).
Outcome of the 95 ALCL patients according to the magnitude of the antibody response against ALK. (A) Cumulative incidence of relapses. Kaplan-Meier estimates of EFS (B) and OS (C).
Discussion
Unlike the majority of TAAs, ALK fulfills the criteria of an ideal oncoantigen. Not only is it expressed at high levels in tumor cells, absent, or present only at very low levels in normal tissues and possesses a pivotal oncogenic role, it is also immunogenic. ALK-positive ALCL, therefore, constitutes an excellent disease model to study the impact on disease progression and prognosis of a preexisting immune response to an oncoantigen. Although our initial study and subsequent reports describe both B- and T-cell immune responses to ALK in patients with ALK-positive ALCL at diagnosis,6,8,10,17 the present study provides the first clinical evidence that the preexisting antibody response to ALK correlates inversely with tumor dissemination and has prognostic value for patients with this malignancy.
We detected in our 95 patients a significant inverse correlation between the titer of the antibody response against ALK and the following parameters: disease stage and the dissemination of the disease to BM, blood, and visceral organs. These results, obtained from samples taken at diagnosis before treatment, indicate that the titer of the anti-ALK antibody response does not just reflect the extent of the disease. Similar results were obtained in a study on the antibody response to HER-2/neu in breast cancer in early-stage disease.18 The correlation between a high anti-ALK antibody titer at diagnosis and a low clinical stage and an absence of circulating tumor cells suggests that a strong immune response to ALK may prevent lymphoma dissemination, thereby supporting the concept of immunosurveillance. This is strengthened by reports of functional cytotoxic T-cell and T-helper responses to ALK at diagnosis in patients with ALK-positive ALCL.6,8-10
The magnitude of the anti-ALK antibody response may serve as a surrogate marker for the degree of immune-mediated destruction of lymphoma cells in ALK-positive ALCL. Our data cannot determine whether immunomodulation by the tumor and/or the immunogenetic background of the individual patients leads to different anti-ALK immune responses. For example, although the loss of NPM-ALK expression is unlikely, the tumor cells may evade immune recognition by down-regulating major histocompatibility complex class I expression, an event occurring in DLBCL.19 NPM-ALK expression also results in the expression of B7-H1 in ALCL cells, a key immunosuppressive molecule with a role in tumor immune evasion.20 It is of interest that a decreased antibody response was linked to histologic subtypes, such as the lymphohistiocytic subtype, which contains increased numbers of bystander immune cells.21 Immunolabeling studies identifying infiltrating cells, such as dendritic cells,22 cytotoxic T cells,23 and regulatory T cells,24 should provide invaluable information concerning interactions between the tumor microenvironment and the magnitude of the immune response in individual patients. The presence of polymorphisms in genes encoding proteins involved in the immune response, such as the FcRγIIIa receptor for immunoglobulin G, may also affect immunity to tumor antigens.25
Of interest was the finding that higher titers of antibodies were detected in female patients compared with males. Previous reports have described a link between the preponderance of autoimmune disease in females compared with males possibly as a result of estrogens favoring the development of a Th2 response with B-cell activation and subsequent antibody development.26
A significant inverse correlation between the anti-ALK antibody titers and relapse risk was detected in the current study. This finding may shed new light on previous observations that even minimal amounts of circulating ALCL cells in the BM and PB only detected by PCR of the NPM-ALK transcripts are associated with significantly increased risk for relapse.15 The finding of an inverse correlation of the titer of anti-ALK antibodies with the amount of circulating tumor cells in this study suggests that the latter may be the “read out” of the strength of the anti-ALK immune response. The increased risk of relapse in patients with low antibody titers against ALK did not, however, translate into a significant difference in OS. One explanation for this may be that the rescue therapy for the majority of patients surviving after relapse included allogeneic HSCT, thus introducing a potential immunotherapeutic element. The effectiveness of allogeneic HSCT for ALCL relapse patients, even those with chemotherapy refractory or progressive disease,27-29 is suggestive of a graft-versus-ALCL effect.
The strong inverse association between the strength of the preexisting anti-ALK antibody response and relapse risk after chemotherapy is intriguing. First, it implies that the immune response is not completely abrogated during chemotherapy despite the immunosuppressive effects of the treatment. Second, these results suggest that, despite failing to originally prevent tumor development, the immune responses of the patients may have been boosted during chemotherapy, perhaps as a result of increased exposure to ALK-fusion proteins released from dying cells. Conventional cancer chemotherapies, including anthracyclines (also included in ALCL-therapy strategies), have been shown to stimulate dendritic cells to cross-present TAAs, thereby increasing tumor-specific T-cell responses.30
ALK protein expression is not limited to ALCL, being present in inflammatory myofibroblastic tumors, rhabdomyosarcoma, and a subset of B-cell lymphomas.31 Recent studies have also identified ALK expression in a variety of solid tumors. Examples include EML4-ALK and KIF5B-ALK expression in a subset of non-small cell lung carcinoma,32,33 whereas ALK-activating mutations have been described in neuroblastomas.34-36 Our findings of the correlation of circulating antibodies to ALK with tumor dissemination and relapse risk may therefore be of potential relevance in these tumors.
In conclusion, the current study shows, for the first time, in a large cohort of well-characterized and uniformly treated patients, that the magnitude of the autoantibody response to the oncoantigen ALK is inversely correlated with lymphoma dissemination and relapse risk in ALK-positive ALCL. These clinical data support a major role for the adaptive immune response in the development and progression, as well as the final control of ALK-positive ALCL. Our results provide further evidence to support the immunotherapeutic targeting of ALK in ALK-positive ALCL and other ALK-positive tumors.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank J. Schieferstein (expert technical assistance) and U. Meyer (data management) NHL-BFM Study Center, Giessen; German Reference Pathology Panel for NHL in Children Christian-Albrecht-University, Kiel; J. Harbott, Department of Pediatric Hematology and Oncology, Justus-Liebig-University, Giessen and R. Siebert (Department of Human Genetics, Christian-Albrecht-University Kiel (FISH studies), Germany; doctors and nurses in the BFM group, Germany; C. Hatton, Department of Hematology, John Radcliffe Hospital, Oxford, United Kingdom; R. Kusec, Department of Hematology, University of Zagreb, Zagreb, Croatia and A. Szomor Pecs, 1st Department of Medicine, University of Pecs, Pecs, Hungary (for sample collection); and E. Soilleux, Department of Pathology, John Radcliffe Hospital, Oxford, United Kingdom (critical reading of the manuscript).
This work was supported by the Leukemia Research Fund, German Federal Ministry of Education and Research competence network pediatric Oncology and Hematology–Minimal Residual Disease in leukemia and lymphoma (01GI9963/2), the Forschungshilfe Peiper, and the National Institute for Health Research Biomedical Research Center Program.
Authorship
Contribution: K.A.-T. and C.D.-W. performed experimental work; B.B., A.R., and W.W. provided serum samples; and K.A.-T., C.D.-W., B.B., M.Z., W.K., A.R., K.P., and W.W. designed the work, analyzed the data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Karen Pulford, University of Oxford, Nuffield Department of Clinical Laboratory Sciences, John Radcliffe Hospital, Oxford, United Kingdom OX3 9DU; e-mail: karen.pulford@ndcls.ox.ac.uk.
References
Author notes
K.A.-T. and C.D.-W. contributed equally to this study.
K.P. and W.W. are joint last authors.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal