Abstract
B cells require signals delivered through B-cell activating factor of the TNF family receptor (BAFF-R) and CD40 to survive and produce antibody responses in vivo. In vitro data indicate that these signals are controlled by the homologous RING finger proteins cIAP1 and cIAP2, in collaboration with TRAF2 and TRAF3. There is also mounting evidence that all 4 of these signaling molecules can act as tumor suppressors in human B-lineage malignancies. However, it has not been possible to identify the roles of cIAP1 and cIAP2 in controlling B-cell physiology because of the absence of an appropriate in vivo model. Here we describe a unique genetically modified mouse in which the linked cIap1 and cIap2 genes can be independently inactivated. Deletion of cIAP1 plus cIAP2 (but not either protein alone) rendered primary B cells independent of BAFF-R for their survival and led to their uncontrolled accumulation in vivo. B cells deficient in cIAP1 and cIAP2 were also incapable of forming germinal centers, a key step in antibody-mediated immunity. These data define a fundamental role for cIAP1/cIAP2 in regulating B-cell survival and responsiveness, show this requires direct binding to TRAF2, and suggest how mutations of TRAF2, TRAF3, and cIAP1/cIAP2 contribute to B-lineage malignancies, such as multiple myeloma.
Introduction
Appropriate regulation of B lymphocyte survival and activation is critical for ensuring humoral immunity while also avoiding autoimmunity and malignancies, such as B-lymphomas and multiple myeloma (MM). Two members of the tumor necrosis factor (TNF) ligand superfamily, B-cell activating factor of the TNF family (BAFF, TNFSF13B) and CD40 ligand (CD40L, TNFSF5), are central to these processes. Mice lacking BAFF or its B-cell surface receptor BAFF-R (TNFRSF13C) do not possess mature B cells because of the absence of essential survival and maturation signals normally delivered through this ligand-receptor pair.1,2 On the other hand, mice lacking CD40L or its B-cell surface receptor CD40 (TNFRSF5) produce mature B cells but do not mount T-dependent antibody and germinal center (GC) responses because B cells cannot receive the requisite CD40-dependent signals from CD40L+ T-helper cells.3-5
Nondeath domain TNFRs, such as BAFF-R and CD40, activate intracellular signaling pathways by directly binding members of the TNFR-associated factor (TRAF) family. All mammalian TRAFs (bar TRAF1) have amino-terminal RING domains. In the case of TRAF6 and TRAF2, these RING domains can act as lysine 63 (K63) E3 ubiquitin ligases that directly conjugate K63-linked polyubiquitin chains to specific target proteins, thereby directly or indirectly facilitating the activation of downstream signaling enzymes.6-9
A separate group of RING-containing E3 ubiquitin ligases involved in TNFR signaling are the cellular inhibitor of apoptosis (cIAP) proteins. cIAPs are indirectly recruited to TNFRs via their interactions with TRAF proteins, principally TRAF2.10-12 cIAP RING domains can catalyze conjugation of several types of polyubiquitin chains, including lysine 48 (K48) linkages, which directly target proteins for proteasomal degradation.11,13 In vitro, it appears that cIAP1 and cIAP2 act redundantly to control intracellular signaling pathways.7,14-18 It has been difficult, however, to determine whether cIAP1 and cIAP2 function redundantly in vivo because cIap1−/−.cIap2−/− mice cannot be generated by crossing single gene knockout mice because of the close physical linkage of the cIap1 and cIap2 genes.19
Recent studies have indicated that both TRAF2 and TRAF3 play critical roles in the regulation of B-cell survival by BAFF-R. Although only TRAF3 is recruited directly to BAFF-R,20 B cells deficient in either TRAF2 or TRAF3 accumulate in large numbers in vivo and show greatly extended in vitro survival.21-23 This occurs because primary B cells are uniquely dependent on intracellular signaling pathways, such as alternative NF-κB activation (NF-κB2 processing), which are constitutively suppressed by the nonredundant and cooperative actions of TRAF2 and TRAF3.22 BAFF-R is normally required to reverse this suppression and activate these pathways by triggering the proteolytic degradation of TRAF3,24 a process that also requires TRAF2.22 Proteolysis of TRAF3 prevents constitutive TRAF2/TRAF3-dependent degradation of the serine-threonine kinase NIK, resulting in the accumulation of NIK, processing of p100 NF-κB2 to the active p52 form, and nuclear translocation of p52.7,16,24
NIK degradation occurs in proteasomes.24 Although TRAF2 and TRAF3 both bind to NIK and are required for its degradation, they lack endogenous K48-ubiquitin ligase activity, indicating that a separate ubiquitin ligase must also be involved. In vitro studies have indicated that cIAP1 can mediate NIK ubiquitylation and degradation and that this depends on the TRAF2-binding site of cIAP1.14,15 Further work has indicated that TRAF2 binds cIAP1/cIAP2 and directs its K48-ubiquitin ligase activity against TRAF3-complexed NIK,7,16 but it is not clear whether cIAP1/cIAP2 is also involved in triggering BAFF-R–mediated TRAF3 degradation. Although global deficiency of either cIAP1 or cIAP2 has no obvious effect on B cells,25,26 it is yet to be determined whether these homologs perform redundant functions in controlling the survival of primary B cells.
TRAF2, TRAF3, and cIAP1/cIAP2 also play major roles in CD40 signaling. Unlike BAFF-R, activated CD40 recruits both TRAF2 and TRAF3 to its cytoplasmic domain. cIAP1/cIAP2 that is recruited to CD40 via TRAF2 becomes K63-ubiquitylated and CD40-bound TRAF3 subsequently K48 ubiquitylated by cIAP1/cIAP2 and thus targeted for proteasomal degradation.7 TRAF3 degradation releases TRAF2 and cIAP1/cIAP2 into the cytoplasm, as well as the other components of the signaling complex assembled on CD40, resulting in the activation of a variety of downstream MAP kinases, including c-Jun N-terminal kinase (JNK) and p38.27 It is unknown, however, whether the apparent importance of TRAF2 or cIAP1/cIAP2 in CD40 signaling is reflected in a requirement for these molecules in in vivo T-dependent B-cell responses.
Recent studies have indicated that TRAF2, TRAF3, and cIAP1/cIAP2 may act as tumor suppressors in the B-lineage.28-30 In particular, somatically acquired loss of function mutations in the TRAF2, TRAF3, and cIAP1/cIAP2 genes are prevalent in human MM, a currently incurable cancer of terminally differentiated plasma cells.31-33 The likelihood that TRAF2 and TRAF3 are tumor suppressors in the B-lineage is consistent with the greatly extended survival of TRAF2- and TRAF3-deficient B cells21-23 and raises the question of whether inactivation of cIAP1/cIAP2 expression in B cells may have the same effect.
To clarify the roles of cIAP1 and cIAP2 in primary B-cell survival and responsiveness, we have generated a unique mouse line that facilitates independent or simultaneous inactivation of the linked cIap1 and cIap2 genes in B cells. Comparison of these mice with those possessing B cell-specific inactivation of TRAF2 or TRAF3 expression revealed that cIAP1 and cIAP2 function redundantly in controlling both B-cell survival and responsiveness and suggest an explanation for the prevalence of loss of function mutations in TRAF3 as opposed to TRAF2 or cIAP1/cIAP2 in human MM.
Methods
Mice
Conditional Traf2 knockout (Traf2flox),21 conditional Traf3 knockout (Traf3flox),22 and Tnfr13c−/−2 mice have all been previously described. B6.SJL-Ptprca (C57BL/6 CD45.1-congenic) mice were purchased from Animal Resources Center. The production of the various cIAP-deficient mouse lines is described in “Generation of cIap1ΔB, cIap2−/−, and cIap1ΔB.cIap2−/− mice.” Mice were screened by polymerase chain reaction analysis of blood or tail-tip DNA. All mice were maintained on an inbred C57BL/6 genetic background at the animal facilities of the Garvan Institute and La Trobe University and analyzed between 2 and 4 months of age. All mouse experiments were approved by the Garvan/St Vincent's Animal Ethics Committee.
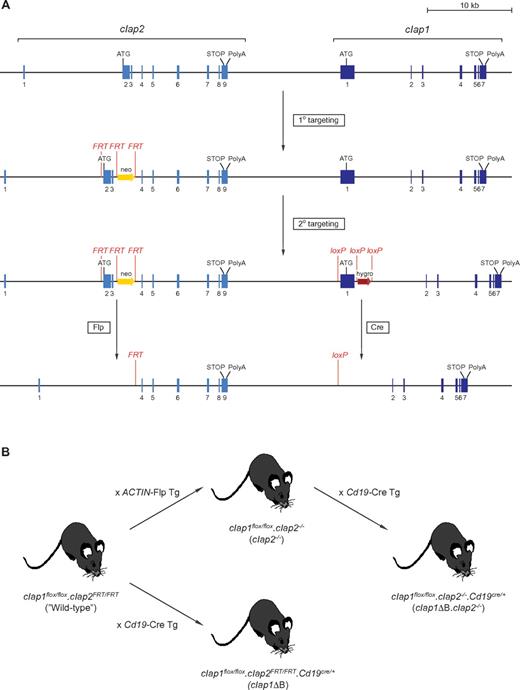
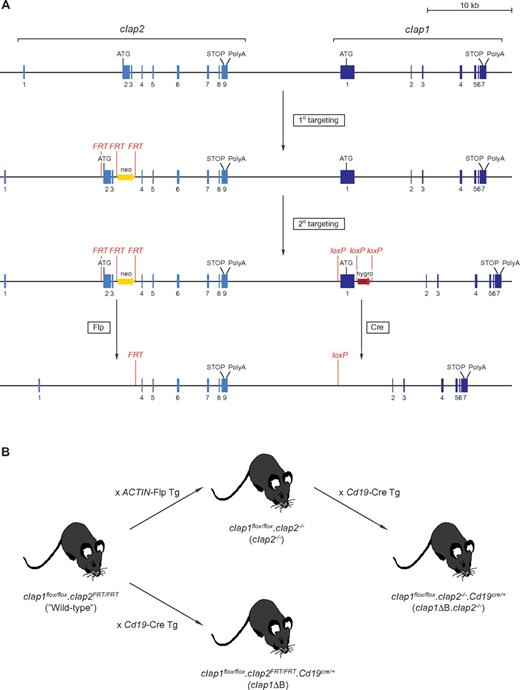
Generation of cIap1ΔB, cIap2−/−, and cIap1ΔB.cIap2−/− mice
A cIap2 targeting vector designed to flank exons 2 and 3 and an intronic neomycin resistance cassette with FRT sites was electroporated into the C57BL/6 embryonal stem (ES) cell line Bruce4. Transfected clones were selected in neomycin (200 μg/mL) and homologous recombinants identified by Southern hybridization. Targeted clones were injected into BALB/c blastocysts to assess their capability to yield high-percentage chimeras. One clone was chosen for secondary electroporation with a cIap1 targeting vector designed to flank exon 1 and a hygromycin resistance marker with loxP sites. Double-targeted clones were selected in hygromycin (150 μg/mL) and confirmed by Southern blotting. Chimeras obtained from BALB/c blastocyst injections of 3 clones were backcrossed to C57BL/6. F1 progeny sired by one chimera tested positive by Southern analysis for both targeted mutations, confirming that homologous recombination had occurred on the same chromatid (Figure 1A). To globally inactivate cIap2, mice carrying the doubly targeted cIap locus were crossed with ACTIN-Flp transgenic mice and the Flp-mediated germline deletion of cIap2 bred to homozygosity (cIap1flox/flox.cIap2−/− = cIap2−/−). For B cell-specific inactivation of cIap1 alone, mice carrying the dual-targeted cIap locus were crossed with Cd19-Cre mice and bred to homozygosity at the targeted cIap locus and heterozygosity at the targeted Cd19 locus (cIap1flox/flox.cIap2FRT/FRT.Cd19cre/+ = cIap1ΔB; Figure 1B). These 2 breeding steps were performed in sequence to obtain mice with global inactivation of cIap2 and B-cell specific inactivation of cIap1 (cIap1flox/flox.cIap2−/−.Cd19cre/+ = cIap1ΔB.cIap2−/−) (Figure 1B). Primers used for polymerase chain reaction screening: cIap1 gene: AGA CCC TTT CTA AGT AGA CTG GTT and TTA TAG AAA TGT TCA GAT GTC (231bp = untargeted, 311 bp = targeted); cIap2 gene: CCC TCA GGG TGT GTG GCT TA and TGT GCA TGG CTT CTG GTC GG (275bp = wild-type, 351 bp = targeted, no fragment = Flp-deleted).
Flow cytometry
Flow cytometric staining and analysis were performed as described.22 The following antibodies and conjugates were purchased from BD Biosciences: anti-CD16/CD32 (2.4G2), anti–B220-fluorescein isothiocyanate (FITC), -phycoerythrin (PE), -peridinin chlorophyll protein, -allophycocyanin (APC), -PB (RA3-6B2), anti-CD21/CD35–FITC (7G6), anti-CD23–PE (B3B4), anti–Fas-biotin (Jo2), anti–T- and B-cell activation antigen-FITC (GL7), anti–IgG1-PE (A85-1), anti–CD4-FITC (L3T4), anti–CD8-PE (53-6.7), anti–CD1d-biotin (1B1), anti–CD35-biotin (8C12) and streptavidin-APC, -PE, -peridinin chlorophyll protein Cy5.5 (Streptavidin). The following antibodies and conjugates were purchased from eBioscience: anti–CD38-FITC, -PE (90), anti–C1qRp-APC (AA4.1), anti–CD45.1-PECy7 (A20), and anti–CD45.2-peridinin chlorophyll protein-Cy5.5. (104) Anti–human CD4-APC (S3.5) was purchased from Invitrogen. Light scatter gating was performed on all samples to include lymphocytes but exclude doublets, dead cells, and debris. In vitro survival assays were performed as previously described.22 For survival assays using retrovirally transduced B cells, unpurified lymph node cells were cultured and results expressed relative to B cells transduced with empty vector.
B-cell isolation and culture
B cells were purified from lymph nodes using Mouse B Cell Isolation Kit (Miltenyi Biotec) as per the manufacturer's instructions. Cells were stimulated with culture supernatant from HEK 293 cells expressing murine CD40L. To obtain CD40L supernatants, HEK 293 cells were transfected using FuGENE6 transfection reagent (Roche Diagnostics) with a pcDNA4 expression plasmid (Invitrogen) containing the CD40L extracellular domain (amino acids 47-260), a secretory signal sequence, and an amino terminal FLAG tag (DYKDDDDK). Anti-FLAG antibody (2 mg/mL, clone M2, Sigma-Aldrich) was added to all CD40L stimulations to create multimeric CD40L complexes.
Immunoblotting
Nuclear, cytoplasmic, and whole cell lysates were prepared as described.22 All lysates were subjected to polyacrylamide gel electrophoresis on 4% to 12% gradient NuPAGE Bis-Tris gels (Invitrogen) in XCell SureLock Mini-Cell apparatus (Invitrogen) and transferred onto Immobilon-P PVDF membranes (Millipore) using XCell II Blot module (Invitrogen). Membranes were blocked and antibodies diluted in 5% bovine serum albumin/0.2% Tween20/Tris-buffered saline. Antibodies from Santa Cruz Biotechnology were: anti-TRAF3 (H122), anti-TRAF2 (C20), anti–rabbit IgG–horseradish peroxidase (sc-2030), and anti–mouse IgG–horseradish peroxidase (sc2031). Antibodies from Cell Signaling Technologies were: anti–NF-κB2 p100/p52 (4882), anti–phospho-JNK (9251), anti–phospho-p38 (9211), anti–phospho-p42/44 MAP kinases (extracellular signal-regulated kinase 1/2 [ERK1/2]) (9101), and anti-IκBα (9242). Anti–β-actin (AC15) monoclonal antibody was from Sigma-Aldrich.
Histology
Spleen were frozen in Tissue Tek OCT compound (Sakura); 6- to 7-μm sections were cut using a CM1900 cryostat (Leica), fixed in acetone, and blocked with 30% normal horse serum (Invitrogen). Slides were stained with the following antibodies: anti–CD3e-biotin (eBio500A2, eBioscience), anti–IgD-AlexaFluor-647 (11-26c.2a, BioLegend), and anti–GL7-FITC (GL7, BD Biosciences). Biotinylated antibodies were detected with streptavidin–AlexaFluor-555 (Invitrogen). Slides were analyzed with a Zeiss Axiovert 200M microscope using a 10× objective and Adobe Photoshop software Version 10.0.1.
Immunizations
Mice were immunized with 5 × 108 sheep red blood cells (SRBCs; Institute of Medical and Veterinary Sciences) by intravenous tail vein injection, culled 7 days later, and spleens collected for flow cytometry and histology. GC responses from retrovirally transduced B cells were expressed as a proportion of total transduced B cells in each chimera and then relative to the proportion of wild-type (CD45.1+) B cells with a GC phenotype.
Bone marrow chimeras
To produce bone marrow chimeras, CD45.1 congenic (B6.SJL-Ptprca) mice were first irradiated with a split dose of 850 cGy (2 × 425 cGy, 4 hours apart) using an X-RAD 320 Biologic Irradiator (Precision X-Ray). The following day, recipients received 107 bone marrow cells by intravenous tail injection and were allowed to reconstitute for 8 weeks before analysis. For chimeras reconstituted with retrovirally transduced bone marrow cells (see “Retroviral constructs and transductions”), recipients each received 5 × 105 transduced bone marrow cells and 106 unmanipulated B6.SJL-Ptprca bone marrow cells.
Retroviral constructs and transductions
cDNAs encoding wild-type, Δ1-80, and Δ283-293 versions of murine TRAF2 have been previously described.34,35 cDNAs encoding Δ1-28, Δ355-501, and Δ358-501 were produced by polymerase chain reaction-mediated mutagenesis as previously described36 and verified by DNA sequencing. All mutant versions of murine TRAF2 efficiently expressed proteins of the predicted length (data not shown). TRAF2Δ283-293 has been previously verified to bind both RIPK1 and TRADD normally but to lack cIAP1/cIAP2-binding activity.35 cDNAs were cloned between the NotI and XhoI sites of the pMGfI4 retroviral vector and bone marrow chimeras containing transduced Traf2ΔB hematopoietic stem cells constructed as previously described.37
Results
Conditional inactivation of cIAP1/cIAP2 expression in B cells
To facilitate single or simultaneous deletion of genes for cIAP1 and cIAP2 in vivo, loxP and FRT sites were introduced into adjacent cIap1 and cIap2 genes by sequential gene targeting in C57BL/6 ES cells (Figure 1A). Mice homozygous for the targeted chromosome 9 (cIap1flox/flox.cIap2FRT/FRT) exhibited normal cIAP1 and cIAP2 expression (data not shown) and for simplicity are referred to here as “wild-type.” Global inactivation of cIap2 was achieved by Flp-mediated deletion of exons 2 and 3 of cIap2 in the germline (cIap1flox/flox.cIap2−/− = cIap2−/−), whereas breeding with mice carrying a Cre-targeted Cd19 locus yielded animals with B cellspecific inactivation of cIAP1 expression (cIap1flox/flox.cIap2FRT/FRT .Cd19cre/+ = cIap1ΔB; Figure 1B). These 2 breeding steps were performed in sequence to produce mice in which cIAP2 expression was absent throughout, and B cells specifically lacked expression of both cIAP1 and cIAP2 (cIap1flox/flox.cIap2−/−.Cd19cre/+ = cIap1ΔB.cIap2−/−; Figure 1B). These mice provided the first opportunity to examine the redundant functions of cIAP1 and cIAP2 in vivo.
Production of cIap1ΔB, cIap2−/− and cIap1ΔB.cIap2−/− mice. (A) The wild-type cIap locus was sequentially targeted in ES cells by first introducing FRT sites into cIap2, followed by loxP sites into cIap1. Mice carrying the doubly targeted cIap locus were generated from a single ES cell clone. This approach facilitated independent inactivation of cIap2 and/or cIap1 by Flp- and Cre-mediated recombination, respectively. (B) Breeding strategy used to generate mice containing B cells lacking expression of cIAP1 and/or cIAP2.
Production of cIap1ΔB, cIap2−/− and cIap1ΔB.cIap2−/− mice. (A) The wild-type cIap locus was sequentially targeted in ES cells by first introducing FRT sites into cIap2, followed by loxP sites into cIap1. Mice carrying the doubly targeted cIap locus were generated from a single ES cell clone. This approach facilitated independent inactivation of cIap2 and/or cIap1 by Flp- and Cre-mediated recombination, respectively. (B) Breeding strategy used to generate mice containing B cells lacking expression of cIAP1 and/or cIAP2.
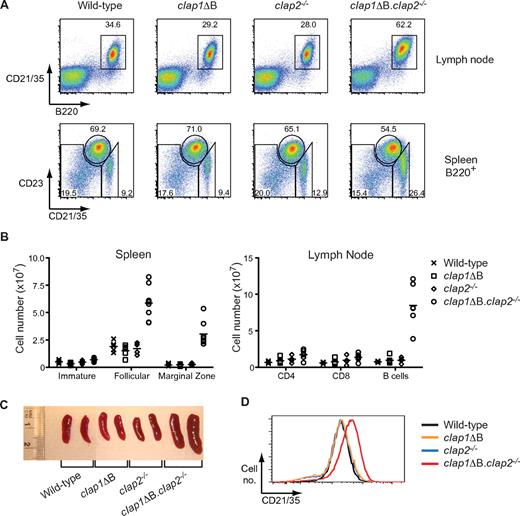
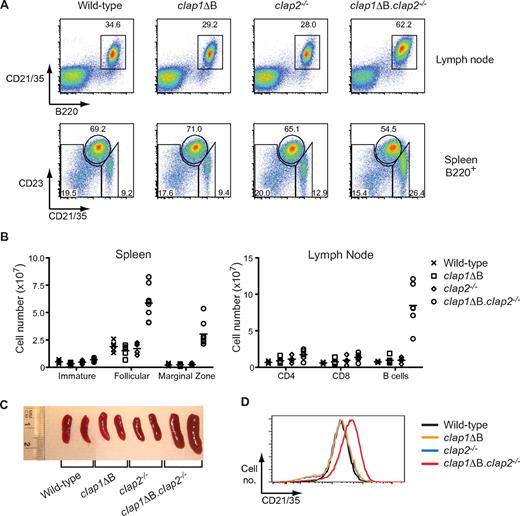
cIAP1/cIAP2-deficient B cells accumulate in vivo
Consistent with previous analyses,25,26 comparison of wild-type, cIap1ΔB, and cIap2−/− mice revealed no differences in spleen or lymph node size or in the numbers or phenotype of the B cells within these peripheral lymphoid tissues (Figure 2). However, inactivation of both cIAP1 and cIAP2 expression in B cells (cIap1ΔB.cIap2−/− mice) resulted in a phenotype indistinguishable from that previously reported in mice with B cell-specific inactivation of Traf2 or Traf3.22 Thus, cIap1ΔB.cIap2−/− mice had increased numbers of B cells within lymph nodes as well as in the follicular (CD21/CD35mid,CD23hi) and marginal zone (MZ) compartments (CD21/CD35hi,CD23lo) of the spleen (Figure 2A-B) sufficient to cause lymphadenopathy and splenomegaly (Figure 2C). In addition, lymph node B cells lacking cIAP1 and cIAP2 displayed elevated expression of CD21/CD35 (Figure 2D) similar to that seen in Traf2ΔB and Traf3ΔB mice.21,22 cIAP1 and cIAP2 therefore act redundantly to limit both mature B-cell numbers and CD21/CD35 expression in vivo.
cIAP1 and cIAP2 perform redundant functions to negatively regulate B-cell accumulation in vivo. (A) Flow cytometric analysis of lymph node cells (top) and splenic B cells (bottom) from the indicated mouse lines. Spleen samples are also gated on total B cells (B220+ gate). The window on lymph node data indicates mature B cells (B220+ gate). Windows on spleen data indicate, from left to right: immature (CD21/CD35lo, CD23lo), follicular (CD21/CD35mid, CD23hi), and marginal zone (CD21/CD35hi, CD23lo) B-cell populations. All numbers indicate the proportion of displayed events falling within the associated windows. (B) Enumeration of lymphocytes from the spleen and lymph nodes (pooled cervical, inguinal, axillary, brachial, and mesenteric nodes) of various mouse lines exhibiting the indicated lymphocyte phenotypes as determined by flow cytometry. Points represent data from individual mice; and lines, the arithmetic means. (C) Photograph showing spleen sizes from mice of the indicated genotypes. (D) CD21/CD35 expression levels on B cells from the lymph nodes of mice of the indicated genotypes. Flow cytometry data were gated on live lymphocytes by light scatter, then on B220+ B cells. All data were representative of at least 3 mice of each genotype.
cIAP1 and cIAP2 perform redundant functions to negatively regulate B-cell accumulation in vivo. (A) Flow cytometric analysis of lymph node cells (top) and splenic B cells (bottom) from the indicated mouse lines. Spleen samples are also gated on total B cells (B220+ gate). The window on lymph node data indicates mature B cells (B220+ gate). Windows on spleen data indicate, from left to right: immature (CD21/CD35lo, CD23lo), follicular (CD21/CD35mid, CD23hi), and marginal zone (CD21/CD35hi, CD23lo) B-cell populations. All numbers indicate the proportion of displayed events falling within the associated windows. (B) Enumeration of lymphocytes from the spleen and lymph nodes (pooled cervical, inguinal, axillary, brachial, and mesenteric nodes) of various mouse lines exhibiting the indicated lymphocyte phenotypes as determined by flow cytometry. Points represent data from individual mice; and lines, the arithmetic means. (C) Photograph showing spleen sizes from mice of the indicated genotypes. (D) CD21/CD35 expression levels on B cells from the lymph nodes of mice of the indicated genotypes. Flow cytometry data were gated on live lymphocytes by light scatter, then on B220+ B cells. All data were representative of at least 3 mice of each genotype.
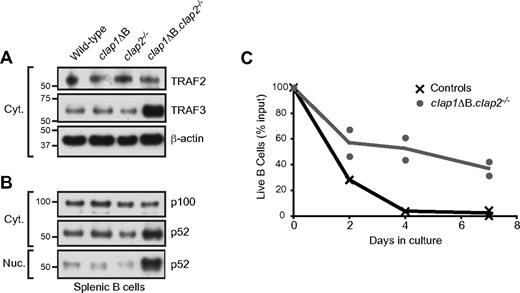
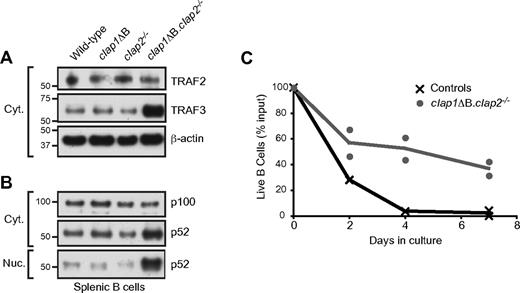
cIAP1/cIAP2 and TRAF2 mediate the in vivo degradation of TRAF3 in response to endogenous BAFF/BAFF-R signaling
B cells undergo sustained BAFF-R–mediated proteolytic degradation of TRAF3 in vivo because of signals delivered by constitutively expressed BAFF. This is reflected by the greatly increased levels of TRAF3 protein (but not Traf3 mRNA) in B cells from BAFF- and BAFF-R–deficient compared with wild-type mice.22 TRAF2-deficient primary B cells also have increased levels of TRAF3,21,22 indicating that TRAF2 is required for BAFF-R–mediated degradation of TRAF3 in vivo. A similar result was obtained in B cells that lacked both cIAP1 and cIAP2 but not either of these proteins alone (Figure 3A). cIAP1 and cIAP2 therefore function redundantly in mediating BAFF-R–dependent degradation of TRAF3 in primary B cells.
Increased TRAF3 expression, hyperactivity of the alternative NF-κB pathway, and extended in vitro survival of B cells in the absence of cIAP1 plus cIAP2. (A-B) Cytoplasmic and nuclear extracts from purified lymph node B cells were subjected to Western blot analysis with antisera directed against the indicated proteins. β-Actin was used as a loading control. (C) Purified lymph node B cells from the indicated mouse lines were incubated in unsupplemented culture medium, and the number of live cells present at the indicated time points were assayed by flow cytometry. Control data are from wild-type, cIap1ΔB, and cIap2−/− mice. Points represent data from individual mice; and lines connect the mean value obtained at each time point. Data are representative of 3 individual experiments.
Increased TRAF3 expression, hyperactivity of the alternative NF-κB pathway, and extended in vitro survival of B cells in the absence of cIAP1 plus cIAP2. (A-B) Cytoplasmic and nuclear extracts from purified lymph node B cells were subjected to Western blot analysis with antisera directed against the indicated proteins. β-Actin was used as a loading control. (C) Purified lymph node B cells from the indicated mouse lines were incubated in unsupplemented culture medium, and the number of live cells present at the indicated time points were assayed by flow cytometry. Control data are from wild-type, cIap1ΔB, and cIap2−/− mice. Points represent data from individual mice; and lines connect the mean value obtained at each time point. Data are representative of 3 individual experiments.
cIAP1/cIAP2-deficient B cells display hyperactive NF-κB2 activity and increased survival
B cells lacking either cIAP1 or cIAP2 alone displayed normal activation of the alternative NF-κB pathway, with the cytoplasmic and nuclear levels of p52 being indistinguishable from those in wild-type B cells (Figure 3B). In contrast, B cells deficient in both cIAP1 and cIAP2 displayed increased amounts of p52 in the cytoplasm and nucleus (Figure 3B). Similar to TRAF2-deficient B cells,21,22 this augmented activation of the alternative NF-κB pathway in cIAP1/cIAP2-deficient B cells occurred despite the high levels of cellular TRAF3 (Figure 3B). This highlights the cooperative and essential roles played by TRAF2 and cIAP1/cIAP2 in activation of both the alternative NF-κB pathway and the BAFF-R–mediated degradation of TRAF3.
We have previously shown that B cells from Traf2ΔB and Traf3ΔB mice survive for extended periods in medium free of any added mitogenic or survival factors.21,22 This property was shared by B cells from cIap1ΔB.cIap2−/− mice (Figure 3C), further extending the phenotypic similarities between TRAF2-, TRAF3-, and cIAP1/cIAP2-deficient B cells. In contrast, B cells from wild-type, cIap1ΔB, and cIap2−/− mice died rapidly under these conditions (controls, Figure 3C). Taken together, these data show that cIAP1 and cIAP2 act redundantly in naive primary B cells to suppress both the alternative NF-κB pathway and cellular survival.
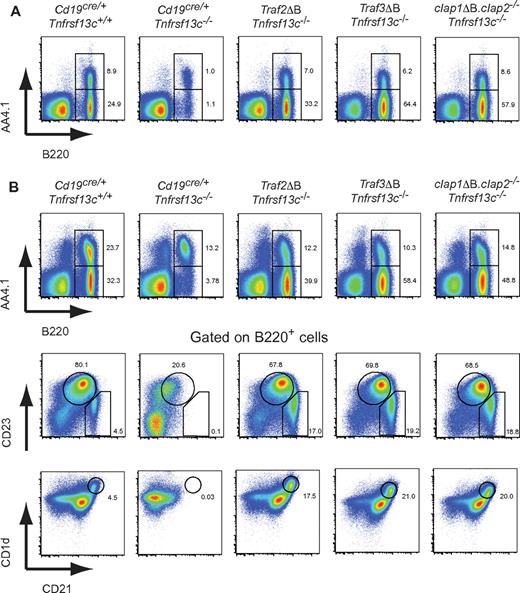
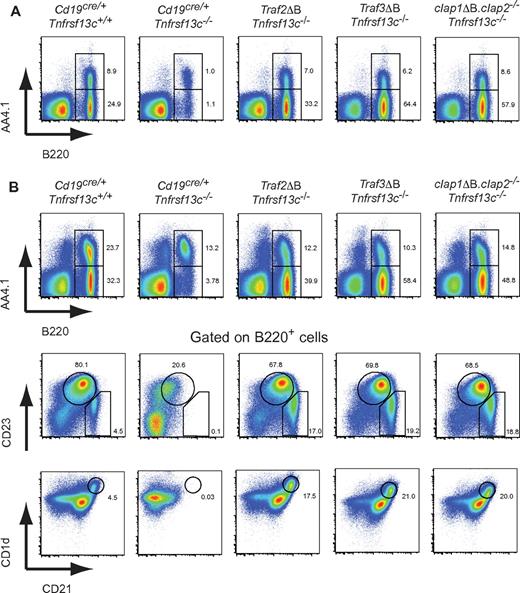
B cells deficient in TRAF2, TRAF3, or cIAP1/cIAP2 no longer require BAFF-R to mature and survive in vivo
Traf2ΔB, Traf3ΔB, and cIap1ΔB.cIap2−/− mice were bred onto a BAFF-R–deficient (Tnfrsf13c−/−) background. Comparison of spleen and lymph node cells from wild-type and Tnfrsf13c−/− mice (both also carrying the Cd19cre/+ gene) illustrated the fundamental requirement for BAFF-R in the development of mature B-cell populations (B220+, AA4.1−) in both tissues (Figure 4). Strikingly, the development of mature B cells, including the follicular and MZ subpopulations of the spleen, were unimpaired in BAFF-R–deficient mice that also lacked B-cell expression of either TRAF2, TRAF3, or cIAP1/cIAP2 (Figure 4). Thus, the survival and maturation pathways normally activated by physiologic triggering of BAFF-R by BAFF are constitutively activated when the expression of TRAF2, TRAF3, or cIAP1/cIAP2 is absent from B cells.
B cells lacking TRAF2, TRAF3 or cIAP1 plus cIAP2 no longer require BAFF-R for their in vivo development and survival. Traf2ΔB, Traf3ΔB, and cIap1ΔB.cIap2−/− mice were crossed onto a BAFF-R–deficient (Tnfrsf13c−/−) background. Flow cytometric analysis of (A) lymph node or (B) spleen from the indicated mice lines. Windows indicate immature (B220+, AA4.1+) and mature (B220+, AA4.1−) phenotype B cells. Data in CD21 versus CD23 and CD21 versus CD1 days profiles are from total B cells (B220+ gate), and windows show immature (CD21/CD35lo, CD23lo), follicular (CD21/CD35mid, CD23hi), and marginal zone (CD21/CD35hi, CD23lo and CD21/CD35hi, CD1 dayshi) B-cell populations. All numbers indicate the proportion of displayed events falling within the associated windows.
B cells lacking TRAF2, TRAF3 or cIAP1 plus cIAP2 no longer require BAFF-R for their in vivo development and survival. Traf2ΔB, Traf3ΔB, and cIap1ΔB.cIap2−/− mice were crossed onto a BAFF-R–deficient (Tnfrsf13c−/−) background. Flow cytometric analysis of (A) lymph node or (B) spleen from the indicated mice lines. Windows indicate immature (B220+, AA4.1+) and mature (B220+, AA4.1−) phenotype B cells. Data in CD21 versus CD23 and CD21 versus CD1 days profiles are from total B cells (B220+ gate), and windows show immature (CD21/CD35lo, CD23lo), follicular (CD21/CD35mid, CD23hi), and marginal zone (CD21/CD35hi, CD23lo and CD21/CD35hi, CD1 dayshi) B-cell populations. All numbers indicate the proportion of displayed events falling within the associated windows.
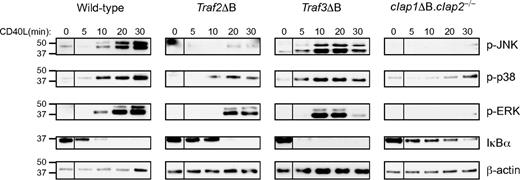
CD40 signaling in primary B cells is compromised in the absence of either cIAP1/cIAP2 or TRAF2
The mice assembled for this work provided the first opportunity to compare CD40L-mediated signal transduction in primary B cells deficient in TRAF2, TRAF3, or cIAP1/cIAP2. Phosphorylation of JNK, ERK, and p38 was accelerated in TRAF3-deficient compared with wild-type B cells (Figure 5). In addition, activation of the classic NF-κB pathway (I-κBα degradation) was also more rapid in TRAF3-deficient B cells (Figure 5). In contrast to previous studies,21,27 our analysis of TRAF2-deficient B cells revealed clear, albeit slower and less extensive, activation of the ERK, p38, and classic NF-κB pathways. JNK activation, however, was reproducibly absent (Figure 5). cIAP1/cIAP2-deficient B cells displayed the most impaired signaling, with minimal apparent activation of any of the pathways examined (Figure 5). Thus, despite the virtually identical phenotypes of TRAF2-, TRAF3-, and cIAP1/cIAP2-deficient B cells in terms of their development and survival, each exhibited a different pattern of activation of intracellular signaling pathways in response to CD40L.
CD40-mediated activation of intracellular pathways in B cells requires the presence of TRAF2 and cIAP1/cIAP2. B cells were purified from the spleens of mice of the indicated genotypes and stimulated for the indicated times with CD40L. Whole cell lysates were prepared and subjected to Western blot analysis with antisera directed against the indicated proteins. β-Actin was used as a loading control. Note that, in each case, intervening lanes (which were part of a separate study) between the “0 minutes” and “5 minutes” time points were removed using Adobe Photoshop software Version 10.0.1. All samples in each blot are from the same cells stimulated at the same time and run on the same gel. Duplicate experiments in each case generated similar results.
CD40-mediated activation of intracellular pathways in B cells requires the presence of TRAF2 and cIAP1/cIAP2. B cells were purified from the spleens of mice of the indicated genotypes and stimulated for the indicated times with CD40L. Whole cell lysates were prepared and subjected to Western blot analysis with antisera directed against the indicated proteins. β-Actin was used as a loading control. Note that, in each case, intervening lanes (which were part of a separate study) between the “0 minutes” and “5 minutes” time points were removed using Adobe Photoshop software Version 10.0.1. All samples in each blot are from the same cells stimulated at the same time and run on the same gel. Duplicate experiments in each case generated similar results.
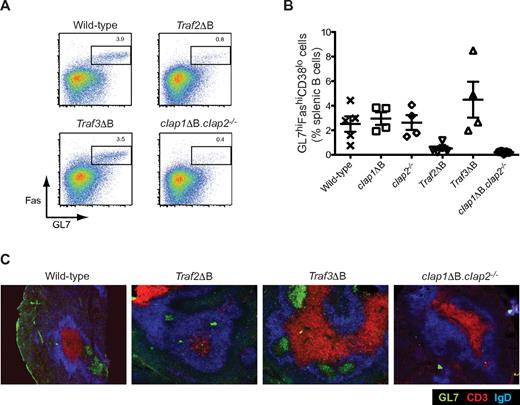
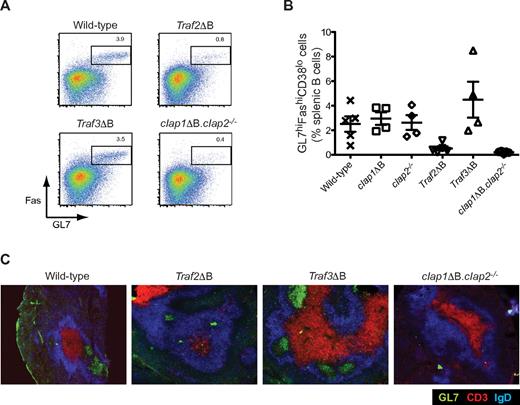
B-cell expression of TRAF2 and cIAP1/cIAP2 but not TRAF3 is required for GC formation
In vivo, CD40L is expressed on T-helper cells and binds to B-cell CD40 to deliver signals that are essential for effective T-dependent antibody and GC responses.5 As shown in Figure 5, loss of TRAF2, TRAF3, or cIAP1/cIAP2 in B cells had very different impacts on CD40 signaling. To determine their respective contributions to T-dependent GC responses, we examined TRAF2-, TRAF3-, and cIAP1/cIAP2-deficient B cells after intravenous immunization of the various genetically modified mice with SRBCs. Visualization of GC B cells (B220+, Fas+, GL7+) by flow cytometric analysis of spleen cells 7 days after SRBC immunization (Figure 6A) revealed that mice containing B cells lacking expression of either cIAP1 or cIAP2 alone made normal GC responses (Figure 6B). Consistent with the inability of cIAP1/cIAP2-deficient B cells to respond to CD40L in vitro (Figure 5B), approximately 10-fold lower numbers of GC phenotype B cells were produced in cIap1ΔB.cIap2−/− mice (Figure 6A-B). Production of GC phenotype B cells was also, albeit not so dramatically (∼ 5-fold), reduced in Traf2ΔB mice. In contrast, Traf3ΔB mice produced normal or even slightly increased numbers of GC B cells (Figure 6A,B). Immunohistologic analysis of spleen sections from immunized mice yielded results consistent with the measurement of the GC responses by flow cytometry. Thus, GL7+, IgD− GCs within B-cell follicles were readily apparent in SRBC-immunized wild-type and Traf3ΔB mice but were of greatly reduced size or absent in Traf2ΔB and cIap1ΔB.cIap2−/− mice, respectively (Figure 6C).
Mice lacking either TRAF2 alone or both cIAP1 and cIAP2 in their B cells are unable to form GCs. (A-C) Mice of the indicated genotypes were immunized with SRBCs and killed on day 7. (A) Flow cytometric analysis of splenic B cells from the indicated mouse lines. Data are from total B cells (B220+ gate). Window indicates CG B cells (GL7hi, Fashi). Numbers indicate the proportion of displayed events falling within the associated window. (B) Enumeration of the proportion of splenic B cells that were GC B cells as determined by flow cytometry. Points represent data from individual mice; and lines, the arithmetic means. Error bars represent SD. (C) GC formation in the spleens of immunized mice as detected by immunohistochemistry on spleen sections from mice of the indicated genotypes. Sections were stained for CD3+ T cells (red), IgD+ B cells (blue), and GCs (GL7+, green).
Mice lacking either TRAF2 alone or both cIAP1 and cIAP2 in their B cells are unable to form GCs. (A-C) Mice of the indicated genotypes were immunized with SRBCs and killed on day 7. (A) Flow cytometric analysis of splenic B cells from the indicated mouse lines. Data are from total B cells (B220+ gate). Window indicates CG B cells (GL7hi, Fashi). Numbers indicate the proportion of displayed events falling within the associated window. (B) Enumeration of the proportion of splenic B cells that were GC B cells as determined by flow cytometry. Points represent data from individual mice; and lines, the arithmetic means. Error bars represent SD. (C) GC formation in the spleens of immunized mice as detected by immunohistochemistry on spleen sections from mice of the indicated genotypes. Sections were stained for CD3+ T cells (red), IgD+ B cells (blue), and GCs (GL7+, green).
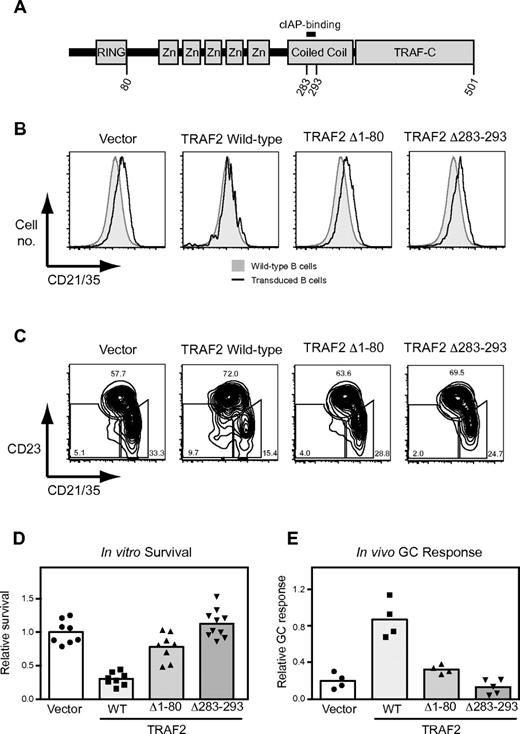
TRAF2 regulates B-cell survival and GC B-cell differentiation through direct interactions with cIAP1/cIAP2
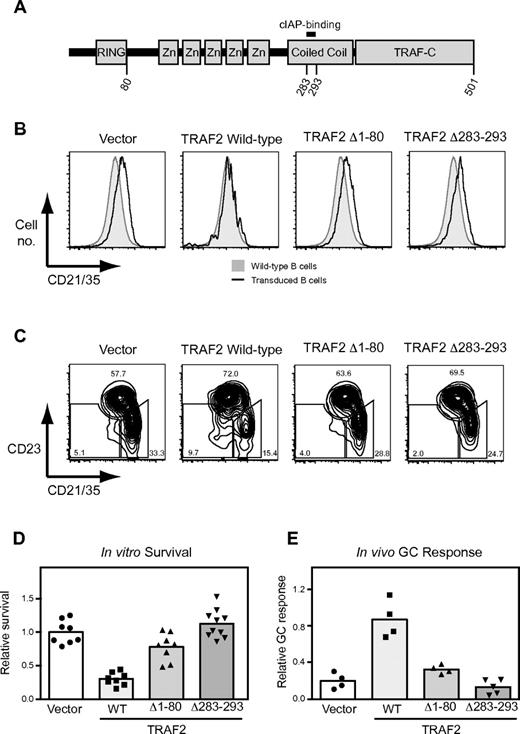
Because TRAF2 and cIAP1/cIAP2 interact directly with one another10 and this interaction is required for TRAF2 or cIAP1/cIAP2 function in certain contexts,15,35 we hypothesized that the phenotypic identity of B cells lacking expression of TRAF2 or cIAP1/cIAP2 may be the result of these proteins functioning as a complex to regulate the in vivo survival and responsiveness of primary B cells. To test this, we designed a system whereby Traf2ΔB B cells could develop from hematopoietic stem cell precursors in vivo carrying retroviral vectors encoding various forms of TRAF2, including versions lacking either the RING finger domain (TRAF2Δ1-80) or the cIAP1/cIAP2-binding site (TRAF2Δ283-293)12,35 (Figure 7A). This was achieved by using pMGfI4, a retroviral vector recently developed in our laboratory to obtain Cre-dependent expression of cDNA inserts.37 In this way, expression of Cd19-cre during early B-cell development simultaneously inactivated the endogenous Traf2lox alleles and activated expression of pMGfI4-encoded wild-type or mutant TRAF2 protein (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Suppression of B-cell survival and maturation pathways requires the cIAP binding site and RING domain of TRAF2. (A) Structure of TRAF2 protein indicating relevant domains. Flow cytometric analysis of (B) lymph node or (C) spleen cells from mice reconstituted with Traf2ΔB bone marrow transduced with retroviral constructs designed to express the indicated TRAF2 mutants. Mice were also reconstituted with wild-type CD45.1 congenic bone marrow. Plots show data from transduced B cells (CD45.1−, B220+, GFP−, hCD4+). (B) Histograms are overlaid on wild-type B cells (CD45.1+, B220+) from the same chimera. (C) Windows indicate, from left to right: immature (CD21/CD35lo, CD23lo), follicular (CD21/CD35mid, CD23hi), and marginal zone (CD21/CD35hi, CD23lo) B-cell populations. All numbers indicate the proportion of displayed events falling within the associated windows. (B-C) Data are representative of results from at least 3 chimeras (supplemental Figure 2). (D) Survival of transduced Traf2ΔB B cells in vitro. Lymph node cells from chimeras were incubated for 4 days in unsupplemented media. The proportion of input transduced B cells (CD45.1−, B220+, GFP−, hCD4+) that survived was calculated and expressed as a fraction of the mean value obtained for vector-transduced B cells. Points indicate duplicate data from individual chimeras mice. Bars represent means. (E) GC differentiation of transduced Traf2ΔB B cells in vivo. Spleens from chimeras were harvested 7 days after SRBC challenge. The proportion of transduced B cells (CD45.1−, B220+, GFP−, hCD4+) displaying a GC B-cell phenotype (CD38lo, Fashi) were expressed as a fraction of proportion of wild-type B cells (CD45.1+, B220+) in the same spleen that possessed the GC B-cell phenotype. (D-E) Data represent pooled results from 2 independent experiments. Points represent data from individual chimeras. Bars represent means.
Suppression of B-cell survival and maturation pathways requires the cIAP binding site and RING domain of TRAF2. (A) Structure of TRAF2 protein indicating relevant domains. Flow cytometric analysis of (B) lymph node or (C) spleen cells from mice reconstituted with Traf2ΔB bone marrow transduced with retroviral constructs designed to express the indicated TRAF2 mutants. Mice were also reconstituted with wild-type CD45.1 congenic bone marrow. Plots show data from transduced B cells (CD45.1−, B220+, GFP−, hCD4+). (B) Histograms are overlaid on wild-type B cells (CD45.1+, B220+) from the same chimera. (C) Windows indicate, from left to right: immature (CD21/CD35lo, CD23lo), follicular (CD21/CD35mid, CD23hi), and marginal zone (CD21/CD35hi, CD23lo) B-cell populations. All numbers indicate the proportion of displayed events falling within the associated windows. (B-C) Data are representative of results from at least 3 chimeras (supplemental Figure 2). (D) Survival of transduced Traf2ΔB B cells in vitro. Lymph node cells from chimeras were incubated for 4 days in unsupplemented media. The proportion of input transduced B cells (CD45.1−, B220+, GFP−, hCD4+) that survived was calculated and expressed as a fraction of the mean value obtained for vector-transduced B cells. Points indicate duplicate data from individual chimeras mice. Bars represent means. (E) GC differentiation of transduced Traf2ΔB B cells in vivo. Spleens from chimeras were harvested 7 days after SRBC challenge. The proportion of transduced B cells (CD45.1−, B220+, GFP−, hCD4+) displaying a GC B-cell phenotype (CD38lo, Fashi) were expressed as a fraction of proportion of wild-type B cells (CD45.1+, B220+) in the same spleen that possessed the GC B-cell phenotype. (D-E) Data represent pooled results from 2 independent experiments. Points represent data from individual chimeras. Bars represent means.
After 8 weeks of reconstitution, transduced Traf2ΔB B cells from the spleens and lymph nodes of chimeric mice were analyzed by flow cytometry. B cells transduced with empty vector exhibited the phenotype typical of TRAF2-deficient B cells, including expression of high levels of surface CD21/CD35 (Figure 7B; supplemental Figure 2B) and increased proportions of MZ phenotype B cells (CD21/CD35hi,CD23lo; Figure 7C; supplemental Figure 2C). Importantly, retroviral expression of wild-type TRAF2 led to reversal of both CD21/CD35 expression and MZ B-cell development to levels seen in normal wild-type B cells (Figure 7B-C; supplemental Figure 2B-C). In contrast, retroviral expression of either TRAF2Δ1-80 or TRAF2Δ283-293 failed to restore wild-type CD21/CD35 expression or MZ B-cell development, indicating that these mutants are nonfunctional in these respects. Several additional TRAF2 mutants were tested in this way, with a mutant lacking the first 28 amino acids before the RING finger domain of TRAF2 restoring wild-type CD21/CD35 expression and MZ B-cell development, and mutants lacking the C-terminal TRAF-C domain failing to do so (supplemental Figure 2B-C).
Transduced B cells were also tested for their ability to survive in vitro and to undergo GC B-cell differentiation in vivo. As expected, B cells reconstituted with wild-type TRAF2 exhibited the low in vitro survival and high in vivo GC B-cell differentiation responses characteristic of wild-type B cells (Figure 7D-E). However, B cells reconstituted with either TRAF2Δ1-80 or TRAF2Δ283-293 maintained the high in vitro survival and poor in vivo GC B-cell differentiation typical of TRAF2-deficient B cells (Figure 7D-E). Thus, both the RING finger domain and the cIAP1/cIAP2-binding site of TRAF2 are essential for it to control B-cell survival and responsiveness. The close phenotypic similarities between TRAF2- and cIAP1/cIAP2-deficient B cells can therefore be attributed to the fact that these proteins must directly bind to each other to regulate B-cell survival and responsiveness in vivo.
Discussion
Previous in vitro analyses have indicated that cIAP1 and cIAP2 play pivotal but redundant roles in the regulation of a number of signal transduction pathways.7,14-18 The largely normal phenotypes of cIap1−/− and cIap2−/− mice25,26 are consistent with this picture. However, verifying whether cIAP1 and cIAP2 function redundantly within in vivo physiologic situations has not previously been possible because of the close (∼ 15 kb) linkage of cIap1 and cIap2 on chromosome 9.19 This problem has been overcome here by the generation of mice homozygous for an engineered chromosome 9 in which the contiguous cIap1 and cIap2 genes have been modified with loxP and FRT sites, respectively. By combining global cIAP2 deficiency with B-cell specific inactivation of cIAP1 expression via Cd19-Cre, we have provided the first confirmation that these genes play critical but redundant functions in vivo. As previously seen for Traf2ΔB and Traf3ΔB mice,21-23 simultaneous deletion of cIap1 and cIap2 in B cells led to their accumulation in vivo and elevated activation of the alternative NF-κB pathway. Strikingly, we also showed that removing expression of TRAF2, TRAF3, or cIAP1/cIAP2 from B cells allowed them to develop and survive in vivo completely independent of the normally essential BAFF-R molecule. These data show that TRAF2, TRAF3, and cIAP1/cIAP2 perform independent but cooperative functions to suppress B-cell survival. In addition, they demonstrate that the primary role of BAFF-R is to reverse the constitutive inhibition of prosurvival pathways mediated by the collaborative action of TRAF2, TRAF3, and cIAP1/cIAP2.
In combination with previous data published by our own and other laboratories, the results presented here support the following model for the cooperative regulation of B-cell survival by TRAF2, TRAF3, and cIAP1/cIAP2 (supplemental Figure 3). If BAFF does not bind to BAFF-R or BAFF-R is not expressed on the B cell, TRAF3 constitutively binds to NIK, facilitating the binding of TRAF2 to NIK and the TRAF2-mediated recruitment of cIAP1/cIAP2 to the complex.7,16 This predicts that TRAF2 must bind cIAP1/cIAP2 to suppress B-cell survival signals in vivo, a result we confirmed here by showing that TRAF2Δ283-293, a non–cIAP1/cIAP2-binding TRAF2 mutant,35 fails to reverse the extended survival phenotype of Traf2ΔB B cells (Figure 7D). cIAP1/cIAP2 recruited to NIK mediates its K48-ubiquitylation and thus targets NIK for degradation in the proteasome,14,15,38 which in turn suppresses NF-κB2 processing and B-cell survival (supplemental Figure 3A). To overcome the constitutive repression of NIK and B-cell survival by TRAF2, TRAF3, and cIAP1/cIAP2, BAFF-R recruits TRAF3, which triggers TRAF2- and cIAP1/cIAP2-dependent TRAF3 degradation22 (Figure 3A; supplemental Figure 3B). Reducing TRAF3 levels in this way removes the cofactor required for recruitment of the TRAF2-cIAP1/cIAP2 complex to NIK, thereby preventing NIK degradation (supplemental Figure 3B). The absence of TRAF3 in Traf3ΔB B cells therefore mimics maximal BAFF-R signaling and promotes B-cell survival, even in the absence of BAFF-R (Figure 4; supplemental Figure 3D). The absence of cIAP1/cIAP2 or TRAF2, on the other hand, prevents NIK degradation by either deleting the key K48 ubiquitin ligase (cIAP1/cIAP2) or removing its means of recruitment to NIK (TRAF2; supplemental Figure 3C,E).
Complementation of TRAF2 expression in Traf2ΔB B cells with retrovirally expressed TRAF2 mutants demonstrated the essential role of the interaction between TRAF2 and cIAP1/cIAP2 in suppression of B-cell survival signals (Figure 7D). This was also true for CD21/CD35 expression and MZ B-cell differentiation (Figure 7B-C). Importantly, TRAF2 molecules lacking the RING finger domain were also nonfunctional (Figure 7) despite retaining the ability to bind cIAP1/cIAP2.12,35 One explanation for this is that the TRAF2 RING domain K63-ubiquitylates cIAP1/cIAP2 and thus promotes its K48-ubiquitylation activity.7,16 The requirement for the TRAF-C domain of TRAF2 (supplemental Figure 2) is less clear. The TRAF-C domain is not required for cIAP1/cIAP2 binding12 but instead may be involved in establishing an effective binding to the TRAF3-NIK complex.
In contrast to the virtually identical phenotypes of mature naive B cells lacking expression of TRAF2, TRAF3, or cIAP1/cIAP2, the ability of the same B cells to activate CD40-dependent signaling in vitro (Figure 5) and CD40-dependent GC differentiation in vivo (Figure 6) varied greatly. Nevertheless, TRAF2- and cIAP1/cIAP2-deficient B cells displayed similar hyporesponsive phenotypes. Our analysis of Traf2ΔB B cells expressing TRAF2Δ283-293 once again indicated that this phenotypic similarity is because TRAF2 must interact with cIAP1/cIAP2 to function, at least in sustaining an in vivo GC B-cell response (Figure 7E). TRAF3-deficient B cells, on the other hand, made unimpaired and even slightly enhanced CD40-dependent responses both in vitro and in vivo.
In addition to the critical roles of BAFF-R and CD40 in regulating B-cell survival and responsiveness, the signaling pathways triggered through these receptors appear to play a significant role in the generation of several malignancies of the B-lymphocyte lineage.39,40 Consistent with this is the fact that NF-κB activation, a major outcome of both BAFF-R and CD40 signaling, is commonly associated with many B-lineage tumors, including diffuse large B-cell lymphoma,41 Hodgkin lymphoma,42 and MM.43 The high-level activation of the alternative NF-κB pathway and extended BAFF-R–independent survival of TRAF2-, TRAF3-, and cIAP1/cIAP2-deficient B cells indicates that they are all strong candidates for tumor suppressor proteins within the B-lymphocyte lineage. Strikingly, somatically acquired deletions or mutations in the TRAF2, TRAF3, or the linked cIAP1/cIAP2 loci were recently found to be common in human MM primary samples and cell lines.31,32 Inactivation of TRAF3 was particularly frequent, suggesting that mutations resulting in the absence of TRAF3 as opposed to TRAF2 or cIAP1/cIAP2 activity probably favor the development of MM. The phenotypic comparisons between Traf2ΔB, Traf3ΔB, and cIap1ΔB.cIap2−/− mice do not indicate that absent TRAF3 expression promotes mature B-cell survival any more than loss of TRAF2 or cIAP1/cIAP2 expression does. However, MM is a malignancy of terminally differentiated plasma cells generated from active GC responses. It is possible, therefore, that mutations in TRAF3 are most common in MM because they not only allow factor-independent survival but, unlike TRAF2 and cIAP1/cIAP2 mutations, do not retard the GC responses required to generate the plasma cells that represent the precursors of MM cells. Thus, the different functions of TRAF2, TRAF3, and cIAP1/cIAP2 in regulating B-cell survival and differentiation probably influence their precise roles as tumor suppressors in B-lineage malignancies.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the staff of the Garvan Institute and La Trobe University animal facilities for animal husbandry, Tahra Camidge and Katherine Wood for mouse screening and practical assistance, Elissa Deenick for assisting with intravenous injections, Chris Brownlee and the Garvan flow cytometry facility, Prof Klaus Rajewsky for providing Tnfr13c−/− mice, and Drs Shane Gray, Alex Swarbrick, and Stuart Tangye for critically reviewing the manuscript.
This work was supported by the National Health and Medical Research Council of Australia (program grant 427620, A.B., R.B.; project grants 433013, 541901, and 541902, J.S.; and project grants 384404 and 433063, D.L.V.) as well as a Leukemia & Lymphoma Society Center (D.L.V.). S.G. was supported by a National Health and Medical Research Council Postgraduate Research Scholarship. V.M.T. was supported by an Australian Postgraduate Research Award and Cancer Institute of NSW Award. J.S. and R.B. were supported by National Health and Medical Research Council Senior Research Fellowships.
Authorship
Contribution: S.G., V.M.T., J.S., A.B., F.K., D.L.V., and R.B. designed research; S.G., V.M.T., H.A., S.L., and F.K. performed research; S.G., V.M.T., J.S., and R.B. analyzed and interpreted data; and S.G., J.S., and R.B. wrote the manuscript.
Conflict-of-interest disclosure: J.S. is a consultant for TetraLogic Pharmaceuticals. D.L.V. is on the scientific advisory board of TetraLogic Pharmaceuticals. The remaining authors declare no competing financial interests.
The current affiliation of S.L. is Department of Immunology, Concord Hospital, Concord NSW, Australia. The current affiliation of J.S. is Walter and Eliza Hall Institute of Medical Research, Parkville, Australia.
Correspondence: Robert Brink, Immunology Research Program, Garvan Institute of Medical Research, 384 Victoria Street, Darlinghurst NSW 2010, Australia; e-mail: r.brink@garvan.org.au.
References
Author notes
S.G. and V.M.T. contributed equally to this study.
J.S. and R.B. contributed equally to this study.