Key Points
Mutation clearance in CML does not directly result in successful treatment in CML.
Clinical implications of patterns of mutation acquisition, persistence, and clearance in CML should be interpreted with caution.
Abstract
Somatic mutations commonly detected in a variety of myeloid neoplasms have not been systematically investigated in chronic myeloid leukemia (CML). We performed targeted deep sequencing on a total of 300 serial samples from 100 CML patients; 37 patients carried mutations. Sixteen of these had evidence of mutations originating from preleukemic clones. Using unsupervised hierarchical clustering, we identified 5 distinct patterns of mutation dynamics arising following tyrosine kinase inhibitor (TKI) therapy. This study demonstrates that patterns of mutation acquisition, persistence, and clearance vary but have a number of interesting correlations with clinical outcomes. Mutation burden often persisted despite successful TKI response (pattern 1), providing indirect evidence that these mutations also originated from preleukemic mutations, whereas patients exhibiting mutation clearance (pattern 3) showed mixed clinical outcomes. Unsurprisingly, patients acquiring new mutations during treatment failed TKI therapy (pattern 2). These patterns show that CML mutation dynamics following TKI therapy are markedly distinct from other myeloid neoplasms. In summary, clinical implications of mutation profiles and dynamics in CML should be interpreted with caution.
Introduction
Chronic myeloid leukemia (CML) is characterized by a translocation event t(9;22)(q34;q11.2) which rearranges the Abelson murine leukemia viral oncogene homolog 1 (ABL1) and breakpoint cluster region (BCR) genes, yielding a BCR-ABL gene rearrangement.1 The development of tyrosine kinase inhibitors (TKIs) targeting the BCR-ABL fusion protein has had an incredible impact on the treatment of CML.2-4 A majority of CML cases now have better long-term outcomes than cases of most other myeloid malignancies. However, some patients show resistance to these treatments through BCR-ABL–dependent or –independent mechanisms, and as a result, have a much higher risk of progression to an accelerated phase (AP) or blastic phase (BP) of disease. The survival of patients who progress to BP is comparable to the pre-TKI era, even with other salvage treatment modalities such as allogeneic stem cell transplantation.5
Taking advantage of high-throughput technologies, extensive investigations into other myeloid malignancies have uncovered commonly mutated genes and their affected pathways.6-10 The Cancer Genome Atlas (TCGA) Consortium has compiled a list of commonly mutated genes found in 199 of 200 adult de novo acute myeloid leukemia (AML) cases; these mutations were then classified into 8 categories based on the biological pathways they affect (activated signaling, chromatin modification, cohesion complex, DNA methylation, myeloid transcription factors, tumor suppressors, NPM1, and splicing machinery).6 Genomic studies in myelodysplastic syndromes, myeloproliferative neoplasms, chronic myelomonocytic leukemia, and atypical CML have since demonstrated that most patients with myeloid malignancies carry somatic mutations that fall within these 8 pathway categories.7,11-13
In CML, the most well-understood mechanisms of TKI resistance are caused by mutations within the kinase domain (KD) of ABL1, which account for approximately half of nonresponsive patients.14 Clones that develop ABL1 KD mutations, whether they exist prior to treatment or develop later, block the binding of TKI, accounting for TKI resistance.15-20 Although many studies have investigated ABL1 KD mutations,21-26 less is known about the mutation spectrum in other genes in TKI-resistant cases before and after treatment.
Previous studies have shown that progression of CML into AP or BP is associated with the acquisition of genetic or epigenetic abnormalities in addition to BCR-ABL gene rearrangement.27-31 In particular, somatic mutations in genes associated with chromatin modification and DNA methylation are often enriched; in contrast, the other 6 pathways are not enriched in CML.27-29,32 The origins, clinical implications, and associations with BCR-ABL transcript changes of relevant somatic mutations remain mostly unknown.
In addition, the potential role of preleukemic somatic mutations in CML has been investigated in relatively few studies.32 Preleukemia is a stage of the evolution of cancer in many patients, characterized by the growth of cells carrying a subset of genetic or epigenetic mutations necessary for leukemogenesis.33 Leukemic transformation occurs upon the acquisition of additional genetic lesions. The preleukemic clone can be retained or expand during leukemogenesis while differentiation potential is maintained.33
To investigate how mutation acquisition, persistence, and clearance affect the treatment outcomes in CML, we used targeted deep sequencing on serial samples from 100 CML patients (Table 1) to profile somatic variants in 92 genes commonly mutated in myeloid malignancies. For each patient, samples taken at the initial diagnosis (prior to TKI therapy) and after TKI treatment, as well as corresponding T-cell fraction, were subjected for sequencing.
Patients and methods
The study was approved by the research ethics board at Chonnam National University, Hwasun, Korea.
Patients
Samples from a total of 100 patients were sequenced, of whom 78 were treated with imatinib, 11 with nilotinib, 8 with dasatinib, and 3 with radotinib. Clinical information is detailed in Table 1. With a median follow-up duration of 55 months (range, 6-158 months), response outcomes were as follows: 68.3% (57.7%-76.7%) of complete cytogenetic response at 12 months, 49.9% (39.5%-59.5%) of major molecular response at 18 months, 43.5% (33.2%-53.3%) of molecular response of 4.5 log reduction at 3 years. Treatment failure was estimated as 10.2% (0.3%-15.9%) at 3 years whereas progression-free survival at 5 years was 91.0% (82.7%-95.5%). The overall survival at 5 years was 92.6% (83.8%-96.7%). According to the response, 74 patients were determined to have optimal response by European LeukemiaNet (ELN),34 18 failed but remained in chronic phase, and 8 had progressed to AP or BP. We will henceforth refer to these outcome categories as the responsive group, the resistant group, and the progressed group.
Sample preparation
Marrow samples at the time of diagnosis were prospectively procured and banked. Follow-up marrow samples while on TKI therapy were also collected 1 to 1.5 years after starting TKI therapy in the responsive group, whereas it was taken at the time of confirmation of resistance in the resistant group or confirmation of progression to AP/BP in the progressed group. Isolated T-cell samples (CD3+) were procured from the diagnostic samples using the CD3+ monoclonal antibody magnetic bead-based isolation method. DNA was extracted per samples and processed for targeted deep sequencing. DNA for all 300 bone marrow mononuclear cells was extracted using the QIAamp DNA Blood Mini kit (Qiagen). Each case had a trio of samples: T-cell fraction taken at diagnosis, the diagnostic leukemic sample, and a follow-up sample. The median duration from diagnosis to blood sampling was 12.0 months without any significant differences among 3 subgroups (12.0 months in responsive, 12.5 months in resistant, and 6.5 months in progressed group; P = .3 by median test).
Definition of end points
Complete cytogenetic response (CCyR) was defined using the conventional criteria of 0% Philadelphia chromosome–positive (Ph+) cells in marrow by conventional cytogenetics of 20 metaphases, whereas major molecular response (MMR) was defined as <0.1% of the BCR-ABL transcript level by polymerase chain reaction. Molecular response with 4.5 log reduction (MR4.5) was defined as 0.0032% or less BCR-ABL transcript level. Treatment failure includes primary and secondary resistance, defined as transformation to the AP or BP, loss of CCyR, appearance of an ABL1 KD mutation, or additional cytogenetic abnormalities in the Ph+ clone. Progression-free survival was defined as the interval between the initiation of TKI therapy and progression to AP or BP, or death from any cause, whereas overall survival was defined as the time from initiation of the TKI therapy until the time of death from any cause or time of last follow-up.
List of genes associated with epigenetic regulation
Chromatin modifiers (14 genes): ASXL1, BCOR, CREBBP, EED, EZH2, KAT6A, KAT6B, KMD6A, KMT2A (MLL), KMT2D (MLL2), KMT2C (MLL3), MECOM, PRDM9, PRDM16.
DNA methylation (7 genes): DNMT1, DNMT3A, DNMT3B, IDH1, IDH2, TET1, TET2.
Targeted NGS and sequencing read processing and computational analyses
Available in supplemental Methods (see supplemental Data available on the Blood Web site).
Definition of preleukemic mutations
The presence of mutation in T-cell samples as well as the bulk cell at diagnosis implies the presence of such mutations in hematopoietic stem cells. Less directly, the presence of mutations in follow-up samples for responsive patients also implies that Ph− cells carried the mutation. The most natural interpretation is that the Ph− clone descended from a preleukemic (Ph−) clone carrying the mutation. We classify patients as having evidence of preleukemic mutations if they carried somatic mutations in their T-cell samples and/or if the mutation in responsive patients had a variant allele frequency (VAF) >5% at follow-up.
Results
Mutational landscape of 100 CML patients in serial samples
Targeted deep sequencing of 92 myeloid malignancy–associated genes (supplemental Table 1) in 300 serial samples from 100 CML patients chosen retrospectively (74 responsive, 18 resistant, and 8 progressed; Table 1) revealed a total of 63 variants in 37 patients. Three of these patients carried only silent mutations in these genes. The remaining 63 patients did not carry mutations at any disease stage. The average read depth over the targeted regions was 840x (456x-944x) (supplemental Table 2).
The 63 variants consisted of 37 nonsynonymous single nucleotide variants (SNVs), 12 synonymous SNVs, 8 frameshift deletions, 2 stop-gain mutations, 2 nonframeshift deletions, and 2 splicing variants from 32 genes (supplemental Table 3). Among the 32 genes, 5 genes were nonsilently mutated in >1 patient (ABL1 in 6 patients, ASXL1 in 9 patients, DNMT3A in 2 patients, RUNX1 in 2 patients, and TET2 in 6 patients). ABL1 (16%, 6 of 37) and genes related to chromatin modification and DNA methylation (51%, 19 of 37) were the most commonly mutated (65%, 24 of 37 patients in total). Surprisingly, aside from a single SF1 variant, we did not observe any mutation within splicing machinery pathway genes, which are common in other myeloid disorders. As seen in Figure 1, ABL1 KD mutations were specific to nonresponsive patients. As expected, the frequency of somatic variants was highest among progressed patients (maroon, 8 of 8, 100%), second-highest among resistant patients (orange, 11 of 18, 61.1%), and lowest in the responsive group of patients (blue, 18 of 74, 24.3%; Fisher exact test, P < .00001), showing a clear association of increasing mutation burden with poor TKI response and progression to advanced disease (Figure 1).
Landscape of somatic variants in 100 CML patients in serial samples. (A) At the time of initial diagnosis and (B) at the time of follow-up. Bar plots above each table indicate the number of variants each patient carried; bar plots on the left indicate the number of patients with variant in each gene. Intensities of heatmap cells indicate the VAFs of each somatic variant. Pie charts below the first 3 subplots indicate the portion of patients from each response group with mutations at the relevant stage. Columns (patients) are first sorted by their patient subgroup (responsive, resistant, and progressed), then by the mutation burden in all stages combined within their subgroup. Rows are sorted by cohort occurrence frequency in the diagnosis and follow-up samples combined. Row and column order is the same for all subfigures.
Landscape of somatic variants in 100 CML patients in serial samples. (A) At the time of initial diagnosis and (B) at the time of follow-up. Bar plots above each table indicate the number of variants each patient carried; bar plots on the left indicate the number of patients with variant in each gene. Intensities of heatmap cells indicate the VAFs of each somatic variant. Pie charts below the first 3 subplots indicate the portion of patients from each response group with mutations at the relevant stage. Columns (patients) are first sorted by their patient subgroup (responsive, resistant, and progressed), then by the mutation burden in all stages combined within their subgroup. Rows are sorted by cohort occurrence frequency in the diagnosis and follow-up samples combined. Row and column order is the same for all subfigures.
Lastly, 10 patients (6 responsive patients, 3 resistant patients, and 1 progressed patient) carried a nonsilent mutation in their T-cell samples. Each of the 10 patients carried exactly 1 T-cell mutation (VAF >1%). The mean VAF for all variants in T-cell samples was 10.57%. Eight of these 10 patients carried a mutation in genes associated with epigenetic regulation (4 in TET2, 3 in ASXL1, 1 in DNMT3A). All T-cell mutations were detected in the corresponding diagnosis samples.
Hierarchical clustering to deconvolute mutation dynamics patterns following TKI therapy
Unsupervised hierarchical clustering on a 51-by-3 matrix (the number of nonsilent mutations by the number of series samples per patient) for the 34 patients with nonsilent variants suggested that different mutation patterns are clinically relevant and can provide important insights into the roles of somatic mutations beyond BCR-ABL gene rearrangement (Figure 2). VAFs of each mutation were linearly normalized to the maximum VAF among the 3 time points in order to measure the relative expansion/reduction without biasing the algorithm toward grouping mutations with similar absolute VAFs. Clearly, we see 5 patterns based on relative mutation burden at each of the 3 time points. Combinatorially, there are 8 possible broad patterns of high VAF vs low VAF across time points (ordered by T-cell, diagnosis, and follow-up samples). No high-low-high patterns and high-low-low patterns were apparent. We labeled the observed patterns as patterns 1 through 5, and refer to the lack of mutations (the low-low-low pattern) as pattern 0. With the exception of 2 cases (CML-37 and CML-99), only 1 pattern of clone dynamics was observed per patient, suggesting a relatively simple clonal architecture of CML compared with other hematologic malignancies such as AML. Patterns 4 and 5 contained too few cases and variants to make strong generalizations about, leaving 3 very distinctive and common clinically associated mutation dynamics patterns.
Mutation dynamics of somatic variants sorted and grouped using unsupervised hierarchical clustering. Rows are the gene names of all nonsilent variants found in the cohort (sorted by the clustering algorithm). Columns are the sample time points: T-cell, diagnosis, and follow-up (fixed temporal order). Color intensity indicates the row-normalized VAF. Major pattern groups are highlighted and labeled. The dot plot on the right represents the raw VAFs of the variants within each pattern group. Cells on the left indicate mutation presence in Catalogue of Somatic Mutations in Cancer (COSMIC) and Clinvar databases.
Mutation dynamics of somatic variants sorted and grouped using unsupervised hierarchical clustering. Rows are the gene names of all nonsilent variants found in the cohort (sorted by the clustering algorithm). Columns are the sample time points: T-cell, diagnosis, and follow-up (fixed temporal order). Color intensity indicates the row-normalized VAF. Major pattern groups are highlighted and labeled. The dot plot on the right represents the raw VAFs of the variants within each pattern group. Cells on the left indicate mutation presence in Catalogue of Somatic Mutations in Cancer (COSMIC) and Clinvar databases.
Pattern 1 contains mutations that were detected at the time of diagnosis and persisted after TKI therapy, but were absent in the T-cell samples; this is in the face of successful molecular response to TKI therapy in all cases whose variants exhibited this pattern. Pattern 2 contains mutations that were absent in both T-cell and diagnosis samples and only present in the follow-up samples. All patients with pattern 2 mutations were in nonresponsive groups. Pattern 3 contains mutations that appeared at diagnosis (or significantly increased between the T-cell samples and diagnosis samples) and significantly decreased at the time of follow-up. Patients with pattern 3 mutations had mixed clinical outcomes with no outcome group significantly overrepresented.
Pattern 1: Mutation persistence after TKI therapy does not correspond to treatment failure
The 7 patients with pattern 1 mutations all responded despite failing to achieve mutation clearance after TKI treatment. Nine of the 16 genes in this group are involved in transcription (ASXL1, ATRX, BCOR, CREBBP1, CUX1, EP300, JAK3, SF1, TRRAP), all of which except for ASXL1 are rarely reported in CML, but are more commonly found in myelodysplastic syndromes and AML.35-37 All pattern 1 mutations and genes were unique within the pattern. Because the mutations were not cleared in spite of significant reduction of BCR-ABL transcript level at the time of follow-up, they are likely to be indicative of a preleukemic Ph− clone that existed independent of Ph+ clones. The presence of mutations in these genes at diagnosis did not have any significant association with treatment failure or progression, except in the case of ASXL1 (5 of 9 patients, 55.6%).
Pattern 2: Acquisition of new mutations is a strong indicator of TKI treatment failure
The 9 patients with pattern 2 mutations acquired 13 new somatic variants after TKI treatment (Figure 2). Perhaps unsurprisingly, all 9 patients either showed resistance to TKI therapy, or progressed to more advanced disease stages (Figure 3). This pattern contained a high portion of ABL1 KD mutations (7 of 13 mutations in 6 patients including Q252H, F317L, E355G, F359V, and H396P); these mutations were also completely absent from the other patterns. All of these ABL1 KD mutations have been previously reported in association with TKI resistance.38,39 Other mutations were within genes known to be commonly mutated in myeloid disorders including CML such as TP53, KMT2D (MLL2), and TET2.27-29,32,40 Our results clearly indicate that the acquisition of new mutations during TKI therapy was strongly correlated with treatment failure.
BCR-ABL transcript level at follow-up compared with changes in VAF.BCR-ABL level indicated on a log10 percentage scale for both subplots. Each circle in the left bee swarm plot represents a variant. Filled circles indicate TKI treatment failure in the patient that had that variant; empty circles indicate successful response. The right bee swarm plot shows the BCR-ABL transcript reduction level for patients without extra mutations. Each dot indicates an individual patient. The boxes on the far right indicate the number of patients within each decade of TKI response colored by pattern (patients with both pattern 2 and pattern 3 mutations are labeled here as pattern 2).
BCR-ABL transcript level at follow-up compared with changes in VAF.BCR-ABL level indicated on a log10 percentage scale for both subplots. Each circle in the left bee swarm plot represents a variant. Filled circles indicate TKI treatment failure in the patient that had that variant; empty circles indicate successful response. The right bee swarm plot shows the BCR-ABL transcript reduction level for patients without extra mutations. Each dot indicates an individual patient. The boxes on the far right indicate the number of patients within each decade of TKI response colored by pattern (patients with both pattern 2 and pattern 3 mutations are labeled here as pattern 2).
Pattern 3: Mutation dynamics of Ph+ clone
The 17 mutations of pattern 3 in 15 patients have VAFs that rise significantly at the time of initial diagnosis and vanish or decrease following TKI therapy. Two patients with pattern 3 mutations also had pattern 2 mutations. Preleukemic mutations were more frequently detected in the T-cell samples of patients with pattern 3 mutations than in the rest of the cohort, at 27% (4 of 15 patients) vs 7% (6 of 85 patients; P = .038 by Fisher exact test). Because TKI targets the BCR-ABL oncoprotein, these mutations are likely to concurrently exist in Ph+ clones as well as Ph− clones in some cases. As such, there is a linear relationship between the rate of allelic burden and BCR-ABL reduction rate for most pattern 3 mutations in responsive patients. However, DNMT3A-I705T from patient 15 was detectable with a moderate VAF (14.79%) at follow-up even though the patient showed successful response to TKI therapy (BCR-ABL measured at 0.12% at follow-up), suggesting its presence in a Ph− clone as well. Most notably, their clinical outcomes were diverse: 6 of the 15 patients responded well to TKI treatment whereas the other 9 cases did not have a meaningful response to treatment (Figure 3). Unlike pattern 1 and 2 mutations, pattern 3 mutations were frequently within genes associated with chromatin modification and DNA methylation, which are epigenetic regulation pathways (11 of 17, 64.7%).
Patterns 4 and 5: Two patterns characterized by the presence of preleukemic mutations
The common trait of pattern 4 and 5 mutations was the presence of mutations in T-cell samples with high relative VAFs. These mutations were likely early events that preceded CML leukemogenesis, which are more directly measurable than the preleukemic mutations implied by mutation persistence alone (ie, pattern 1). All 5 mutations from 5 patients were located in genes associated with epigenetic regulation (4 in TET2 and 1 in ASXL1). The mutations of both patterns plateaued at the time of diagnosis (average change in VAF between T-cell and diagnosis samples of <5%). The patterns were distinguished from each other by persistence (pattern 4) or clearance (pattern 5) at follow-up. The small number of patients exhibiting mutations with these patterns makes generalization difficult, however, the presence of preleukemic mutations in the Ph+ clone at least did not have an obvious effect on treatment outcomes (3 responsive and 2 resistant patients).
Mutations in genes associated with epigenetic regulation pathways
Because 11 of the epigenetic pathway regulation mutations belonged to pattern 3, and 5 more belonged to the other 2 mixed-outcome groups, patterns 4 and 5, we compared the treatment outcomes of patients with these mutations at diagnosis to the rest of the cohort (Figure 4). Patients with mutations in epigenetic regulation pathways at diagnosis had a significantly lower response to TKI therapy, regardless of mutation clearance by the follow-up (Fisher exact test, P = .02 for CCyR by 12 months, P = .04 for MMR by 24 months, and P = .03 for MR4.5 by 36 months, respectively).
Presence of mutation in genes associated with epigenetic regulation confer poor long-term TKI response. Barplots comparing percentage of patients that successfully achieve 3 treatment response milestones (1 per barplot) in patients that had mutations in genes associated with epigenetic regulation (DNA methylation and chromatin modifiers) vs all other patients.
Presence of mutation in genes associated with epigenetic regulation confer poor long-term TKI response. Barplots comparing percentage of patients that successfully achieve 3 treatment response milestones (1 per barplot) in patients that had mutations in genes associated with epigenetic regulation (DNA methylation and chromatin modifiers) vs all other patients.
Multivariate analysis revealed that the presence of mutations in epigenetic regulators at the time of diagnosis predicted poor response to TKIs independent of other clinical factors with respect to CCyR at 12 months (P = .015; odds ratio, 0.204; 95% confidence interval, 0.057-0.737) (supplemental Table 4).
Pattern 0: Patients without mutations other than BCR-ABL transcript
Of the 100 patients included in this study, 63 did not carry mutations other than the BCR-ABL fusion transcript. Three additional patients only carried 1 synonymous mutation each, which did not have a clear influence on TKI response (2 responsive patients and 1 resistant patient). Eight of the 63 patients were in the TKI-resistant group. None were progressed by the time of follow-up.
Discussion
The present study used targeted sequencing on 300 serial samples from 100 CML patients with varying TKI responses to investigate the frequency and dynamics of somatic mutations in genes commonly mutated in other myeloid neoplasms as well as the clinical implications of these mutations on TKI therapy outcomes. Our result showed that longitudinal follow-up of somatic mutations using a custom myeloid gene panel (supplemental Table 1) illustrates a useful genetic spectrum of somatic mutation dynamics during TKI therapy in CML patients as well as providing insight on the origin of mutations.
We tracked the origins of mutational burden as well as its dynamics after TKI therapy using targeted deep sequencing. In our cohort of 100 CML patients, the leukemic cells of 37 patients carried mutations. Among those 37 patients, we identified 5 distinct mutation patterns, for a total of 6 patterns after including the mutation-free pattern (pattern 0). Furthermore, this study also revealed that preleukemic mutations exist in CML patients (16%, 10 of 100 via direct T-cell evidence and an additional 6/100 due to presence in follow-up samples despite significant BCR-ABL reduction), although we could not find a clear association between T-cell presence and TKI therapy response. Four of the 16 patients with preleukemic mutations carried TET2-F868L (3 from pattern 4 and 1 from pattern 5). An additional 2 patients carried the mutation following pattern 2 and pattern 3. It is not obvious whether TET2-F868L is a rare single-nucleotide polymorphism or a somatic mutation because the T-cell VAF was quite high in all 4 from patterns 4 and 5. Further investigation and functional studies would be required in order to reach a clearer conclusion. When analyzing the VAF changes of mutations in conjunction with BCR-ABL transcript reduction, screening serial samples provides in-depth insight into TKI response. Also, longitudinal follow-up of serial samples helped us to track the origin of mutations including preleukemic mutations and mutations that may have been induced or selected for by TKI therapy (pattern 2 mutations).
Changes of VAF in pattern 1 mutations behaved independently of BCR-ABL transcript changes. Pattern 1 mutations are characterized by their persistence at follow-up, although all patients carrying them responded well to TKI therapy and maintained durable response. Interestingly, the genes with pattern 1 mutations have not been commonly reported in CML, suggesting distinct function from mutations originating from Ph+ cells. Only 1 of these cases (CML-26) had a small amount of direct T-cell evidence of preleukemic mutations, which had a low enough T-cell VAF for it to be classified as pattern 1. The remaining 6 cases with pattern 1 mutations can be considered to have indirect evidence of preleukemic mutations (Figure 5). Our results suggest that the presence of pre- and/or non-Ph+ clones does not confer high risk of treatment failure following TKI therapy. Unlike pattern 4 and 5 mutations, pattern 1 mutations were absent in T-cell samples (with the exception of the 1 FANCA mutation from case CML-26), suggesting that these mutations may have occurred after myeloid lineage differentiation. In AML, a recent study showed significant negative association between mutation clearance and risk of relapse.41 In contrast, pattern 1 mutations show that mutation clearance in CML cannot be interpreted the same way without knowledge of the clonal origin of the mutations.
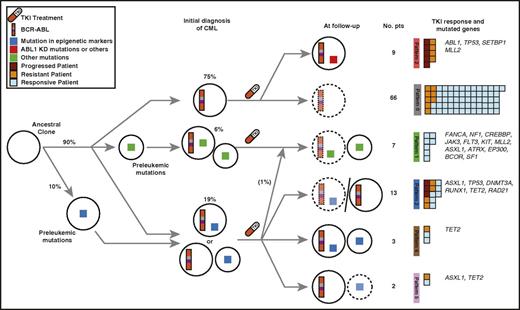
Clonal diversity of CML patients across disease stages. Clonal evolution models per sample stage based on our mutation pattern model. Paired circles indicate separate inferred subclones, with the smaller circle always representing Ph− clones. Dotted lines indicate clones that were successfully treated and remain only in low levels (pattern 3 at follow-up denotes the 2 different clonal scenarios). Boxes on the right are colored to indicate TKI response per patient.
Clonal diversity of CML patients across disease stages. Clonal evolution models per sample stage based on our mutation pattern model. Paired circles indicate separate inferred subclones, with the smaller circle always representing Ph− clones. Dotted lines indicate clones that were successfully treated and remain only in low levels (pattern 3 at follow-up denotes the 2 different clonal scenarios). Boxes on the right are colored to indicate TKI response per patient.
A notable finding of pattern 3 mutations is the high number of mutations in genes associated with epigenetic regulation. There are hints of a correlation between mutation clearance and reduction of BCR-ABL transcript level, but without obvious clinical associations. A larger number of patients with this pattern would be required to reach clearer conclusions of its prognostic implications. Of the 15 patients with pattern 3 mutations at diagnosis of CML, 9 (60%) showed resistance or progression, whereas 6 (40%) achieved good response to TKI therapy, suggesting that the clinical implications of pattern 3 mutations are different from pattern 1 or 2 mutations (Figure 3) in CML patients.
Genes in epigenetic pathways have been reported in healthy individuals without a diagnosis of hematologic malignancies.42-44 Cells carrying them appear to lack measurable morphological characteristics of a myeloid malignancy, but contain recurrent mutations that increase the likelihood of developing overt disease (usually by acquisition of further mutations).42-44 Such preleukemic mutations have been reported in other hematologic malignancies but have not been explored in CML extensively.32,42-47 The present study showed the presence of such mutations in CML patients (16%, 16 of 100 cases) which needs to be confirmed in a larger number of patients and investigated for its clinical relevance. Pattern 1 mutations can be considered indirect evidence of a preleukemic Ph− clone from which the leukemic Ph+ clone evolved (illustrated in Figure 5). One pattern 1 mutation was detected in the patient’s T-cell sample (FANCA-T826M in CML-26 with a VAF of 8.19%). There was no statistically significant response pattern among those 16 patients compared with the other 84. Ten of the 16 patients with preleukemic mutations had their early mutation in epigenetic regulation genes (ASXL1, DNMT3A, KMT2D [MLL2], and TET2). In general, epigenetic regulation genes were also most commonly mutated (57%, 21 of 37 cases), whereas genes associated with the other 6 pathways (activated signaling, cohesion complex, myeloid transcription factors, tumor suppressors, NPM1, and splicing machinery) were rare with the exception of ABL1, an activated signaling gene.
It is unsurprising to find pattern 2 mutations, given existing knowledge of CML patients with ABL1 KD mutation during TKI therapy.39 Another view of pattern 2 mutations is that the absence of mutations (at least using high-throughput sequencing) at diagnosis does not always indicate a higher chance of successful TKI therapy because pattern 2 mutations were absent or undetectable at diagnosis. In line with previous studies, ABL1 KD mutations were exclusive to pattern 2.20,48,49 However, there were 3 patients with pattern 2 mutations that lacked ABL1 KD mutations. Interestingly, there were also 8 TKI-resistant patients among the mutation-free group (pattern 0). Methylation profiling and/or RNA sequencing might help uncover the underlying biology behind the development of their resistance. It is also possible that these patients carry mutations in genes not targeted in our study, which whole-exome sequencing could reveal.
Utilizing mutation dynamics and BCR-ABL fusion transcript reduction level from the present study, we postulate possible clonal development models of CML (Figure 5). Ten cases (10%) had preleukemic mutations in their T-cell samples. Although further functional study is required to investigate the association of these variants with BCR-ABL gene rearrangement, as well as TKI responses, preleukemic mutations in CML are not as rare as might be expected. Six cases (6%) carried preleukemic mutations in the Ph− clone, inferred by the persistence of pattern 1 mutations in spite of successful TKI response. The majority of CML cases (75%, 75 of 100 cases) did not carry any nonsilent mutations other than BCR-ABL at the initial diagnosis. Seven of these patients, as well as 2 who had nonsilent diagnosis mutations, had Ph+ clones that acquired extra mutations by the follow-up time. All 9 did not have a meaningful response to TKI therapy. The overall clinical picture of the quarter of patients with nonsilent diagnosis mutations is not straightforward for patients with pattern 3, 4, or 5 mutations. However, pattern 3 mutations in nonresponsive patients imply the existence of additional somatic mutations in Ph+ clones, often in genes commonly mutated in other myeloid malignancies.
Overall, this study demonstrates that patterns of mutation acquisition, persistence, and clearance vary but have a number of interesting correlations with clinical outcomes. We found that 16% (16 of 100 patients) had evidence of preleukemic mutations, though no clear association between their presence and TKI response was observed. Our data show that mutation burden often persists despite successful TKI response in CML (pattern 1), whereas patients exhibiting mutation clearance (pattern 3) show mixed patterns of clinical outcomes. Patients that acquired new mutations during treatment (pattern 2) all failed TKI therapy. Diverse patterns of somatic mutations in CML patients following TKI therapy is markedly distinct from other hematologic malignancies.
The sequencing data reported in this article have been deposited in the Sequence Read Archive (study accession number SRP090804).
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank John Woolley on the insightful discussion on the manuscript. They also thank 3 reviewers for critical and helpful review on the manuscript.
This work was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT and Future Planning (NRF-2015R1A2A1A10054579) and the Leading Foreign Research Institute Recruitment Program through the NRF, funded by the Ministry of Science, ICT and Future Planning (NRF-2011-0030034). The biospecimens and data used for this study were provided by the Biobank of Chonnam National University Hwasun Hospital, a member of the Korea Biobank Network. T.K. was supported by the Queen Elizabeth II Graduate Scholarship for Science and Technology (University of Toronto).
The funding agencies were not involved in any stage of the study.
Authorship
Contribution: T.K., H.J.K., J.H.L., Z.Z., and D.K. designed the study; J.-S.A., S.H.C., H.J.P., Y.-k.K., and S.Y.K. collected samples and performed experiments; T.K., M.S.T., and Z.Z. analyzed the sequencing data; T.K., Z.Z., and D.K. interpreted the data and statistical analyses; and T.K., M.S.T., H.J.K., J.H.L., Z.Z., and D.K. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Hyeoung Joon Kim, Genome Research Center for Hematopoietic Disease, College of Medicine, Chonnam National University, 322 Seoyang-ro, Hwasun-eup, Hwasun-gun, Jeollanam-do, 519-763, Republic of Korea; e-mail: hjoonk@chonnam.ac.kr; and Zhaolei Zhang, Donnelly Centre for Cellular and Biomolecular Research, University of Toronto, 160 College St, Rm 608, Toronto, ON, Canada, M5S 3E1; e-mail: zhaolei.zhang@utoronto.ca.