Comment on Chandra et al, page 2501
There is increasing evidence that chemotherapeutic drugs can work via acceleration of reactive oxygen species in human malignancy.
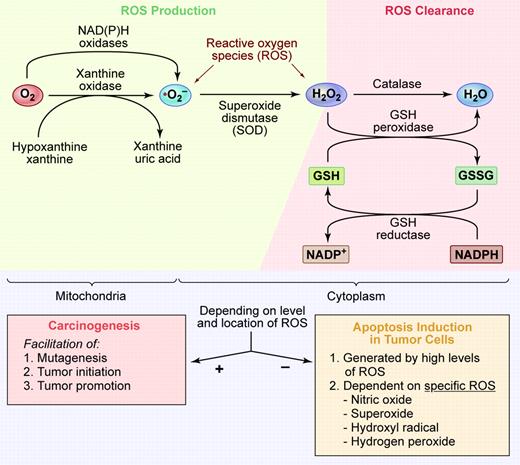
In this issue of Blood, Chandra and colleagues describe the activity of the unique molecule adaphostin, a tyrphostin kinase inhibitor, to kill imatinib mesylate (IM)–resistant cell lines through the generation and/or up-regulation of oxidative stress within these cells. Importantly, adaphostin was able to kill IM-resistant cell lines and even primary blood cells from IM-resistant chronic myelogenous leukemia (CML). This work is of great clinical potential and interest since IM resistance is so frequent in Philadelphia chromosome–positive (Ph+) acute lymphoblastic leukemia (ALL) and chronic myelogenous leukemia (CML) blast crisis.1 This latter clinical observation prompted work on generation and study of second-generation drugs that target the abl kinase. There are now several small-molecule inhibitors of p210Bcr/abl that are showing some clinical benefit but still cannot overcome drug-resistant patients who harbor the T315I mutation site.2 The T315I mutation site has been linked to poor clinical responses, whether to higher-dose IM or to second-generation inhibitors such as AMN107. Enter adaphostin, also originally thought to be an agent that would work primarily by inhibiting the substrate of the Bcr/abl kinase.3 However, this agent is also known to cause an elevation of reactive oxygen species (ROS), and can induce DNA single-strand breaks and DNA damage responses. Consistent with this Bcr/abl-independent mechanism, adaphostin has been found to result in the induction of apoptosis and/or killing of chronic lymphocytic leukemia (CLL) lymphocytes and acute myeloid leukemia (AML) blasts.4,5 In those studies, the antioxidant N-acetylcysteine (NAC) was shown to protect leukemic cells from the lethal impact of adaphostin providing further evidence for the importance of ROS. Chandra and colleague's report now extends the spectrum of adaphostin killing of leukemic cells to IM-resistant leukemic lymphoid and myeloid cells. In Chandra et al's work, both NAC and Trolox (water-soluble vitamin E) protects these cells from apoptosis or other functional damage and provides further evidence for the importance of ROS in adaphostin cytotoxicity. Their report also shows that adaphostin can induce down-regulation of both wild-type (WT) and mutant Bcr/abl protein but independent of ROS generation. Does this mean that the former activity can still contribute to IM-resistant cell killing? We agree with the investigators that their findings strongly encourage further studies of unique agents that work by the up-regulation of ROS. Encouragingly, earlier studies by this group have shown relative selectivity of this drug for leukemic and not normal cells.5,6 As is the case with important scientific works, many other related questions arise, including: what is the exact mechanism of action for this drug in ROS generation; and can it be used in combination with other drugs to affect more complete clinical responses? Recent published work has indeed shown synergism with proteasome inhibition drugs.7 In addition, the remaining challenge is to also understand the fine balance that must exist for ROS collectively or individually (see figure) in their important regulatory role(s) for maintenance of a healthy cell; their role in selection of tumorigenic cells by DNA damage and induction of oncogenic events versus the growing evidence that elevation of ROS levels in human malignant cells can effectively kill these cells. If agents such as adaphostin are to be used wisely in future clinical trials, we will need a more complete biologic understanding of how ROS can be manipulated so as to result in meaningful tumor reduction without impairing normal cellular function. ▪FIG1
(Top) Summary of the primary cell site of ROS generation and the major clearance mechanisms for ROS. (Bottom) Our speculation that dependent on the levels of ROS generated and its compartmentalization in the cell ROS could either induce critical carcinogenic events (arrow with + sign) or alternatively play a more dominant role in tumor cell killing (arrow with the – sign). More work is needed to clearly define the level and type of ROS in tumor cells, their innate clearance mechanism(s), and the levels and species of ROS that can be manipulated to kill tumor cells. Illustration by Kenneth Probst.
(Top) Summary of the primary cell site of ROS generation and the major clearance mechanisms for ROS. (Bottom) Our speculation that dependent on the levels of ROS generated and its compartmentalization in the cell ROS could either induce critical carcinogenic events (arrow with + sign) or alternatively play a more dominant role in tumor cell killing (arrow with the – sign). More work is needed to clearly define the level and type of ROS in tumor cells, their innate clearance mechanism(s), and the levels and species of ROS that can be manipulated to kill tumor cells. Illustration by Kenneth Probst.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal