Key Points
EPO-EPOR signaling reduces UCB CD34+ HSPC engraftment through inhibition of BM homing and enhancement of erythroid differentiation.
When used in clinical UCB transplantation, HBO therapy is safe and reduces EPO serum levels, potentially improving blood count recovery.
Abstract
Umbilical cord blood (UCB) engraftment is in part limited by graft cell dose, generally one log less than that of bone marrow (BM)/peripheral blood (PB) cell grafts. Strategies toward increasing hematopoietic stem/progenitor cell (HSPC) homing to BM have been assessed to improve UCB engraftment. Despite recent progress, a complete understanding of how HSPC homing and engraftment are regulated is still elusive. We provide evidence that blocking erythropoietin (EPO)-EPO receptor (R) signaling promotes homing to BM and early engraftment of UCB CD34+ cells. A significant population of UCB CD34+ HSPC expresses cell surface EPOR. Exposure of UCB CD34+ HSPC to EPO inhibits their migration and enhances erythroid differentiation. This migratory inhibitory effect was reversed by depleting EPOR expression on HSPC. Moreover, systemic reduction in EPO levels by hyperbaric oxygen (HBO) used in a preclinical mouse model and in a pilot clinical trial promoted homing of transplanted UCB CD34+ HSPC to BM. Such a systemic reduction of EPO in the host enhanced myeloid differentiation and improved BM homing of UCB CD34+ cells, an effect that was overcome with exogenous EPO administration. Of clinical relevance, HBO therapy before human UCB transplantation was well-tolerated and resulted in transient reduction in EPO with encouraging engraftment rates and kinetics. Our studies indicate that systemic reduction of EPO levels in the host or blocking EPO-EPOR signaling may be an effective strategy to improve BM homing and engraftment after allogeneic UCB transplantation. This clinical trial was registered at www.ClinicalTrials.gov (#NCT02099266).
Introduction
Umbilical cord blood (UCB) is a rich source of transplantable hematopoietic stem/progenitor cells (HSPCs) for patients lacking an HLA-matched donor, particularly those in under-represented minorities.1-3 However, UCB units have limited cell doses available for optimal transplantation in adults, sometimes leading to delayed engraftment and higher rates of engraftment failure.4 UCB HSPC bone marrow (BM) homing may also be impaired.5 Current studies to enhance clinical UCB transplantation outcomes have focused on expanding UCB HSPC ex vivo and/or improving their BM homing.2,3,6
Erythropoietin (EPO) affects the fate of hematopoietic progenitor cells (HPCs) in favor of erythroid differentiation.7 In addition, circulating HPCs rapidly decline after birth,8,9 which has been shown to coincide with a decrease in EPO blood concentration.9 These findings potentially indicate an opposing relationship between EPO signaling and HSPC BM homing. Therefore, we investigated whether EPO signaling negatively affects the efficiency of UCB CD34+ HSPC transplantation, and if inhibition of EPO signaling would improve BM homing of transplanted HSPCs. Because hyperbaric oxygen (HBO) therapy has been shown to lower EPO levels in healthy volunteers,10 and as in our previous experience, HBO treatment of the host before UCB CD34+ cell infusion was associated with improved engraftment of UCB CD34+ cells in a murine model,11 we examined HBO effects on HSPC differentiation and homing in vivo. In the first in-human clinical trial, HBO treatment of UCB transplantation recipients was well tolerated, significantly reduced serum EPO levels, and resulted in encouraging rates and kinetics of UCB blood count recovery.
Patients and methods
Isolation of CD34+ cells
Freshly obtained human UCB units were immediately processed for CD34+ selection using magnetic beads (details in the supplemental material, available on the Blood Web site). Isolated CD34+ cells were maintained for up to 24 hours in StemSpan media (STEMCELL Technologies, Vancouver, BC, Canada) before testing. Culture media components are detailed in the supplemental material.
Transplantation of NOD/SCID/IL-2Rgcnull (NSG) mice
Institutional Animal Care and Use Committee approval was obtained for all animal experiments. Six- to eight-week-old male NSG mice (Jackson Laboratory, Bar Harbor, ME) were treated with sublethal irradiation 270 cGy). Twenty-four hours later, mice received HBO therapy with 100% oxygen for 2 hours at 2.5 atmospheres absolute. Four hours after the end of HBO treatment, HBO and control mice were infused IV with 1 × 105 UCB CD34+ cells per mouse. Irradiated mice not receiving human UCB CD34+ cells served as negative controls. Mice were killed at various time intervals and the BM and spleens were harvested and processed for studies. For EPO rescue experiments, 200 U EPO (R&D Systems, Minneapolis, MN) was injected intraperitoneally in the EPO-treated mice 24 hours after irradiation.
Fluorescence-activated cell sorting
For assessment of EPO receptor expression, UCB cells were stained with APC- or PE-conjugated anti-human EPOR (Clone 38421; R&D Systems), FITC- or PE-conjugated anti-human CD34 (Clone 581; BD Biosciences), and/or FITC- or PE-conjugated anti-human CD38 (Clone HIT2; BD Biosciences) monoclonal antibodies. Unstained, isotype, and single-color controls were used for optimal gating strategy (for examples of CD34+ CD38– and CD34+ CD38+ gating strategy, see supplemental Figure 1). For gating EPOR+ populations and median fluorescent intensity (MFI) calculations, please refer to the supplemental material. To evaluate engraftment, peripheral blood (PB) and BM samples were stained using PE-conjugated anti-human CD34 (Clone AC136; Miltenyi Biotec, Bergisch Gladbach, Germany). UCB, PB, and BM samples were run on either a LSRII flow cytometer or an LSRFortessa (BD Biosciences), and the data were analyzed using FACSDiva software.
Western blot assay
Enriched UCB CD34+ cells were lysed in Radio-ImmunoPrecipitation-Assay buffer (Sigma-Aldrich, St. Louis, MO), and proteins were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and then transferred onto an Immobilon polyvinylidene difluoride (PVDF) membrane. The PVDF membranes were probed with PE-conjugated anti-human EPOR MAb (Clone 38421; R&D Systems). Secondary horseradish peroxidase–conjugated anti-mouse IgG (No. 7076, 1:40 000; Cell Signaling) was used with SuperSignal Sensitivity Substrate (Pierce) to enhance the image.
RNA interference and UCB CD34+ cell transduction
EPOR mRNA was targeted by lentiviral vectors containing shRNA (clone ID TRCN0000058313, Open Biosystem, mature antisense sequence TTCATTGATGTGGATGACACG) or scrambled shRNA. After 48 hours, UCB CD34+ cells were selected with puromycin. Knockdown analysis and further experiments were performed 3 days post puromycin selection. After 48 hours, transduction efficiency was assessed by fluorescence-activated cell sorting analysis of green fluorescent protein (GFP) expressing UCB CD34+ cells. Flow-sorted GFP+ UCB CD34+ cells were tested in subsequent experiments.
Colony-forming unit assays
Femoral BM of sacrificed mice was harvested and processed.11 BM was suspended in RPMI 1640 with 2% fetal bovine serum (STEMCELL Technologies) and cultured using a MethoCult H4034 Optimum kit (STEMCELL Technologies). 2.5 × 104 cells were plated in 35-mm culture dishes (STEMCELL Technologies) and incubated at 37°C in a humidified, 5% CO2 environment for 10 days. Colony growth was enumerated using an inverted microscope.
Murine serum EPO measurement
PB was harvested from mice for serum isolation. Murine EPO levels were determined by Quantikine enzyme-linked immunosorbent assay (ELISA) (R&D Systems) according to the manufacturer’s recommendations.
Transmigration assay
Chemotaxis assays were performed using Costar 24-well transwell plates with 6.5-mm-diameter inserts and 5.0-μm pores (Sigma-Aldrich) into which the following were added: 650 μL prewarmed (37°C) Iscove Modified Dulbecco Media with HEPES, l-glutamine (Lonza, Walkersville, MD), and 0.5% bovine serum albumin (Sigma-Aldrich) containing either 0 or 125 ng/mL recombinant human stromal cell–derived factor-1 (SDF-1) in the bottom well. The plates were allowed to acclimate at 37°C for 30 minutes before chemotaxis assay. Cells were then suspended at 1 × 105 cells/100 μL in prewarmed media and loaded to the top chamber of the transwell assay unit. The transwell plates were placed in a 37°C incubator (95% humidity, 5% CO2) for 4 hours. After collection from the bottom chambers, percent cell migration was determined by counting both input and output of the specific HSPC population using flow cytometry (LSRFortessa, BD Biosciences). Background migration (cells migrating toward media alone) was subtracted from total migrated cells. To examine the effect of EPO on migration, CD34+ UCB cells were pretreated overnight at 37°C with rhEPO (R&D Systems) at 0, 100, or 200 ng/mL in RPMI 1640 (Lonza) + 10% fetal bovine serum (Fisher Scientific, Waltham, MA) and then washed before being used in the chemotaxis assay. UCB CD34+ cells were treated with EPO 200 ng/mL (R&D Systems) for 24 hours. To examine the direct effects of EPO and EPOR,1 hour before adding EPO, anti-human EPOR neutralizing antibody (500 μg/mL; USBiological, Salem, MA), and anti-human EPO-neutralizing antibody (3 μg/mL; Abcam, Cambridge, MA) were used to separately treat UCB CD34+ cells. Rabbit IgG (R&D Systems) was used as an isotype control. In transmigration experiment using SDF-1 and C57BL/6 murine BM, a transwell set with 8-µm pores (Falcon, Durham, NC) was used and the migrated UCB cells and murine BM collected from the lower chambers were plated for colony-forming unit (CFU) assessment.
Molecular assays
To distinguish human- from murine-derived CFUs, cells were genotyped with species-specific primers targeting the human prostaglandin E receptor 2 (PTGER2) gene region on human chromosome 14q22.12
Clinical study design
Our pilot study was conducted at the University of Kansas Cancer Center (KUCC) between April 2013 and March 2015 investigating the safety and efficacy of HBO in unrelated allogeneic UCB transplantation. The study was approved by the institutional review board at the University of Kansas Medical Center and registered at ClinicalTrials.gov (#NCT02099266). All patients gave written informed consent for their testing and for their data to be obtained in accordance with the Declaration of Helsinki.
Patient eligibility
Patients 17 to 70 years of age with a hematologic malignancy for which allogeneic UCB transplantation was indicated were eligible. (Inclusion/exclusion criteria are included in the supplemental material).
HBO treatment and transplant
Subjects included in the study received either a myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) regimen of fludarabine/cytoxan/total body irradiation (supplemental Figure 2A). On day 0, subjects were exposed to HBO for 90 minutes after compression to 2.5 atmospheres absolute in a monoplace hyperbaric chamber (Model 3200/3200R, Sechrist Industries, Inc.), breathing 100% oxygen (treatment details are in the supplemental material). Six hours after the start of HBO therapy, patients received single- or double-UCB unit infusion based on published recommendations (supplemental Figure 2B summarizes the study schema).13 Supportive care measures are also summarized in the supplemental material.
Pilot study assessments
Safety.
Treatment-limiting toxicities, defined in the supplemental material, were assessed 24 hours post-HBO therapy. Any adverse events or severe adverse events were noted and graded using Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Incidence and severity of graft-versus-host disease (GVHD) were recorded according to standard grading criteria.
Efficacy.
Time to neutrophil and platelet recovery and red blood cell (RBC) time to transfusion independency (TTI) were determined (definitions are provided in the supplemental material). Study data were compared with historic data of patients with hematologic malignancies receiving UCB transplantation at our institution between 2008 and 2013.
Serum EPO measurement by ELISA
PB was collected and processed for serum from patients before HBO therapy on day 0, 6 hours (just before UCB infusion), 8 hours (2 hours after UCB infusion), and at 24 and 48 hours from the start of HBO therapy. EPO levels were determined using the Human EPO ELISA Kit (STEMCELL Technologies).
Statistical methods
Data are expressed as mean ± standard error of mean (SEM) and means compared by the Student t test. A P value ≤ .05 was considered statistically significant. Calculations were completed using GraphPad Prism software version 6 (GraphPad Software, Inc.).
For the clinical study, descriptive statistics of patient characteristics and adverse events are reported. The Fisher exact test was used to compare the HBO and control cohort day 100 survival and blood count recovery outcomes. Kaplan-Meier survival curves were generated to display 100-day survival. EPO and continuous measures of time to neutrophil and platelet recovery were assessed using Student t test and paired t tests (the latter for within-subject changes) when normality assumptions were appropriate; otherwise nonparametric analogs (Wilcoxon signed-rank test and the Wilcoxon rank-sum test) were used instead. A P value ≤ .05 was considered statistically significant.
Results
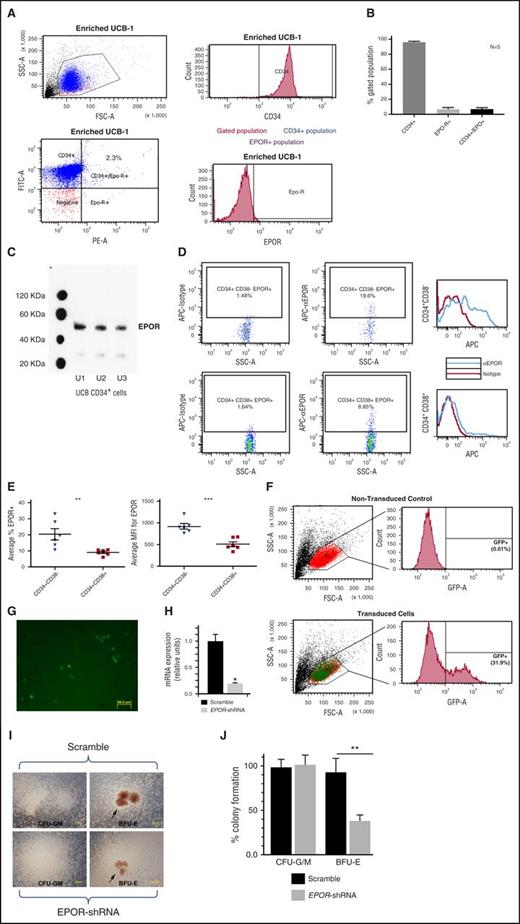
EPOR is expressed on a subset of UCB CD34+ cells and is enriched in CD34+CD38- population
EPOR expression is known to be expressed on the surface of immature erythroid cells.13 However, EPOR expression in the context of purified human UCB CD34+ subsets has not previously been reported. We used flow cytometry and western blot analyses. Analyses of 5 UCB units revealed that an average of 6.5% (SEM 2.6%) CD34+ UCB cells express EPOR (Figure 1A-B); these results were confirmed by western blot (Figure 1C).
EPOR is expressed on a subset of UCB CD34+cells and is enriched in the CD34+CD38–population. (A) Representative flow cytometry data showing EPOR and CD34 expression on UCB CD34+-enriched cells with gating strategy. (B) The percentage of CD34+, EPOR+, and CD34+EPOR+ expression on enriched UCB cells from 5 units with high purity (90% or higher CD34+ cells) by flow cytometry. (C) EPOR expression in enriched cells from 3 UCB units by western blot. (D) Representative flow cytometry data showing EPOR expression on UCB CD34+ cell subsets CD34+CD38– and CD34+CD38–. (E) EPOR expression by cell percentage (left) and MFI (right) on UCB CD34+ subsets. (F) Verification of EPOR shRNA transfection efficiency of UCB CD34+ cells by determining the percentage of GFP+ cells. (G) Micrograph showing GFP-expressing UCB CD34+ cells post lentiviral infection, confirming expression of EPOR shRNAs. Fluorescent images were taken at room temperature using an Olympus IX71 inverted microscope and Olympus DP71 camera. DP controller was used for software acquisition and Adobe Photoshop was used for image processing (scale bar represents 50 µm). (H) mRNA in EPOR knocked down UCB CD34+ relative to control confirming depletion of EPOR by RNAi. (I) Micrographs show formation of hematopoietic cell colonies. Erythroid colonies are shown on the right side with EPOR-depleted UCB CD34+ colonies shown in the right lower corner. Bright field images were taken at room temperature using an Olympus IX71 inverted microscope, 10x objective lens, and Olympus DP71 camera. DP controller was used for software acquisition and Adobe Photoshop was used for image processing (scale bar represents 200 µm). (J) Quantitation of CFU-G/M vs BFU-E colonies with or without EPOR-depletion. Single (*) and double (**) asterisks indicate statistical significance. CFU-G/M, colony-forming units–granulocytes and macrophages.
EPOR is expressed on a subset of UCB CD34+cells and is enriched in the CD34+CD38–population. (A) Representative flow cytometry data showing EPOR and CD34 expression on UCB CD34+-enriched cells with gating strategy. (B) The percentage of CD34+, EPOR+, and CD34+EPOR+ expression on enriched UCB cells from 5 units with high purity (90% or higher CD34+ cells) by flow cytometry. (C) EPOR expression in enriched cells from 3 UCB units by western blot. (D) Representative flow cytometry data showing EPOR expression on UCB CD34+ cell subsets CD34+CD38– and CD34+CD38–. (E) EPOR expression by cell percentage (left) and MFI (right) on UCB CD34+ subsets. (F) Verification of EPOR shRNA transfection efficiency of UCB CD34+ cells by determining the percentage of GFP+ cells. (G) Micrograph showing GFP-expressing UCB CD34+ cells post lentiviral infection, confirming expression of EPOR shRNAs. Fluorescent images were taken at room temperature using an Olympus IX71 inverted microscope and Olympus DP71 camera. DP controller was used for software acquisition and Adobe Photoshop was used for image processing (scale bar represents 50 µm). (H) mRNA in EPOR knocked down UCB CD34+ relative to control confirming depletion of EPOR by RNAi. (I) Micrographs show formation of hematopoietic cell colonies. Erythroid colonies are shown on the right side with EPOR-depleted UCB CD34+ colonies shown in the right lower corner. Bright field images were taken at room temperature using an Olympus IX71 inverted microscope, 10x objective lens, and Olympus DP71 camera. DP controller was used for software acquisition and Adobe Photoshop was used for image processing (scale bar represents 200 µm). (J) Quantitation of CFU-G/M vs BFU-E colonies with or without EPOR-depletion. Single (*) and double (**) asterisks indicate statistical significance. CFU-G/M, colony-forming units–granulocytes and macrophages.
It has been previously reported that EPOR expression in human BM was highest in CD34+CD38– cells, which decreased upon differentiation to CD34+CD38+ cells.14 Similarly, a significantly higher percentage (P = .01) of EPOR-positive cells (20.3% ± 3.2%) were observed within the UCB CD34+CD38– population compared with UCB CD34+CD38+ population (9.02% ± 0.68%) (Figure 1 D-E, left). EPOR expression measured by MFI was significantly higher in the UCB CD34+CD38– population compared with the UCB progenitor-enriched CD34+CD38+ populations (Figure 1E, right). These data support the previous findings in human BM that as UCB CD34+ cells differentiate from CD38– to CD38+ cells, the surface expression of EPOR is decreased.14
To test whether a functional EPO-EPOR signaling cascade was activated in EPOR-expressing UCB CD34+ HSPCs, we next depleted EPOR expression via RNA interference (RNAi) (Figure 1F-H) and compared their erythroid differentiation potential (Figure 1I,J). Depletion of EPOR expression by RNAi greatly reduced the size of erythroid colonies (Figure 1I) and UCB CD34+ differentiation potential toward erythroid burst-forming units (BFU-E) (Figure 1J), indicating that EPO promotes a functional EPO-EPOR signaling response in these cells.
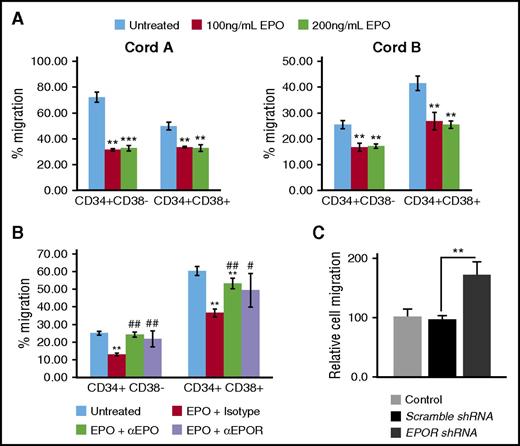
EPO exposure impedes SDF-1–induced migration of UCB CD34+ cells
BM homing of HSPCs is regulated by SDF-1 expressed in the BM niche, and CXCR4 expressed on HSPC.15 Because earlier studies implicated EPO signaling with HSPC homing,9 we tested whether cell EPO-EPOR signaling promotes or abrogates SDF-1–induced migration of UCB CD34+ HSPCs by examining UCB CD34+ cell transmigration toward an SDF-1 gradient after a pre-exposure of the cells to EPO. Exposure of UCB CD34+cells to rhEPO (100 ng/mL or 200 ng/mL) significantly reduced SDF-1–induced directional migration of both CD34+CD38– and CD34+CD38+ populations (Figure 2A). Blocking EPO signaling by using neutralizing anti-EPOR or anti-EPO antibodies rescued SDF-1–induced migration of both UCB CD34+CD38– and CD34+CD38+ populations (Figure 2B). Similarly, EPO-induced inhibition of migration was reversed (Figure 2C) through depletion of EPOR expression by RNAi.
EPO exposure impedes stromal-derived factor-1–induced migration of UCB CD34+cells. (A)The percentage of freshly enriched UCB CD34+ cell subsets CD34+CD38– and CD34+CD38– that migrated toward SDF-1 gradient after culture in erythropoietin at 100 and 200 ng/mL concentrations. (B) UCB CD34+CD38– and CD34+CD38+ populations cell migration toward SDF-1 after incubation with neutralizing EPO (αEPO) and EPOR (αEPOR) antibodies and culture in erythropoietin at 200 ng/mL concentration. (C) The percentage of EPOR-depleted UCB CD34+ cells migrated toward SDF-1 in the presence of erythropoietin at 200 ng/mL concentration relative to control (nontransfected UCB CD34+ cells) normalized to 100%. Two separate UCB units were examined with 3 experimental replicates per cord. The data are presented as mean ± SEM. Single (*), double (**), and triple (***) asterisks indicate statistical significance when compared with untreated. Single (#) and double (##) hatchmarks indicate statistical significance when compared with isotype control.
EPO exposure impedes stromal-derived factor-1–induced migration of UCB CD34+cells. (A)The percentage of freshly enriched UCB CD34+ cell subsets CD34+CD38– and CD34+CD38– that migrated toward SDF-1 gradient after culture in erythropoietin at 100 and 200 ng/mL concentrations. (B) UCB CD34+CD38– and CD34+CD38+ populations cell migration toward SDF-1 after incubation with neutralizing EPO (αEPO) and EPOR (αEPOR) antibodies and culture in erythropoietin at 200 ng/mL concentration. (C) The percentage of EPOR-depleted UCB CD34+ cells migrated toward SDF-1 in the presence of erythropoietin at 200 ng/mL concentration relative to control (nontransfected UCB CD34+ cells) normalized to 100%. Two separate UCB units were examined with 3 experimental replicates per cord. The data are presented as mean ± SEM. Single (*), double (**), and triple (***) asterisks indicate statistical significance when compared with untreated. Single (#) and double (##) hatchmarks indicate statistical significance when compared with isotype control.
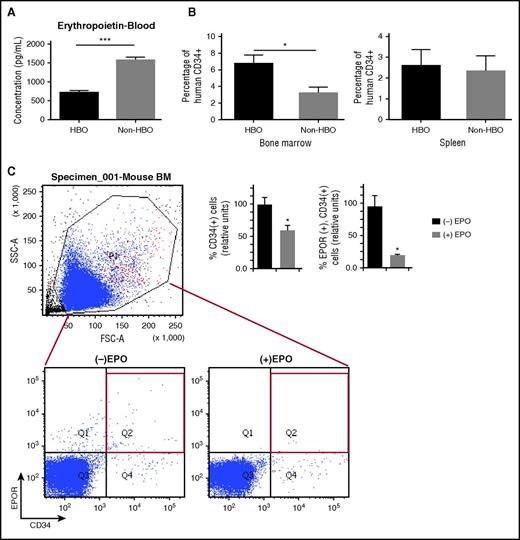
Transient reduction of systemic EPO levels in hosts increases BM homing of UCB CD34+ cells
We recently have shown that HBO treatment of sublethally irradiated immunosuppressed mice before UCB CD34+ cell infusion improved engraftment of cytokine-expanded and gene-transduced UCB CD34+ cells.11 In addition, HBO treatment has been shown to reduce systemic EPO levels in healthy volunteers.10 Because our current in vitro studies indicated that EPO-EPOR signaling inhibits SDF-1–induced migration of UCB CD34+ cells, we examined whether HBO pretreatment of mice before UCB CD34+ infusion would enhance BM homing.
We first measured serum EPO levels in our murine transplant model 7 hours after HBO exposure (or 3 hours post-UCB CD34+ infusion). HBO exposure significantly reduced serum EPO levels compared with controls (Figure 3A). In addition, a higher percentage of the UCB CD34+ cells were present in the BM, but not the spleen, of HBO-treated mice 3 hours post-UCB CD34+ infusion (Figure 3B). To determine the basis of HBO effect on homing as related to EPO, we rescued HBO-treated mice by giving them EPO after HBO treatment. In this experiment, EPO rescue resulted in reduced homing of human UCB CD34+ and CD34+/EPOR+ cells (Figure 3C).
Transient reduction of systemic EPO levels in hosts using HBO increases BM homing of UCB CD34+cells. (A) Serum EPO levels in pg/mL in HBO-treated mice (n = 6) and in non-HBO mice (n = 6) 3 hours after UCB CD34+ cell infusion. (B) Percent of human CD34+ cells in BM and spleen of HBO mice (n = 8) and in non-HBO mice (n = 8) 3 hours after UCB CD34+ cell infusion. (C) EPO rescue effects on UCB CD34+EPOR+ cell homing and engraftment in HBO-treated mice (n = 8). (C, left) Representative flow cytometry data showing dual expression of human CD34+ and EPOR+ in EPO-treated (n = 4) and control mice (n = 4) BM-gated populations. (C, right) Bar graph showing the relative percentage of human CD34+ (hCD34+) and separately human CD34+EPOR+ (hCD34+EPOR+) cells in BM of HBO-treated mice with either EPO treatment (+EPO) or without EPO treatment (–EPO) normalized to 100%. The data are presented as mean ± SEM. Single (*) and triple (***) asterisks indicate statistical significance.
Transient reduction of systemic EPO levels in hosts using HBO increases BM homing of UCB CD34+cells. (A) Serum EPO levels in pg/mL in HBO-treated mice (n = 6) and in non-HBO mice (n = 6) 3 hours after UCB CD34+ cell infusion. (B) Percent of human CD34+ cells in BM and spleen of HBO mice (n = 8) and in non-HBO mice (n = 8) 3 hours after UCB CD34+ cell infusion. (C) EPO rescue effects on UCB CD34+EPOR+ cell homing and engraftment in HBO-treated mice (n = 8). (C, left) Representative flow cytometry data showing dual expression of human CD34+ and EPOR+ in EPO-treated (n = 4) and control mice (n = 4) BM-gated populations. (C, right) Bar graph showing the relative percentage of human CD34+ (hCD34+) and separately human CD34+EPOR+ (hCD34+EPOR+) cells in BM of HBO-treated mice with either EPO treatment (+EPO) or without EPO treatment (–EPO) normalized to 100%. The data are presented as mean ± SEM. Single (*) and triple (***) asterisks indicate statistical significance.
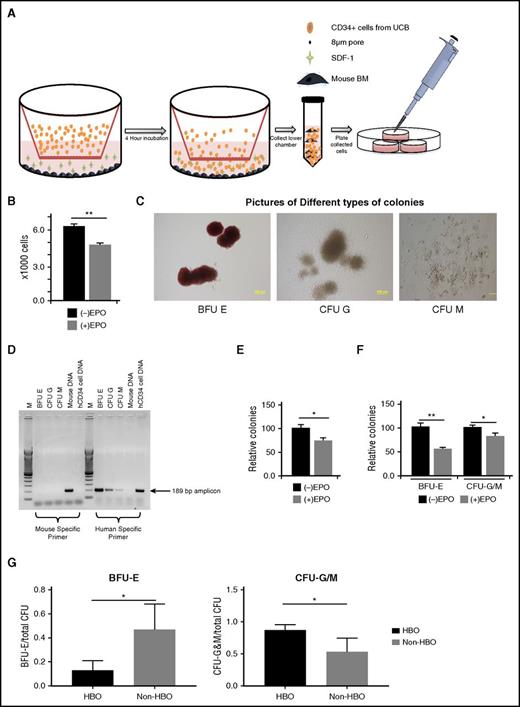
Next, we evaluated the impact of low-EPO host environment on human UCB CD34+ cell differentiation after their transmigration toward SDF-1 in the presence of murine BM cells, a system that closely mimics the host BM environment during HSC homing (Figure 4A). We confirmed that fewer UCB CD34+cells migrated to an SDF-1 gradient after preculture with EPO (Figure 4B). Colonies formed when UCB CD34+ cells combined with murine BM cells were plated for CFU assay (Figure 4C) were entirely human in origin (Figure 4D). Fewer colonies formed when human UCB CD34+cells were pretreated with EPO (Figure 4E). This decrease in colony formation was seen in erythroid and myeloid colonies (Figure 4F).
Low EPO environment enhances myeloid differentiation of UCB CD34+cells in vitro and in vivo. (A) Experimental design of in vitro experiment in which human UCB CD34+ cells migrate toward SDF-1 gradient in the presence of murine BM. The migrated human UCB and murine BM cells are collected and plated for CFU assay. (B) Number of migrated human UCB CD34+ cells in the presence or absence of EPO. (C) Images of types of CFU formed after plating migrated human UCB CD34+ cells and murine BM. Bright field images were taken at room temperature using an Olympus IX71 inverted microscope and Olympus DP71 camera. DP controller was used for software acquisition and Adobe Photoshop was used for image processing (scale bar represents 200 µm). (D) Genomic DNA polymerase chain reaction of 3 types of colonies appeared in methylcellulose medium confirming their human origin. (E) Relative percentage of total colonies formed in the presence of EPO compared with control conditions in the absence of EPO normalized to 100%. (F) Relative percentage of CFU-G/M and BFU-E colonies formed in the presence of EPO compared with control conditions in the absence of EPO normalized to 100%. (G) HBO, as an inducer of low EPO environment, effects on differentiation of transplanted UCB CD34+ cells. BM-isolated mononuclear cells from HBO (n = 3, done in duplicate) and non-HBO mice (n = 3, done in duplicate) 1 week after UCB CD34+ cell infusion were plated and counted. Ratio of BFU-E to total CFU and CFU-G/M to total CFU and in HBO and control mice. The asterisk (*) indicates statistical significance.
Low EPO environment enhances myeloid differentiation of UCB CD34+cells in vitro and in vivo. (A) Experimental design of in vitro experiment in which human UCB CD34+ cells migrate toward SDF-1 gradient in the presence of murine BM. The migrated human UCB and murine BM cells are collected and plated for CFU assay. (B) Number of migrated human UCB CD34+ cells in the presence or absence of EPO. (C) Images of types of CFU formed after plating migrated human UCB CD34+ cells and murine BM. Bright field images were taken at room temperature using an Olympus IX71 inverted microscope and Olympus DP71 camera. DP controller was used for software acquisition and Adobe Photoshop was used for image processing (scale bar represents 200 µm). (D) Genomic DNA polymerase chain reaction of 3 types of colonies appeared in methylcellulose medium confirming their human origin. (E) Relative percentage of total colonies formed in the presence of EPO compared with control conditions in the absence of EPO normalized to 100%. (F) Relative percentage of CFU-G/M and BFU-E colonies formed in the presence of EPO compared with control conditions in the absence of EPO normalized to 100%. (G) HBO, as an inducer of low EPO environment, effects on differentiation of transplanted UCB CD34+ cells. BM-isolated mononuclear cells from HBO (n = 3, done in duplicate) and non-HBO mice (n = 3, done in duplicate) 1 week after UCB CD34+ cell infusion were plated and counted. Ratio of BFU-E to total CFU and CFU-G/M to total CFU and in HBO and control mice. The asterisk (*) indicates statistical significance.
Because HBO lowers EPO levels at the 3-hour time point post transplant, we studied the impact of low EPO environment induced by HBO on human UCB CD34+ cell differentiation. Mice treated with HBO demonstrated significantly lower proportion of BFU-E (P = .043) and an increasing proportion of CFU-G/M (P = .05; Figure 4G) 1 week after transplant, effects not apparent by the second week of transplant (supplemental Figure 3).
Clinical study
By demonstrating the relative safety of HBO along with encouraging in vivo data, we proceeded to test HBO as a modality to improve engraftment in UCB transplantation. The primary objective of the study was safety and tolerability of HBO in the UCB transplantation setting, with a secondary endpoint of assessing the rates and kinetics of neutrophil and platelet engraftment. HBO treatment timing and duration were designed to align with the preclinical murine study.
Patient characteristics
Eighteen patients were screened for this study; 15 were enrolled and treated (Table 1). Patient characteristics including age, diagnosis, preparative regimen, and CD34+ cell dose were comparable with historical controls. However, a greater number of patients in the HBO cohort had single UCB transplantation (8/15) compared with the controls (6/48) (P = .0009).
Safety
Fourteen of 15 treated patients completed the planned HBO therapy. One patient treatment was shortened by ∼10 minutes because of nausea attributed to concomitant medications. Few unexpected complications with an unclear relationship to HBO were reported (details in the supplemental material). All patients experienced grade IV leukopenia. Twelve of 15 patients experienced grade III/IV neutropenia and anemia, and 13 of 15 experienced grade III/IV thrombocytopenia (supplemental Table 1). Frequent and specific severe adverse events (supplemental Table 2) or an unexpected grade III/IV nonhematologic adverse event (supplemental Table 3) were not observed among HBO-treated patients.
Efficacy
Neutrophil recovery.
All patients undergoing HBO treatment demonstrated neutrophil engraftment except for one RIC patient who demonstrated prompt autologous blood count recovery, with neutrophils recovered by day 6 post transplant. Median time to neutrophil count recovery for all patients was 14 days (range 6-45). Median time to neutrophil recovery in patients who received RIC (n = 9) was 7 days (range 6-17) and in MAC patients (n = 6) was 24.5 days (range 16-45) (Table 2). This compares favorably with our historic data, with neutrophil recovery occurring in 42 of 48 (88%) patients with median time to neutrophil recovery of 20.5 days (range 5-71) in all patients, 14 days (range 5-28) in RIC patients (n = 27), and 33 days (range 13-71) in MAC patients (n = 21) (Table 2).
Platelet recovery.
All HBO-treated patients attained platelet recovery. This compares favorably with our historic data because platelet recovery occurred in only 33 of 48 (69%) patients. In HBO-treated patients, median time to platelet count recovery was 37.5 days (range 0-85) for all patients, 32 days (range 0-85) for RIC patients (n = 9), and 54.5 days (range 30-84) for MAC patients (n = 6) (Table 2). These results compare favorably in the case of RIC, but not in the case of time to platelet recovery in MAC, when compared with historic controls, with median time to platelet recovery of 38 days (range 0-161) in all patients (n = 48), 38 days (range 0-112) in RIC patients (n = 27), and 50 days (range 29-161) in MAC patients (n = 21).
RBC recovery.
The average RBC TTI was 33, 24, and 23 days in all, MAC, and RIC HBO patients, respectively. These results compare favorably with control patients whose average RBC TTI was 56, 66, and 45 days in all, MAC, and RIC controls, respectively. These differences demonstrated only a positive trend and did not show statistical significance except in the case of RIC (P = .02).
Chimerism studies in RIC patients
Seven of 9 engrafted RIC patients achieved ≥90% donor chimerism in PB/BM at a median of 19 days (range 15-31) post transplant (supplemental Table 4). Full-donor chimerism was achieved in 7 of 8 (88%) engrafted RIC patients by day +30.
Acute GVHD
Eleven of the 15 (73%) patients developed acute GVHD, with only 9% demonstrating grade III/IV severity (Table 3).
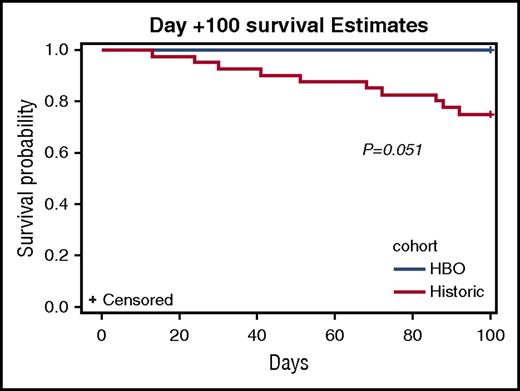
Day +100 post-transplant survival
For all patients, day +100 survival was 15 of 15 (100%) patients in the HBO cohort compared with 34 of 49 (76%) patients in historic cohorts (P = .051) (Figure 5). For MAC patients, day +100 survival was 6 of 6 (100%) patients in the HBO cohort compared with 11 of 21 (52%) patients in the control cohort (P = .03). For RIC patients, day +100 survival was 9 of 9 (100%) patients in the HBO cohort compared with 23 of 27 (96%) in the control cohort (NS).
Day +100 Kaplan-Meier survival curves of HBO-treated patients (blue) compared with historic controls (red).
Day +100 Kaplan-Meier survival curves of HBO-treated patients (blue) compared with historic controls (red).
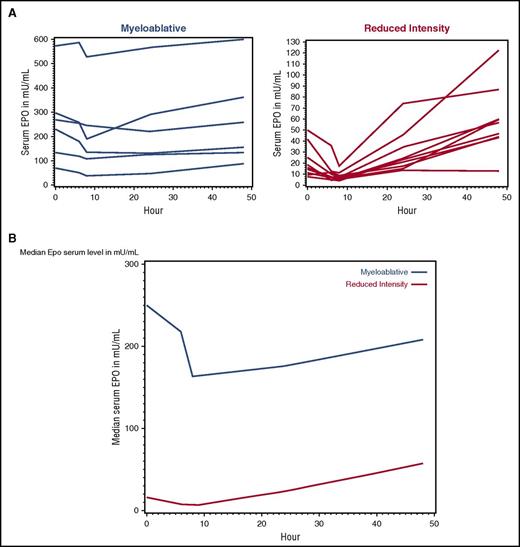
Pre- and post-HBO EPO levels in clinical study patients
EPO levels were reduced in both MA and RIC patients in response to HBO therapy, with the lowest level observed 8 hours after the start of HBO therapy (Figure 6A). Compared with RIC, MAC patients had significantly higher mean baseline EPO levels before transplant (262.1 mU/mL vs 21.5 mU/mL, P = .004) (Figure 6B).
Recipient pretreatment with HBO significantly, but transiently, reduces EPO serum levels at the time of UCB transplantation. (A) Serum EPO levels in mU/mL from individual patients who received myeloablative (blue line) and reduced-intensity preparative regimen (red line) plotted over time (in hours) from the start of HBO therapy. (B) The median serum EPO levels (mU/mL) in myeloablative (blue line) and reduced-intensity preparative regimen (red line) are plotted over time (in hours) from the start of HBO therapy. Baseline value (0-hour) was drawn just before HBO therapy. Blood levels were also drawn 6 hours, 8 hours, 24 hours, and 48 hours from the start of HBO.
Recipient pretreatment with HBO significantly, but transiently, reduces EPO serum levels at the time of UCB transplantation. (A) Serum EPO levels in mU/mL from individual patients who received myeloablative (blue line) and reduced-intensity preparative regimen (red line) plotted over time (in hours) from the start of HBO therapy. (B) The median serum EPO levels (mU/mL) in myeloablative (blue line) and reduced-intensity preparative regimen (red line) are plotted over time (in hours) from the start of HBO therapy. Baseline value (0-hour) was drawn just before HBO therapy. Blood levels were also drawn 6 hours, 8 hours, 24 hours, and 48 hours from the start of HBO.
Discussion
In a series of preclinical experiments, we demonstrated that, although EPOR is expressed on a minority of UCB CD34+ cells, it is particularly enriched in the CD34+CD38– population. We also demonstrated that exposure of UCB CD34+ cells to EPO results in decreased migration to an SDF-1 gradient, and conversely blocking EPO/EPOR signaling through the use of neutralizing antibodies to either EPO or EPOR improves UCB CD34+ cell migration. In addition, we showed that a low EPO environment, such as that induced by HBO host treatment, results in decreased erythroid differentiation and an increase in early BM homing of human CD34+cells in an immune-deficient mice model, an effect that was reversed by EPO rescue, suggesting that HBO effects were mediated by EPO signaling. Moreover, HBO pretreatment resulted in relative increases in myeloid differentiation. Also, standard HBO treatment given before UCB transplantation in our clinical trial was safe and feasible. Importantly, HBO significantly reduced EPO blood levels in the treated patients, resulting in improved rates and kinetics of allogeneic blood count recovery and improved early survival.
Our findings demonstrate that EPOR is highly expressed in the UCB CD34+CD38– (HSC/MPP-enriched) population and that the level of expression is lower in the progenitor-enriched CD34+CD38+ population, thus supporting the previous findings in BM HSPC.14
This is the first report to identify the impact of EPO signaling via EPOR on HSPC SDF-1–induced migration and on homing. Our in vitro results suggest that pretreatment of UCB CD34+ cells with EPO impairs UCB CD34+CD38– cell and CD34+CD38+ cell transmigration toward an SDF-1 gradient. This impairment is reversed by blocking EPO/EPOR signaling or by knocking down EPOR on UCB CD34+ cells. In addition, lowering EPO levels by using HBO, at the time of UCB infusion, improves early UCB CD34+ cell BM homing.
In addition to EPO effects on homing, our data suggest that EPO affects erythroid differentiation of UCB CD34+ cells. Knocking down EPOR on UCB CD34+ cells led to reduced BFU-E, and lowering EPO in recipients led to reduced BFU-E and increased CFU-G/M in our in vivo HBO experiments. Interestingly, we observed a favorable trend in RBC TTI in our pilot study in the case of RIC patients. To reconcile these discrepancies, we point out that HBO effects on EPO and erythroid differentiation in our in vivo experience were transient, yet showed observations of improved homing of undifferentiated UCB CD34+ cells to the bone marrow with unbiased multilineage differentiation; improvement in allogeneic rates and kinetics of blood count recovery in HBO-treated patients was not restricted to one lineage.
HBO treatment effects on EPO levels in the PB and its impact, if any, on the rates and kinetics of allogeneic engraftment and blood count recovery were examined in a clinical UCB transplant setting. Neutrophil recovery was favorable in the HBO cohort compared with our historic cohort, but without statistical significance. A median time to neutrophil recovery of 7 days in our series of RIC compares favorably with data published in a similar contemporary cohort of patients.16 In that report, median time to neutrophil recovery was 15 (range 4-53) days. Although recipient hematopoiesis could have resulted in early hematopoietic engraftment in RIC transplants in our study, full-donor chimerism was achieved in 7 of 8 (88%) engrafted RIC patients by 30 days’ post transplant. These results are favorable given findings from the same study,16 in which only 47% of single-UCB transplant and 77% of double-UCB transplant recipients achieved full-donor chimerism at day +30.
Platelet recovery is delayed in UCB transplantation with a median time to untransfused platelet count of >20 K/UL of 38 to 91 days.17-21 Only 69% of UCB transplant patients achieve platelet independence by 6 months’ post transplant.22 We observed favorable rates and kinetics of platelet recovery in HBO-treated patients because all HBO-treated patients demonstrated platelet transfusion independence compared with 85% observed in historic controls. Also, the median time to platelet count recovery in the RIC cohort was 33 days, comparing well with historic data (38 days) and with a contemporary published cohort whereby platelet recovery occurred at a median of 36 days.16 In that study, only 62% of patients achieved platelet count recovery by 180 days’ post transplant. Given the limitations in interpreting single-arm pilot study data compared with historic controls, a prospective randomized study is indicated in light of the favorable preliminary data summarized herein.
In conclusion, lowering EPO levels at the time of UCB CD34+ cell infusion has favorable effects on infused UCB CD34+ cell differentiation, homing, and engraftment. Given the potential benefits of relatively fast recovery and lack of toxicity, transient reduction of systemic EPO via HBO or small-molecule administration may be a reasonable strategy to promote effective engraftment in allogeneic UCB transplantation.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors acknowledge the Flow Cytometry Core Laboratory, which is sponsored, in part, by the National Institutes of Health/National Institute of General Medical Sciences Centers of Biomedical Research Excellence grant P30 GM103326. The human specimens were processed and stored by the Biospecimen Repository Core Facility, The University of Kansas Cancer Center. Finally, we would like to thank Jane Liesveld for her review of the manuscript. This manuscript was reviewed and edited by a technical writer for clarity.
They thank the St. Louis Cord Blood Bank for making umbilical cord blood units available for preclinical studies. They also thank Jeff D. Eskew, Nikhil K. Parelkar, Megan Swink, Dandan Li, Aaron Cheung, Jeff Radel, and Bruce F. Kimler for their direct involvement with these laboratory studies; Linheng Li for his advice regarding the preclinical work; Shana L. Palla and Qing Yu for their help with statistical analyses of clinical study; Mary Eapen for her guidance regarding historic data analysis; Renee Sol, Cristal Hernandez, Jennifer Bunch, Stacey Supancic, Anthony Arnone, and Kelly Daniels from the Cancer Center Clinical Trial Office for their help with patient screening, enrollment, and data management; the transplant coordinators who helped with patient screening and enrollment; and BM Unit, Hyperbaric Medicine, Radiation Oncology, and Apheresis nurses for their care of the patients treated on study.
This work was supported by a grant from the Office of Scholarly, Academic & Research Mentoring at the University of Kansas Medical Center, a bridging grant from the University of Kansas Medical Centers' Research Institute, by the Robert K. Dempski Cord Blood Research Fund, by a Frontiers Pilot and Collaborative Study grant, and by the Division of Hematologic Malignancies and Cellular Therapy at the University of Kansas Medical Center. Additionally, this work was partly supported by the Southwest Oncology Group/Hope Foundation grant (O.S.A.); and the National Institutes of Health, National Cancer Institute (K23CA158146) (T.L.L.), National Heart, Lung, and Blood Institute (grants HL056416 and HL112669) (H.E.B.), and National Institute of Diabetes and Digestive and Kidney Diseases (grants U54DK106846 [H.E.B.] and T32 DK07519 [H.E.B. and M.L.C.]).
Authorship
Contribution: O.S.A., S.P., G.V., M.L., and H.E.B. designed the preclinical experiments; O.S.A., D.A., A.C., J.D.M., and J.P.M. designed the clinical study; A.G., G.V., M.L.C., A.W., and A.B. performed the laboratory experiments; O.S.A., T.L.L., S.G., A.K.S., C.L., S.A., D.A., L.S., and J.P.M. performed the clinical research; O.S.A., T.L.L., B.L., S.P., M.L.C., H.E.B., A.W., A.G., and M.L. analyzed the preclinical data; O.S.A., T.L.L., B.L., J.D.M., M.L., J.P.M., and A.C. analyzed the clinical data; O.S.A., S.P., A.W., A.B., and M.L.C. wrote the manuscript; and O.S.A., S.P., T.L.L., B.L., M.L., C.L., J.P.M., and H.E.B. reviewed and approved the manuscript.
Conflict-of-interest disclosure: H.E.B. is a member of the medical advisory board of CORD:USE, a cord blood banking company. The remaining authors declare no competing financial interests.
Correspondence: Omar S. Aljitawi, 601 Elmwood Ave, Box 704, Rochester, NY 14642; e-mail: omar_aljitawi@urmc.rochester.edu.