The kinetics of proliferation of primitive murine bone marrow (BM) cells stimulated either in vitro with growth factors (fetal liver tyrosine kinase ligand 3 [FL], Steel factor [SF], and interleukin-11 [IL-11], or hyper–IL-6) or in vivo by factors active in myeloablated recipients were examined. Cells were first labeled with 5- and 6-carboxyfluorescein diacetate succinimidyl ester (CFSE) and then incubated overnight prior to isolating CFSE+ cells. After 2 more days in culture, more than 90% of the in vivo lymphomyeloid repopulating activity was associated with the most fluorescent CFSE+ cells (ie, cells that had not yet divided), although this accounted for only 25% of the repopulating stem cells measured in the CFSE+ “start” population. After a total of 4 days in culture (1 day later), 15-fold more stem cells were detected (ie, 4-fold more than the day 1 input number), and these had become (and thereafter remained) exclusively associated with cells that had divided at least once in vitro. Flow cytometric analysis of CFSE+ cells recovered from the BM of transplanted mice indicated that these cells proliferated slightly faster (up to 5 divisions completed within 2 days and up to 8 divisions completed within 3 days in vivo versus 5 and 7 divisions, respectively, in vitro). FL, SF, and ligands which activate gp130 are thus efficient stimulators of transplantable stem cell self-renewal divisions in vitro. The accompanying failure of these cells to accumulate rapidly indicates important changes in their engraftment potential independent of accompanying changes in their differentiation status.
Over the last few years, many studies have described culture conditions (including a variety of growth factor combinations) that support the production of large numbers of murine and human hematopoietic progenitors which are capable of further proliferation and terminal differentiation in semisolid media.1 It is now widely appreciated that regardless of their origin, very few if any of these cells have long-term multilineage in vivo engrafting potential. Moreover, a surface phenotype that can be uniquely associated with transplantable hematopoietic stem cell activity, even when the cells are variably stimulated in vitro or in vivo, has not yet been identified. Thus, progress in defining factors that regulate the maintenance or loss of hematopoietic stem cell integrity has had to depend on studies that use quantitative methods to measure changes in cells which can express long-term multilineage repopulating activity in transplanted recipients.2-4 The competitive repopulation unit (CRU) assay3,5,6 is 1 example of such a method, in which stem cells are defined by their ability to sustain circulating levels of at least 105 lymphoid and myeloid cells for more than 4 months. The period of 4 months appears to be of sufficient duration to distinguish stem cells that can remain active for much longer periods from those that may not.2 7 CRU frequencies are determined using the technique of limiting dilution analysis in combination with one of several strategies for ensuring the survival of all of the recipients. This is accomplished independent of whether or not the mice are injected with any CRU in the population being assessed.
In the last 10 years, several cytokines expressed by stromal cells have been cloned. The fact that stromal cells are the presumed source of factors that stimulate stem cell proliferation both in vivo8 and in the long-term culture (LTC) system,9 prompted the investigation of the abilities of these cytokines to stimulate murine stem cell amplification in stroma-free cultures. From such studies, it has been found that Steel factor (SF) or c-kit–ligand in combination with interleukin-6 (IL-6)5 or IL-11, either without10,11 or with fetal liver tyrosine kinase ligand 3 (FL)6 can stimulate a significant, albeit modest, net expansion of murine stem cell numbers in short-term cultures. More recently, evidence of cyclic oscillations in stem cell activity within such cultures has suggested that these cells may transiently (ie, reversibly) lose their engrafting ability.12 The latter observations have complicated the definition of what constitutes a stem cell self-renewal division and have raised new questions about the contribution of proliferation to the stem cell populations obtained from cytokine-stimulated cultures.
In the present study, we used a high-resolution cell tracking procedure to monitor the stem cell activity of cultured cells with different proliferative histories. This procedure relies on the ability of 5- and 6-carboxyfluorescein diacetate succinimidyl ester (CFSE) to stably label a population of cells such that their fluorescence is precisely halved at each successive cell generation.13 By preselection of a starting population with a minimal variation in fluorescence, we have shown that up to 7 successive generations of human hematopoietic cells can be subsequently resolved.14,15 We have used this technology here to analyze the kinetics of murine CRU proliferation in short-term cultures of CRU-enriched suspensions of normal adult mouse bone marrow (BM) cells stimulated with SF, FL, and either IL-11 or hyper-IL-6 (H–IL-6, a recombinant fusion protein of IL-6 and its soluble receptor16). We then compared these results with the initial cell division kinetics seen in vivo when freshly isolated CFSE+cells were transplanted into myeloablated congenic recipients. The results indicate that currently available culture conditions can closely mimic the potent and rapidly mitogenic environment of the myeloablated host. This suggests that other mechanisms may be responsible for the general inability to obtain large amplifications of hematopoietic stem cell populations in vitro.
Materials and methods
Animals
Breeding pairs of mice with the following genetic codes were purchased: C57BL/6J (B6, Ly-5.2, Gpi-1a); B6-Pep3b (Pep3b, Ly-5.1); (B6 × C3H)F1 (B6C3, Ly-5.2/5.2); and (Pep3b × C3)F1 (PepC3, Ly-5.1/5.2) (Jackson Laboratory, Bar Harbor, MN). Breeding pairs of mice also included B6-Gpi-1b(Gpi-1b) and B6-W41/W41 (W41 ) (Dr J. Barker, Jackson Laboratory). All mice were subsequently bred and maintained at the Joint Animal Facility of the British Columbia Cancer Research Center in microisolator units provided with sterilized food, water, and bedding. Irradiated animals were additionally provided with acidified water (pH 3.0).
Isolation of lineage marker− BM cells
Suspensions of mouse femoral and tibial BM cells were depleted of cells expressing CD5, CD11b, CD45RA, Ly-6G, and the antigen recognized by Ter119 using a murine lineage depletion kit (StemSep; StemCell Technologies, Vancouver, BC, Canada) as described.17 In brief, cells were first incubated with 5% normal rat serum in Hanks' balanced salt solution containing 2% fetal calf serum (HF/2, StemCell) on ice, and then biotinylated monoclonal antibodies (mAbs) against the above-named markers were added. After 15 minutes at 4°C, the cells were washed once in HF/2 and resuspended at 5 × 107mL in HF/2. After further addition and mixing with tetrameric antibiotin/antidextran complexes, the cells were incubated for another 15 minutes at 4°C. The magnetic colloid was added, and 15 minutes later the cells were applied to a primed column (StemSep, StemCell Technologies) of an appropriate size placed inside the magnet. Lineage marker− (lin−) BM cells were collected using a peristaltic pump.
CFSE labeling
BM cells (either lin− or unmanipulated) to be labeled with CFSE (Molecular Probes, Eugene, OR) were first centrifuged at 350g for 5 minutes, and the cell pellet was resuspended in phosphate-buffered saline (PBS, StemCell). Samples were set aside for flow cytometric analysis and functional assays prior to CFSE labeling. CFSE was then added to the remainder at a final concentration of 10 or 20 μmol/L. After 10 minutes at 37°C, further dye uptake was prevented by the addition of a quarter volume of cold FCS. Cells were washed once in a serum-free medium (SFM) consisting of Iscove's medium with 1% wt/vol bovine serum albumin, 10 μg/mL insulin, 200 μg/mL iron-saturated transferrin (BIT, StemCell), 40 μg/mL low-density lipoproteins (Sigma Chemicals, St. Louis, MO), 100 μmol/L 2-mercaptoethanol, and 2 mmol/L L-glutamine. Cells were then transferred to 35-mm petri dishes (StemCell), and the following growth factors were added: 100 ng/mL human FL (Immunex Corporation, Seattle, WA); 50 ng/mL murine SF (expressed in COS cells and purified in the Terry Fox Laboratory); and either 100 ng/mL human IL-11 (Genetics Institute, Cambridge, MA) or 20 ng/mL H-IL-616(provided by S. Rose-John, University of Mainz, Mainz, Germany). The CFSE-labeled cells were then cultured overnight at 37°C and harvested from the dishes (including cells obtained by rinsing each dish twice with HF/2).
Labeled cells that had not been depleted of lin+ cells prior to the CFSE labeling and overnight incubation step were centrifuged at 1000g for 20 minutes on a 1.087 g/mL solution (Lympholyte-M; CedarLane Laboratories, Hornby, ON, Canada) to isolate the low-density (LD) fraction. These and the CFSE-labeled lin− cells were then washed once in HF/2 at 600g for 10 minutes and sorted using a fluorescence-activated cell sorter (FACStar Plus; Becton Dickinson, San Jose, CA) equipped with an argon (excitation 488 nm) and a helium-neon (excitation 633 nm) laser using a narrow gate (30-36 channels wide with a 1024 channel log amplifier) for collecting CFSE+ cells (Figure1), as previously described.14This narrow gating interval was chosen slightly to the left of the median CFSE fluorescence to include the majority of cells with low-side and forward light scattering characteristics. In 2 experiments the harvested CFSE-labeled lin− cells were also stained with an R-phycoerythrin–conjugated (R-PE–conjugated) anti–Sca-1 antibody (PharMingen, San Diego, CA) prior to sorting to allow isolation of lin−Sca-1+ CFSE+cells as described.6
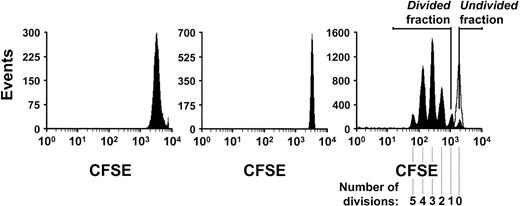
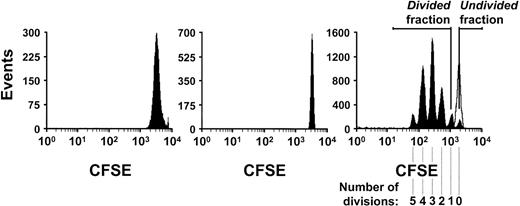
Fluorescence profiles of CFSE-labeled mouse lin− BM cells.
Profiles shown are of cells before (left panel) and after (middle panel) FACS selection of the most brightly labeled subpopulation using a 30 channel-wide gate. The right panel shows the fluorescence profile of the cells recovered another 2 days later, after placing the selected CFSE+ cells (middle panel) into serum-free cultures containing FL, SF, and IL-11 either with (open peak) or without (solid peaks) colcemid. The distribution of cells according to the number of divisions they completed in the 2 days in culture after being labeled is shown by the different sized peaks corresponding to serial 2-fold decreases of fluorescence intensity. The fluorescence intensity of the cells incubated with colcemid confirms the position on a similar plot of the cells that had not divided.
Fluorescence profiles of CFSE-labeled mouse lin− BM cells.
Profiles shown are of cells before (left panel) and after (middle panel) FACS selection of the most brightly labeled subpopulation using a 30 channel-wide gate. The right panel shows the fluorescence profile of the cells recovered another 2 days later, after placing the selected CFSE+ cells (middle panel) into serum-free cultures containing FL, SF, and IL-11 either with (open peak) or without (solid peaks) colcemid. The distribution of cells according to the number of divisions they completed in the 2 days in culture after being labeled is shown by the different sized peaks corresponding to serial 2-fold decreases of fluorescence intensity. The fluorescence intensity of the cells incubated with colcemid confirms the position on a similar plot of the cells that had not divided.
Suspension cultures
Sorted CFSE+ cells were suspended at ≤ 4 × 104 cells/mL in SFM plus FL, SF and IL-11, or H-IL-6 (at the same final concentrations used during the CFSE labeling procedure). Aliquots of 2.5 mL were incubated at 33°C in 35-mm petri dishes for 3 or 4 days and in 50-mL volumes in 150 cm2 tissue culture flasks for 10 days. In each experiment, 0.1 μg/mL of colcemid (Karyomax, Gibco BRL Life Technologies, Grand Island, NY) was added to a separate culture containing 105 cells. The colcemid-treated cells were used to calibrate the fluorescence intensity of cells that did not undergo a single division in each experiment because there is a slow but continuous loss of fluorescence from CFSE-labeled cells over time. The cells to be incubated for 10 days were given new colcemid on day 7. Cells were harvested by removing the suspended cells and then rinsing the dishes (or flasks) twice with Iscove's medium. When present, adherent cells were removed by incubating them for 2-5 minutes in a Trypsin/EDTA (ethylenediaminetetraacetic acid) solution (Gibco BRL), scraping any remaining cells off the bottom of the flask with a rubber policeman (Falcon), and rinsing two times with HF/2. Cells were then pooled, centrifuged at 350g for 5 minutes, resuspended in HF/2 with 1 μg/mL propidium iodide (PI) (Sigma), centrifuged again, and finally resuspended in HF/2 for sorting into fractions of divided and undivided cells as described below.
FACS analysis and isolation of divided and undivided cells
Gates were set using a 1024 channel scale. Undivided cells were collected between a gate set at equal to the median intensity of the colcemid-treated CFSE+ cells and extending to higher fluorescence levels. To minimize cross-contamination, the upper gate for collecting cells that had divided was set 60 channels beneath the lower gate used to define the fraction of undivided cells (ie, approximately twice the channel width originally used to isolate the CFSE+ cells; Figure 1, middle panel). Cells that had divided were collected between this upper channel and channel 350 to provide a gate width such that the maximum fluorescence of unstained BM cells corresponded to the minimal fluorescence level (channel 350) used to identify cells that had divided. Cells that had divided 8 times could then be reliably resolved as distinct from unstained cells. Comparison of viable (trypan blue dye excluding) presort and postsort cell numbers showed that 75%-89% of the presort cells were recovered using these 4 collection gates. For the calculations of numbers of recovered cells, the median recovery value of 83% was used. Sorted cells were collected in HF/2, centrifuged, counted, and injected into irradiated recipients for CRU assays, as indicated.
Assays for colony-forming cells
Numbers of committed progenitors (burst-forming units—erythroid [BFU-E], colony-forming units—granulocyte/macrophage [CFU-MG], CFU-granulocyte, erythroid, macrophage, megakaryocyte [CFU-GEMM]) were determined by plating suitable aliquots of test cells in methylcellulose medium supplemented with 10 ng/mL murine IL-3, 10 ng/mL human IL-6, 50 ng/mL murine SF, and 3 units/mL human erythropoietin (HCC-3434, StemCell) and scoring the corresponding types of colonies (containing more than 30 cells each) present after 12 days of incubation at 37°C.
Competitive repopulation unit assays
Various doses of Pep3b (Ly-5.1) or PepC3 (Ly-5.1/5.2) BM cells were injected intravenously into irradiated congenic Ly-5.2 recipients as previously described.5,6 Recipients were either W41 mice given a sublethal dose of 450 cGy, B6 mice given a lethal dose of 900 cGy, or B6C3 mice given a lethal dose of 950 cGy. In the latter 2 cases, 105normal marrow cells of the same genotype as the recipient were coinjected with the test cells to ensure the survival of all recipients but not to interfere with the detection of engrafted test cells.5 At the subsequent times indicated, cells obtained from tail blood samples were stained first with a combination of biotinylated antibodies (PharMingen) against either myeloid (CD11b, Mac-1 [clone M1/70] and Ly-6G, Gr-1 [clone RB6-8C5]) or lymphoid (CD5, Ly-1 [clone 53-7.3] and CD45R, B220 [clone RA3-6B2]) markers. Cells were then washed twice in HF/2 and finally stained with a fluorescein isothiocyanate–labeled (FITC-labeled) anti-CD45.1 (Ly-5.1, [clone A20]) antibody (prepared in the Terry Fox Laboratory) and streptavidin-conjugated R-PE (Southern Biotechnologies, Birmingham, AL). After 2 washes in HF/2, with 1 μg/mL PI in the last wash, a minimum of 5000 PI−cells were analyzed (FACSort, Becton Dickinson). Positively-stained cells were defined by gates that excluded more than 99.9% of cells stained with an appropriate isotype control antibody. A CRU assay recipient was considered positive only if its Mac-1/Gr-1+ and Ly-1/B220+ populations each contained at least 1% Ly-5.1+ (donor-derived) cells.
In experiment No. 4 (Table 1), various doses of Gpi-1b BM cells were injected intravenously into lethally irradiated (900 cGy) congenic B6-Gpi-1a mice. Tail blood samples in this experiment were divided into 2 aliquots. In 1 aliquot, the red blood cells were first lysed by a brief exposure to NH4Cl. The cells of both aliquots were then centrifuged, frozen, and thawed 3 times, and the 2 Gpi-1 isoenzymes were separated by electrophoresis in cellulose acetate gels (Helena Laboratories, Bearmont, TX), as described earlier.2 In this case a CRU assay recipient was considered positive only if both the red and white blood cell lysates each contained 1% Gpi-1bisoenzyme. Estimates of CRU frequencies were obtained from the proportions of negative mice in each of the various cell dose groups using the method of maximum likelihood18 (L-Calc software, StemCell). Previous experiments have shown that CRU frequencies determined using either Gpi-1 isoenzyme differences or the Ly-5.1/5.2 system to distinguish regenerated donor and recipient granulocytes and lymphocytes are the same.
Results
Kinetics of expansion of mouse BM cells in culture
A total of 8 experiments were performed. In 7 of these, CFSE labeling was used to analyze the proliferative activity of adult mouse BM cells in serum-free cultures containing 100 ng/mL FL, 50 ng/mL SF, and either 100 ng/mL IL-11 or 20 ng/mL H-IL-6. The associated change over time in the distribution of CRU between the fractions of cells that had and had not yet begun to divide under these conditions was also determined. A summary of these experiments is given in Table 1. Cultures were initiated with either LD, lin−, or lin− Sca-1+ BM cells obtained from Pep3b, PepC3, or Gpi mice. In 4 experiments, most of the CFSE+ cells were injected directly into congenic myeloablated mice. These were given 900 or 950 cGy, as with the CRU assays, followed by 3 × 106 LD CFSE+cells or 1.8 × 105 to 1.5 × 106lin− CFSE+ cells per mouse (4 mice per group). This allowed concomitant comparison of the in vivo and in vitro proliferation kinetics of the same starting populations (see below). Thus in most experiments, sufficient cells to examine only a single culture time point were available. Nevertheless, the consistency of the cell count (Table 1) and CRU data (Tables 2 and3) between like experiments, regardless of the cytokine combination used, support their consideration as single groups. The ability of these 2 cytokine combinations to give similar CRU expansions in vitro has also been confirmed in multifactorial design experiments (manuscript in preparation). Because the isolation of an appropriately CFSE-labeled population required an initial overnight culture procedure, this was carried out in the presence of the same combination of growth factors that the cells were subsequently exposed to. Thus, the total period of culture included 1 day prior to the initiation of CFSE cell division tracking.
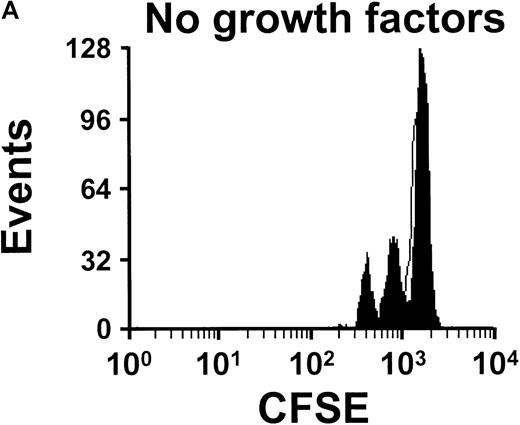
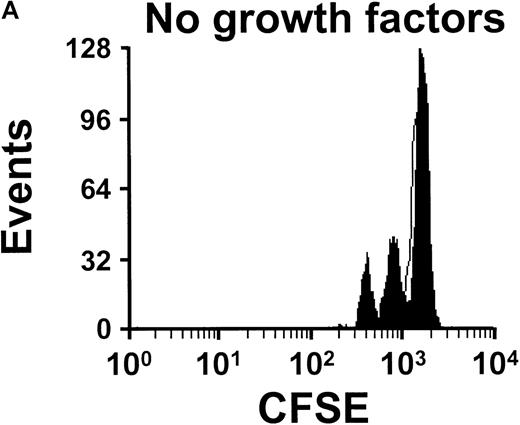
Between the end of the first and third days in culture of lin− cells maintained in SFM with FL, SF, and IL-11, the total number of cells present remained constant (Table 1). Nevertheless, during this interval, analysis of the distribution of cell numbers according to their persisting fluorescence revealed that some cells had already completed up to 5 divisions (Figure 1, right panel). Thus, during this short 2-day period of incubation, there must have been a substantial loss of cells to offset the considerable amplification that would have been anticipated from the extent of proliferative activity indicated by the loss of the CFSE label. Similar analysis of cultures harvested 1 day later showed that within a 3-day tracking period (but 4 days of growth factor stimulation), up to 7 cell cycles were completed by some of the initially labeled cells (Figure2, bottom panel). This was associated with an average 3-fold net expansion in total cell numbers in these cultures. Interestingly, in the absence of added growth factors, we did not detect any cells that had completed more than 3 divisions (Figure2, top panel), and the yield of cells was 4-fold lower. After 9 days of tracking (10 days of culture), most cells had divided more than 7 times, and the proportion classified as still undivided was 0.005% of the total present at that time (Table 1). The total cell number was increased approximately 60-fold. However, this number cannot be readily compared with the total cell expansions measured at earlier times, since the 10-day cultures were initiated with more highly purified stem cell populations (ie, lin−Sca-1+ cells). Accordingly, the expansions observed would be correspondingly increased, (see, for example, the approximately 2-fold greater expansion of total cells already seen after 4 days of culture of lin− versus LD cells; Table 1, experiment No. 8 versus experiment Nos. 2, 5, and 7).
Distribution of cells according to their CFSE fluorescence after being cultured.
Distribution is shown after 3 days of incubation in serum-free culture with (B) or without (A) exogenous growth factors (as shown) in addition to an initial period of overnight culture prior to selection of a LD CFSE+ population. Open peaks show the data for control (undivided) cells incubated under the same conditions but in the presence of colcemid to block cell division. The presence of FL, SF, and H-IL-6 stimulated the cells in this experiment to complete an extra 4 cycles (7 divisions shown in B versus 3 divisions in A).
Distribution of cells according to their CFSE fluorescence after being cultured.
Distribution is shown after 3 days of incubation in serum-free culture with (B) or without (A) exogenous growth factors (as shown) in addition to an initial period of overnight culture prior to selection of a LD CFSE+ population. Open peaks show the data for control (undivided) cells incubated under the same conditions but in the presence of colcemid to block cell division. The presence of FL, SF, and H-IL-6 stimulated the cells in this experiment to complete an extra 4 cycles (7 divisions shown in B versus 3 divisions in A).
Kinetics of recruitment of CRU into division in culture
Cultured cells from the experiments described in Table 1 were also sorted according to their level of fluorescence to isolate those that had not yet divided as a separate population from those that had, as outlined previously. Essentially all of the cells recovered were used to estimate the distribution of CRU between the 2 fractions. The CRU frequency values obtained (and their 95% confidence limits) are shown in Table 2. From these values and the total cell recoveries in each fraction, the total absolute number of CRU in each fraction was then calculated. These values are shown in Table 3. Four of the 5 mice we injected with 300 undivided cells from day 3 cultures (2 days of tracking) showed stable levels of lymphoid and myeloid engraftment from the cultured cells for at least 6 months (at which time the average total repopulation was 18%). In contrast, only 1 of the 20 mice injected with up to 7500 cells that had divided within 3 days of exposure to FL, SF, and IL-11 showed multilineage engraftment (3%). Curiously, although more than 90% of the CRU detected in these cultures had not yet divided, their absolute numbers had decreased 3- to 5-fold relative to the input lin−CFSE+ population (Table 3).
Cultures analyzed 1 day later showed the opposite picture. In these later cultures, all of the repopulating stem cell activity was detected in the fraction of cells which had, by that time, divided. Moreover, the CRU assays of these cells indicated the number of CRU detectable to be 3- to 5-fold higher than the number of CRU in the CFSE+input population (Table 3) and 15-fold higher than the number of CRU detected in the day 3 cultures. The lack of any positive mice among the 12 recipients of cells that had not divided within 4 days in vitro indicates that any persisting quiescent CRU in these cultures must have been present at a frequency of less than 1 per 5 × 104 undivided cells. This upper limit is the same as the measured frequency in the input CFSE+population. Thus the possibility of persisting quiescent CRU in the day 4 cultures cannot be excluded, although it is clear that they would no longer represent a significant proportion of the total CRU present. In vitro assays were performed on small aliquots of cells removed from both fractions of the day 4 cultures in 2 experiments (Nos. 5 and 7). These showed an overall 9-fold expansion of the CFC compartment in both experiments between day 1 and day 4 of culture. These CFC were also detected only among the cells that had divided at least once.
Analysis of cultures that had been maintained for 10 days also showed CRU activity to be present only in the fraction of cells that had divided. However, in these experiments, the total CRU population detected after 10 days was 3- to 5-fold smaller than the input (day 1) value. CRU were not identified among the even smaller population of undivided cells that were still present after 10 days. However, because of the very small number of these cells, it was again possible only to exclude the persistence of CRU in this fraction at or above the frequency of CRU measured for the input lin−Sca-1+ CFSE+ cells.
Secondary transplants of cells from primary recipients of cultured cells
Some of the mice that were injected with cells which had divided (or had not divided) in culture were sacrificed from 4-12 months after transplantation, and CRU assays were performed on the cells that had been regenerated in their BM. As can be seen in Table4, when primary mice had initially been injected with at least 1 cultured CRU, regenerated CRU capable of producing multilineage engraftment in secondary recipients could be consistently demonstrated in the BM of the primary mice, regardless of the time after transplantation when the primary mice were killed. In addition, there was no evidence of reactivation of “silenced” CRU in primary recipients of cultured cells that had divided within 3 days in vitro or of cells that had remained quiescent after 4 to 10 days in vitro.
Kinetics of division of donor cells after transplantation
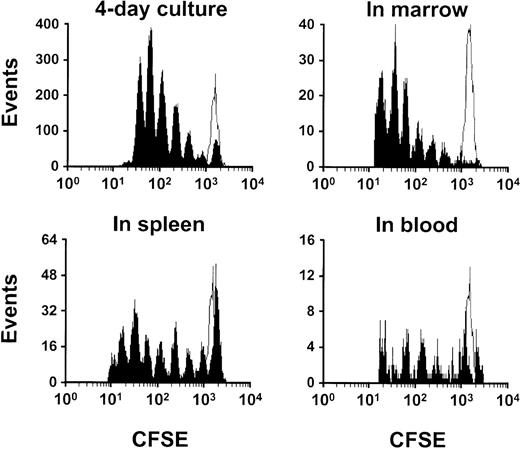
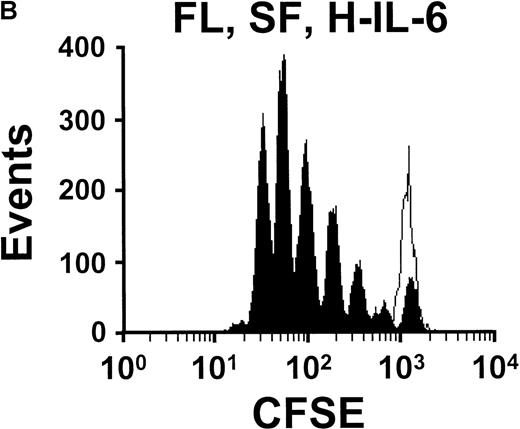
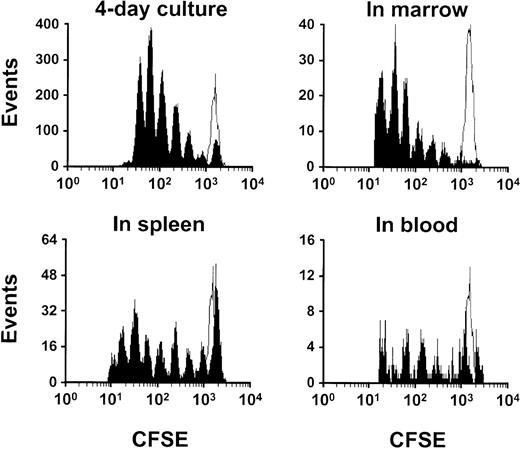
To analyze the rate at which murine BM cells are stimulated to proliferate in vivo when transplanted into myeloablated mice, 1.5-18 × 105 lin− BM cells or 3 × 106 LD BM cells isolated at the end of the overnight CFSE-labeling procedure were injected directly into irradiated (900 or 950 cGy) congenic mice (with at least 4 mice per experiment), and these were then sacrificed 2 or 3 days later. Detectable levels of donor (CFSE+) cells could be found in the BM, spleen, blood, liver, and thymus of mice at both time points, as reported by others.19-21 However, only in BM, blood, and spleen were sufficient numbers of these recovered to permit examination of their in vivo proliferative history. Representative profiles for CFSE+ cells recovered 2 and 3 days after transplantation showed that these cells underwent up to 5 divisions after 2 days in vivo and up to 8 divisions after 3 days (Figures3 and 4). This is, at most, 1 cell generation more than what was seen when aliquots of the same cells were stimulated in vitro with FL, SF, and IL-11 or H-IL-6. Interestingly, in 3 out of 4 evaluable experiments, the proportion of undivided CFSE+ cells recovered from the BM of mice within 2 or 3 days after transplantation was also slightly lower than that seen when aliquots of the same original lin− or LD CFSE+ cells were maintained for the same time in vitro with FL, SF, and IL-11 or H-IL-6 (data not shown).
Comparison of the fluorescence profiles of CFSE+ BM cells after maintenance in culture or in vivo in different tissues.
LD BM cells were labeled overnight, and then CFSE+ cells were analyzed after 3 further days of culture (labeled BM cells cultured with FL, SF, and H-IL-6 growth factors, top left panel) or after 3 days after transplantation of 3 × 106–labeled LD BM cells. Results are shown for cells harvested from the BM (top right panel), spleen (bottom left panel), and blood (bottom right panel) of the injected mice. The distribution of cells among different subpopulations with different proliferative histories is similar for the cells expanding in vitro and in vivo, although there is a slight but obvious shift to the left of the cells obtained from the mice (up to 8 cell divisions in the spleen) compared with the cells maintained in culture for the same period prior to analysis (just a few cells entering the seventh progeny generation). The open peak indicates the fluorescence profile of the same cells maintained in vitro with colcemid to fix the position of the undivided cells.
Comparison of the fluorescence profiles of CFSE+ BM cells after maintenance in culture or in vivo in different tissues.
LD BM cells were labeled overnight, and then CFSE+ cells were analyzed after 3 further days of culture (labeled BM cells cultured with FL, SF, and H-IL-6 growth factors, top left panel) or after 3 days after transplantation of 3 × 106–labeled LD BM cells. Results are shown for cells harvested from the BM (top right panel), spleen (bottom left panel), and blood (bottom right panel) of the injected mice. The distribution of cells among different subpopulations with different proliferative histories is similar for the cells expanding in vitro and in vivo, although there is a slight but obvious shift to the left of the cells obtained from the mice (up to 8 cell divisions in the spleen) compared with the cells maintained in culture for the same period prior to analysis (just a few cells entering the seventh progeny generation). The open peak indicates the fluorescence profile of the same cells maintained in vitro with colcemid to fix the position of the undivided cells.
Comparison of the fluorescence profiles of lin− CFSE+ BM cells after maintenance in culture or in vivo (in the marrow) for 3 and 4 days.
Lin− BM cells were labeled overnight, and then CFSE+ cells were analyzed after being maintained in vitro or for another 2 or 3 days with FL, SF, and IL-11 (left panels) or for 2 or 3 days in vivo (after 1 day in culture) prior to being recovered from the BM of mice injected with cells taken immediately after they were labeled (right panel). The open peak indicates the fluorescence profile of cells maintained in vitro with colcemid to block cell division and analyzed at the same time. In the top right graph, the recipient was injected with 1.8 × 105lin− CFSE+ cells, and in the bottom right graph the recipient was injected with 1.5 × 106 lin−CFSE+ cells. The 2 right-hand graphs show the results obtained from 1 of 2 mice sacrificed at each time point. The results show the same slight shift to the left in the profiles obtained for the transplanted cells as seen in Figure 3.
Comparison of the fluorescence profiles of lin− CFSE+ BM cells after maintenance in culture or in vivo (in the marrow) for 3 and 4 days.
Lin− BM cells were labeled overnight, and then CFSE+ cells were analyzed after being maintained in vitro or for another 2 or 3 days with FL, SF, and IL-11 (left panels) or for 2 or 3 days in vivo (after 1 day in culture) prior to being recovered from the BM of mice injected with cells taken immediately after they were labeled (right panel). The open peak indicates the fluorescence profile of cells maintained in vitro with colcemid to block cell division and analyzed at the same time. In the top right graph, the recipient was injected with 1.8 × 105lin− CFSE+ cells, and in the bottom right graph the recipient was injected with 1.5 × 106 lin−CFSE+ cells. The 2 right-hand graphs show the results obtained from 1 of 2 mice sacrificed at each time point. The results show the same slight shift to the left in the profiles obtained for the transplanted cells as seen in Figure 3.
Discussion
In the present studies we used a high-resolution tracking procedure to document the proliferative history of CFSE-labeled mouse BM cells stimulated in short-term cultures with FL, SF, and IL-11 or H-IL-6. The results provide new evidence that stem cells with long-term lymphomyeloid reconstituting activity do not complete a first division for at least 3 days in vitro, even under conditions that will stimulate their subsequent proliferation without loss of their original stem cell integrity. Alternative evidence that this is likely to be the case has been inferred from the direct observation or FACS-based detection of the cell cycle progression of individual cells in cultures of highly enriched stem cell populations.22-27 Delayed effects of cell cycle–active agents on stimulated populations of primitive hematopoietic cells have also been observed, 28-31 and the inability to retrovirally mark hematopoietic stem cells, unless they are exposed to active virus after more than 24 hours in culture,32 further supports this kinetic behavior of quiescent stem cells following their exposure to growth factor combinations with mitogenic activity.
The present studies also provide indirect evidence that hematopoietic stem cells can be stimulated to execute self-renewal divisions in vitro. We observed that after 4 days of exposure to FL, SF, and IL-11 or H-IL-6, all of the detected stem cell activity became associated with cells that had completed at least 1 division. Moreover, this association did not alter during the following week of culture. Such findings confirm and extend previous observations of modest net increases in murine stem cell numbers in these cultures.6Recently, analogous results from studies of transplantable CFSE-labeled human stem cells stimulated in vitro have been reported.15,33 Taken together, these findings suggest that failure to obtain larger expansions of stem cells in vitro is not due to inadequate mitogenic stimulation within a relatively short period. Our data, in fact, indicate that at least 90% of the CRU detectable after 4 days in vitro are the progeny of cells that have undergone at least 1 division during the previous 3 days and most likely during the previous 24 hours. These findings are further reinforced by the results of secondary transplant experiments. These confirmed a lack of stem cells in cultured cell populations that did not regenerate mature cells in primary mice. They also showed that CRU proliferation in vitro does not reduce their subsequent in vivo self-renewal capacity, as reported previously.6
Proliferation of primitive hematopoietic cells has been previously studied in cultures of cells with membrane-labeling fluorescent dyes such as PKH-2,34,35 PKH-26,36-38and PKH-67.39 All of these labels confer a measurable and relatively stable level of fluorescence on the cells initially stained, and this has allowed the detection of a significantly decreased level of fluorescence to identify populations that have subsequently proliferated extensively. Conversely, maintenance of a highly fluorescent phenotype by PKH-2– or PKH-26–labeled cells has been used to identify cells that have divided little or not at all. However, the heterogeneity in staining intensity obtained with these dyes does not allow small numbers of divisions to be resolved. The high-precision tracking possible with CFSE-labeling, particularly as modified by Nordon et al14 obviates this problem and thus allows definitive and unique information about the initial proliferative behavior of functionally defined stem cells to be obtained. For example, a predominance of G1/G0cells in the PKH-26bright population recovered from the marrow of mice injected 48 hours previously with PKH-26-labeled R/O or FR25lin− cells20 does not preclude the possibility that some of these cells may have already divided during the previous 48 hours after transplantation, as suggested by the data presented here.
Our analysis of the total CFSE+ cell population recovered from the BM of myeloablated recipients indicated that the injected cells, as a whole, began to proliferate only slightly sooner than was achieved in vitro through activation of the flt-3, c-kit, and gp130 receptors by soluble ligand binding. Thus it may be predicted that most of the long-term repopulating stem cells, which are highly enriched in the FR25lin− population but still represent a minor subset, would not begin to divide within the first 2 days after transplantation, in contrast to other FR25lin− cells. Further investigation of this question must await functional studies of the undivided and divided fractions of in vivo harvested donor-derived cells.
It is now clear, however, that CRU numbers can be amplified many-fold over prolonged periods in vivo,6,40 whereas a comparable net expansion in vitro has not yet been reported. Although modest increases in CRU numbers can be documented,6 these must now be reconciled with the large and rapid fluctuations in their numbers that are detectable just before and immediately following completion of a first division, as noted in the present study (Table 3) and suggested by others.12 The magnitude of these fluctuations points to the operation of a cell cycle and/or time-dependent mechanism that may reversibly affect the ability of stem cells to either home into the extravascular space of the marrow or to respond to stimuli that recruit them to proliferate in this tissue. Such a model is further supported by evidence that the exit of human CD34+ cells from G0/G1 is also associated with a decrease in their ability to repopulate irradiated nonobese diabetic severe combined immunodeficiency (NOD/SCID) mice.25 Conversely, using the same xenotransplant model, Peled et al41 showed that up-regulation of CXCR4 expression on human CD34+ cells following their exposure to SF and IL-6 increased the effective repopulating activity of these cells within a time frame too short to be readily accounted for by stem cell divisions. Thus transplantability and control of the “undifferentiated” status of cells with hematopoietic stem cell potential may be subject to independent regulation. Such a possibility underscores the need for definitive molecular indicators of each of these functions so that their degree of overlap and extrinsic control can be further delineated.
Acknowledgments
We thank C. Miller (StemCell Technologies, Vancouver, BC, Canada) and T. Holyoake (University of Glasgow, Glasgow, Scotland) for critical discussions; J. Barker (Jackson Laboratory, Bar Harbor, MN) for breeding pairs of B6-Gpi-1b and B6-W41/W41 mice; S. Rose-John (University of Mainz, Mainz, Germany) for H-IL-6; M. Sinclaire and N. Raymond for technical assistance; G. Cameron, G. Thornbury, and R. Zapf for operating the FACS; Y. Yang for typing the manuscript; and Cangene, Genetics Institute, Immunex, and StemCell Technologies for reagent gifts.
Supported by the National Cancer Institute of Canada (NCIC), with funds from the Terry Fox Run (Toronto, ON, Canada), and by grant PO1-HL55435 from the National Institutes of Health (Bethesda, MD).
J. A. holds a studentship from the Natural Sciences and Engineering Research Council of Canada (Ottawa, ON, Canada) and a scholarship from the Science Council of British Columbia (Vancouver, BC, Canada). C. E. is a Terry Fox Research Scientist of the NCIC.
Reprints:Connie J. Eaves, Terry Fox Laboratory, 601 West 10th Avenue, Vancouver, BC, V5Z 1L3, Canada; e-mail:connie@terryfox.ubc.ca.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.