Abstract
Immunomodulatory agents (IMiDs) are a cornerstone of treatment for patients with multiple myeloma. IMiDs are used in therapeutic combinations at all stages of disease and are approved as a single-agent maintenance treatment after autologous stem cell transplantation. However, patients become resistant to ongoing therapy over time and inevitably relapse. It is only in the last decade that the mechanism of IMiD action has been elucidated; through binding to the cereblon component of the CRL4CRBN E3 ubiquitin ligase, a set of neosubstrates is designated for degradation by the proteasome. In myeloma cells, this includes the zinc-finger B-cell transcription factors Ikaros and Aiolos, which, in turn, lead to decreased levels of IRF4 and c-MYC and cell death. As our knowledge of IMiD mechanism of action has advanced, the ability to study resistance mechanisms has also developed. This review explores the existing work on IMiD resistance and proposes areas of future research that may advance our understanding and management of this common clinical condition.
Background
Outcomes for patients with multiple myeloma (MM) have improved significantly over the last 20 years, driven by the development of novel therapeutics (eg, immunomodulatory agents [IMiDs], proteasome inhibitors, and anti-CD38 monoclonal antibodies), autologous stem cell transplantation, and enhanced supportive care.1 Most patients respond well to initial therapy, but over time their disease will relapse, and a new line of treatment will be required. Eventually, a treatment refractory state will evolve, driven by drug-resistant subclones and protection provided by the malignant bone marrow (BM) niche.2-4
IMiDs are a critical component of therapeutic combinations for all stages of the disease and are also used as a single-agent maintenance therapy after autologous stem cell transplantation. At diagnosis, most patients are sensitive to IMiD-based combination therapy; however, about 5% are refractory and form an important group with difficult-to-manage disease.5 Patients who are initially sensitive eventually acquire resistance, and IMiD refractory states are associated with shorter progression-free survival (PFS) and overall survival (OS) in response to subsequent therapies.6
Thalidomide, the first-in-class IMiD, was synthesized in the 1950s but was quickly withdrawn because of reports of severe congenital anomalies.7 In the years that followed, thalidomide was found to have anti-inflammatory and antiangiogenic properties and was used to treat inflammatory skin disorders such as lepromatous leprosy.7 In the 1990s, 5 patients with end-stage MM were treated with thalidomide, and success in this setting prompted further trials.7,8 Newer generation compounds were developed in the 2000s, including lenalidomide and then pomalidomide, which share common phthalimide and glutarimide moieties but have specific differences in the glutarimide ring.7
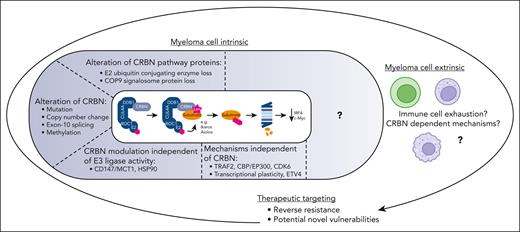
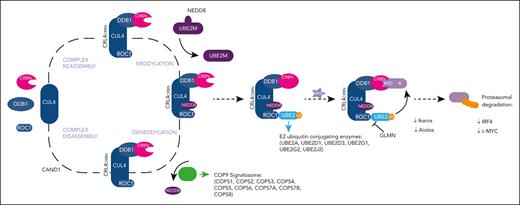
Despite this demonstrated efficacy, the molecular target of IMiDs and its mechanism of action as an antimyeloma agent were not uncovered until the 2010s.9,10 Work from several groups showed that IMiD activity against myeloma cells results from its ability to bind to a specific tritryptophan pocket of cereblon (CRBN), a substrate receptor of the CRL4CRBN E3 ubiquitin ligase. Through acting as a molecular glue, a different set of proteins is designated for ubiquitination and subsequent degradation by the proteasome. In myeloma cells, the critical neosubstrates are the B-cell zinc-finger transcription factors Ikaros and Aiolos.10-12 The rapid degradation of Ikaros and Aiolos is associated with decreased expression of interferon regulatory factor 4 (IRF4) and c-MYC, leading to growth inhibition and cell death.13 Both Ikaros and Aiolos belong to the Cys2-His2 zinc-finger protein family,14 and the presence of this motif has also been found in more recently identified IMiD neosubstrates, such as zinc-finger protein 91 (ZFP91).15 The CRL4CRBN E3 ubiquitin ligase is maintained by the COP9 signalosome, a multiprotein complex that regulates cullin ring ubiquitin ligases by removing their activator NEDD816 (Figure 1). In addition to its well-established role as a ubiquitin ligase for protein degradation, CRBN may also have other functions, such as promoting maturation of proteins17 and acting as a cochaperone for heat shock protein 90 (HSP90).18
Components of the CRL4CRBN E3 ubiquitin ligase complex, COP9 signalosome and Ikaros/Aiolos/IRF4 axis. Adapted from Jones et al.89http://creativecommons.org/licenses/by/4.0/
Components of the CRL4CRBN E3 ubiquitin ligase complex, COP9 signalosome and Ikaros/Aiolos/IRF4 axis. Adapted from Jones et al.89http://creativecommons.org/licenses/by/4.0/
Direct IMiD-induced myeloma cell toxicity is linked to a number of mechanisms, in addition to decreased IRF4 and c-MYC, including the inhibition of nuclear factor κB signaling, activation of caspases, increased expression of proapoptotic factors, decreased expression of antiapoptotic factors, and disruption of the phosphatidylinositol 3-kinase/protein kinase B signaling pathway.7 IMiDs also affect the interaction of myeloma cells with several components of the BM niche and have broad immunomodulatory effects, including increased T-cell priming, increased activity of natural killer (NK) and NK T cells, and inhibition of T regulatory cells.7,19 IMiD treatment leads to upregulation of interleukin-2 (IL-2) in T cells and interferon gamma (IFN-γ) in NK cells, and this is associated with the degradation of Ikaros and Aiolos, which are thought to act as transcriptional repressors in this cellular context.20 The action of IL-2 and IFN-γ in the microenvironment leads to further immune cell expansion and immune-mediated myeloma cell destruction.20 IMiDs also have broad antiangiogenesis effects associated with the inhibition of fibroblast growth factor 2.7
Further advancements in understanding the mechanism of action of CRBN binders led to the development of next generation cereblon E3 ligase modulators (CELMoDs), for example, iberdomide (CC-220) and mezigdomide (CC-92480). CELMoDs are larger molecules with a higher CRBN-binding affinity21 and a different spectrum of neosubstrate degradation (Table 1), compared with IMiDs. Patients who have become refractory to an earlier generation IMiD may respond to a later generation IMiD or CELMoD. For example, approximately one-third of patients who have become resistant to lenalidomide therapy still respond to pomalidomide.22 A recent analysis of the OPTIMISMM trial showed that in patients at first relapse who had previously received lenalidomide, the combination of pomalidomide, bortezomib, and dexamethasone led to a significantly prolonged PFS compared with bortezomib and dexamethasone alone (median 22.0 vs 13.1 months; P = .03).23 Patients refractory to lenalidomide and pomalidomide can also respond to iberdomide and mezigdomide24-26; a phase 1/2 trial of iberdomide in nearly 200 patients who had received ≥2 prior lines of therapy, including lenalidomide or pomalidomide and a proteasome inhibitor, found an overall response rate of ∼30%.27
The reasons underpinning the response to sequential generations of IMiDs may relate to several factors. Over time, a reduction in the level of CRBN in malignant plasma cells commonly occurs28,29; longitudinal analysis of BM biopsy samples frequently shows decreased CRBN mRNA and protein levels in patients who acquire lenalidomide resistance.29 A CRBN binder with a higher binding affinity may be able to better "utilize" the remaining CRBN to degrade neosubstrates and overcome resistance in the low CRBN state.21 Importantly, it is the function of IMiDs as molecular glues that enables this phenomenon; 1 IMiD molecule binds to 1 CRBN molecule, but this can lead to the degradation of multiple neosubstrate molecules, amplifying the effect of very low levels of CRBN. In addition, CELMoDs are larger in size, and this may increase physical interactions with CRBN.21 Futhermore, each CRBN binder may exhibit certain differences in the neosubstrate profile.30 For example, lenalidomide is the only IMiD that has clinical benefits for the treatment of deletion 5q myelodysplastic syndrome.31 Casein kinase I α (CK1α) is a unique neosubstrate of lenalidomide, and in the CK1α haploinsufficient state present in deletion 5q myelodysplastic syndrome, further CRBN-mediated degradation of CK1α leads to cell death because of the activation of p53.31
IMiDs are increasingly being explored in other hematological cancers and show promising clinical efficacy in chronic lymphocytic leukemia and several non-Hodgkin lymphomas.32,33 The mechanism of action of IMiDs has also been exploited to develop additional molecular glues and CRBN-directed heterobifunctional proteolysis-targeting chimeras (PROTACs), which are compounds with an IMiD-like domain that binds to CRBN and a domain that binds to a target protein, leading to its degradation via the ubiquitin-proteasome system.34 Understanding mechanisms of resistance is therefore increasingly important.
Mechanisms of resistance
Concepts of resistance
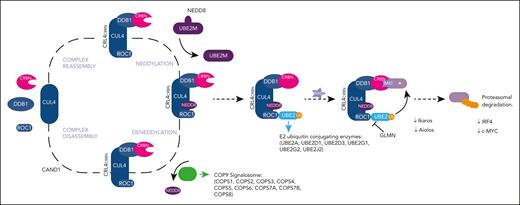
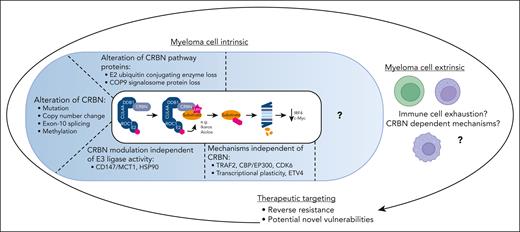
Conceptually, IMiD resistance can be divided into factors intrinsic to the myeloma cell and extrinsic factors in the tumor microenvironment (Figure 2). Low CRBN protein levels are commonly, but not universally, observed in the resistant setting, including certain cell line models,35 mouse models,36 and samples from patients.29 Decreased CRBN may be associated with genetic alteration, but alternative drivers of the low CRBN state and other mechanisms of resistance are currently not well understood. Given the mechanism of IMiD action, alterations in the CRL4CRBN E3 ubiquitin ligase complex, the COP9 signalosome, and the Ikaros/Aiolos/IRF4 axis are likely targets for the generation of resistance.2 Indeed, genome-wide CRISPR-Cas9 screens have identified CRBN and the proteins that directly regulate its expression and function as involved in IMiD resistance.37,38 Similarly, a genome-wide CRISPR study exploring resistance to PROTACs operating via CRBN found that the top individual loss-of-function events were those that disrupted the degradation machinery itself.39
Concepts of IMiD resistance. IMiD resistance can be divided into myeloma cell–intrinsic factors and myeloma cell–extrinsic factors. Myeloma cell–intrinsic factors include genetic alteration of CRBN (including mutations, copy number changes and differential splicing), alterations to the E2 ubiquitin conjugating enzymes and the COP9 signalosome, and transcriptional plasticity. There are also changes in the tumor microenvironment, for example, immune cell exhaustion. To target IMiD resistance we can consider reversing resistance or exploiting potential vulnerabilities that may develop alongside the generation of resistance. Image created using biorender.com.
Concepts of IMiD resistance. IMiD resistance can be divided into myeloma cell–intrinsic factors and myeloma cell–extrinsic factors. Myeloma cell–intrinsic factors include genetic alteration of CRBN (including mutations, copy number changes and differential splicing), alterations to the E2 ubiquitin conjugating enzymes and the COP9 signalosome, and transcriptional plasticity. There are also changes in the tumor microenvironment, for example, immune cell exhaustion. To target IMiD resistance we can consider reversing resistance or exploiting potential vulnerabilities that may develop alongside the generation of resistance. Image created using biorender.com.
Resistance may also be generated by the changes in the tumor microenvironment and could include failure of the usual function of IMiDs on immune cells, including T cells and NK cells.20
Myeloma cell–intrinsic mechanisms of resistance
Resistance associated with the alteration of CRBN
Point mutations in CRBN are rare in patients with newly diagnosed MM (<1%),40 but this increases to ∼12% in patients treated with IMiDs.41 Select CRBN mutations found in patients have been modeled in the OCI-MY5 cell line (characterized by low expression of CRBN and IMiD resistance).41 OCI-MY5 cells transduced with wild-type CRBN gained lenalidomide sensitivity, whereas those transduced with vectors containing CRBN mutants or empty vector remained resistant.41,42
A recent study performed whole-genome sequencing and RNA sequencing on samples from patients with newly diagnosed, lenalidomide-refractory and pomalidomide-refractory MM to further explore the incidence of CRBN alteration, specifically in the IMiD refractory setting.43 Genetic alteration of CRBN occurred in nearly 30% of the patients with relapsed/refractory MM, if mutations, copy loss/structural variations, and high exon-10 spliced CRBN transcripts were considered together.43 The splice variant lacking exon-10 is translated into a stable protein that can still bind to DDB1/cullin 4A (CUL4A) but can no longer interact with IMiDs. In myeloma cell line models, high exon-10 splicing of CRBN was sufficient to stop lenalidomide cytotoxicity.44 These genetic changes were associated with inferior outcomes for patients after treatment with pomalidomide-based regimes in those already refractory to lenalidomide.43
CRBN expression may also be controlled through epigenetic mechanisms. For example, deep bisulfite sequencing to evaluate CpG methylation at the single DNA molecule resolution was used to assess the role of promoter methylation in drug resistance in primary MM tumor samples.45 High methylation in the CRBN promoter–flanking region was found in 18 out of 27 samples from patients with IMiD resistance but in none of the matched control samples.45
There are also several cell line models of acquired IMiD resistance that show decreased CRBN protein expression of unclear etiology. Understanding how resistance is generated in these cases is important to allow identification of new mechanisms of resistance that can then be evaluated in patients. It is sometimes difficult to assess whether changes identified in the IMiD-resistant state are the cause or the effect of IMiD resistance, but either way they may represent useful targets. For example, acquired lenalidomide and pomalidomide resistant cell lines were created from 2 initially IMiD-sensitive cell lines (OPM2 and NCI-H929), by taking cells and culturing them with low doses of IMiDs over a period of several weeks.46 Both cell lines had low CRBN levels, genome-wide increases in DNA methylation, reductions in chromatin accessibility and gene expression, and SMAD3 was identified as a commonly downregulated gene.46 The team showed that a combination of 5-azacytidine and the EZH2 inhibitor EPZ-6438 restored the observed accessibility changes as well as SMAD3 expression and resensitized the resistant cells to IMiDs.46 There is also early data supporting the presence of synergy between EZH2 inhibitors and pomalidomide in both in vitro and in vivo models.47 Recent work from our laboratory has shown that cell line models of acquired IMiD and CELMoD resistance (including MM1s and NCI-H929 cells with acquired resistance to lenalidomide, pomalidomide and iberdomide), all of which represent a low CRBN state, had common changes in the protein components of lipid synthesis pathways on mass spectrometry analysis, and these alterations may represent targetable vulnerabilities.48
A reduction in functional CRBN is also important because substrates have been shown to compete for access to it.30 A zinc-finger protein (ZNF692) was mutated such that it could interact with CRBN but could not be degraded. This construct was expressed in the IMiD-sensitive MM1s cell line and resistance to lenalidomide was induced.30 Conversely, decreased levels of nonessential substrates were shown to sensitize cells to lenalidomide.30 Therefore, in a given cell type, the efficacy of an IMiD/CELMoD may be influenced by both the level of CRBN expression and levels of alternative substrates.30
Resistance associated with the alteration of CRBN pathway proteins
In samples from patients, point mutations41,42 and copy number loss49,50 have been observed in CRBN pathway members. When compared with patients with newly diagnosed MM, those with IMiD-resistant disease show an increase in mutations in IKZF1, IKZF3, IRF4, and CUL4B (∼10%).41,42 Four IKZF1 mutations observed in patients have been modeled, and only mutations affecting the IZKF1 degron sequence were found to induce IMiD resistance.42 A CUL4B knockout has been performed in IMiD-sensitive L363 cells, and the knockout was more resistant to lenalidomide treatment, as confirmed by a clonal competition assay.42 Copy number loss is also likely to be important; the 2q37 chromosome region contains the COP9 signalosome members COPS7B and COPS8 and copy loss here is significantly enriched between newly diagnosed patients (incidence 5.5%), patients with lenalidomide refractory disease (incidence 10%), and lenalidomide-then-pomalidomide–refractory states (incidence 16.4%).49
Modulators of the CRBN and Ikaros/Aiolos/IRF4 axis may also be involved in the generation of resistance. For example, runt-related transcription factor 1 (RUNX1) and RUNX3 compete with CRBN to bind Ikaros and Aiolos, thus preventing their degradation.51 Inhibition of RUNX1/3 via genetic manipulation or small molecule led to the reversal of lenalidomide resistance in both myeloma cell lines and samples from patients.51
Translocations involving the immunoglobulin λ (IgL) locus confer poor prognosis, and it has been shown that Ikaros binds to the IgL enhancer at high levels.52 Data from the Multiple Myeloma Research Foundation (MMRF) CoMMpass study showed that patients with t(IgL) had poor PFS and OS regardless of whether they received IMiD-containing therapy or not, in contrast with patients with non-t(IgL) who derived a clear benefit. These data suggest t(IgL) can lead to IMiD resistance, perhaps because the high level of bound Ikaros makes it relatively insensitive to IMiD-based depletion of Ikaros.52
Resistance associated with CRBN but independent of CRL4CRBN E3 ubiquitin ligase activity
CRBN has been suggested to have important functions independent from its role in protein degradation. CRBN has been shown to promote the maturation of CD147 and MCT1 proteins, allowing for the formation of an active CD147-MCT1 transmembrane complex, which promotes angiogenesis, proliferation, invasion, and lactate export.17 IMiDs outcompete CRBN binding to CD147 and MCT1, leading to mislocalization and destabilization of the complex.17 IMiD-sensitive MM cells lose CD147 and MCT1 expression, whereas IMiD-resistant cells retain their expression.17 A combination of cell-surface proteomics and functional CRBN interactome screens has shown that CRBN determines the chaperone activity of HSP90 by antagonizing activator of HSP90 ATPase activity 1 (AHA1), and IMiDs disrupt the interaction of CRBN with HSP90.18 One of the possible clients of the CRBN–-AHA1-HSP90 axis is the amino acid transporter LAT1/CD98hc, which becomes destabilized and inactivated upon IMiD treatment.18 Persistence of LAT1/CD98hc may be associated with resistance to IMiD treatment.18
Resistance independent of CRBN and its related proteins
Although low CRBN expression often correlates with resistance, some samples from patients and MM cell lines show resistance to IMiDs despite normal CRBN levels and without currently identified abnormalities in CRBN or its associated proteins.2 Resistance may be caused by the activation of alternative signaling pathways that could upregulate IRF4, c-MYC, or other prosurvival pathways.2
A genome-wide knockout CRISPR-Cas9 screen in the IMiD-sensitive cell line MM1s was performed in cells cultured with pomalidomide to allow for the identification of genes that, when inactivated, diminish the effects of IMiDs.37 Single guide RNAs targeting tumor necrosis factor receptor–associated factor 2 (TRAF2) were enriched after IMiD selection, and TRAF2 knockout MM1s showed significant resistance to lenalidomide and pomalidomide treatment.53TRAF2 knockout had no effect on CRBN expression, and there was persistent Ikaros and Aiolos degradation and reduction of IRF4 in response to IMiD treatment.53TRAF2 knockout cells showed strong activation of the noncanonical nuclear factor κB pathway and extracellular signal–regulated kinase pathway, and in vitro and in vivo murine xenograft studies showed that MEK inhibitor AZD6244 could overcome IMiDs resistance in TRAF2 knockout MM cells.53
Further examples of IMiD resistance without low CRBN levels come from acquired IMiD-resistant cell line models. The XG1 myeloma cell line was cultured with low doses of lenalidomide to create the lenalidomide resistant line XG1LenRes (which displayed no genetic changes in CRBN).54 XG1LenRes showed constitutive STAT3 activation, and selective STAT3 inhibition led to resensitization of the cell line to lenalidomide.54 The XG1LenRes cells also expressed a truncated IRF4 that was not downregulated by lenalidomide. The IRF4/c-MYC axis was targeted with a selective inhibitor of CBP/EP300 (which directly suppresses IRF4), and this compound restored lenalidomide response in the XG1LenRes cells.54
Transcriptional plasticity, with the expression of extralineage transcription factors, may also be important in the development of IMiD resistance. Resistance to IMiDs and loss of c-MYC repression can occur despite continued Ikaros and Aiolos degradation.55 Ikaros, BRD4, lysine acetyl transferase P300, and the mediator subunit MED1 have been shown to colocalize within the MM genome.55 In the IMiD-sensitive cell line MM1s, exposure to lenalidomide reduced Ikaros, BRD4, P300, and MED1 at enhancer loci. However, in the resistant cell line RPMI8226, Ikaros was displaced, but BRD4, P300, and MED1 were retained.55 A computational analysis showed strong enrichment of the GGAA motif, which is recognized by the erythroblast transformation specific (ETS) family of transcription factors, at enhancers co-occupied by Ikaros and BRD4.55 The ETS family transcription factor ETV4 was expressed in IMiD-resistant but not -sensitive cell lines.55 Lenalidomide treatment induced global depletion of Ikaros but not ETV4 at BRD4-occupied enhancers in resistant cell lines.55 Knockout of ETV4 in RPMI8226 cells sensitized them to lenalidomide, with c-MYC downregulation and cell death.55
Although cell line models have provided useful insights into resistance generation, evaluation of samples from patient is critical. Proteome analysis is particularly key because of the effect of IMiDs on protein degradation, but there are limited proteomic data available to date. Proteomic and phosphoproteomic analyses were performed in 5 paired samples of patients: pretreatment and IMiD relapse.56 These patients did not show significantly reduced CRBN levels at relapse but did show an increase in cyclin-dependent kinase 6 (CDK6).56 Overexpression of CDK6 in IMiD-sensitive myeloma cell lines led to reduced IMiD sensitivity, and CDK6 inhibition (by palbociclib or degradation via a proteolysis-targeting chimera) was found to be highly synergistic with IMiDs in vitro and in an MM1s xenograft mouse model.56
Myeloma cell–extrinsic mechanisms of resistance
IMiDs and CELMoDs lead to profound changes in the composition and activity of immune cells in the microenvironment, but resistance in this context needs further study. IMiD treatment leads to increased T-cell proliferation, IL-2 and IFN-γ secretion, and NK and NK T-cell activation.20 IMiDs also inhibit IL-6 production from monocytes and macrophages.20 However, IMiDs can also lead to inhibitory immune responses, including increased T regulatory cells and myeloid-derived suppressor cells.20 This may play a role in immune escape; however, some studies reporting changes in these immune populations are in the context of combination treatment with IMiD and the immunosuppressive steroid dexamethasone.20 A loss of IMiD-induced IFN response in resistant myeloma cells may also contribute to immune escape; genes with a key role in modulating IFN response (including NLRP4 and NFKBIZ) were differentially expressed in samples from patients who had developed resistance to lenalidomide compared with those who remained sensitive.57
Mass cytometry before and after treatment with the CELMoD iberdomide has been used to evaluate T-, B-, and NK-cell subpopulations in the BM aspirates of 99 patients with heavy pretreatment.58 Treatment with iberdomide was associated with significant increases in effector T and NK cells, demonstrating innate and adaptive immune enhancement.58 In patients relapsing after prior therapy (including IMiDs), an increase in the markers of immune cell exhaustion has been identified, including upregulation of programmed cell death protein 1 (PD-1) on the surface of T cells.20,59,60 These changes suggest an element of IMiD resistance may be related to immune cell exhaustion.20
One mechanism to overcome the phenomenon of exhaustion in the clinic is the addition of the anti-CD38 antibody daratumumab, which enhances the adaptive immune response and contributes to enhanced efficacy in combination with IMiDs.61,62 For example, the combination of daratumumab, lenalidomide, and dexamethasone led to an increased proportion of effector memory T cells, reduced immunosuppressive T regulatory cells, and increased T-cell repertoire clonality compared with those of lenalidomide and dexamethasone alone.63 These combinations are now used widely in the clinic. Changes within key immune cell populations have been assessed in the context of treatment with pomalidomide, daratumumab, and low dose dexamethasone.64 Although the effect of the individual agents is difficult to differentiate in the absence of single-agent treatment arms, there appeared to be a reduction in the number of absolute NK and B cells, in keeping with the reported mechanism of action of daratumumab.64 In contrast, the proportion of activated and proliferating NK cells and CD8+ T cells increased with treatment, which correlated with the pomalidomide dosing schedule.64 Similar changes were observed in patients with lenalidomide-refractory conditions, highlighting the importance of combining distinct therapeutic modalities in the treatment of relapsed MM but, also, the potential use of later generation IMiD/CELMoDs among patients who are refractory to earlier generation compounds.64
An alternative approach is to alter the function of checkpoints that regulate T-cell function. PD-1 is an immunosuppressive protein critical to regulating immune system responses, and its ligand, PD-L1, is overexpressed on myeloma cells, leading to reduced proliferation of PD-1–positive T cells.65 The PD-1 inhibitor pembrolizumab was studied in early phase trials in combination with lenalidomide and showed good response rates.66 However, the phase 3 KEYNOTE 18367 and 18568 IMiD/pembrolizumab combination trials were stopped prematurely by the US Food and Drug Administration because of a higher than expected number of deaths in the intervention arms.
Targeting the resistant state
Approaches to the further exploration of resistance mechanisms
Cell line models, drug screens, and ex vivo primary samples
The exploration of resistance generation has often been performed in cell line models because of the difficulty in keeping primary myeloma cells in culture for a prolonged period. MM cell lines display differing levels of sensitivity to IMiD treatment, and these distinctions are not binary, with dose and time course–dependent responses.69 Several teams have generated lines with acquired resistance,35,46,48,69 which can then be explored through genetic sequencing, RNA-seq analysis, whole-proteome analysis, or more targeted approaches.
Cell line models have also allowed for knockout genome-wide CRISPR-Cas9 screens to be performed. As discussed earlier, the forward screens conducted to date predominately identified direct regulators of the degradation mechanism as important in IMiD resistance, as opposed to resistance pathways independent of CRBN. The opposite approach, genome-wide CRISPR screening myeloma cells with acquired IMiD resistance, can be performed to identify genes that may reinduce sensitivity to IMiDs when knocked out. From one such screening, DNA topoisomerase II β (TOP2B) was identified as a putative candidate.70 CRISPR screening approaches could also be used to detect novel vulnerabilities in the acquired resistant setting, which may represent synthetic lethal targets in the low CRBN state. A genome-wide CRISPR-Cas9 screen in an MM1s cell line with acquired resistance to iberdomide allowed for the identification of a number of genes for which knockout led to a greater reduction in proliferation in the iberdomide resistant setting compared with the sensitive setting, and these may represent novel vulnerabilities gained during the acquisition of IMiD resistance.48
Cell lines with acquired resistance have also been used in drug screening efforts to find more potent CRBN binders that may be able to overcome resistance to existing IMiDs/CELMoDs. Mezigdomide was discovered through a phenotypic screen of a CRBN modulator library in NCI-H929 with acquired resistance to lenalidomide (which had low levels of CRBN).71,72 Ex vivo primary myeloma samples cannot be used for such large drug screens, but efforts to maintain primary myeloma cell viability ex vivo, such as the myeloma drug sensitivity testing system may help overcome this.73
Biomarkers of sensitivity and resistance
Well-validated biomarkers of sensitivity and resistance to IMiDs would be useful for the prognosis and monitoring of the disease in the clinic but could also improve our understanding of the biology of IMiD resistance and provide potential future targets. Increased CRBN gene expression was significantly associated with longer PFS among 96 patients who received maintenance with thalidomide as part of the HOVON-65/GMMG-HD4 trial.74 However, there was no association between CRBN expression and survival in the bortezomib maintenance arm of the trial, suggesting an IMiD-specific effect.74 Several studies have also shown that a high level of CRBN protein expression is associated with good prognosis in patients treated with IMiDs,69,75 but whether Ikaros, Aiolos, and IRF4 expression correlates with IMiD response is not completely clear.2,76,77 As discussed previously, reduced expression and mutations in CRBN, CRBN pathway genes and methylation changes have been identified in samples from patients relapsing with IMiDs, but whether these can be used as predictive biomarkers of response is not certain. Data from the Myeloma XI trial also showed that mutations in IRF4 and early growth response 1 (EGFR1) were associated with favorable OS in this patient population treated with IMiD,78 and the possible mechanisms behind this are being investigated.
Exploration of the myeloma cell surface proteome, known as the surfaceome, which determines malignant cell interaction with the BM microenvironment, has been carried out using glycoprotein cell-surface capture proteomics to evaluate the surfaceome at baseline, in drug resistance, and in response to short-term drug treatment.79 Cell-surface capture proteomics was performed on OPM2 and NCI-H929 cell lines with acquired lenalidomide resistance, and there was a common signature of increased CD33 and CD45/PTPRC, which, if validated, could potentially be used as a biomarker of resistance.79
Overcoming resistance in the clinical setting
Targeted approaches are needed in the clinic to improve outcomes for patients who are resistant to IMiDs. Based on the body of data described previously, these approaches can be divided into those aiming to overcome resistance while still targeting CRBN or those exploiting the IMiD-resistant state either by reversing resistance or by synthetic lethality. As discussed previously, newer generation IMiDs/CELMoDs may be able to overcome resistance to early generation compounds.2,80 Several CELMoDs are currently in clinical trials, with iberdomide and mezigdomide now moving into phase 3 trials.26,27 In patients with CRBN mutations, it is important to understand whether a given mutation is likely to lead to resistance to only selected or all IMiDs/CELMoDs (as well as potential CRBN-directed novel glues and PROTACs). In patients with low CRBN levels, stronger binders may be able to use the lower levels of CRBN or stabilize CRBN. Recently, a new class of related compounds, known as monofunctional degradation activating compounds, have been developed and have entered early phase trials.81 The monofunctional degradation activating compound CFT7455 was developed to induce potent, rapid, and sustained degradation of Ikaros and Aiolos and have a high binding affinity to CRBN, in an attempt to overcome IMiD resistance.81 In comparison with mezigdomide, CFT7455 had different pharmacokinetics and pharmacodynamics that led to longer exposure and it demonstrated superior efficacy in an NCI-H929 MM xenograft mouse model.81 In an open-label, multicentre, phase 1/2 clinical trial (NCT04756726) that included patients who were heavily pretreated, early pharmacodynamic data showed deep degradation of Ikaros and Aiolos and evidence of single-agent activity.81
Exploiting the IMiD-resistant state requires a different approach. Several novel pathways and their associated small molecule inhibitors have been discussed, with the most promising based on the current data of those targeting the MEK pathway,53 extralineage transcription factors, such as ETV4,55 and epigenetic regulators, such as CRBP/EP30054 and EZH2.46,47 Protein components in lipid synthesis pathways may also be novel and targetable synthetic lethal vulnerabilities in the IMiD-resistant setting.48
Conclusions
The generation of IMiD resistance is a critical challenge in the management of MM, and although our understanding is growing, there are still many unanswered questions. Even as the variety of myeloma therapeutics expands, for example, the rapid adoption of T-cell redirection therapies, IMiDs continue to be used in therapeutic combinations throughout the treatment course, and understanding resistance remains central to improving patient outcomes.
Along with additional studies of myeloma cell–intrinsic mechanisms, it is also important to further explore the interaction of myeloma cells with the tumor microenvironment. Given the action of IMiDs in T and NK cells, a future path of study is to understand whether CRBN pathway members are altered in these immune cells and whether this might contribute to resistance generation. It is also currently unclear whether myeloma cell–intrinsic and –extrinsic resistance mechanisms can interact; for example, whether myeloma cell–intrinsic resistance mechanisms can influence T- and NK-cell function.
As we move forward, all clinical trials should report the IMiD refractory/resistant status of patients as well as biomarkers such as CRBN mutation status, to enable subgroup analysis. Novel trials should be designed specifically for the IMiD-resistant subgroup of patients to explore agents with novel mechanisms of action targeting resistance biology. Advances in our knowledge will enable the design of next generation molecular glues and PROTACs as well as strategies to reverse resistance and/or exploit vulnerabilities that evolve during resistance development, enabling targeted approaches to overcome resistance in the clinical setting.
Acknowledgment
The authors acknowledge that many investigators have contributed substantially to this area of research and apologise if, due to a lack of space, any colleague’s work has not been mentioned.
S.B. is a Wellcome Trust Clinical Research Fellow (222880/Z/21/Z), C.P. is a CRUK Clinician Scientist (C47608/A29649).
Authorship
Contribution: S.B. and C.P. conducted the literature review and wrote the paper.
Conflict-of-interest disclosure: C.P. is a consultant for and has received honoraria from AbbVie, Sanofi, Janssen, and Celgene/BMS; and received travel support from Janssen to attend meetings. S.B. declares no competing financial interests.
Correspondence: Charlotte Pawlyn, Division of Cancer Therapeutics, The Institute of Cancer Research, London SM2 5NG, United Kingdom; e-mail: charlotte.pawlyn@icr.ac.uk.