To the editor:
Sickle cell disease (SCD) is caused by a single nucleotide mutation in the β-globin gene resulting in abnormal hemoglobin polymerization and formation of sickle red blood cells. Although vaso-occlusive crises and hemolytic anemia are the primary pathologies, SCD is also associated with chronic vascular inflammation and activation of coagulation.1-3 This hypercoagulable state is characterized by increased tissue factor (TF) expression and elevated levels of thrombin generation measured by thrombin-antithrombin (TAT) complexes.4 We have recently shown that short-term inhibition of all sources of TF in sickle mice attenuates activation of coagulation and reduces endothelial cell (EC) activation and systemic inflammation measured by plasma levels of soluble vascular cell adhesion molecule 1 (sVCAM-1) and interleukin-6 (IL-6), respectively.3 Furthermore, SCD is 1 of a few pathological conditions in which increased TF expression is observed not only on leukocytes but also on ECs,3,5-7 in particular on the pulmonary endothelium.8 Interestingly, we showed that EC-specific deletion of TF significantly attenuated plasma levels of IL-6, but had no effect on thrombin generation or EC activation.3 This surprising result suggests that EC TF is primarily involved in inflammation rather than coagulation in SCD.
TF is constitutively expressed by perivascular cells surrounding blood vessels and parenchymal cells in certain organs.9 During pathologic conditions that result in increased vascular permeability, this nonhematopoietic cellular source of TF will be exposed to circulating clotting factors and could activate the coagulation cascade, as we previously demonstrated in a mouse model of endotoxemia.10 Because increased vascular permeability has been reported in mouse models of SCD,11 we investigated if perivascular cell TF expression contributes to the activation of coagulation in sickle mice. To test this hypothesis, we used so-called “low TF mice” that are completely deficient in mouse TF but express human TF (mTF−/−, hTF+) from a transgene at about 1% of normal levels; heterozygous littermates (mTF+/−, hTF+) were used as controls.12 These mice were transplanted with bone marrow (BM) from either Berkley (BERK) or wild-type (WT) mice, as previously described.3 Importantly, transplantation of both types of BM into low TF mice resulted in the reconstitution of TF expression on all hematopoietic cells and generated mice that express low levels of TF only on nonhematopoietic cells.
Engraftment of the BM was determined by electrophoretic analysis of hemoglobin, as previously described.3 Red blood cell counts, hemoglobin levels, and hematocrit levels were significantly lower, whereas white blood cell counts and plasma levels of lactate dehydrogenase were higher in heterozygous (Het) mice transplanted with BM from BERK mice (BERKBM/Het) compared with these parameters observed in Het mice transplanted with BM from non-sickle controls (WTBM/Het). This demonstrated successful reconstitution with sickle BM. Low level of TF on nonhematopoietic cells did not affect these parameters, indicating no effect on anemia or leukocytosis in sickle mice (Table 1).
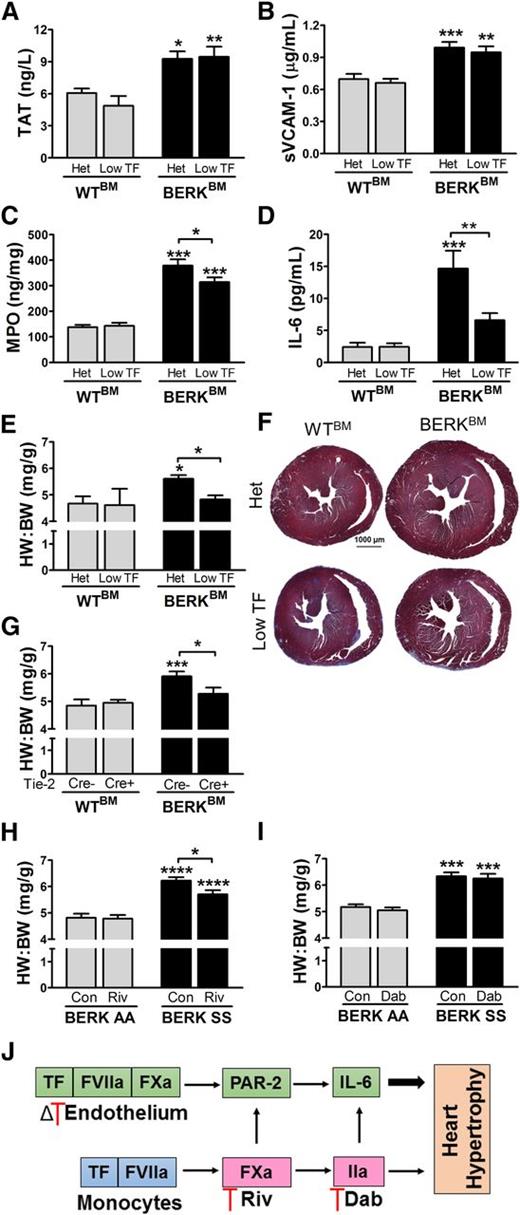
Consistent with our previous studies, plasma levels of TAT, sVCAM-1, and IL-6 as well as levels of myeloperoxidase (MPO) in the lung were significantly elevated in BERKBM/Het mice compared with these parameters observed in WTBM/Het mice (Figure 1A-D); however, low TF expression by nonhematopoietic cells had no effect on TAT or sVCAM-1 in sickle mice (BERKBM/low TF). This suggests that TF expression by nonhematopoietic cells does not contribute to either thrombin generation or EC activation in sickle mice, and, by deduction, these parameters must be driven by TF expressed by hematopoietic cells. Although this hypothesis has to be yet experimentally proven, we speculate that approaches specifically targeting pathological TF expression on hematopoietic cells could attenuate the prothrombotic state in SCD without interfering with hemostasis and increasing the risk of bleeding. The slight attenuation of MPO levels in the lung of BERKBM/low TF mice (Figure 1C) indicates that TF expressed by nonhematopoietic cells can modestly contribute to local lung inflammation independently of any change in systemic thrombin generation.
Eight-week-old heterozygous (mTF+/−, hTF+) and low TF (mTF−/−, hTF+) female mice were lethally irradiated and transplanted with BM from WT (n = 6-8) and BERK (n = 12) mice. Blood and tissues were collected 4 months after transplantation and assessed for plasma levels of (A) TAT, (B) sVCAM-1, and (C) MPO levels in lung and (D) plasma levels of IL-6. (E) The HW:BW and (F) representative images of hearts from control Het or low TF mice transplanted with BM from either WT (WTBM) or BERK mice (BERKBM). (G) In a separate study, 8-week-old mice (both males and females) with EC-specific deletion of TF (TFflox/flox, Tie 2 Cre+) or controls (TFflox/flox, Tie 2 Cre−) were irradiated and transplanted with WTBM (n = 10-12) or BERKBM (n = 12-13) and HW:BW was determined 4 months later. HW:BW was also assessed in 4-month-old BERK AA (n = 9-10) and BERK SS (n = 10-12) mice (both males and females) that were fed for 10 days with chow containing (H) rivaroxaban (0.2 mg/g chow) or (I) dabigatran (10 mg/g chow), as previously described.2 Data are presented as mean ± standard error of the mean. Asterisks above bars indicate significance vs WTBM or BERK AA within the same genotype or treatment group, respectively. Data were analyzed by 2-way analysis of variance followed by Bonferroni post-hoc analysis: *P < .05, **P < .01, ***P < .001. (J) Proposed model of cell type–specific contribution of TF to vascular inflammation and heart hypertrophy via both thrombin-dependent and thrombin-independent mechanisms. Dab, dabigatran; Δ, deletion; Riv, rivaroxaban.
Eight-week-old heterozygous (mTF+/−, hTF+) and low TF (mTF−/−, hTF+) female mice were lethally irradiated and transplanted with BM from WT (n = 6-8) and BERK (n = 12) mice. Blood and tissues were collected 4 months after transplantation and assessed for plasma levels of (A) TAT, (B) sVCAM-1, and (C) MPO levels in lung and (D) plasma levels of IL-6. (E) The HW:BW and (F) representative images of hearts from control Het or low TF mice transplanted with BM from either WT (WTBM) or BERK mice (BERKBM). (G) In a separate study, 8-week-old mice (both males and females) with EC-specific deletion of TF (TFflox/flox, Tie 2 Cre+) or controls (TFflox/flox, Tie 2 Cre−) were irradiated and transplanted with WTBM (n = 10-12) or BERKBM (n = 12-13) and HW:BW was determined 4 months later. HW:BW was also assessed in 4-month-old BERK AA (n = 9-10) and BERK SS (n = 10-12) mice (both males and females) that were fed for 10 days with chow containing (H) rivaroxaban (0.2 mg/g chow) or (I) dabigatran (10 mg/g chow), as previously described.2 Data are presented as mean ± standard error of the mean. Asterisks above bars indicate significance vs WTBM or BERK AA within the same genotype or treatment group, respectively. Data were analyzed by 2-way analysis of variance followed by Bonferroni post-hoc analysis: *P < .05, **P < .01, ***P < .001. (J) Proposed model of cell type–specific contribution of TF to vascular inflammation and heart hypertrophy via both thrombin-dependent and thrombin-independent mechanisms. Dab, dabigatran; Δ, deletion; Riv, rivaroxaban.
Notably, BERKBM/low TF mice expressed significantly less IL-6 compared with BERKBM/Het mice (Figure 1D). Therefore, a reduction of TF from all nonhematopoietic cells gave a similar result to that observed in sickle cell mice lacking TF specifically in ECs (TFfl/fl, Tie-2 Cre+ mice transplanted with BM from BERK mice, as previously published3 ), and suggests that EC are the primary nonhematopoietic cell source of TF that contributes to IL-6 expression in SCD. Recently, we showed that PAR-2 but not PAR-1 deficiency on nonhematopoietic cells was also associated with lower IL-6 expression in sickle mice.2 Together, these data are consistent with in vitro studies describing PAR-2 activation by the TF/factor (F) VIIa/FXa complex,13 and support the concept that in sickle cell mice this signaling complex induces cellular activation independently of thrombin generation.2,3,14 Future studies should determine the role of TF pathway inhibitor and endothelial protein C receptor in the regulation of TF/FVIIa/FXa complex signaling in sickle mice.15,16
The chronic procoagulant and inflammatory state of SCD results in pathological changes to the cardiopulmonary system.4 A recent study demonstrated that a long-term reduction of prothrombin levels (to 10% to 15% of baseline) protected sickle mice against multiorgan dysfunction and prolonged their survival.17 In addition, several markers of chronic inflammation, including plasma levels of IL-6, were also attenuated in sickle cell mice with low levels of prothrombin. However, it is unclear if the lower incidence of end-organ damage, including pathologic heart remodeling, was due to a reduction of coagulation and/or a secondary reduction in inflammation.
In our study, control mice receiving sickle BM exhibited heart hypertrophy, as demonstrated by an increase in heart weight to body weight ratio (HW:BW) and gross morphological analysis (Figure 1E-G). Importantly, reduction of TF in all nonhematopoietic cells, as well as only ECs, resulted in attenuation of heart hypertrophy in sickle mice (Figure 1E-G). Because thrombin generation was not attenuated in these 2 groups of mice3 (Figure 1A), the data suggest that cardiac changes were thrombin independent. We hypothesize that the attenuation of heart hypertrophy likely results from the lower plasma levels of IL-6, inasmuch as a similar reduction in IL-6 was observed in both BERKBM/low TF and BERKBM/Tie2 Cre+ mice compared with sickle mice with normal TF expression. Indeed, IL-6 triggers hypertrophic growth of cardiomyocytes,18 induces proliferation of cardiac fibroblasts,19 contributes to heart hypertrophy in various mouse models,20-22 and is a marker of cardiovascular disease.23
To further investigate the potential link between IL-6 and heart hypertrophy, we examined HW:BW ratios in BERK sickle (BERK SS) mice that received either FXa or thrombin inhibitors.2 Heart hypertrophy was significantly attenuated by FXa inhibition with rivaroxaban in BERK SS mice (Figure 1H), whereas it was not affected by thrombin inhibition with dabigatran (Figure 1I). Although both rivaroxaban and dabigatran reduced TAT levels in BERK SS mice, only FXa inhibition with rivaroxaban attenuated plasma IL-6 levels.2 We attribute the only modest reduction in HW:BW ratio by rivaroxaban, despite a significant attenuation of plasma IL-6, to the short-term nature of our study (10 days). Together, these data suggest that interventions targeting IL-6 expression will also attenuate heart hypertrophy, independent of an effect on thrombin generation in SCD. Moreover, our data also suggest that the heart remodeling observed in SCD may not only be caused by volume overload or iron toxicity as recently suggested,24 but also by chronic inflammation. Of note, the inconsistency observed between short-term dabigatran treatment in our study and long-term (10 to 12 months) genetic reduction of prothrombin levels17 regarding reduction of IL-6 expression and heart remodeling can be simply explained by the difference in experimental observation periods, as suggested by Arumugam and colleagues.17 Also, it is conceivable that in the short term, treatment with rivaroxaban was more effective than dabigatran because inhibition of FXa reduced vascular inflammation via both PAR-2 and thrombin-dependent mechanisms (Figure 1J). Long-term treatment of sickle mice with both anticoagulants would answer this question.
In summary, we have demonstrated that TF expressed by ECs plays an important role in systemic inflammation and pathological changes in the hearts of sickle mice. Our study adds to a growing body of evidence that targeting the coagulation cascade at an upstream point has beneficial effects in not only reducing the chronic procoagulant milieu, but also vascular inflammation and end-organ damage in mouse models of SCD. Importantly, that TF-dependent effects can be mediated by both thrombin-dependent and thrombin-independent mechanisms should be taken into consideration when selecting the optimal anticoagulant for clinical trials in SCD patients (Figure 1J).
Authorship
Acknowledgments: This work was supported by National Institutes of Health, National Heart, Lung, and Blood Institute grants HL117659 (R.P., N.M., and N.S.K.), F32-HL121990-01 and T32-HL007149 (E.M.S.), and HL096679 (R.P.).
Contribution: E.M.S. performed research, analyzed data, and wrote the paper; P.C. and K.C. performed research; N.M. contributed reagents, analyzed data, and wrote the paper; N.S.K. analyzed data and wrote the paper; and R.P. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Rafal Pawlinski, Division of Hematology/Oncology, Department of Medicine, 120 Mason Farm Rd, 1043 Genetic Medicine Building, Chapel Hill, NC 27599-7035; e-mail: rafal_pawlinski@med.unc.edu.