Abstract
Nonmyeloablative regimens for allogeneic hematopoietic cell transplantation (HCT) have been developed for patients ineligible for myeloablative conditioning. We compared regimen-related toxicities (RRTs) and nonrelapse mortality (NRM) in 73 nonmyeloablative and 73 myeloablative recipients of HLA-matched related donor HCT, using the National Cancer Institute (NCI) Common Toxicity Criteria. Nonmyeloablative regimens were 2 Gy total body irradiation (TBI), either alone (n = 40) or combined with fludarabine, 30 mg/m2/d for 3 days (n = 33). Posttransplantation immunosuppression included mycophenolate mofetil and cyclosporine. Myeloablative regimens consisted mostly of cyclophosphamide + TBI or busulfan + cyclophosphamide, followed by posttransplantation methotrexate and cyclosporine. Nonmyeloablative patients were at higher risk than ablative patients because of greater age, longer time from diagnosis to HCT, more frequent preceding high-dose HCT, and higher pretransplantation Charlson comorbidity scores. Nevertheless, they experienced significantly less severe toxicities in 7 organs/systems: hematologic, gastrointestinal, hepatic, hemorrhage, infection, metabolic, and pulmonary. This translated into less NRM at day 100 (3% versus 23%, P = 10-4) and 1 year (16% versus 30%, P = .04). In multivariate analysis, the strongest factor predicting lessened RRT and NRM was nonmyeloablative conditioning, whereas high pretransplantation comorbidity scores predicted higher NRM. In conclusion, nonmyeloablative regimens had lower RRT and NRM and could be considered for comparative studies, including younger patients with more favorable Charlson comorbidity scores.
Introduction
Allogeneic hematopoietic cell transplantation (HCT) represents a curative treatment option for many patients with advanced hematologic malignancies. Conventional, myeloablative HCT can cause acute toxicities and even mortality because of the intensity of the conditioning regimens used. In addition to direct adverse effects on various organs, regimen-related toxicities (RRTs) may impede the effective delivery of drugs used in the prophylaxis or treatment of infections and graft-versus-host disease (GVHD).1-4 RRTs have restricted the use of conventional HCT to relatively young patients, given that the frequency of fatal toxicities increased with age. However, most patients who could benefit from allogeneic HCT are older and, therefore, ineligible for such treatment.5
The most frequent nonhematologic RRTs were gastrointestinal mucosal damage, infection, and hepatic venoocclusive disease, also called sinusoidal obstruction syndrome (SOS).6 These RRTs might set the stage for a cascade of events, starting from bacterial translocation in already immunocompromised patients, proinflammatory cytokine release (eg, tumor necrosis factor α [TNF-α]), fever, and other organ toxicities, such as acute lung and renal injuries and, eventually, multiorgan failure and death (reviewed in Singer and Bianco7 ). Attempts have been made to reduce RRTs by using pharmacologic agents thought to interfere with these pathophysiologic mechanisms, including pentoxifylline, heparin, or amifostine. Most of these efforts have not translated into significant clinical benefits.8-11 More recently, nonmyeloablative regimens have been developed with the purpose of decreasing RRTs and, thereby, increasing patient eligibility for allogeneic HCT by allowing the inclusion of older patients and those who were debilitated by other concomitant diseases (comorbidities).12-17
In the present retrospective, matched cohort analysis, 3 aims were pursued: first, to describe RRTs in patients receiving HLA-matched related HCT after a nonmyeloablative regimen; second, to compare their RRTs and nonrelapse mortality (NRM) to those among similar and concurrent patients who received transplants after myeloablative regimens; and third, to identify pretransplantation factors that affected HCT outcomes, including the Charlson comorbidity index.18,19
RRTs were analyzed until day 100 and NRM until 1 year after HCT. RRTs beyond day 100 were related to GVHD and late infections, and these RRTs were comparable among nonablative and ablative recipients.20-22
Patients, materials, and methods
This retrospective analysis was approved by the institutional review board of the Fred Hutchinson Cancer Research Center (FHCRC).
Patients
Seventy-three consecutive patients with hematologic malignancies received HCT after a nonmyeloablative regimen (nonablative patients), between December 1997 and December 2000 (Table 1).
Patient characteristics
Characteristic . | Nonablative; n = 73 . | Ablative; n = 73 . | P . |
|---|---|---|---|
| Median age, y | 54 | 48 | < 10-4 |
| Range, y | 21-72 | 21-63 | |
| Age group, % | .35 | ||
| Younger than 20 y | 0 | 0 | |
| 20-40 y | 12 | 18 | |
| Older than 40 y | 88 | 82 | |
| Sex, M/F, % | 64/36 | 60/40 | .61 |
| Diagnosis, % | .005 | ||
| MM | 26 | 16 | |
| MDS | 18 | 12 | |
| NHL | 15 | 18 | |
| CLL | 12 | 10 | |
| HD | 10 | 1 | |
| AML | 8 | 30 | |
| CML | 7 | 7 | |
| Waldenstrom | 3 | 0 | |
| ALL | 1 | 5 | |
| Time to transplantation, mo (range) | 22 (2-159) | 12 (1-198) | .002 |
| Previous failed auto, % | 16 | 0 | < 10-4 |
| Previous planned auto, % | 21 | 0 | < 10-4 |
| Disease status, %* | .60 | ||
| Low risk | 10 | 12 | |
| High risk | 90 | 88 | |
| Hematopoietic cell source, % | < 10-4 | ||
| Marrow | 0 | 30 | |
| G-PBMC | 100 | 70 | |
| CMV risk group, %† | .62 | ||
| High risk | 52 | 48 | |
| Low/intermediate risk | 48 | 52 | |
| Conditioning regimen, % | — | ||
| TBI (2 Gy) | 55 | — | |
| Fludarabine + TBI (2 Gy) | 45 | — | |
| Cy + TBI (12-13.5 Gy) | — | 48 | |
| Bu(t) + Cy‡ | — | 25 | |
| Bu(t) + TMI (9 Gy) ± Cy | — | 16 | |
| Bu + TBI | — | 11 | |
| GVHD prophylaxis, % | — | ||
| CSP + MMF | 100 | 7 | |
| CSP + MTX | — | 92 | |
| CSP + TMTX | — | 1 |
Characteristic . | Nonablative; n = 73 . | Ablative; n = 73 . | P . |
|---|---|---|---|
| Median age, y | 54 | 48 | < 10-4 |
| Range, y | 21-72 | 21-63 | |
| Age group, % | .35 | ||
| Younger than 20 y | 0 | 0 | |
| 20-40 y | 12 | 18 | |
| Older than 40 y | 88 | 82 | |
| Sex, M/F, % | 64/36 | 60/40 | .61 |
| Diagnosis, % | .005 | ||
| MM | 26 | 16 | |
| MDS | 18 | 12 | |
| NHL | 15 | 18 | |
| CLL | 12 | 10 | |
| HD | 10 | 1 | |
| AML | 8 | 30 | |
| CML | 7 | 7 | |
| Waldenstrom | 3 | 0 | |
| ALL | 1 | 5 | |
| Time to transplantation, mo (range) | 22 (2-159) | 12 (1-198) | .002 |
| Previous failed auto, % | 16 | 0 | < 10-4 |
| Previous planned auto, % | 21 | 0 | < 10-4 |
| Disease status, %* | .60 | ||
| Low risk | 10 | 12 | |
| High risk | 90 | 88 | |
| Hematopoietic cell source, % | < 10-4 | ||
| Marrow | 0 | 30 | |
| G-PBMC | 100 | 70 | |
| CMV risk group, %† | .62 | ||
| High risk | 52 | 48 | |
| Low/intermediate risk | 48 | 52 | |
| Conditioning regimen, % | — | ||
| TBI (2 Gy) | 55 | — | |
| Fludarabine + TBI (2 Gy) | 45 | — | |
| Cy + TBI (12-13.5 Gy) | — | 48 | |
| Bu(t) + Cy‡ | — | 25 | |
| Bu(t) + TMI (9 Gy) ± Cy | — | 16 | |
| Bu + TBI | — | 11 | |
| GVHD prophylaxis, % | — | ||
| CSP + MMF | 100 | 7 | |
| CSP + MTX | — | 92 | |
| CSP + TMTX | — | 1 |
MM indicates multiple myeloma; MDS, myelodysplastic syndrome; NHL, non-Hodgkin lymphoma; CLL, chronic lymphocytic leukemia; HD, Hodgkin disease; AML, acute myeloid leukemia; CML, chronic myelogenous leukemia; ALL, acute lymphocytic leukemia; G-PBMC, granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cells; CMV, cytomegalovirus; —, not applicable; TBI, total body irradiation; Cy, cyclophosphamide; Bu(t), busulfan (targeted); TMI, total marrow irradiation (modified TBI); GVHD, graft-versus-host disease; CSP, cyclosporine; MMF, mycophenolate mofetil, MTX, methotrexate; TMTX, trimetrexate.
Low risk disease includes CML in first chronic phase; AML or ALL in first complete remission; early MDS (refractory anemia or refractory anemia with ringed sideroblasts); or agnogenic myeloid metaplasia/myelofibrosis without prior treatment. High-risk disease includes all other classifications
High-risk CMV indicates patient CMV+; Low/intermediate risk, patient- and the donor- or+21
One patient received 16 mg/kg Bu
Eligibility criteria for nonablative conditioning included (1) age 50 years or older for patients with lymphoid malignancies or acute leukemias and 66 years or older for chronic myelogenous leukemia and myelodysplastic syndromes; or (2) younger patients at high risk of RRTs through preceding high-dose HCT and/or pre-existing comorbidities affecting heart, lungs, kidneys, or liver. Exclusion criteria were (1) cardiac ejection fraction less than 40%; (2) severe defects in pulmonary function tests (diffusing capacity of lung for carbon monoxide [DLCO], forced expiratory volume at 1 second [FEV1], or total lung capacity [TLC] < 30%); (3) liver function test (LFT) abnormalities: total bilirubin more than 2 times upper limit of normal (ULN) or aspartate-aminotransferase/alanine-aminotransferase (AST/ALT) more than 4 times ULN; and/or (4) a Karnofsky score less than 50.
Cohort matching procedure. One-to-one matching of nonablative patients with 73 concurrent ablative patients was attempted for the following factors, in descending order: diagnoses, age group (< 20, 20-40, > 40 years old), disease status (high versus low risk of relapse), and sources of hematopoietic cells (marrow versus granulocyte colony-stimulating factor–mobilized peripheral blood mononuclear cells [G-PBMCs]). The 73 patients were identified among 470 recipients of HLA-matched related donor HC transplants, given ablative regimens between January 1997 and December 2000. Exclusion criteria for receiving ablative regimens included (1) age 66 years or older, (2) cardiac ejection fraction less than 45%, (3) pulmonary function tests less than 50%, (4) creatinine greater than 124 μM (1.4 mg/dL), (5) LFT more than 2 times ULN, and/or (5) Karnofsky score less than 70.
Patient characteristics. Patient characteristics are shown in Table 1. Median ages were 54 years (range, 21-72 years) for nonablative and 48 years (range, 21-63 years) for ablative patients (P < 10-4). Diagnoses were slightly different between the 2 patient groups, because there were more nonablative patients with multiple myeloma and Hodgkin disease and fewer with acute myelogenous leukemia. Times from diagnoses to transplantation were longer for nonablative patients (median, 22 versus 12 months, P = .002). Twenty-seven nonablative patients (37%) had received previous high-dose autologous HCT; twelve patients (16%) had relapsed after autografting, whereas in 15 (21%) the autografts were planned for disease reduction.23 None of the ablative patients had received previous high-dose HCT (P < 10-4). All nonablative patients received G-PBMCs, compared with 70% of ablative patients (P < 10-4). Disease status, sex, and cytomegalovirus (CMV) serostatus of recipients and donors were comparable between the 2 groups.
Conditioning regimens
Forty nonablative patients received a single dose of 2 Gy total body irradiation (TBI), delivered at 7 cGy/min on day 0 (Table 1). The remaining 33 patients received fludarabine, 30 mg/m2 body surface area/d intravenously on days -4 to -2, in addition to 2 Gy TBI.16,24
The most common regimens for ablative patients were cyclophosphamide, 60 mg/kg/d for 2 consecutive days, combined with fractionated TBI, 12 to 13.5 Gy3,25 (Cy + TBI, n = 35) and busulfan, given over 4 consecutive days and either targeted to steady-state plasma levels of 800 to 900 ng/mL26 (n = 17), or for a total dose of 16 mg/kg27 (n = 1), followed by cyclophosphamide, 60 mg/kg/d for 2 consecutive days (Bu + Cy). Other regimens were modified TBI28 (9 Gy) and targeted busulfan, with (n = 6) or without (n = 6) a single dose of cyclophosphamide, 60 mg/kg; busulfan, total dose 7 mg/kg given over 4 consecutive days, followed by fractionated TBI, 12 Gy29 (n = 8).
GVHD prophylaxis and treatment
Nonablative patients received mycophenolate mofetil (MMF) and cyclosporine (CSP) for GVHD prophylaxis.20 MMF was administered at 15 mg/kg orally twice a day, from days 0 to +27. CSP was started at 6.25 mg/kg orally twice a day on day -3 and targeted to a trough level of 500 to 600 ng/mL. In 6 patients (8%), CSP was stopped on day +35; in the remaining 67 patients (92%), CSP was gradually tapered from day +35 until day +56, according to evolving GVHD prophylaxis protocols.
Ablative patients received 1 of 3 GVHD prophylaxis regimens, most commonly a short course of methotrexate (MTX) and CSP30 (n = 67). MTX was given at 15 mg/m2 intravenously on day +1 and 10 mg/m2/d on days +3, +6, and +11. CSP was started at 1.5 mg/kg intravenously twice a day, targeted to a trough level of 150 to 450 ng/mL and then switched to oral administration, using a 2.5:1 (oral-intravenous) conversion factor. CSP was gradually tapered from day +50 until day +180.
Supportive care
Comparable supportive care strategies were used in both patient groups. Prophylactic antibiotics (ceftazidime or ciprofloxacin) were administered when the neutrophil counts were less than 0.5 × 109/L. Neutropenic fever was treated with broad-spectrum intravenous antibiotics. Prophylaxis for Pneumocystis carinii was trimethoprim-sulfamethoxazole as first line and dapsone as second line.33 Fluconazole was used for fungal prophylaxis.34 Acyclovir or valacyclovir was used for herpes simplex virus or varicellazoster virus prophylaxis in serologically positive patients.35 Pre-emptive CMV therapy with ganciclovir was used, based on positive CMV antigenemia testing.21 Transfusions with irradiated packed red blood cells and platelets were targeted to maintain hematocrits more than 0.26 (26%) and platelet counts more than 10 × 109/L. Patients did not receive hematopoietic growth factors while on MMF treatment.
Pretransplantation comorbidities
Concomitant diseases at the time of transplantation have been reported to influence the incidence and severity of RRTs and/or NRM.36 Patients were often given nonablative regimens because of comorbidities, which excluded them from ablative HCT. Data on comorbidities were extracted from the patients' pretransplantation evaluation notes and scored by using a template form, shown in Table 2. The template was adapted from the Charlson comorbidity index, a weighted index that took into account the numbers and seriousness of individual diseases.18,19 The Charlson comorbidity index was developed from studies of 1-year mortality for patients admitted to the medical unit of a teaching hospital and subsequently validated to predict mortality for patients with breast cancer. Each individual comorbidity was assigned a specific number of points, and each patient's total score represented the sum of all points assigned. To receive points for a given comorbidity, patients needed to have active symptoms or be on medical treatment at the time of HCT. No points were assigned for hematologic malignancy, as this was the indication for HCT in all patients. As suggested by Charlson et al,18,19 age was not included in the score, because the follow-up was shorter than 5 years. Secondary malignancy (ie, myelodysplastic syndrome resulting from previous chemotherapy for lymphoma) was not assigned comorbidity points, although such patients were considered to have high-risk disease.
Template for determining a patient's comorbidity score
Comorbidities . | Points . |
|---|---|
| Hypertension | 0 |
| Angina | 0 |
| Arrhythmia | 0 |
| Gastrointestinal disease (not ulcer) | 0 |
| Pulmonary disease (mild) | 0 |
| Renal disease (mild) | 0 |
| Endocrine disease (not diabetes) | 0 |
| Myocardial infarction | 1 |
| Congestive heart failure | 1 |
| Peripheral vascular disease | 1 |
| Cerebrovascular disease | 1 |
| Dementia | 1 |
| Peptic ulcer | 1 |
| Liver disease (mild) | 1 |
| Pulmonary disease (moderate/severe) | 1 |
| Connective/rheumatologic | 1 |
| Diabetes (no end organ damage) | 1 |
| Diabetes (end organ damage) | 2 |
| Renal disease (moderate/severe) | 2 |
| Hemiplegia | 2 |
| Liver disease (moderate/severe) | 3 |
| Solid tumor (no metastases) | 2 |
| Solid tumor (metastatic) | 6 |
| AIDS | 6 |
| Other/comment | |
| Patient's score | Total |
Comorbidities . | Points . |
|---|---|
| Hypertension | 0 |
| Angina | 0 |
| Arrhythmia | 0 |
| Gastrointestinal disease (not ulcer) | 0 |
| Pulmonary disease (mild) | 0 |
| Renal disease (mild) | 0 |
| Endocrine disease (not diabetes) | 0 |
| Myocardial infarction | 1 |
| Congestive heart failure | 1 |
| Peripheral vascular disease | 1 |
| Cerebrovascular disease | 1 |
| Dementia | 1 |
| Peptic ulcer | 1 |
| Liver disease (mild) | 1 |
| Pulmonary disease (moderate/severe) | 1 |
| Connective/rheumatologic | 1 |
| Diabetes (no end organ damage) | 1 |
| Diabetes (end organ damage) | 2 |
| Renal disease (moderate/severe) | 2 |
| Hemiplegia | 2 |
| Liver disease (moderate/severe) | 3 |
| Solid tumor (no metastases) | 2 |
| Solid tumor (metastatic) | 6 |
| AIDS | 6 |
| Other/comment | |
| Patient's score | Total |
Posttransplantation toxicity grading
The patients' charts were reviewed, and adverse events reported by attending physicians were graded according to the National Cancer Institute's Common Toxicity Criteria (CTC), version 2.0 (http://ctep.cancer.gov/reporting/CTC-3.html; then select link “Common Toxicity Criteria Document”). Laboratory data (chemistries and hematologic values) were extracted from the FHCRC database. The CTC provided a descriptive terminology for adverse events and a coded grading (severity) scale for each toxicity. It was more sensitive to small changes in toxicity than the Bearman scale,1,2 which made it more suitable to evaluate RRTs after nonablative conditioning.
Each toxicity was recorded within its corresponding affected organ system, noting a grade (1 mild, 2 moderate, 3 severe, 4 life-threatening, or 5 lethal) and the day of occurrence after transplantation. Event collection was censored at the moment of disease relapse or progression, to focus exclusively on RRTs and NRM. Toxicities related to GVHD and infections were scored only once under 1 of the 2 categories and not under the specific organs affected to avoid multiple grading of individual RRTs. An infectious event required microbiologic confirmation, or clinical/radiologic suspicion (ie, febrile neutropenia, positive imaging study). Whenever available, information from consult notes and biopsy or autopsy data were used to corroborate RRTs or NRM. Because of their clinical implications, only toxicity grades 3 to 5 were considered in the analyses and, hereafter, have been referred to as “severe toxicities.”
Patients could experience several RRTs within the same organ system during the study period. In those cases, events were registered at each occurrence, to have qualitative and quantitative evaluations of posttransplantation toxicities.
Statistical analyses
For comparison of characteristics between the 2 patient groups, chi-square statistics were used to compare proportions, and 2-sample t tests were used to compare continuous outcomes. Cumulative incidence curves were estimated according to published methods,37 treating death and relapse/progression as competing events. Multivariate analyses of proportions were performed by using logistic regression. Cox proportional hazards analyses were performed to model hazard ratios for 1-year NRM. Pretransplantation parameters considered for the model were type of regimen, comorbidity score, CMV risk, diagnosis, disease risk, hematopoietic cell source, age, previous HCT, time from diagnosis to transplantation, and donor sex. All P values were based on likelihood ratio statistics and were 2-sided. Multivariate P values for a variable reflected adjustment for all other variables in the model.
Results
Comorbidities before HCT
Nonablative patients had higher comorbidity scores than ablative patients (Table 3). The highest comorbidity scores were 4 among nonablative and 3 among ablative patients. Thirty-two (44%) of the nonablative patients had scores of 1 or greater, compared with 16 (22%) of the ablative patients (P = .005). The most frequent serious comorbidities were pulmonary, hepatic, and renal, all more prevalent among nonablative patients. Comorbid conditions unique to nonablative patients were moderate/severe liver disease (cirrhosis, n = 2; nonalcoholic steatohepatitis, n = 1; and portal hypertension, n = 1), pneumonia (Aspergillus, n = 2; and CMV, n = 1), renal failure requiring hemodialysis (n = 2), and poor left-ventricular function (n = 2).
Patients' Charlson comorbidity scores at the time of transplantation
. | Scores . | . | . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
. | 0 . | 1 . | 2 . | 3 . | 4 . | Total . | ||||
| Nonablative patients, n | 41 | 21 | 5 | 4 | 2 | 73 | ||||
| Ablative patients, n | 57 | 13 | 1 | 2 | 0 | 73 | ||||
. | Scores . | . | . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
. | 0 . | 1 . | 2 . | 3 . | 4 . | Total . | ||||
| Nonablative patients, n | 41 | 21 | 5 | 4 | 2 | 73 | ||||
| Ablative patients, n | 57 | 13 | 1 | 2 | 0 | 73 | ||||
Toxicities after HCT
Nonablative patients. The incidence of severe (grades 3-5) toxicities was significantly lower (P ≤ .05) among nonablative patients within 8 of 12 categories studied, which included neutropenia, thrombocytopenia, gastrointestinal, hemorrhage, hepatic, infection, metabolic, and pulmonary (Table 4). No significant differences were seen for cardiovascular, neurologic, renal, and other RRTs. Following is a description of grades 3 to 5 toxicities.
CTC grades 3 to 5 toxicities
. | Cumulative incidences . | . | . | Mean number of events per patient . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Category . | Nonablative patients, % . | Ablative patients, % . | P . | Nonablative patients . | Ablative patients . | P . | ||||
| Hematologic | 2.3 | 4.7 | < 10-4 | |||||||
| Neutropenia | 58 | 100 | < 10-4 | — | — | — | ||||
| Thrombopenia | 18 | 97 | < 10-4 | — | — | — | ||||
| Rejection | 7 | 0 | .008 | — | — | — | ||||
| Cardiovascular | 58 | 66 | .31 | 0.7 | 0.8 | .28 | ||||
| Gastrointestinal | 8 | 78 | < 10-4 | 0.1 | 0.9 | < 10-4 | ||||
| Hemorrhage | 1 | 8 | .04 | 0.01 | 0.1 | .05 | ||||
| Hepatic | 16 | 49 | < 10-4 | 0.2 | 1.0 | < 10-4 | ||||
| Infection | 58 | 88 | < 10-4 | 0.9 | 2.4 | < 10-4 | ||||
| Metabolic | 58 | 74 | .04 | 1.1 | 1.7 | .01 | ||||
| Neurologic | 7 | 15 | .11 | 0.1 | 0.2 | .09 | ||||
| Pulmonary | 4 | 14 | .04 | 0.04 | 0.2 | .03 | ||||
| Renal | 12 | 18 | .35 | 0.2 | 0.3 | .41 | ||||
| Other | 12* | 18† | .35 | 0.1 | 0.3 | .08 | ||||
. | Cumulative incidences . | . | . | Mean number of events per patient . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Category . | Nonablative patients, % . | Ablative patients, % . | P . | Nonablative patients . | Ablative patients . | P . | ||||
| Hematologic | 2.3 | 4.7 | < 10-4 | |||||||
| Neutropenia | 58 | 100 | < 10-4 | — | — | — | ||||
| Thrombopenia | 18 | 97 | < 10-4 | — | — | — | ||||
| Rejection | 7 | 0 | .008 | — | — | — | ||||
| Cardiovascular | 58 | 66 | .31 | 0.7 | 0.8 | .28 | ||||
| Gastrointestinal | 8 | 78 | < 10-4 | 0.1 | 0.9 | < 10-4 | ||||
| Hemorrhage | 1 | 8 | .04 | 0.01 | 0.1 | .05 | ||||
| Hepatic | 16 | 49 | < 10-4 | 0.2 | 1.0 | < 10-4 | ||||
| Infection | 58 | 88 | < 10-4 | 0.9 | 2.4 | < 10-4 | ||||
| Metabolic | 58 | 74 | .04 | 1.1 | 1.7 | .01 | ||||
| Neurologic | 7 | 15 | .11 | 0.1 | 0.2 | .09 | ||||
| Pulmonary | 4 | 14 | .04 | 0.04 | 0.2 | .03 | ||||
| Renal | 12 | 18 | .35 | 0.2 | 0.3 | .41 | ||||
| Other | 12* | 18† | .35 | 0.1 | 0.3 | .08 | ||||
— indicates not done.
Hematopoietic cell infusion reactions (n = 5), musculoskeletal events (n = 2), hemolytic-uremic syndrome (HUS, n = 1), and allergic reaction (n = 1)
Dermatological (n = 4), musculoskeletal (n = 4), HUS (n = 3) and hematopoietic cell infusion reactions (n = 2)
Hematologic. Fifty-eight percent of patients had neutropenia less than 0.5 × 109/L for a median of 9 days (range, 1-39 days); 18% had thrombocytopenia less than 20 × 109/L for a median of 6 days (range, 1-49 days). Five patients (7%) experienced graft rejection between days 83 and 127 after transplantation.
Cardiovascular. Fifty-eight percent of patients had grade 3 toxicities, most often hypertension requiring therapy (52%). Five percent developed grade 3 congestive heart failure, responsive to treatment. None developed grade 4 or 5 toxicities.
Gastrointestinal. There were no grade 4 or 5 gastrointestinal toxicities and no grade 3 to 5 mucositis. Eight percent of patients had grade 3 nausea and/or vomiting.
Hemorrhage. Severe gastrointestinal hemorrhage developed in 1 patient (1%).
Hepatic. Sixteen percent of patients had grade 3 or 4 LFT abnormalities, consisting of total bilirubin more than 3 times ULN (> 51 μM [> 3.0 mg/dL]). One patient had grade 4 elevation of bilirubin (> 10 × ULN, or 171 μM [10.0 mg/dL]). None had SOS.
Infection. Eleven percent of patients had fever and bacteremia during neutropenia, and 36% had only non-neutropenic events, primarily CMV antigenemia. Eleven percent experienced both neutropenic and non-neutropenic events.
Metabolic. Fifty-eight percent of patients had at least one severe metabolic abnormality, including hyponatremia (< 130 mM) in 42%, hyperglycemia (> 13.9 mM [> 250 mg/dL]) in 37%, hypokalemia (< 3 mEq/L) in 11%, and hypomagnesemia (< 0.4 mM [< 0.9 mg/dL]) in 3% of patients.
Neurologic. Seven percent of patients had central nervous system (CNS) events. There were 2 episodes of CNS bleeding and 1 each of depression, seizure, and confusion.
Pulmonary. Two patients had acute lung injuries, and one experienced hypoxia.
Renal. Twelve percent of patients had creatinine elevations more than 3 times ULN (318 μM [3.6 mg/dL]). Four percent required de novo hemodialysis.
GVHD. The incidence of grades 3 to 4 acute GVHD before day 100 was 19%, with a median onset on day 46. The 1-year incidence of chronic extensive GVHD was 56%.
Other toxicities. There were 9 severe events, 5 related to hematopoietic cell infusion (fever, shortness of breath), 2 musculoskeletal events (gout and bone pain), 1 hemolytic-uremic syndrome related to CSP, and 1 allergic reaction (rash).
Ablative patients. The distribution of toxicities among ablative patients was as follows.
Hematologic. One hundred percent of the patients had neutropenia (< 0.5 × 109/L), for a median of 16 days (range, 7-37 days), and 97% had thrombopenia (< 20 × 109/L), for a median of 5 days (range, 1-33 days). No patient experienced graft rejection.
Cardiovascular. Hypertension was seen in 58% and congestive heart failure in 7% of patients.
Gastrointestinal. Seventy-eight percent of patients had severe events. Mucositis requiring parenteral nutrition was the most frequent (70%), and nausea, vomiting, or diarrhea was encountered in an additional 8% of patients.
Hemorrhage. Eight percent of patients had bleeding episodes, most commonly affecting the gastrointestinal tract.
Hepatic. Eighteen percent of patients had SOS, and 31% had elevations of LFTs: total bilirubin more than 3 times ULN; AST, ALT, or alkaline phosphatase more than 5 times ULN, without SOS.
Infection. Thirty-two percent of patients experienced neutropenic events, including fever and bacteremia, 19% had non-neutropenic events, primarily CMV antigenemia, and 37% had both neutropenic and non-neutropenic events.
Metabolic. Seventy-four percent of patients had at least one severe metabolic abnormality. Hyponatremia occurred in 40%, hyperglycemia in 21%, hypokalemia in 21%, hyperkalemia (> 6 mEq/L) in 14%, and hypomagnesemia in 8% of patients.
Neurologic. Fifteen percent of ablative patients had neurologic toxicity. Delirium (8%) and ataxia (3%) were the most common events.
Pulmonary. Fourteen percent of patients had severe RRTs, most often acute lung injury (8%).
Renal. Eighteen percent of patients had severe renal failure, and 12% needed de novo hemodialysis.
GVHD. The incidence of grades 3 to 4 acute GVHD before day 100 was 16%, with a median onset on day 20. The 1-year incidence of chronic extensive GVHD was 43%.
Other toxicities. There were 13 severe events, including 4 dermatologic, 4 musculoskeletal (pathologic fracture, muscle weakness, or rhabdomyolysis), 3 episodes of hemolytic-uremic syndrome, and 2 hematopoietic cell infusion reactions.
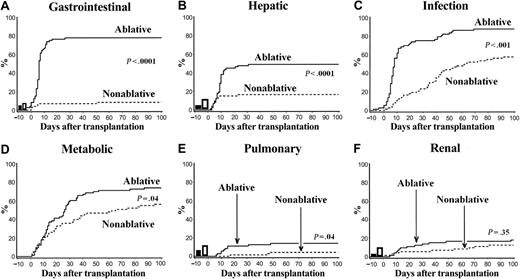
Cumulative incidences of toxicities.Figure 1 compares the day-100 cumulative incidences of severe toxicities in 6 of the above-mentioned categories. Most RRTs occurred early after transplantation in both patient groups. The curves diverged as early as day 10 for gastrointestinal, hepatic, infectious, and pulmonary events and between days 20 and 30 for metabolic events. The day-100 cumulative incidences of RRTs in these 5 categories were significantly lower among nonablative patients. For the renal system, events occurred later in the nonablative patients, with median times of occurrence being day 36 in the nonablative compared with day 13 for ablative patients. However, the day-100 cumulative incidences of renal toxicities were similar. The percentages of patients with comorbidities at the time of HCT are also shown for 4 organs. Nonablative patients had greater degrees of hepatic, pulmonary, and renal comorbidities and comparable gastrointestinal comorbidity.
Comparisons of cumulative incidences of severe day-100 nonhematologic toxicities among HCT recipients given nonablative versus ablative conditioning. Shown are CTC grades 3 to 5 toxicities in the following individual organ systems: (A) gastrointestinal, (B) hepatic (C) infection, (D) metabolic, (E) pulmonary, and (F) renal. Percentages of patients having organ-specific comorbidities before HCT are represented as open bars (□) for nonablative and as solid bars (▪) for ablative recipients.
Comparisons of cumulative incidences of severe day-100 nonhematologic toxicities among HCT recipients given nonablative versus ablative conditioning. Shown are CTC grades 3 to 5 toxicities in the following individual organ systems: (A) gastrointestinal, (B) hepatic (C) infection, (D) metabolic, (E) pulmonary, and (F) renal. Percentages of patients having organ-specific comorbidities before HCT are represented as open bars (□) for nonablative and as solid bars (▪) for ablative recipients.
Mean number of toxicities in individual organ systems. Some patients experienced multiple or repeated toxicities within the same organ system (Table 4). In the 7 systems described earlier, there were lower numbers of severe events per patient in the nonablative group. Specifically, nonablative patients had approximately half as many episodes of cytopenias, infection, or metabolic abnormalities, 5 times fewer episodes of hepatic and pulmonary RRTs, and 9 to 10 times fewer episodes of gastrointestinal RRTs or hemorrhage than ablative patients.
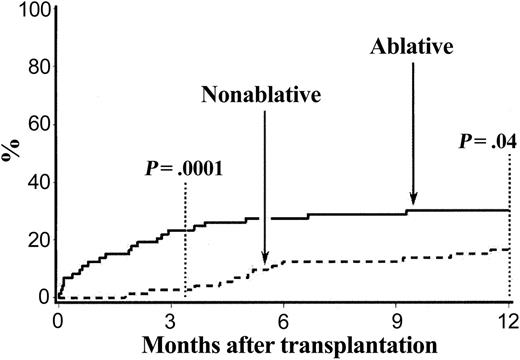
Nonrelapse mortality
Day-100 and 1-year NRMs were 23% and 30% for ablative patients, compared with 3% and 16% for nonablative patients, respectively (P = 10-4 and .04; Figure 2). Most deaths among ablative patients occurred during the first 3 months after HCT, whereas most deaths among nonablative patients occurred between 3 and 6 months. Overall, 12 nonablative and 22 ablative patients died within the first year from infections with or without preceding GVHD (n = 24), SOS (n = 5), acute lung injury (n = 2), and CNS complications (n = 3) (P = .04; Table 5). Twelve infectious deaths were from fungal infections (11 Aspergillus and one Acremonium), 8 from bacterial infections (6 septic shock, one Klebsiella pneumonia, and 1 bacterial peritonitis), and 4 from CMV infections.
Cumulative incidences of 1-year nonrelapse mortality among HCT recipients given nonablative versus ablative conditioning.
Cumulative incidences of 1-year nonrelapse mortality among HCT recipients given nonablative versus ablative conditioning.
One-year nonrelapse mortality
. | Nonablative . | Ablative . | P . |
|---|---|---|---|
| Causes of death, n | |||
| Infection/GVHD | 10 | 14 | |
| SOS | 0 | 5 | |
| Acute lung injury | 0 | 2 | |
| CNS | 2 | 1 | |
| Total, n | 12 | 22 | .04 |
| Cumulative incidence, % | 16 | 30 |
. | Nonablative . | Ablative . | P . |
|---|---|---|---|
| Causes of death, n | |||
| Infection/GVHD | 10 | 14 | |
| SOS | 0 | 5 | |
| Acute lung injury | 0 | 2 | |
| CNS | 2 | 1 | |
| Total, n | 12 | 22 | .04 |
| Cumulative incidence, % | 16 | 30 |
GVHD indicates graft-versus-host-disease; SOS, sinusoidal obstruction syndrome; CNS, central nervous system toxicity.
Risk factors for RRT and NRM (multivariate analyses)
The analyses shown in Table 6 were directed at identifying factors predicting both infectious and hepatic toxicities and 1-year NRM. Significant associations are detailed below.
Multivariate analysis for specific toxicities (grades 3-5) and NRM
. | Infection . | . | Hepatic . | . | 1-year NRM . | . | |||
|---|---|---|---|---|---|---|---|---|---|
| Risk factor . | OR (95% CI) . | P . | OR (95% CI) . | P . | HR (95% CI) . | P . | |||
| Type of regimen | |||||||||
| Nonablative vs ablative | 0.2 (0.1-0.4) | < 10-4 | 0.3 (0.1-0.6) | .002 | 0.4 (0.2-1.0) | .06 | |||
| Comorbidity score | NS | NS | .002 | ||||||
| 0 | Reference | ||||||||
| 1,2 | 3.3 (1.6-7.1) | ||||||||
| 3 or more | 7.9 (2.0-31) | ||||||||
| CMV risk* | |||||||||
| High vs low/intermediate | 3.4 (1.4-8.1) | .004 | NS | NS | |||||
| Diagnosis group | .04 | NS | NS | ||||||
| AML, MDS | Reference | ||||||||
| MM | 0.3 (0.1-0.9) | ||||||||
| NHL, HD, Waldenstrom | 0.5 (0.2-1.6) | ||||||||
| CLL, CML, ALL | 1.5 (0.4-5.5) | ||||||||
| Hematopoietic cell source | |||||||||
| Marrow vs G-PBMC | NS | 3.1 (1.1-8.8) | .03 | 2.9 (1.3-6.9) | .02 | ||||
. | Infection . | . | Hepatic . | . | 1-year NRM . | . | |||
|---|---|---|---|---|---|---|---|---|---|
| Risk factor . | OR (95% CI) . | P . | OR (95% CI) . | P . | HR (95% CI) . | P . | |||
| Type of regimen | |||||||||
| Nonablative vs ablative | 0.2 (0.1-0.4) | < 10-4 | 0.3 (0.1-0.6) | .002 | 0.4 (0.2-1.0) | .06 | |||
| Comorbidity score | NS | NS | .002 | ||||||
| 0 | Reference | ||||||||
| 1,2 | 3.3 (1.6-7.1) | ||||||||
| 3 or more | 7.9 (2.0-31) | ||||||||
| CMV risk* | |||||||||
| High vs low/intermediate | 3.4 (1.4-8.1) | .004 | NS | NS | |||||
| Diagnosis group | .04 | NS | NS | ||||||
| AML, MDS | Reference | ||||||||
| MM | 0.3 (0.1-0.9) | ||||||||
| NHL, HD, Waldenstrom | 0.5 (0.2-1.6) | ||||||||
| CLL, CML, ALL | 1.5 (0.4-5.5) | ||||||||
| Hematopoietic cell source | |||||||||
| Marrow vs G-PBMC | NS | 3.1 (1.1-8.8) | .03 | 2.9 (1.3-6.9) | .02 | ||||
Other factors considered, but not found to be significant, were age, previous HCT, time from diagnosis to transplantation, disease risk, and donor sex. NRM indicates nonrelapse mortality; OR, odds ratio; HR, hazard ratio; CI, confidence interval; NS, not significant; CMV, cytomegalovirus; AML, acute myeloid leukemia; MDS, myelodysplastic syndrome; MM, multiple myeloma; NHL, non-Hodgkin lymphoma; HD, Hodgkin disease; CLL, chronic lymphocytic leukemia; CML, chronic myelogenous leukemia; ALL, acute lymphocytic leukemia; G-PBMC, granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cells.
High-risk CMV indicates patient CMV+
Infection. Nonablative conditioning lessened the risk of infection (odds ratio [OR] = 0.2, 95% confidence interval [CI] = 0.1-0.4), whereas high risk of CMV was an adverse risk factor (OR = 3.4, 95% CI = 1.4-8.1). Diagnosis of malignancy was also a risk factor; reduced incidences of infections were seen in patients with multiple myeloma (OR = 0.3, 95% CI = 0.1-0.9) and lymphoma (OR = 0.5, 95% CI = 0.2-1.6), and increased numbers of infections in patients with chronic lymphocytic leukemia, chronic myelogenous leukemia, and acute lymphocytic leukemia (OR = 1.5, 95% CI = 0.4-5.5).
Hepatic toxicity. Nonablative conditioning resulted in less toxicity (OR = 0.3, 95% CI = 0.1-0.6). Marrow as hematopoietic cell source was an independent adverse risk factor (OR = 3.1, 95% CI = 1.1-8.8).
NRM. Nonablative conditioning showed a trend toward lower 1-year NRM (hazard ratio, [HR] = 0.4, 95% CI = 0.2-1.0). High pretransplantation comorbidity scores had an adverse effect on 1-year NRM (HR = 3.3 for scores 1 or 2 and HR = 7.9 for scores ≥ 3). This was mainly due to higher mortality among ablative patients with scores of 1 or more (9 of 16 patients died versus 7 of 32 nonablative patients; HR = 0.3, 95% CI = 0.1-0.7, P = .008). Although 1-year NRM appeared to be lessened among nonablative compared with ablative patients with scores of 0 (5 of 41 nonablative patients died compared with 13 of 57 ablative patients), this difference did not reach statistical significance (HR = 0.5, 95% CI = 0.2-1.3, P = .14).
Marrow as a stem cell source was an adverse risk factor (HR = 2.9, 95% CI = 1.3-6.9) for 1-year NRM. Marrow was used exclusively in the ablative patients. When results in ablative recipients of marrow were compared with those in patients given G-PBMCs, more grades 4 to 5 (life-threatening and lethal) infections were seen (27% versus 8%, P = .03), along with hepatic toxicities, such as sepsis-associated cholestasis or SOS in the context of multiorgan failure, as previously described.38 Marrow recipients also had a higher infectious mortality (HR = 3.0, 95% CI = 1.0-8.5, P = .05), explained in part by the longer duration of neutropenia in this group (18 versus 15 days, P < 10-4).
Discussion
Nonablative regimens for allogeneic HCT have been developed to reduce toxicities associated with conventional, high-dose regimens. This has permitted extending treatment with allogeneic HCT to include older patients and those with comorbidities. Accordingly, current nonablative patients were both significantly older and had significantly greater pretransplantation Charlson comorbidity scores than their counterparts who received conventional transplants. Also, more than one third of them had received preceding high-dose HCT, compared with none of the ablative patients. A previous study had shown poor outcomes after second ablative HCT.39 Even so, current nonablative patients had significantly lower rates of severe toxicities than ablative patients in 7 of 11 systems, including hematologic, gastrointestinal, hemorrhagic, hepatic, infection, metabolic, and pulmonary systems.
In an analysis of a larger cohort of nonablative patients we found slightly worse outcomes after conditioning with Fludarabine + TBI compared with TBI alone.40 That finding was not addressed in the current study, given that patient numbers were too small for sufficient statistical power.
The greatest difference was seen in gastrointestinal toxicities, with no severe mucositis among nonablative patients, as opposed to a 70% incidence among ablative patients. This difference was likely related to the more intense conditioning used in ablative patients, with increased cell death from high doses of radiation and/or alkylating agents1 in tissues having high cell turnover rates, such as the gastrointestinal tract. Additionally, postgrafting MTX might have delayed DNA damage repair, thereby further increasing the severity of mucositis.30,41,42
The breakdown of mucosal barriers in ablative patients might lead to bacterial translocations in immunocompromised hosts,43 and this explained the previously described increased risk of mucositis-associated bacteremias in these patients,22 a finding which was corroborated by the current study. Early infectious events were lower among current nonablative patients, as were infectious deaths, which were the leading cause of NRM. The lesser degree and duration of neutropenia after the nonablative regimen, and the prolonged persistence of host immunity after HCT (mixed T-cell chimerism) might also have contributed to lessened infectious rates, as suggested previously.21,44 Multivariate analysis showed that CMV seropositivity was an adverse risk factor for infection, also consistent with the earlier studies.21,44
Moreover, nonablative patients experienced less hepatic toxicities, and none developed SOS, even though more of them had pretransplantation hepatic comorbidities (11% versus 4%). Absence of SOS in a larger cohort of nonablative patients from our institution was also shown in a previous study.45 By comparison, 13 ablative patients developed SOS, which was fatal in 5 instances. SOS was the second most frequent cause of NRM. This underscores the deleterious effects of cellular cytotoxicity and release of proinflammatory cytokines on hepatocytes caused by ablative regimens.38,46 In addition, posttransplantation MTX has been implicated in hyperbilirubinemia after Cy + TBI regimens30 and both hyperbilirubinemia and SOS after Bu + Cy regimens.47
Pulmonary toxicity, mainly acute lung injury, was less frequent among nonablative patients (3% versus 8%), despite more frequent pretransplantation pulmonary comorbidities (12% versus 7%). Metabolic events were also less frequent, reflecting better renal homeostasis of serum electrolytes. The incidence of renal failure was similar, even though nonablative patients received higher doses of CSP, and more of them had pretransplantation renal comorbidities (10% versus 3%).
Finally, rates of grades 3 to 4 acute GVHD were comparable in the 2 patient groups, a finding which was consistent with results of a previous study focused on GVHD.20 This could, in part, be explained by the early discontinuation of CSP among current nonablative patients (days +35 or +56). More recently, CSP has been continued through days +77 and then +180, and the incidence of grades 3 to 4 acute GVHD has declined.48 Also consistent with the previous study,20 the time of onset of acute GVHD was significantly delayed in nonablative patients (P = .003). Reasons for this delay could include both different conditioning regimens (preserved integrity of the intestinal mucosal barrier and reduced inflammatory cytokine release), and different GVHD prophylaxis strategies (MMF for 28 days and MTX up to day 11). Of note, chronic GVHD was not increased in the nonablative group, despite more frequent (exclusive) use of G-PBMCs. Others have reported less chronic GVHD among nonablative than ablative patients, with stem cell sources in the 2 groups being comparable to the present study.49
The reduction in early RRTs translated into proportional improvements in day-100 and 1-year NRM. Relapse rates and overall survival, considered as competing risk factors, did not confound the analysis, because they were similar in the 2 patient groups (data not shown).
The pretransplantation Charlson comorbidity scores were important risk factors for NRM. Ablative patients with pretransplantation scores of 1 or greater had a 56% 1-year NRM rate, compared with a significantly lower NRM of 22% for nonablative patients. For patients with a score of 0, the 1-year NRM was 22% for ablative and 12% for nonablative patients, a difference which did not reach statistical significance. Others have analyzed the predictive role of pretransplantation evaluation by using different scales with similar results. In the ablative HCT setting, an Eastern Cooperative Oncology Group performance status of more than 0 increased the risk of toxic day-100 mortality 3.7-fold,36 whereas a Karnofsky performance status of 90 or greater decreased the risk of death by a factor of 0.42.50 In the reduced intensity setting, Karnofsky scores of 70 or less decreased the event-free survival by 0.555.51 The Charlson comorbidity index had the advantage of combining organ function assessment into a weighted score, providing perhaps a more comprehensive patient evaluation than the general performance status. As for its predictive capacity, this will need to be validated in prospective studies with larger numbers of patients, to establish more definite guidelines for safely performing HCT with myeloablative versus nonmyeloablative regimens.
Marrow as hematopoietic cell source was an adverse risk factor for hepatic toxicities and NRM among ablative patients. Both longer periods of neutropenia and poorer survival with marrow versus G-PBMCs have already been described in randomized studies.52,53
This study was the first to compare RRT and NRM among nonmyeloablative and myeloablative patients undergoing HCT from HLA-matched related donors. Other investigators have reported their results with reduced-intensity conditioning regimens in patients with hematologic malignancies,54-57 malignant and nonmalignant hematologic disorders,58 and renal cell carcinoma.59 The following paragraphs show a comparison of RRTs and NRM with these regimens; however, comparisons of disease responses and global outcomes could not be made given the heterogeneity of the patients studied.
An MD Anderson Cancer Center study included 39 patients conditioned with fludarabine/melphalan or cladribine/melphalan.54 Patient pretransplantation factors appeared either comparable (median age, 52 years; preceding HCT, 28%; and comorbidities) or higher risk (more advanced diseases) than current ones. Toxicities, graded with use of the Bearman scale, were comparable for mucosa and higher for liver, lung, kidney, heart, and infection, and the day-100 NRM was 33% compared with 3% in the current study.
A report from England included 36 patients conditioned with alemtuzumab (CAMPATH-1H), fludarabine, and melphalan.55 Patients were younger than the current ones with a median age of 41 years, and they had less pretransplantation comorbidities. They experienced more mucositis, but other toxicities were comparable (no SOS). One-year NRM was 11%, with a median follow-up of 9 months.
In a study from Israel, 26 good-risk patients with a median age of 31 years were conditioned with fludarabine, busulfan, and antithymocyte-globulin (ATG).58 Mucosal toxicities, graded with use of the World Health Organization criteria, were comparable, infection and SOS were more frequent, and pulmonary toxicity was less frequent than in the current study. NRM was 15% with 8 months median follow-up.
A report from the University of Arkansas included 25 patients with myeloma conditioned with melphalan, 100 mg/m2.56 Median patient age was 56 years, and patients had received at least one previous autologous HCT. Pneumonitis, seizures, and infections were more frequent than in the current study, whereas liver toxicity was comparable. NRM was 28%, with a median follow-up of 6 months.
A study from the Massachusetts General Hospital described 21 patients conditioned with cyclophosphamide, thymic irradiation, and ATG.57 The median patient age was 44 years, 14% had previous HCT, and patients had fewer comorbidities than those in the current study. Toxicities included engraftment syndrome in 14 patients, cardiac events in 3, and sepsis in 2. NRM was 10% with a median follow-up of 15 months.
A report from the National Institutes of Health included 19 patients with renal cell carcinoma, having a median age of 48 years, conditioned with cyclophosphamide, 120 mg/kg, and fludarabine, 125 mg/kg.59 There were more infectious and pulmonary toxicities than in the current study, whereas gastrointestinal toxicity was similar (no mucositis). NRM was 11% with a median follow-up of 13 months.
In summary, our study showed that nonablative regimens resulted in lower RRTs and NRM than ablative regimens, even though nonablative patients were at higher risk of toxicities because they were older, had higher pretransplantation comorbidities, and more often had received preceding HCT. The Charlson comorbidity score appeared to be a valuable tool for predicting NRM, a finding which should be validated by prospective studies.
Prepublished online as Blood First Edition Paper, May 18, 2004; DOI 10.1182/blood-2004-03-0804.
Supported in part by grants from the National Institutes of Health (CA78902, HL36444, CA18029, CA15704, CA92058, and CA09515).
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Heather Hildebrant, Deborah Bassuk, and Chris Davis for data processing; the research nurses Steve Minor, Mary Hinds, and John Sedgwick; the medical, nursing, and clinical staffs for their dedicated care of the patients; and Bonnie Larson and Helen Crawford for help with manuscript preparation.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal