Abstract

Patients with acute myeloid leukemia (AML) who achieve complete remission (CR) after frontline therapy have better outcomes in terms of relapse-free survival and overall survival than those who fail to achieve CR. Patients that achieve complete remission with incomplete platelet recovery (CRp) have an inferior outcome than those with CR, but better than those with no response (Walter et al, JCO 2010). In the setting of relapsed or refractory patients who receive salvage therapy, responses such as CRp and CR with incomplete blood count recovery (CRi) may be seen more frequently. However the clinical benefit of such responses is not known.
To evaluate if less-than-complete remissions (CRi) after salvage therapy impact overall survival in relapsed or refractory AML patients when compared to complete remission and no response.
We conducted a retrospective analysis of all patients who received salvage therapy (1st and 2nd salvage only) for relapsed or refractory AML at our institution between 2010 and 2012. To assess achievement of response, patients usually have to survive at least 4 weeks as the bone marrow assessment is done at this time. Thus, to adjust for the lead-time bias of patients who achieved any kind of response, only patients who survived at least 4 weeks from the initiation of therapy were included in the analysis. The responses were classified into 3 categories – 1. Complete remission (CR); 2. Incomplete response which includes incomplete blood count recovery (CRi), morphologically leukemia free (MLF), partial response (PR) and 3. No response. Response categories were defined according to the International Working Group response definitions (Cheson et al, 2003).
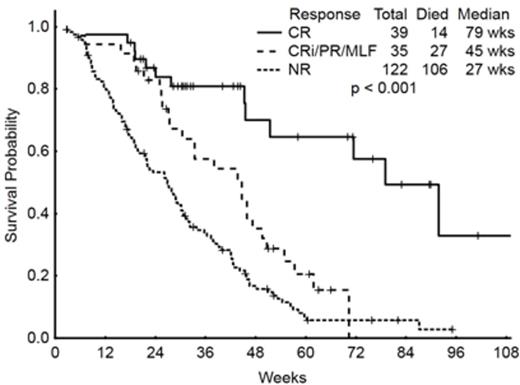
During the observation period, 217 patients received 1st or 2nd salvage therapy. Twenty-one of these patients died before 4 weeks after initiation of treatment and were therefore excluded from this analysis. Median age of all patients was 60 years (18-86). 118 patients had received one prior therapy (i.e., 1st salvage group) while 78 had two prior therapies (i.e., 2nd salvage group). Salvage therapy for this analysis was heterogeneous and was classified into hypomethylating agent based therapy in 23 (12%) patients, high-dose cytarabine (>500mg/m2) based regimens in 133 (68%) patients and various investigational regimens in 40 (20%) patients. The last group included investigational new agents or standard agents (other than hypomethylating or cytarabine) being studied in investigational doses or combinations. Prognostic groups based on cytogenetics showed 11(6%), 25(13%), 71(36%) and 76(38%) patients had favorable, intermediate, diploid and adverse cytogenetics, respectively. In 13 (7%) patients, we had insufficient or no sample for cytogenetics. Thirty-five (18%) were FLT3-ITD positive, FLT D835 point mutation was positive in 10 (5%) patients, 2 patients had both ITD and point mutation and FLT3 status was not available in 8(4%) patients; all others were negative. After salvage therapy, 39 (20%) patients achieved CR at some point in their therapy. CRi/PR/MLF was seen in 35 (18%) patients and remaining had no response. Within the CRi/PR/MLF group, the number of patients achieving CRi, MLF and PR were 28, 6 and 1, respectively. The median survival of all patients was 28.4 weeks. Median overall survival for patients in three groups was 79 weeks, 45 weeks and 27 weeks, respectively (p<0.001). Considering only patients receiving 1st salvage therapy, the median survivals for the three groups were 45.6, 41.0 and 28.9 weeks, respectively. Corresponding values for those receiving 2nd salvage were 42.1, 28.1 and 26.7 weeks, respectively. A total of 62(31%) patients received stem cell transplant out of which 47 (24%) had received it after the salvage therapy. Three patients had received two stem cell transplants and salvage therapy was in between the two. The number of patients receiving transplant in three groups (CR, CRi and no response) were 21 (11%), 16(8%) and 13(7%), respectively.
This analysis suggests that achievement of CRi, MLF or PR in AML patients receiving 1st or 2nd salvage therapy is associated with clinical benefit manifested by improved survival. Although CR still confers the greatest benefit, lesser responses also have a significant impact in survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract