Abstract
Impressive advances in defining the properties of receptors for the Fc portion of immunoglobulins (FcR) have been made over the past several years. Ligand specificities were systematically analyzed for both human and mouse FcRs that revealed novel receptors for specific IgG subclasses. Expression patterns were redefined using novel specific anti-FcR mAbs that revealed major differences between human and mouse systems. The in vivo roles of IgG receptors have been addressed using specific FcR knockout mice or in mice expressing a single FcR, and have demonstrated a predominant contribution of mouse activating IgG receptors FcγRIII and FcγRIV to models of autoimmunity (eg, arthritis) and allergy (eg, anaphylaxis). Novel blocking mAbs specific for these activating IgG receptors have enabled, for the first time, the investigation of their roles in vivo in wild-type mice. In parallel, the in vivo properties of human FcRs have been reported using transgenic mice and models of inflammatory and allergic reactions, in particular those of human activating IgG receptor FcγRIIA (CD32A). Importantly, these studies led to the identification of specific cell populations responsible for the induction of various inflammatory diseases and have revealed, in particular, the unexpected contribution of neutrophils and monocytes to the induction of anaphylactic shock.
Advances in FcγR ligand specificities and expression
Human FcγRs
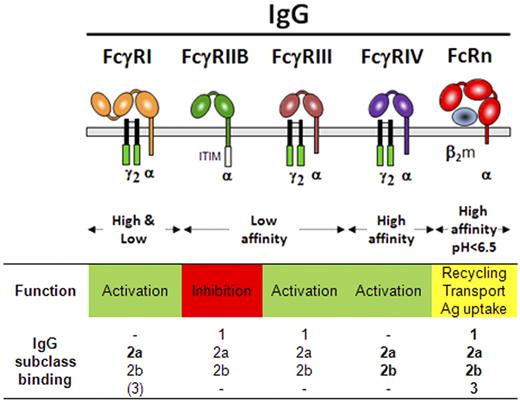
The human IgG receptor family consists of several activating receptors (hFcγRI, hFcγRIIA, hFcγRIIC, and hFcγRIIIA), 1 inhibitory receptor (hFcγRIIB), 1 receptor with unclear functions (hFcγRIIIB),1,2 and 1 receptor (hFcRn) involved in recycling and transport of IgG among other functions3,4 (Figure 1). Activating hFcγRI and hFcγRIIIA requires the association of the FcRγ subunit (Fcer1g) to be expressed and functional at the cell surface. FcRγ indeed contains an immunoreceptor tyrosine-based activation motif (ITAM) that, after aggregation of these latter receptors at the cell membrane, is required for cell activation. hFcγRIIA and hFcγRIIC possess their own ITAM in their intracellular domain and do not associate with the FcRγ subunit.5 hFcγRIIB possesses an immunoreceptor tyrosine-based inhibition motif (ITIM) in its intracellular domain and negatively regulates cell activation and degranulation, cell proliferation, endocytosis, and phagocytosis when coaggregated to an activating FcR.6,7 hFcγRIIB and hFcγRIIC share the same extracellular domain, but hFcγRIIC is expressed by only 20% of persons (FcgR2C-ORF) because of an allelic polymorphism introducing a stop codon in its third exon (FcgR2C-Stop).8,9 In 2007, the characterization of the 2 first human FcγRIIB/C-specific mAbs (clone GB310 and clone 2B611 ) allowed reexamination of the expression patterns of hFcγRIIB, particularly in FcgR2C-Stop persons.
Human IgG receptors. Schematic representation of human IgG receptors at the cell membrane (gray bar) and their association or not to the FcRγ-chain dimer (black). Green boxes represent ITAMs; and the white box, the ITIM. Binding of a human IgG subclass is indicated in bold (high affinity), plain (low affinity), or between parentheses (very low affinity). - indicates no binding.
Human IgG receptors. Schematic representation of human IgG receptors at the cell membrane (gray bar) and their association or not to the FcRγ-chain dimer (black). Green boxes represent ITAMs; and the white box, the ITIM. Binding of a human IgG subclass is indicated in bold (high affinity), plain (low affinity), or between parentheses (very low affinity). - indicates no binding.
Published data using human FcR-specific mAbs can be summarized by the following features: hFcγRI (CD64) is restricted to monocytes/macrophages and dendritic cells (DCs) and, inducibly, expressed on neutrophils12 and mast cells13 ; hFcγRIIA (CD32A) is expressed on all myeloid cells but not on lymphocytes; hFcγRIIB (CD32B) is highly expressed only on circulating B cells11 and basophils (L. Cassard, F. Jönsson, S. Arnaud, P.B., M. Daëron, manuscript submitted, October 2011), poorly expressed on 20% of the monocytes and 4% of the neutrophils,10,11 and expressed on tissue macrophages and DCs,11 but not on mast cells14 ; hFcγRIIC (CD32C) is expressed on NK cells,8 monocytes, and neutrophils9 ; hFcγRIIIA (CD16A) is expressed on NK cells and monocytes/macrophages; hFcγRIIIB (CD16B) is expressed on neutrophils and, as recently demonstrated, on subsets of basophils.15 These expression patterns highlight that hFcγRIIA is the only activating IgG receptor constitutively expressed by mast cells, basophils, neutrophils and eosinophils. Importantly, human activating IgG receptors may be negatively regulated by hFcγRIIB only on B cells and basophils, but not on mast cells, NK cells, and on most neutrophils and monocytes that do not express this inhibitory receptor. Recently, nevertheless, a novel polymorphism affecting the locus encoding human FcRs has been reported that leads to hFcγRIIB expression on NK cells and has been shown to negatively regulate IgG-induced NK cell activation.9 Finally, hFcRn is expressed on antigen-presenting cells, monocytes/macrophages,16 neutrophils,4 vascular endothelial cells, intestinal epithelial cells, and, importantly, on syncytiotrophoblasts, which allow transfer of IgG from mother to fetus antenatally17 (Table 1). hFcRn was reported not only to transport and recycle IgG but also to transport IgG-bound antigens favoring antigen presentation and subsequent immune responses,3 and to enable phagocytosis of IgG-opsonized bacteria by neutrophils.4
We have recently reanalyzed the ligand specificity of hFcγRs using both Surface Plasmon Resonance on soluble hFcγRs (Table 2) and flow cytometry on a collection of transfectants expressing similar levels of hFcγRs.18 Polymorphic variants were included in this analysis when the mutation was in the extracellular domain of the receptors: hFcγRIIA variants H131 and R131; hFcγRIIIA variants F158 and V158; hFcγRIIIB variants NA1 (R36 N65 D82 V106), NA2 (S36 S65 N82 I106), and SH (S36 S65 D78 N82 I106). We found that IgG1 and IgG3 bound to all hFcγRs, IgG2 bound not only to hFcγRIIA but also to hFcγRIIIA(V158), and, unexpectedly, IgG4 had several receptors: hFcγRI, hFcγRIIA, hFcγRIIB, hFcγRIIC, and hFcγRIIIA(V158) (Table 2). Polymorphisms within the extracellular domain affected binding properties for only IgG1 and IgG2, and hFcγRIIA and hFcγRIIIA, but not hFcγRIIIB.18 The identification of receptors for IgG4 is of importance. IgG4 was, indeed, considered a “neutral” IgG isotype because it does not bind complement and was thought not to bind hFcγRs.19 Indeed, IgG4-based therapeutic antibodies have been designed based on this assumption, for example, natalizumab (anti–VLA-4), gemtuzumab (anti-CD33),20 and TGN1412 (anti-CD28); the 2 latter drugs have now been withdrawn from the market. Notably, hFcγRI was found to be a high-affinity receptor for IgG4.18 The capacity of hFcγRI to bind IgG1, IgG2, and IgG4 with high affinity was proposed to rely on the third extracellular domain (unique to FcγRI).12 However, recent crystallographic data suggest that this capacity is the result of a shorter loop between the F and G β-sheets (FG-loop) in the second extracellular domain of hFcγRI, compared with low-affinity hFcγRs.21 Of note, the high-affinity IgG receptor hFcRn22 is quite dissimilar from hFcγRI in that hFcRn binds IgG through the CH2-CH3 hinge region of IgG1, IgG2, IgG3, and IgG423 only at acidic pH (pH 6-6.5), hFcRn is structurally related to MHC class I molecules and hFcRn expression requires association to β2-microglobulin.17
Mouse FcγRs
In 2005, the characterization of a novel activating mouse IgG receptor, FcγRIV, was reported24 that subsequently led to a profound reanalysis of mouse FcR ligands and expression patterns. FcγRIV exists in rodents (mouse, rat, hamster)25 and in some nonhuman primates (macaque, gibbon, orangutan) but not in others (gorilla, chimpanzee), and importantly not in humans (J. Lejeune, B. Piégu, P. Gaudray, M. Ohresser, H. Watier, manuscript submitted, April 2012). FcγRIV, like the 2 other mouse activating IgG receptors, FcγRI and FcγRIII, requires the association of the FcRγ subunit to be expressed and functional at the cell surface.5 FcγRIV is a high-affinity receptor for mouse IgG2a and IgG2b, as it binds monomers of both IgG subclasses.26 FcγRIV has, however, no affinity for mouse IgG1 or IgG3. FcγRIV has therefore a distinct IgG subclass specificity than other mouse FcγRs: FcγRI is a high-affinity receptor for mouse IgG2a only and a low-affinity receptor for mouse IgG2b26 and IgG327 ; FcγRIII and FcγRIIB, the only inhibitory IgG receptor, are low-affinity receptors for mouse IgG1, IgG2a, and IgG2b1 (Figure 2). It follows that all activating mouse FcγRs (FcγRI, FcγRIII, and FcγRIV) bind to IgG2a and IgG2b, whereas FcγRIII is the only activating FcγR binding IgG1 and FcγRI the only activating FcγR binding IgG3. Surprisingly, mouse FcγRIIB, FcγRIII, and FcγRIV, but not FcγRI, were also described to be low-affinity receptors for IgE.26,28 FcγRIIB, FcγRIII, and FcγRIV are therefore IgG and IgE receptors, and FcγRI is a “strict” IgG receptor. Polymorphic variants of mouse IgG receptors have been described for FcγRIIB, haplotypes Ly17.1 (129, NFS, SWR) and Ly17.2 (C57BL/6, BALB/c, DBA/1),29 and for FcγRIII haplotypes T (C57BL/6 and 10), V (SWR), and H (BALB/c, DBA/1, NZB, NZW, NOD, BXSB, MRL/lpr, CBA),30 but no effect on IgG or IgE binding has been reported. Finally, FcRn, the neonatal IgG receptor, is a high-affinity receptor for all IgG subclasses at pH less than 6.5 (Figure 2). FcRn does not directly induce or regulate cell activation but enables IgG protection and recycling,31 transport of IgG, phagocytosis of IgG-opsonized bacteria by neutrophils,4 and protection against bacterial infections,32 as reviewed recently.17
Mouse IgG receptors. Schematic representation of mouse IgG receptors at the cell membrane (gray bar) and their association or not to the FcRγ-chain dimer (black). Green boxes represent ITAMs; and the white box, the ITIM. Binding of a mouse IgG subclass is indicated in bold (high affinity), plain (low affinity), or between parentheses (very low affinity). - indicates no binding.
Mouse IgG receptors. Schematic representation of mouse IgG receptors at the cell membrane (gray bar) and their association or not to the FcRγ-chain dimer (black). Green boxes represent ITAMs; and the white box, the ITIM. Binding of a mouse IgG subclass is indicated in bold (high affinity), plain (low affinity), or between parentheses (very low affinity). - indicates no binding.
Novel specific mAbs generated against mouse FcγRs have facilitated the examination of the expression pattern of FcγRIII and of the newly cloned FcγRIV. Reports in wild-type (WT) mice have described FcγRI to be restricted to monocyte-derived DCs,33,34 FcγRIV to be restricted to Ly6Clo monocytes,35 macrophages, and neutrophils,26 whereas FcγRIIB and FcγRIII were shown to be expressed on all myeloid populations12 ; FcγRIIB is also expressed on B cells and FcγRIII also on NK and NKT cells.36 FcRn is expressed on antigen-presenting cells on neutrophils,4 on splenic monocytes and B cells,37 on the vascular endothelium, and, during the neonatal period, on epithelial cells of the intestine17 (Table 3). Among the newly described FcR-specific mAbs, blocking mAbs were characterized for FcγRIII (clone 275003)38 and FcγRIV (clone 9E9).24 FcγRIIB-specific blocking mAbs (clone K75.325 anti-Ly17.1 haplotype or clone K9.361 anti-Ly17.2 haplotype) were described in the 1980s.29 However, a FcγRI-specific blocking mAb has still not been reported.
Human versus mouse FcγRs
Most human FcγRs bear the same name and CD as mouse FcγRs. They are, however, quite dissimilar in binding abilities and expression pattern. Recent analyses revealed 3 major differences between human and mouse FcγRs binding abilities: (1) all human activating FcγRs bind the major human IgG subclass IgG1,18 whereas only mouse activating FcγR FcγRIII binds mouse IgG126 ; (2) human inhibitory hFcγRIIB has a lower affinity for IgG1, IgG2, and IgG3 than all other hFcγRs,18 which is not the case in mice for IgG1 and IgG2b24 ; and (3) no human FcγR binds human IgE,18 whereas 3 of the 4 mouse FcγRs (FcγRIIB, FcγRIII, FcγRIV) bind mouse IgE.26,28 Interestingly, mouse FcγRs and FcRn efficiently bind human IgG subclasses, whereas human FcγRs and FcRn do not or poorly bind mouse IgG subclasses. For example, human FcγRI binds mouse IgG2a and IgG2b, but not mouse IgG1 (D. A. Mancardi, M. F. Albanesi, F. Jönsson, B. Iannascoli, N. V. Rooijen, X. Kang, M. Daëron, P.B., manuscript in preparation), human FcγRIIA binds mouse IgG1, 2a, and 2b, but not mouse IgG3, and human FcγRIIIB does not bind mouse IgG.38 Notably, human FcRn has no affinity for mouse IgG1, but its low affinity for mouse IgG2a and IgG2b39 is sufficient to restore a mouse IgG2-dependent autoimmune arthritis in a transgenic mouse model (mice deficient for FcRn and transgenic for hFcRn).40,41 Major differences between human FcγR expression patterns and that of their mouse homolog also exist: (1) the expression of mouse, but not human, FcγRI is restricted to monocyte-derived DCs; (2) the expression of human, but not mouse, FcγRIIB is mainly restricted to B cells and basophils; (3) the expression of human FcγRIIIA, but not mouse FcγRIII, is restricted to NK cells and monocytes/macrophages; (4) FcγRIV exist in mice but not in humans24,25 ; and (5) FcγRIIA, FcγRIIC, and FcγRIIIB exist in humans but not in mice.12 FcγR homologs between humans and mice may thus be defined based on expression and ligand binding, rather than on amino acid similarity. Illustrating this concept, when binding IgG, mouse FcγRIV was proposed to be a “functional” homolog of human IgG receptors hFcγRIIIA24,42 or hFcγRI (D. A. Mancardi, M. F. Albanesi, F. Jönsson, B. Iannascoli, N. V. Rooijen, X. Kang, M. Daëron, P.B., manuscript in preparation). Furthermore, when binding IgE, mouse FcγRIV was proposed to be a “functional” homolog of human IgE receptor FcϵRI.26
Advances in the roles of FcγRs in antibody-mediated pathologies
Several IgG-mediated mouse models of inflammatory disease have been recently used to address the properties of FcγRs in vivo. The identification of mouse FcγRIV as a novel activating IgG receptor24 led, indeed, to readdress the contributions of mouse activating IgG receptors FcγRI and FcγRIII. Data are summarized in the next 2 sections from models of inflammatory diseases that highlight the contribution of this novel IgG receptor in inflammatory reactions.
Data using FcγR-deficient mice
Mice deficient for the FcRγ subunit (FcRγ−/− mice) that is required for all activating FcγRs to be expressed and functional were reported as early as 1994.43 These mice lack expression of FcγRI, FcγRIII, and FcγRIV (and FcϵRI)1 but present also multiple non-FcR–related abnormalities. The FcRγ-chain is, indeed, also required for the expression of macrophage-inducible C-type lectin (Mincle)44 and osteoclast-associated receptor (OSCAR),45 and contributes to the signal transduction of several other molecules. FcγRIIB−/− mice were reported in 1996,46 FcγRIII−/− mice in 199647 and 1999,48 FcγRI−/− mice in 2002,49,50 FcRn−/− in 2003,51 and, finally, FcγRIV−/− mice in 2010.52 Notably, FcγRIIB−/− (P.B., unpublished data, August 2003) and FcγRIII−/−,38,52,53 but not FcγRI−/− mice, exhibit increased expression of FcγRIV compared with WT mice. No significant variation in the expression of other FcγRs has been reported in these mice. Studies using FcγRI−/− mice have reported FcγRI to contribute to IgG2a-induced models of type I and II hypersensitivity (passive systemic anaphylaxis [PSA]) and experimental autoimmune hemolytic anemia, respectively), to collagen-induced arthritis50 and to reversed passive Arthus reaction.49 Studies using FcγRIIB−/− mice have reported that FcγRIIB negatively regulates inflammatory and hypersensitivity reactions in several autoimmune, allergic, and inflammatory models, as exhaustively reviewed recently.7 Studies using FcγRIII−/− mice have reported that FcγRIII triggers Arthus reaction and passive cutaneous anaphylaxis (PCA),47 IgG1-induced PSA,38,54 K/BxN arthritis,55,56 and collagen-induced arthritis.57 A study using FcγRIV−/− mice reported that FcγRIV triggers experimental nephrotoxic nephritis.52 Finally, studies using FcRn−/− mice reported that: (1) FcRn binds and prolongs the life span of IgG and albumin51 ; (2) FcRn is essential for the induction of K/BxN arthritis58 ; and (3) FcRn is required for efficient phagocytosis of IgG-opsonized bacteria by FcγRs.4 This latter unexpected property of FcRn may explain why cells that do not express FcRn (eg, NK cells) are incapable of phagocytosis after engagement of activating FcγRs.
Although inhibitory FcγRIIB was considered to be the main FcγR involved in the anti-inflammatory effects of intravenous immunoglobulin,56,59,60 FcRn58 and FcγRIII61-64 have also been reported to be involved/mandatory. Indeed, an increasing number of reports have revealed that activating FcγRIII mediates the anti-inflammatory effects of intravenous immunoglobulin in experimental thrombocytopenia when expressed on DCs61 or on macrophages,62 in allergic airway inflammation when expressed on NKT cells,63 and in a nonimmune inflammation model of obstructive nephropathy.64
Using knockout mice for a particular FcR was for a long time considered the standard approach to address the function of a particular FcγR in vivo (ie, by studying the effect of its absence). Recently, however, the generation of multiple FcR-knockout mice has enabled the study of a particular FcR in the absence of most/all other FcRs. FcγRI/IIB/III-triple knockout (3KO) mice, lacking 3 of the 4 mouse FcγRs, were indeed described to retain the ability to develop collagen-induced arthritis after immunization with bovine collagen type II in Freund adjuvant.65 Because these mice express only FcγRIV as an activating IgG receptor, it was deduced that FcγRIV contributes to collagen-induced arthritis. These mice, nevertheless, express the high-affinity IgE receptor FcϵRI that may also contribute to collagen-induced arthritis, as immunizations in Freund adjuvant leads to antigen-specific IgG but also IgE production.38 FcγRI/IIB/IIIA FcϵRI/II-quintuple knockout mice, which do not express FcγRs or FcϵRs other than FcγRIV (5KO, also known as “FcγRIV-only”), were subsequently generated and have circumvented this potential issue. Using “FcγRIV-only” mice we reported that FcγRIV induced arthritic inflammation in the passive K/BxN model of arthritis66 in the presence of IgG2-immune complexes.41 These results are in agreement with those obtained when inducing collagen-induced arthritis in 3KO mice.65 “FcγRIV-only” mice also developed lung inflammation after activation of alveolar macrophages in the presence of IgE-immune complexes,26 and experimental thrombocytopenia induced by antiplatelet mouse IgG2a mAbs.38 Furthermore, using FcγRI/IIB/III FcϵRI/II FcRn-sextuple knockout (6KO) mice, we have reported that FcγRIV-dependent induction of K/BxN arthritis requires FcRn, probably to transport pathogenic IgG2 antibodies to the joints and to protect these antibodies from degradation.41
These analyses using “FcγRIV-only” mice, have not yet been performed using “FcγRI-only” or “FcγRIII-only” mice to evaluate their contribution to the induction of inflammatory models. “FcγRIII-only” mice may not be particularly worthy to generate because FcγRIII is the only activating IgG receptor that binds IgG1. Disease models that rely on pathogenic antibodies of the IgG1 subclass depend therefore on FcγRIII. “FcγRI-only” mice may be worth generating because FcγRI, like FcγRIV, binds mouse IgG2a and IgG2b.24,26 FcγRI and FcγRIV may play redundant roles that may explain why studies using FcγRI−/− mice have not reported a contribution of FcγRI to K/BxN arthritis56 or to experimental thrombocytopenia after injections of IgG2b antiplatelet antibodies for example.24 “FcγRI-only” mice may, however, reveal the contribution of FcγRI to these and/or other models that may be undetectable when FcγRIV is coexpressed with FcγRI. Of note, FcγRI is reported to be expressed in unchallenged mice only on DCs33 and, among DC subsets, specifically on monocyte-derived DC subsets, as recently shown in the muscle tissue and its draining lymph nodes.34
Data using anti–mouse FcγR blocking mAbs
Using specific blocking mAbs has proven efficient to analyze the properties of a particular FcR in vivo in WT mice without necessitating simple or multiple FcγR knockouts. Specific in vivo blocking abilities of mAbs were, indeed, described for FcγRIIB in 2001,29,59 for FcγRIII in 2011,38,41 and for FcγRIV in 2005.24 Unfortunately, no blocking mAb exists for FcγRI. WT mice treated with anti-FcγRIII mAbs have shown that FcγRIII contributes to K/BxN arthritis,41 to active systemic anaphylaxis (ASA), and is mandatory for IgG1-induced PSA.38 WT mice treated with anti-FcγRIV mAbs have revealed that FcγRIV contributes to experimental thrombocytopenia,24 K/BxN arthritis,41 and ASA and is mandatory for IgG2b-induced PSA.38 WT mice treated with a combination of anti-FcγRIII and anti-FcγRIV mAbs have revealed that these receptors are, together, responsible for K/BxN arthritis41 and for ASA.38 That these receptors are responsible for the induction of K/BxN arthritis is in agreement with previous reports using knockout mice.52,55,56 However, that these receptors are responsible for the induction of ASA is unexpected. Altogether, these results in WT mice validate and extend the results obtained using single or multiple FcR-deficient mice. Therefore, using specific blocking anti-FcR mAbs in WT mice will certainly become the method of choice to study FcR properties in vivo.
Data using FcR-humanized mice
Studying human FcRs in vivo constitutes a major challenge that many have attempted by generating human FcR-transgenic mice. Human FcγRItg mice were reported in 1996,67 hFcγRIIAtg mice in 1999,68 hFcγRIIBtg in 2011,69 hFcγRIIIAtg and hFcγRIIIBtg mice in 1996,70 and hFcRntg in 2003.51 hFcγRIICtg mice have not yet been generated. hFcγRIIAtg and hFcγRIIIBtg mice closely recapitulated their respective expression patterns in humans. Unfortunately, hFcγRI is constitutively expressed on neutrophils in hFcγRItg mice, whereas an inducible expression is reported on human neutrophils.71 hFcγRIIIA and hFcγRIIIB have recently been reported to be both expressed on spleen and circulating DCs, and hFcγRIIIA on eosinophils from hFcγRIIIAtg hFcγRIIIBtg mice72 but are not expressed on these cell populations in humans. hFcγRIIBtg mice have high hFcγRIIB expression on more than 90% mouse monocytes and granulocytes compared with the poor expression on minor fractions of these cell types reported in humans.11 Crossing these transgenic mice together resulted in a mouse model expressing multiple hFcγRs (ie, hFcγRI/IIA/IIB/IIIA/IIIB, except hFcγRIIC and hFcRn) that conserved the original expression patterns of these human transgenes and, unfortunately, also their abnormal expression on several cell populations.72 The in vivo properties of these human FcγRs can, nevertheless, be studied in these transgenic mice, but conclusions on their contribution to disease and therapy models are thus to be drawn carefully to remain meaningful. Another difficulty to analyze the contribution of these receptors to disease and therapy models in FcR-humanized mice comes from the cross-binding of human and mouse IgG to human and mouse FcRs (detailed in “Advances in FcγR ligand specificities and expression”). This cross-binding can potentially lead to a competition in vivo for IgG binding between the transgenic human FcγR and the endogenous mouse FcγR. This phenomenon may also induce the aggregation of receptors originating from different species, which result in artifactual situations. The expression of a supplementary IgG receptor in WT mice, as it is the case when a transgene encodes for a human FcγR, may also lead to adverse reactions. Studies using mice transgenic for hFcγRIIA on a WT background, indeed, reported spontaneous autoimmune diseases (ie, pneumonitis, glomerulonephritis, and rheumatoid arthritis).73 The expression of hFcγRI on a WT mouse background, however, was reported to not lead to adverse reactions. Why a human FcγRIIA encoding transgene, but not a human FcγRI encoding transgene is pathogenic when expressed in vivo in WT mice remains unanswered but may relate to their different expression pattern (Table 1) and/or cross-binding of mouse IgG (detailed in “Advances in FcγR ligand specificities and expression”). hFcγRItg mice have revealed that hFcγRI enables antigen targeting to DCs for enhanced protective immunity67 and IgG-dependent protection against malaria infection.74 In most cases, however, the analysis of the properties of human FcRs in vivo in inflammatory models of disease requires that the transgenes encoding human FcRs are expressed in mice deficient for endogenous FcRs to avoid competition for ligands or artifacts.
For example, hFcγRIIA, which does not require the FcRγ subunit to be expressed and functional (Figure 1), was expressed in FcRγ−/− mice that lack expression of endogenous activating FcγRs (FcγRI, FcγRIII, and FcγRIV). These hFcγRIIAtg FcRγ−/− mice have revealed that hFcγRIIA expression was sufficient to restore IgG-dependent experimental autoimmune thrombocytopenia,68 rheumatoid arthritis,75 and allergic reactions and lung inflammation76 in resistant mice (detailed in “Role of FcγR+ cells in Ab-induced pathologies [eg, arthritis and anaphylaxis]”). The same strategy may be used for the analysis of hFcγRIIB, hFcγRIIC, or hFcγRIIIB that do not require the FcRγ subunit, but not for the analysis of hFcγRI and hFcγRIIIA that require the FcRγ subunit to be expressed and functional. As an alternative to the FcRγ−/− background, we have recently used the multiple FcR-deficient mice we generated (5KO also known as FcγRI/IIB/III FcϵRI/II-deficient mice)26 to express and analyze in vivo hFcγRIIA76 or hFcγRI (D. A. Mancardi, M. F. Albanesi, F. Jönsson, B. Iannascoli, N. V. Rooijen, X. Kang, M. Daëron, P.B., manuscript in preparation) in disease and therapy models. Of note, these mice still express endogenous FcγRIV that may be blocked in vivo using specific blocking mAbs. The recent generation of mice deficient for all endogenous mouse FcγRs and expressing multiple hFcγRs (hFcγRI/IIA/IIB/IIIA/IIIB)72 allowed to study their properties without the interference of endogenous FcγRs or usage of blocking mAbs. These mice confirmed, indeed, the activities reported previously in mice expressing a single hFcγR transgene in models of thrombocytopenia, B-cell depletion, and PSA.68,69,76 Finally, hFcRn was expressed in FcRn−/− mice and revealed that hFcRn prolongs the life span of human IgG40 and albumin,51 enables capture and processing of luminal IgG-bound antigens favoring the adaptive immune response,3 and restores K/BxN arthritis in resistant FcRn−/− mice.41 Most of these analyses were, however, performed in mice expressing only one human IgG receptor and do not recapitulate the complexity of their interactions in the human system. A mouse model expressing the full array of hFcγRs and hFcRn, and lacking all endogenous FcRs, may thus prove an invaluable tool to study human IgG receptor biology, provided that the expression pattern of the human FcRs in transgenic mice reproduces their expression pattern in humans.
Role of FcγR+ cells in Ab-induced pathologies (eg, arthritis and anaphylaxis)
Many attempts have recently been made to determine the cell population(s) responsible for the in vivo properties of a specific FcR in a specific disease model. In this aim, mice deficient for a given cell population are compared with WT mice, or cell-specific depletion is achieved using depleting mAbs or compounds. To illustrate how the recent description of the expression patterns of mouse and human FcγRs, coupled with FcγR-blocking antibodies, cell-depletion experiments, and multiple FcγR-deficient mice, have helped to define the role of FcR-expressing cell populations in disease models, the following 2 sections describe reports on arthritis and anaphylaxis models that have, unexpectedly, demonstrated a major contribution of neutrophils to disease induction.
Arthritis
These approaches described herein were used to analyze the requirement for specific cell subsets in the development of the K/BxN passive arthritis model, which relies on the injection of autoantibody-containing sera from KRNtg C57BL/6 × NOD F1 mice.77 This model was reported to be abrogated in WT mice depleted of monocytes/macrophages78 or depleted of neutrophils.79 This latter result was confirmed by the resistance of Gfi-1−/− mice, which lack mature neutrophils, to develop K/BxN arthritis.80 Further supporting the essential role of neutrophils in K/BxN arthritis, deletion of Syk specifically in neutrophils has been reported to block disease development.81 The contribution of mast cells in this arthritis model, which had originally been suggested by the resistance of mast cell-deficient W/Wv mice82 to develop pathology, has since come under question by our work41 and others81,83,84 using mast cell-deficient Wsh/Wsh mice or Cre-mediated mast cell ablation. Resistance of W/Wv mice to arthritis may indeed rely on the neutropenic state of these mice rather than on their mast cell deficiency, as suggested from another arthritis model.85 The finding that K/BxN arthritis requires monocytes/macrophages and neutrophils, but does not require mast cells, is in agreement with results obtained using multiple FcγR-deficient mice, such as the 3KO (FcγRI/IIB/III-deficient) mice65 or 5KO (FcγRI/IIB/III FcϵRI/II-deficient, also known as “FcγRIV-only”) mice that develop K/BxN arthritis. Indeed, in these mice, K/BxN arthritis was dependent on FcγRIV,41 and FcγRIV is expressed only on monocytes, macrophages and neutrophils.26 Similar results have been reported in a model of collagen-induced arthritis,65 supporting the conclusion that mast cells are not mandatory but may contribute to arthritis in these mouse models. Furthermore, results obtained using human FcR-transgenic mice support these results, as mast cell-deficient hFcγRIIAtg mice (F. Jönsson, unpublished data, September 2011) and hFcγRItg mice (D. A. Mancardi, M. F. Albanesi, F. Jönsson, B. Iannascoli, N. V. Roeijen, X. Kang, M. Daëron, P.B., manuscript in preparation) develop K/BxN arthritis. In these latter mice, K/BxN arthritis was dependent on hFcγRI, and the expression of hFcγRI on effector cells was restricted to monocytes/macrophages and neutrophils. Of note, the deficiency in FcRn was reported to protect mice from experimental arthritis,58 and expressing human FcRn restored K/BxN arthritis in FcRn-deficient mice.41 The FcRn-expressing cell subset that is responsible for disease induction has unfortunately not been identified yet, but the recent generation of conditional FcRn-deficient mice37 might enable investigators to address this question.
Anaphylaxis
Anaphylaxis is a hyperacute allergic reaction that can have fatal consequences. The current paradigm states that anaphylaxis is an immediate hypersensitivity reaction to an allergen/antigen mediated by IgE, resulting in the release of granular mediators by mast cells and basophils in patients sensitized to a particular allergen/antigen. The FcRs and/or cell subsets that were identified to be responsible for anaphylaxis induction are, however, different depending on the experimental protocol used.
IgE-induced PSA.
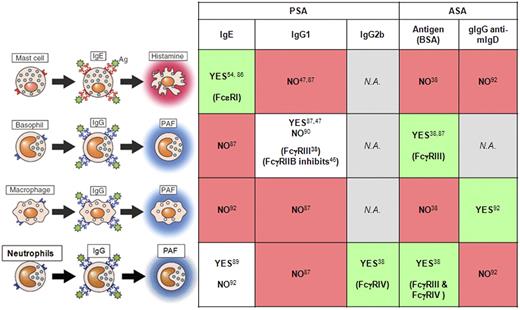
IgE-induced PSA is elicited by injecting WT mice systemically with IgE antibodies 24 to 48 hours before an intravenous challenge with specific antigen. IgE-induced PSA was abrogated in mice deficient for FcϵRI, the high-affinity IgE receptor expressed by mast cells and basophils.86 Notably, it was abrogated in mast cell-deficient W/Wv mice54 but not in basophil-depleted mice.87 It was also abrogated in histidine decarboxylase-deficient mice, which lack histamine,88 and in mice injected with histamine receptor antagonists.89 These findings demonstrate the mandatory role of mast cells, FcϵRI, and histamine in IgE-induced PSA (Figure 3).
Contribution of each pathway in the respective anaphylaxis model. A pathway is represented by a cell type, the antibody class, and the mediator released. Contribution (Yes, green box) or no contribution (No, red box) to a particular anaphylaxis model is indicated. Contradictory results are indicated (white box). If identified, responsible FcRs are indicated between parentheses. N.A. indicates not analyzed. Corresponding references are provided. Adapted with permission from Mukai et al.102
Contribution of each pathway in the respective anaphylaxis model. A pathway is represented by a cell type, the antibody class, and the mediator released. Contribution (Yes, green box) or no contribution (No, red box) to a particular anaphylaxis model is indicated. Contradictory results are indicated (white box). If identified, responsible FcRs are indicated between parentheses. N.A. indicates not analyzed. Corresponding references are provided. Adapted with permission from Mukai et al.102
IgG-induced PSA.
IgG-induced PSA is elicited by injecting mice systemically with IgG antibodies 2 to 3 hours before an intravenous challenge with a specific antigen. Alternatively, preformed IgG immune complexes can be injected intravenously. Similar symptoms, with comparable kinetics, develop during IgE- and IgG-induced PSA. Passively administered IgG1-immune complexes induce anaphylaxis (IgG1-induced PSA) that relied exclusively on FcγRIII.38 IgG1-induced PSA was reported to be negatively regulated by inhibitory FcγRIIB.48 Indeed, FcγRIII and FcγRIIB are the only receptors for mouse IgG1 (Figure 2). Surprisingly, IgG1-induced PSA was not abrogated in mast cell-deficient mice.54 The depletion of monocytes/macrophages, NK cells, or neutrophils had no effect, whereas basophil depletion abrogated IgG1-induced PSA.87 Basophil-deficient mice, however, develop IgG1-induced PSA,90 which is in contradiction with the result obtained after depletion of basophils. Whatever the cell subset involved, the activation of this subset during IgG1-induced PSA should lead to the production of platelet-activating factor (PAF). Indeed, PAF was reported to be responsible for IgG1-induced PSA.87 Passively administered IgG2b-IC also induce anaphylaxis (IgG2b-induced PSA) that relied exclusively on FcγRIV.38 Surprisingly, the depletion of neutrophils was sufficient to abolish IgG2b-induced PSA. IgG2b-induced PSA therefore relies on FcγRIV and neutrophils and is correlated with elevated serum levels of PAF (Figure 3). Passively administered immune complexes made of antigen-specific polyclonal IgG (pIgG) antibodies and antigen also induce anaphylaxis (pIgG-induced PSA). pIgG are essentially of the IgG1 and IgG2a/b subclasses. One may therefore consider that pIgG-induced PSA recapitulates IgG1- and IgG2b-induced PSA. pIgG-induced PSA was reduced after blocking of FcγRIV and was abolished after depletion of neutrophils.38 Therefore, pIgG-induced PSA relies on neutrophils and at least partially on FcγRIV.
ASA.
ASA is elicited by injection of antigen-immunized mice with the same antigen. ASA therefore resemble human anaphylaxis that arises in patients sensitized against a specific antigen/allergen. Unexpectedly, results obtained in ASA models have not correlated well with most results obtained in passive anaphylaxis models. Indeed, neither IgE,91 FcϵRI,54 mast cells, nor basophils86,87 are mandatory for the induction of ASA. ASA even occurred in the absence of both mast cells and basophils.87 In a model of ASA induced by an intravenous injection of goat IgG in mice immunized with goat IgG anti–mouse IgD, the injection of anti-FcγRIIB/III blocking mAb 2.4G2 abolished the reaction, suggesting that FcγRIII is mandatory to induce ASA in this model (GaMD-ASA). Neither mast cells, granulocytes, nor platelets were required, but, surprisingly, blockade of monocyte/macrophage activation abolished the reaction.92 Activation of monocytes/macrophages can result in PAF release93 ; indeed, PAF-R antagonists abolish GaMD-ASA.92 We, however, recently demonstrated that monocyte/macrophages do not contribute to ASA using a different model in which mice are immunized with BSA in Freund adjuvant and challenged with BSA38 (BSA-ASA). Unexpectedly, neutrophils (predominantly) and basophils (modestly) contributed to the shock. As expected,54 ASA occurred in WT mice, but not in FcRγ−/− mice that express no activating IgE and IgG receptors. ASA was abolished in mice injected with anti-FcγRIII and anti-FcγRIV mAbs. Even though antigen-specific IgG and antigen-specific IgE are present in these mice at the time of disease induction, the IgG receptors FcγRIII and FcγRIV are responsible for ASA induction. In agreement with the results obtained in GaMD-ASA,92 PAF receptor antagonists strongly inhibited BSA-ASA.38 Altogether, these data propose on the one hand that macrophages activated after FcγRIII engagement release PAF that is responsible for GaMD-ASA and, on the other hand, that neutrophils (and basophils) activated after FcγRIII and FcγRIV engagement release PAF that is responsible for BSA-ASA (Figure 3). Importantly, the transfer of human neutrophils restored BSA-ASA in anaphylaxis-resistant mice,38 suggesting a role for neutrophils in human anaphylaxis. Supporting this hypothesis, 95% of human neutrophils express only activating IgG receptors (hFcγRIIA and, inducibly, hFcγRI) and, in atopic persons, IgE receptors (FcϵRI),94 but no inhibitory IgG receptor (FcγRIIB).11 Human neutrophils are thus prone to activation after encounter of immune complexes.
Anaphylaxis in FcR-humanized mice.
In 1996, the generation of the first human FcR transgenic mice allowed the investigation of its role in PSA. Indeed, IgE-PSA was restored in mice transgenic for hFcϵRI and deficient for mouse FcϵRI, but not in mice that did not carry the human transgene.95 This pioneer work demonstrated that anaphylaxis could be reconstituted in an “FcR-humanized” mouse. Taking advantage of the cross-binding of mouse IgE to hFcϵRI, the authors injected antigen-specific mouse IgE that bound to hFcϵRI in vivo before antigen challenge to induce anaphylaxis. The responsible cell population was, however, not identified. Until recently, no other report has investigated the role, if any, of human IgG receptors in anaphylaxis using hFcγR-transgenic or knock-in mice. We investigated the ability of hFcγRIIA to induce anaphylaxis in hFcγRIIAtg mice for 2 reasons: (1) human neutrophils can restore anaphylaxis when transferred to anaphylaxis-resistant mice38 ; and (2) human neutrophils constitutively express only one activating IgG receptor, hFcγRIIA. Cross-binding of mouse IgG1, IgG2a, and IgG2b subclasses to hFcγRIIA38 allowed testing of active systemic anaphylaxis (BSA-ASA) in hFcγRIIAtg FcRγ−/−mice but also PSA and PCA using mouse or human immune complexes. hFcγRIIA could induce fatal ASA, PSA, and PCA, which were abolished by specific anti-hFcγRIIA blocking mAbs. hFcγRIIA expressed in transgenic mice can therefore replace mouse IgG receptors FcγRIII and FcγRIV in the induction of anaphylaxis. hFcγRIIA-dependent PCA required mast cells,76 in agreement with FcγRIII-dependent PCA47 and FcϵRI-dependent PCA,96 which also required mast cells. The induction of hFcγRIIA-dependent PSA required neutrophils and monocyte/macrophages but did not require mast cells or basophils. These results support and strengthen results obtained on the contribution of neutrophils and monocytes/macrophages to systemic anaphylaxis in WT mice.38,92 The mediators responsible for the induction of hFcγRIIA-dependent anaphylaxis have not been identified yet. hFcγRIIA engagement on human monocytes and neutrophils has been reported to lead to PAF release38 among that of several anaphylactogenic mediators.93 PAF may therefore contribute to hFcγRIIA-dependent anaphylaxis.
Final considerations
The field of Fc receptors has increased in complexity after the identification of a novel IgG receptor in 2005.24 The generation of knockouts for each mouse FcR and of specific (blocking) anti-FcR mAbs, nevertheless, enabled to establish a refined picture of FcR properties and functions in vivo. Models of arthritis, thrombocytopenia, and anaphylaxis have benefited largely from these advances, and more disease models are currently being similarly analyzed. Blocking FcγRs in vivo using specific mAbs will certainly become the experimental approach of choice to address their function in vivo, as it avoids genetic background issues and phenotypic variations among knockouts. In this line of reasoning, experiments using blocking anti-FcγRIIB mAbs in vivo may enable to determine the exact contribution of this inhibitory receptor to experimental disease models. Indeed, FcγRIIB−/− mice were reported to develop myeloproliferation, hypergammaglobulinemia, and autoantibodies leading to strain-specific spontaneous autoimmune diseases.7,97 These alterations may contribute to render these mice hypersensitive to experimental models of disease without a direct involvement of FcγRIIB during their induction phase.
Like mouse IgE receptor FcϵRI and mouse IgG receptors FcγRIII and FcγRIV, human IgE receptor hFcϵRI and human IgG receptor hFcγRIIA are sufficient to trigger IgE- and IgG-induced systemic anaphylaxis, respectively, when expressed in mice.76,95 Previous studies demonstrated that hFcγRIIA is also sufficient to induce experimental thrombocytopenia68 and arthritis.73,75 All these results, however, have been obtained in mice expressing only one hFcR, in the absence of the inhibitory hFcγRIIB, and in the absence of other activating hFcγRs or hFcRn that may regulate or contribute to disease induction/progression. If other human IgG receptors play a role in these diseases in humans, other cell types than those identified so far may contribute to, or even be responsible for, their induction. Illustrating this view, FcRn was reported to be expressed more widely than expected (ie, also on monocytes/macrophages and neutrophils; Tables 1 and 3). In addition, the functions of FcRn were reported to compose also antigen uptake and processing by DCs17,32 and phagocytosis of IgG-opsonized bacteria by neutrophils.4 hFcRn might therefore contribute to more models of disease (or therapy) than initially thought and should be studied in vivo when coexpressed with hFcγRs. Another example is hFcγRIIIB, which has been reported to be expressed not only on neutrophils, but also on basophils.15 hFcγRIIIB has been recently reported to play specialized roles on neutrophils, different from those played by hFcγRIIA.2 Creating mouse models expressing multiple or, preferably, all hFcRs (with the same expression pattern as that found in humans) may be a necessity to comprehend their role in disease induction/modulation, and thereby of the cells expressing them. The recent report by Smith et al using a model of mice expressing multiple hFcγRs72 opens the way to performing these analyses. More efforts, however, will be necessary to obtain mice whose expression patterns of hFcγRs fully reproduce that found in humans, in particular on DCs and effector myeloid populations.
Finally, data published on different models of systemic anaphylaxis compile in a rather complicated picture on the various cell types, antibody receptors, and mediators involved (Figure 3). That neither mast cells nor IgE, but rather neutrophils, monocytes/macrophages, and IgG, concur to models of ASA is unexpected and opens novel areas of research in human anaphylaxis.98-100 Noticeably, neutrophils not only contribute to ASA, they are also responsible for 2 models of IgG-induced PSA38 in WT mice. Both monocytes/macrophages and neutrophils also contribute to PSA induced by human IgG receptor FcγRIIA.76 This receptor is expressed by human neutrophils that can induce anaphylaxis when transferred in resistant mice and that are the major PAF-producing cell population.93 Therefore, that PAF and, to a minor extent, histamine are responsible for ASA calls to reevaluate PAF contribution in anaphylaxis based on the findings summarized in this review. Supporting a role for PAF in anaphylactic reactions in the clinic, serum PAF concentration was shown to correlate with the severity of anaphylactic shock.101 Of note, one may consider only results obtained with models of ASA as human anaphylaxis is essentially active (ie, allergen-sensitized persons encountering that allergen). Passive cases of anaphylaxis may nevertheless occur, for example, after transfusion or organ transplantation from sensitized donors, or after therapeutic antibody treatment.
Acknowledgments
The author thanks Dr K. Garrod (Unité des Dynamiques des Réponses Immunes, Institut Pasteur, Paris, France) for editing the manuscript.
This work was supported by the Institut Pasteur, Inserm, the Agence Nationale de la Recherche (grant 09-GENO-014-01), the Société Française d'Allergologie, Arthritis-Fondation Courtin, the Association pour la Recherche sur le Cancer, and the Ligue Nationale contre le Cancer.
Authorship
Contribution: P.B. designed and wrote the review.
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Pierre Bruhns, Unité d'Allergologie Moléculaire et Cellulaire, Département d'Immunologie, Institut Pasteur, 25 rue du Docteur Roux, 75015 Paris, France; e-mail: bruhns@pasteur.fr.