Abstract
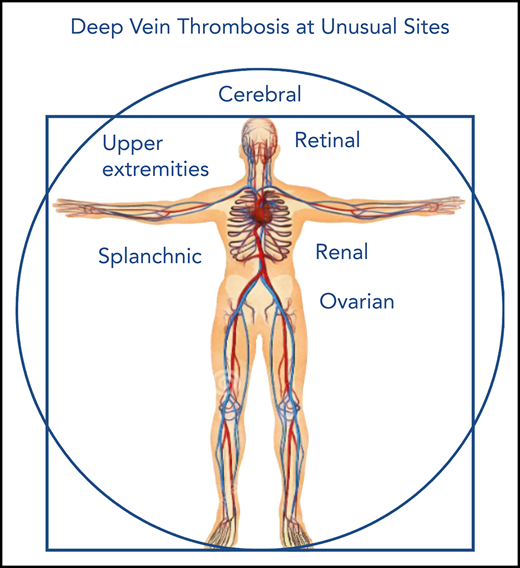
Venous thrombosis rarely occurs at unusual sites such as cerebral, splanchnic, upper-extremity, renal, ovarian, or retinal veins. Clinical features, symptoms, and risk factors of rare thrombotic manifestations are heterogeneous and in large part differ from those typical of the commonest manifestations of venous thrombosis at the lower extremities. The therapeutic approach also varies widely according to the affected site, whether cerebral, abdominal, or extraabdominal. To date, anticoagulant therapy for thrombosis at unusual sites is generally accepted, but the optimal therapeutic approach remains challenging. This review is focused on the treatment of unusual thrombotic manifestations as reported in the most recent guidelines and according to the updated scientific literature.
Introduction
Thrombosis at unusual sites accounts for ∼10% of all cases of venous thrombosis, affecting any venous region other than the deep or superficial veins of the lower limbs or those involved in pulmonary circulation. Its annual incidence varies from 1 to 2 cases per 1 million individuals for splanchnic vein thrombosis to 5 per 1000 individuals for retinal vein thrombosis.1,2 Cerebral venous sinus thrombosis (CVST) occurs more often in young women because of its strong association with oral contraceptive use and pregnancy.3 Splanchnic vein thrombosis (SVT) often complicates underlying diseases such as liver cirrhosis, myeloproliferative neoplasms (particularly those bearing the Janus kinase 2 V617F mutation), paroxysmal nocturnal hemoglobinuria, Behçet’s disease, inflammatory bowel diseases, or abdominal cancers.4 Upper-extremity deep vein thrombosis (UEDVT) is defined as primary when resulting from effort (Paget-Schrotter syndrome) or thoracic outlet syndrome or when unprovoked and as secondary when caused by triggering factors, mainly indwelling central venous catheters (CVCs)5,6 but also pacemakers and cancer. Renal vein thrombosis (RVT) is the most common thrombotic manifestation in neonates, particularly those born prematurely, accounting for 16% to 20% of all thromboembolic events,7 and is mainly related to umbilical or femoral indwelling catheters reaching the inferior vena cava, whereas in adults, it is mainly associated with cancer (66%) and nephrotic syndrome (20%), as well as renal transplantation (0.5%) and local trauma (surgery or venous catheters).8 Ovarian vein thrombosis (OVT) is usually associated with pregnancy or the postpartum setting, pelvic inflammation, abdominal cancer, and pelvic surgery.9 Retinal vein occlusion (RVO) involving the central or branch veins or, more rarely, the hemicentral vein is mainly caused by intraocular hypertension or glaucoma or, in contrast to venous thrombosis at other sites, by the systemic risk factors for arterial thrombosis (ie, arterial hypertension, diabetes, hyperlipidemia).10,11
To date, anticoagulant therapy with low molecular weight heparin (LMWH) or unfractionated heparin (UFH) followed by vitamin K antagonists (VKAs) is generally accepted in patients with thrombosis at unusual sites. With the exception of 4 small randomized controlled trials (RCTs) in patients with CVST, 1 in those with OVT, and 3 in those with RVO, no RCTs have been performed in patients with unusual thrombotic manifestations, whose treatment remains challenging in the absence of high-quality evidence.
The aim of this review is to summarize the therapeutic options for thrombosis at unusual sites, examining the existing guidelines published by various scientific societies and screening their relative references. In addition, we consulted 2 databases of evidence-based content (Trip Medical Database and Dynamed Plus) and searched PubMed for relevant scientific literature on thrombosis at unusual sites after the publication date of the most recent guidelines.
CVST
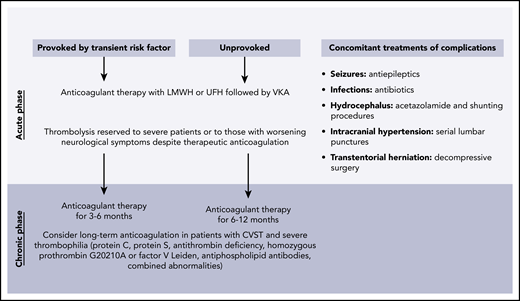
A metaanalysis of 2 small and older RCTs showed that treatment of CVST with LMWH or UFH in the acute phase is safe and efficacious in terms of mortality and disability12-14 and does not enhance the risk of intracranial hemorrhage.15 Therefore, heparin is recommended by several neurological guidelines16-18 and by the American College of Chest Physicians (ACCP),19 even in the presence of intracranial hemorrhage. Two more recent RCTs and a metaanalysis favored LMWH over UFH,20-22 although the small sample size of the studies allowed recommendations of only moderate-quality evidence. UFH, with its shorter half-life and easier reversibility, should be preferred in patients with unstable cases or in those requiring invasive procedures. Endovascular treatment with local thrombolysis (urokinase, streptokinase, or recombinant tissue plasminogen activator) or mechanical thrombectomy has been investigated only in small case series and seems associated with a high risk of intracranial hemorrhage (7.6%) and mortality (9.2%).23 Local thrombolysis was compared with heparin treatment in the TO-ACT trial (registered at www.clinicaltrials.gov as #NCT01204333), which was prematurely interrupted because of futility (no difference in the primary outcome disability) after the inclusion of 67 patients.24,25 A systematic review of 26 patients treated with systemic thrombolysis (mainly urokinase) reported an extracranial or intracranial hemorrhage in 30.7% of patients and partial or complete recanalization in 61.5%.26 Hence, local or systemic thrombolysis should be reserved for patients with severe cases or those with worsening neurological symptoms despite therapeutic anticoagulation.27 In the acute phase, complications could require specific management with antiepileptic drugs in the case of seizures17 ; acetazolamide and shunting procedures to drain excess cerebrospinal fluid in the case of hydrocephalus with neurological deterioration; serial lumbar punctures in the case of intracranial hypertension, papilledema, or reduced visual acuity18 ; or decompressive hemicraniectomy as a lifesaving procedure in the rare case of transtentorial herniation resulting from large hemorrhagic infarcts. The DECOMPRESS-2 registry is an ongoing prospective evaluation of patients with CVST undergoing decompressive surgery, and the interim analysis of 22 patients showed a 6-month mortality rate of 23.8% in patients treated vs 100% in those not treated.28 After the acute phase, anticoagulant therapy is administered for secondary prevention of CVST or venous thrombosis at other sites. The risk of recurrent thrombosis is low, and long-term anticoagulation should be reserved for patients with persistent and unmodifiable risk factors such as severe thrombophilia and solid or hematological neoplasms.29,30 The American Heart Association and American Stroke Association guidelines recommend that patients with CVST secondary to a transient risk factor receive anticoagulant therapy with VKAs for 3 to 6 months, whereas those with unprovoked CVST should receive such therapy for 6 to 12 months.17 Figure 1 summarizes the recommendations for treatment of CVST. For patients with no recognized thrombophilia abnormalities, the same guidelines recommend a switch to antiplatelet therapy, but in the absence of controlled trials or observational studies, this recommendation seems unsupported.31 The ongoing EXCOA-CVT study (registered at http://www.isrctn.com as #ISRCTN25644448) comparing short (3-6 months) with long (12 months) duration of oral anticoagulant therapy in patients with CVST will provide new insights.32
SVT
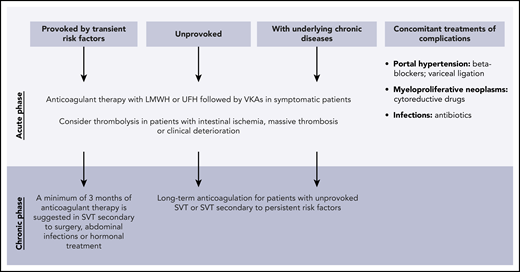
On the basis of observational studies, anticoagulant therapy in patients with SVT (portal intra- or extrahepatic, superior mesenteric, and splenic vein) is recommended by the ACCP guidelines only in symptomatic cases and not in those incidentally detected, unless in the case of extensive thrombosis, thrombus progression, or active cancer.33 This approach is in accordance with the evidence indicating that symptomatic patients have a double risk of recurrent thrombosis rather than bleeding, whereas asymptomatic patients have similar risks.34,35 In contrast, the American Association for the Study of Liver Diseases guidelines recommend anticoagulation for all patients with acute portal vein thrombosis, including asymptomatic patients.36 For patients with isolated portal or splenic vein thrombosis, some authors suggest a watchful waiting approach, based on a retrospective study showing spontaneous thrombus regression in 47% of patients, stability in 45%, and progression in only 7%.37 An exception is acute mesenteric vein thrombosis, which may represent an emergency, requiring prompt initiation of anticoagulation together with support therapy because of the high 30-day mortality (20%) despite treatment.38 The European Society of Vascular Surgery recommends anticoagulation with heparin as first-line treatment followed by oral anticoagulants, in the absence of major contraindications.39 In patients with intestinal ischemia, local catheter–directed thrombolysis should be considered with the aim of avoiding ischemic bowel resection.40 Thrombolysis should also be considered in patients with particularly extended thrombosis or clinical deterioration despite anticoagulant therapy, if their bleeding risk is low. There are insufficient data to suggest local catheter–directed over systemic thrombolysis.40
The optimal duration of anticoagulant therapy is not established, but a minimum of 3 months is suggested for patients with SVT associated with transient risk factors.36 Patients with persistent risk factors, such as myeloproliferative neoplasms or cirrhosis, or those with idiopathic thrombosis should continue anticoagulant therapy for life.36,41 An international prospective cohort study of 604 patients with SVT showed incidence rates per 100 patient-years of 3.8 for major bleeding and 7.3 for recurrent thrombosis, 3.9 and 5.6 during anticoagulation, and 1.0 and 10.5 after anticoagulation discontinuation, respectively. The highest incidence rates of major bleeding and thrombosis were observed in patients with cirrhosis (10.0 and 11.3 per 100 patient-years, respectively).42 The recanalization rates after 1 year of anticoagulant therapy with VKAs were 38%, 61%, and 54% for portal, mesenteric, and splenic veins, respectively.43 These figures indicate indefinite anticoagulation in most patients. However, many patients have risk factors for bleeding, such as liver cirrhosis, possibly associated with portal hypertension and esophageal varices; splenomegaly, possibly associated with thrombocytopenia; or cancer. A large Danish cohort study of 1915 patients followed for 10 years reported higher bleeding rates in patients with all-cause SVT than in those with lower-extremity DVT (LEDVT) or pulmonary embolism.44 However, the risk of bleeding in cirrhotic patients seems to be lower than expected (<5%)45 and is further reduced during anticoagulation.46,47 Hence, esophageal varices and liver dysfunction–associated coagulopathy do not represent absolute contraindications to anticoagulation, as confirmed by a recent metaanalysis, which showed higher recanalization rates and lower variceal bleeding rates in patients with portal vein thrombosis and liver cirrhosis who received anticoagulant therapy compared with those who did not.48 To reduce the bleeding risk, patients with liver cirrhosis often benefit from prophylaxis for variceal bleeding with nonselective β-blockers and/or endoscopic variceal ligation. Regarding anticoagulant treatment in patients with SVT and moderate to severe thrombocytopenia, evidence is limited to expert opinion. In the absence of bleeding complications, the intensity of anticoagulation can be reduced to half therapeutic doses, if platelet counts are between 50 and 100 × 109/L, and to prophylactic doses, if platelet counts are between 30 and 50 × 109/L. In the presence of severe thrombocytopenia (<30 × 109/L), some experts recommend against anticoagulation.40 Recommendations for treatment of SVT are summarized in Figure 2.
UEDVT
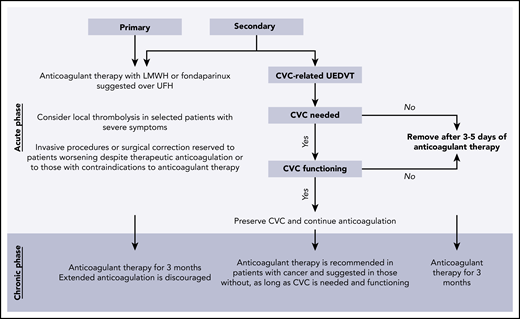
On the basis of moderate-quality and indirect evidence from the treatment of LEDVT, the ACCP guidelines recommend parenteral anticoagulation in the acute phase of primary UEDVT involving the axillary or more proximal veins and suggest LMWH or fondaparinux over UFH or thrombolysis for a minimum duration of 3 months.33 Uncertainty remains regarding full-dose anticoagulation in patients with isolated primary brachial vein thrombosis, a treatment favored only in severe symptomatic patients; for the others, clinical surveillance, LMWH, or fondaparinux at prophylactic doses for 3 months or therapeutic doses for <3 months is suggested.33 Selected patients with severe cases may benefit from catheter-directed thrombolytic treatment, encouraged over systemic thrombolysis.33,49 Like LEDVT, UEDVT may be complicated by postthrombotic syndrome (PTS). Because no RCTs on the prevention of PTS with compression sleeves or venoactive medications are available, the ACCP guidelines recommend against their use, but anecdotal evidence supports bandages or compression sleeves.33 A recent metaanalysis compared the rates of PTS, recurrent thrombosis, and major bleeding in patients with primary or secondary UEDVT treated conservatively with anticoagulant therapy or invasively with thrombolytic therapy and/or decompressive surgery. Patients receiving anticoagulant therapy had a higher risk of PTS (23.2% vs 11.8%), similar risk of recurrent thrombosis (7.6% vs 7.5%), and lower risk of bleeding (1.3% vs 3.8%) than those treated invasively; the frequency of PTS was higher in patients with primary than in those with secondary UEDVT.50 Hence, the decision for aggressive treatment should be weighed against the risk of bleeding and that of PTS, but because the latter is unpredictable, more data are necessary before making recommendations. Limited data are available on percutaneous mechanical thrombectomy, angioplasty along with endovascular stenting, filter insertion, and resection of the first rib for decompression in the presence of thoracic outlet syndrome,51 none of which are routinely recommended in the acute phase; these should be reserved for exceptional cases such as patients for whom anticoagulant therapy fails or those in whom anticoagulant therapy is contraindicated.33
The optimal treatment duration of primary UEDVT beyond 3 months is still debated. A majority of patients are managed with heparin followed by VKAs for up to 3 or 6 months, as recommended.50 Although a prospective population-based study showed a similar rate of recurrent thrombosis in patients with UEDVT and in those with LEDVT,52 a direct comparison between unprovoked UEDVT and LEDVT showed a lower recurrence rate in those with UEDVT (4% vs 19%) over a 5-year period.53 Hence, unlike inLEDVT, extended anticoagulation is discouraged in patients with unprovoked UEDVT.33
For secondary CVC-related UEDVT, the ACCP guidelines support maintaining the CVC if still functioning and needed, despite the presence of the thrombus. Anticoagulation is recommended as long as the CVC remains in place in patients with cancer and suggested in those without.33,54 If the CVC is not functioning or no longer required, it can be removed after a short period of anticoagulation (3-5 days)54 ; thereafter, 3 months of anticoagulant therapy are suggested in patients with cancer and recommended in those without.33,54 Figure 3 summarizes the recommendations for treatment of primary and secondary UEDVT.
RVT
RVT is frequently encountered in neonates, for whom current guidelines provide recommendations; however, its management in adults is not specifically addressed. The pivotal recommendation of the American Society of Hematology for the management of RVT in neonates is to involve a multidisciplinary team that includes neonatologists, radiologists, hematologists, and nephrologists.55 According to the ACCP guidelines, unilateral RVT can be managed only with supportive therapy and radiologic monitoring. Anticoagulant therapy is suggested in patients with thrombus extension as well as in patients with RVT and nephrotic syndrome (pulmonary embolism is reported in up to 76% of cases), impairment of renal function, or extension into the inferior vena cava. In the case of unilateral RVT in monokidney patients or those receiving kidney transplants, worsening RVT despite adequate anticoagulant therapy or lifethreatening bilateral RVT with severe renal deterioration, thrombolysis as well as the placement of a temporary suprarenal inferior vena cava filter should be considered.55,56 In neonates, thrombolysis is complicated by a 21% rate of major bleeding.55 In general, when using heparin, one should consider that neonates have a high clearance and often reduced antithrombin plasma levels (physiologically or resulting from proteinuria in the presence of nephrotic syndrome), so higher heparin doses than those for adults and perhaps antithrombin concentrate may be needed. In contrast, in the frequent clinical case of RVT presenting with renal function impairment, particular attention should be given to anticoagulant dose adjustment to avoid drug accumulation. Despite the scarce evidence, it seems that the same outcome in terms of mortality, resolution of RVT, long-term renal impairment, and hypertension is achieved regardless of the use of anticoagulant therapy.55 The suggested duration of anticoagulant therapy in neonates with RVT secondary to transient risk factors varies from 6 weeks to 3 months, whereas those with unprovoked or nephrotic syndrome–associated RVT should continue until resolution of proteinuria.56,57
OVT
In a vast majority of cases, OVT is a complication of pregnancy or postpartum conditions. Six retrospective studies, 1 prospective study, and a small RCT on the management of pregnancy- and postpartum-associated OVT were included in a systematic review.58 Interventions included mainly antibiotic and/or anticoagulant therapy, the latter for a median duration of 3 months, as reported in the 2 largest cohorts of 13 and 74 patients, respectively.59,60 Concerning the type of anticoagulant therapy, the most frequently used was LMWH, but warfarin58,60,61 and, rarely, an anti–factor Xa oral anticoagulant were also used.9,62 On the basis of this evidence and extrapolating the duration of anticoagulant therapy from the ACCP guidelines on the treatment of LEDVT,49 3 months are suggested for symptomatic postpartum OVT, with the addition of antibiotic therapy, if needed.58 Among the gynecological guidelines, OVT is mentioned only by the Canadian Society of Obstetricians and Gynecologists, which recommends parenteral broad-spectrum antibiotic therapy until 2 days after resolution of symptoms and anticoagulant therapy for 1 to 3 months.63 Anticoagulant therapy is discouraged in asymptomatic postpartum-associated OVT with no evidence of thrombus extension or pulmonary embolism.58 Data on treatment of OVT outside of pregnancy or the postpartum setting are limited to small case series60,64 and do not allow for recommendations.
RVO
The current treatment options for RVO recommended by the Royal College of Ophthalmologists include the use of intravitreal antivascular endothelial growth factor agents if RVO is complicated by macular edema, along with laser photocoagulation of ischemic areas and/or corticosteroids.65 A recent metaanalysis showed that antivascular endothelial growth factor agents are the most effective therapy for macular edema secondary to both central and branch RVO.66 Anticoagulant treatment is a parallel option, although it is not routinely recommended by the Royal College of Ophthalmologists guidelines65 or by the Anticoagulation Forum40 because of the lack of evidence, but it may be limited to patients without local risk factors, with recent onset of symptoms, or with major risk factors for thrombosis (eg, antiphospholipid antibodies). For the latter, long-term anticoagulant therapy may be considered.67 In the most rigorous RCT of 58 patients with early-onset (within 15 days) RVO, treatment with therapeutic doses of LMWH for 7 days and half therapeutic doses thereafter for a total of 3 months was more effective than aspirin in preventing visual loss.68 A metaanalysis including 3 RCTs comparing the effect of LMWH vs aspirin in patients with RVO favored LMWH, which improved visual acuity and was associated with a 78% reduction in the risk of developing adverse ocular outcomes.69 A large prospective cohort study of 686 patients with RVO showed no benefit and even worse visual outcomes in patients receiving aspirin or other antiplatelet drugs compared with nontreated patients.70 Hence, LMWH is suggested for a period of 1 to 3 months in RVO patients with recent onset of symptoms, no local risk factors (ie, glaucoma), and no contraindications,40,67,71 with therapeutic doses for 10 to 15 days, followed by half therapeutic doses for up to 3 months.67 Fondaparinux was also reported to be safe and effective in resolving recent-onset RVO in 13 consecutive patients.72 Local thrombolytic therapy should be considered only in selected cases with total visual loss.40
Thrombophilia testing
The different guidelines considered in this review do not address specifically the benefits of thrombophilia testing in patients with thrombosis at unusual sites. At present, one should approach testing in thrombosis at unusual sites as in LEDVT, although even in thrombosis at such a common site, the issue of testing is debated. Only severe thrombophilia abnormalities (eg, homozygous factor V Leiden or G20210A prothrombin mutation; antithrombin, protein C, or protein S deficiency; antiphospholipid antibodies; or combined abnormalities) may influence the duration of anticoagulant treatment, because they are associated with a higher risk of recurrent venous thrombosis than the common heterozygous mutations in factor V and II. Whether patients with severe thrombophilia may benefit from a longer or indefinite duration of anticoagulant therapy should be investigated in an RCT, but an RCT is almost unfeasible considering the rarity of severe abnormalities.73 In this panorama, routine thrombophilia testing is usually discouraged, because it would not influence patient management. For thrombosis at unusual sites, which often involves local or systemic conditions triggering the event, testing for thrombophilia seems even less useful. It can be reserved for selected patients with unexplained events, young age, or positive family history of thrombosis, with careful consideration given to the interpretation of the results.73
Cancer screening
Apart from myeloproliferative neoplasms, screening for which should be conducted in patients with unprovoked SVT and, to a lesser extent, in those with unprovoked cerebral venous thrombosis (CVT), extensive screening for occult cancer is not recommended in patients with thrombosis at unusual sites.74 Given that radiologic imaging is required for the diagnosis of CVT, SVT, UEDVT, RVT, and OVT, it is usually enough to detect regional occult cancer. Extensive diagnostic cancer screening is also not warranted in patients with RVO, who do not have an increased risk of cancer, as shown in a Danish nationwide population-based cohort study.75
Role of DOACs
Because the phase 3 RCTs conducted on direct oral anticoagulants (DOACs) did not include patients with unusual thrombotic manifestations,76 their safety and efficacy in this setting needs to be proven in dedicated clinical trials, and at present, their use should be discouraged. Limited data are available from 7 case series77-83 reporting on 44 patients with CVST treated with DOACs for a period varying from 3 to 19 months, with complete or partial recanalization achieved in ∼80% of cases without bleeding complications. Table 1 lists the ongoing clinical trials on treatment of CVST with DOACs. Regarding SVT, the only RCT of 80 patients comparing 10 mg of rivaroxaban with warfarin at a 1:1 ratio showed favorable safety and efficacy profiles for rivaroxaban.84 A total of 92 patients with SVT were treated with DOACs in 8 case reports or case series, and 4 major gastrointestinal bleedings and 2 cases of recurrent thrombosis were reported.85-92 On the basis of this evidence and considering the increasing amount of data in patients with cancer (often associated with SVT), the use of DOACs has been suggested in patients with SVT.93 In addition, a pilot prospective single-arm cohort study of patients with SVT and no cirrhosis treated with rivaroxaban is ongoing (registered at www.clinicaltrials.gov as #NCT02627053). The use of DOACs was reported in a retrospective study of 55 patients with UEDVT who developed 1 recurrent UEDVT (2%) and 1 clinically relevant nonmajor bleeding episode (2%) during treatment.94 A pilot study in patients with cancer and CVC-associated UEDVT treated with rivaroxaban has completed recruitment (registered at www.clinicaltrials.gov as #NCT01708850). Two other phase 4 single-arm studies of apixaban for the treatment of UEDVT, 1 in patients with cancer (registered at www.clinicaltrials.gov as #NCT03100071) and 1 in those without (registered at www.clinicaltrials.gov as #NCT02945280), are ongoing. Only 4 cases of RVT treated with DOACs (rivaroxaban and apixaban) have been reported so far, with no evidence of increased risk of bleeding or recurrence.62,95 There is still no experience with DOACs in the treatment of RVO, and their use is discouraged. The only prospective study comparing the use of DOACs (rivaroxaban or apixaban) in patients with thrombosis at unusual sites, including CVST, SVT, OVT, and RVT, and in those with thrombosis at common sites showed comparable safety and efficacy; moreover, the rates of bleeding and recurrent thrombosis in patients treated with DOACs were similar to those in patients treated with enoxaparin.62 Finally, an international registry on DOACs for treatment of all unusual thrombotic manifestations included in this review except for UEDVT is ongoing and will provide new insights (registered at www.clinicaltrials.gov as #NCT03778502).
Authorship
Contribution: M.A., M.C., and I.M. worked collaboratively to develop this review, drafting and revising the text, table, and figures. All authors approved the final submission.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ida Martinelli, Fondazione IRCCS Ca’ Granda–Ospedale Maggiore Policlinico, A. Bianchi Bonomi Hemophilia and Thrombosis Center, Via Pace 9, 20122 Milan, Italy; e-mail: ida.martinelli@policlinico.mi.it.