Abstract
Abstract 3197
Poster Board III-134
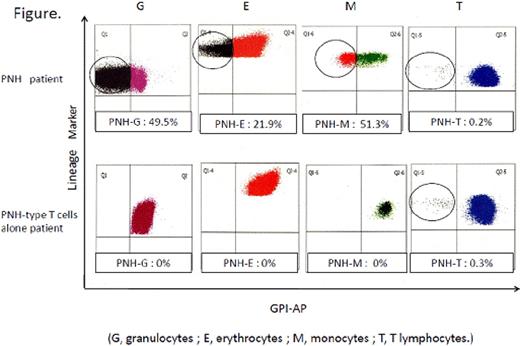
Small populations of glycosylphosphatidylinositol-anchored protein (GPI-AP)-deficient blood cells are often detectable in the peripheral blood (PB) of patients with aplastic anemia (AA) and refractory anemia (RA) of myelodysplastic syndromes defined by the FAB classification. Such PNH-type cells are thought to be derived from PIG-A mutant hematopoietic stem cells (HSCs) that avoid the immunological attack against HSCs. Inefficient T cell responses to PNH-type cells were indeed demonstrated by a murine study. However, there is no direct evidence in support of the escape theory concerning the expansion of PIG-A mutant HSCs in such patients with bone marrow (BM) failure. If the escape theory is true, the PNH-type cells should be detected in myeloid cells derived from HSCs that are targeted by the immune system attack. The PB of 527 patients with BM failure was examined for the presence of GPI-AP deficient cells in various lineages of cells including granulocytes, erythrocytes, monocytes, T cells, B cells, and NK cells using high sensitivity flow cytometry to verify this hypothesis. PNH-type cells were detectable in at least one lineage of cells from 228 (43%) patients. Although most of the positive patients showed PNH-type cells in two or more lineages including granulocytes or monocytes, 14 patients (13 with AA and 1 with amegakaryocytic thrombocytopenia) displayed PNH-type CD48-CD55-CD59- cells only in T cells at a frequency of 0.003-0.3% of the total T cells (Figure). The PNH-type T cells were undetectable in any of 25 healthy individuals. The CD48-CD55-CD59- T cells consisted of predominantly effector memory and terminal effector memory cells with naïve phenotype cells. The phenotypic pattern of the PNH-type T cells was very similar to that of CD48-CD55-CD59- T cells from 11 patients with florid PNH but was different from that of CD48-CD55-CD59- T cells (central and effector memory cells alone) detected in 4 marrow transplant recipients who received anti-CD52 antibody (alemtuzumab) therapy as conditioning. PIG-A gene analyses of CD48-CD55-CD59- T cells revealed a single mutation in 2 patients with PNH-type T cells alone, while two different mutations were revealed in 2 patients treated with alemtuzumab. BM failure patients with PNH-type T cells alone and other BM failure patients possessing PNH-type granulocytes or monocytes showed similar clinical features characterized by predominant thrombocytopenia and good response to immunosuppressive therapy, thus suggesting an increase in the number of PNH-type cells in both groups to be associated with a similar immune pathophysiology. The escape theory cannot account for the presence of PNH-type cells exclusively in T cells in immune-mediated BM failure because T cell precursors are not the target of the immune system attack in AA. Therefore, mechanisms other than the escape theory must be considered for the initial proliferation of PIG-A mutant HSCs associated with the development of AA, such as preferential activation of dormant PIG-A mutant HSCs or T cell precursors due to the deficiency of GPI-APs that transmit negative signal
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal