Abstract
The role of transplantation in infants with acute lymphoblastic leukemia (ALL) is not defined. We analyzed results of 40 infants diagnosed before age 12 months who received a hematopoietic cell transplant (HCT) between July 1982 and February 2003 in first complete remission (CR1; n = 17), CR2/3 (n = 7), or relapse (n = 16). Patients were conditioned with cyclophosphamide with total body irradiation (n = 39) or busulfan (n = 1). Donors were matched related (n = 8), mismatched related (n = 16), or unrelated (n = 16). Graft-versus-host disease (GVHD) prophylaxis was methotrexate or cyclosporine (n = 7) or methotrexate plus cyclosporine (n = 33). Thirty-nine patients engrafted, 20 developed acute GVHD, and 7 developed chronic GVHD. Sixteen patients relapsed and 7 died of other causes. Patients in CR1 had disease-free survival (DFS) of 76% compared with 45% for CR2/CR3 and 8% for relapse (P < .001). Of 33 patients with cytogenetic data, 26 (79%) had MLL gene rearrangement. Fourteen of these 26 were in CR1 and 11 survive in remission. Outcome was associated with phase of disease, but having the MLL gene was not a factor predictive of outcome. Late effects included growth and other hormone deficiencies. These data demonstrate that infants with ALL and MLL gene have excellent DFS when they received transplants in CR1, and consideration for transplantation in CR1 is warranted.
Introduction
Acute lymphoblastic leukemia (ALL) occurring in infants is rare and is characterized clinically by hyperleukocytosis, hepatosplenomegaly, and a high incidence of central nervous system (CNS) disease. Features associated with a particularly poor prognosis following chemotherapy include being younger than 6 months of age at diagnosis, MLL gene rearrangement, CD10- leukemia cell phenotype, and elevated white blood cell count (WBC) at diagnosis.1-4 The presence of the MLL gene rearrangement is the most significant, independent factor predictive of poor outcome.5-9 Event-free survival of infant patients with ALL treated with conventional chemotherapy, including recent intensive multiagent chemotherapy, ranges from 25% to 45%.3,10-12
To date, little data are available regarding the efficacy of allogeneic hematopoietic cell transplantation (HC transplantation) in the treatment of infants with ALL.3,13-20 Pirich et al17 reported 7 infants with ALL who received an allogeneic hematopoietic cell transplant (HCT) following a preparative regimen with 12.0 Gy total body irradiation (TBI), etoposide, and cyclophosphamide (CY). Four of these 7 patients survived from 1.3 to 5.4 years at the time of the report. Marco et al18 reported 3 of 4 patients with infant ALL who survived 1, 15, and 17 months after chemotherapy-only preparative regimen and allogeneic HC transplantation. Pui et al9,21 reported outcome of infants with t(4;11) ALL treated by cooperative groups or single institutions. Those infants had a survival rate of 33% for the 103 who received chemotherapy and a survival rate of 25% among the 28 who received any type of HCT.9,21
We have previously reported the outcome for 4 infants with ALL as part of a larger cohort of children receiving unrelated donor transplants for ALL.22 The present report updates those results and expands the analysis to include 36 additional infants with ALL for a total of 40 infants with ALL who were diagnosed younger than 1 year of age and referred to the Fred Hutchinson Cancer Research Center (FHCRC) for allogeneic transplantation. Results demonstrate excellent outcome for the infants who received transplants in remission.
Patients, materials, and methods
Between July 1982 and February 2003, 40 consecutive children received an allogeneic HCT at FHCRC for ALL diagnosed when younger than 12 months of age and were analyzed as of July 2004. The diagnosis made at the referring institution was confirmed by HC transplantation team review of the diagnostic marrow, cytogenetic analyses, patient medical records, and laboratory data. Patients received initial chemotherapy according to active protocols at the referring institution. Remission or relapse status was determined with bone marrow pathology and cytogenetics review and cerebrospinal fluid analysis performed within 2 weeks prior to initiating the transplantation preparative regimen. Patients who received therapy for their first or second relapse and achieved less than 5% blasts in the marrow and had no extramedullary sites of leukemia were considered to be in second or third remission. Patients whose marrow showed more than 5% blasts with or without evidence of extramedullary disease were considered to be in relapse. Of 33 patients with initial diagnostic cytogenetic studies available, 26 patients had the 11q23 translocation, the MLL gene rearrangement, or both. Two patients also had a hypodiploid karyotype with 42 to 45 chromosomes and the MLL gene rearrangement. The Institutional Review Board (IRB) at FHCRC approved the protocols and consent forms used for these studies, and informed consent was obtained from parents or guardians according to IRB policies.
All patients and donors had histocompatibility testing performed by the Clinical Immunogenetics Laboratory at FHCRC. The standard National Institutes of Health 2-stage microtoxicity assay was used for typing of human leukocyte antigen (HLA)–A and -B antigens.23 HLA-DR typing was done by using nylon wool–purified B lymphocytes in a modified microtoxicity assay. From 1990 on, HLA-D region compatibility was determined by identification of DRB1 alleles through hybridization of sequence-specific oligonucleotide probes.24 All mismatched and unrelated donor-recipient pairs had additional testing with lymphocyte crossmatching before transplantation.25 Matched donor and recipient pairs were identical at HLA-A, -B, -C, and -DR loci.
Myeloablative transplantation preparative regimens were administered to all patients. Regimens used were dependent on the protocols active at the time of the transplantation and were determined by the phase of disease and the type of donor. From 1982 to 1999 TBI was delivered from dual opposing Co60 sources, and from 1999 onward TBI was delivered by using single-source linear accelerator. TBI regimens included CY 60 mg/kg/d for 2 days. One patient received busulfan and CY, and 39 patients received TBI-containing conditioning regimens. After 1986, all boys (n = 9) also received 400 cGy prophylactic testicular irradiation immediately prior to administration of the TBI, and 1 patient with leukemia cutis received 10.0 Gy total skin irradiation. All patients received 2 intrathecal injections of methotrexate before transplantation and were scheduled to receive 4 intrathecal injections of methotrexate after transplantation.26
Hematopoietic cell grafts included unmanipulated bone marrow (BM) from 24 related and 13 unrelated donors, peripheral blood stem cells from 1 unrelated donor, and cord blood from 2 unrelated donors all collected according to established methods.27-29 Hematopoietic cell products were infused through a central venous catheter on day 0, at least 36 hours after the last dose of preparative chemotherapy or within 24 hours after the last dose of irradiation. The median number of nucleated cells infused into the recipient was 6.5 × 108/kg recipient body weight (range, 2.4-22 × 108/kg) for the patients who received BM.
All patients had indwelling central venous catheters and received nutritional support with hyperalimentation. Infection prophylaxis included prophylactic antibiotics for all patients, and other measures varied according to the standard of practice at the time of BM transplantation, including fluconazole for fungal prophylaxis30 and ganciclovir for cytomegalovirus (CMV) prophylaxis,31,32 as well as use of single conventional or laminar airflow rooms, growth factors, and intravenous immunoglobulin.
The day of engraftment was defined as the first of 3 consecutive days on which the granulocyte count exceeded 0.5 × 109/L. Patients were not considered to be evaluable for engraftment if they died without achieving a granulocyte count greater than 0.5 × 109/L before day 28. Donor engraftment was determined by fluorescence in situ hybridization (FISH) for X or Y chromosomes in sex-mismatched transplantations33 or by DNA-based assays for variable number of tandem repeats (VNTRs) in the case of sex-matched transplantations.34
All patients received prophylaxis for acute graft-versus-host disease (GVHD), using either methotrexate (MTX) or cyclosporine (CSP) alone or in combination.35 Acute and chronic GVHD were diagnosed and graded according to standard criteria.27,36,37 Patients were not considered to be evaluable for acute GVHD if they died before engraftment, or for chronic GVHD if they died before day 80 after transplantation.
Medical records, including neurodevelopmental, laboratory, and radiographic studies, were reviewed for long-term side effects. Late effects studied included endocrine, pulmonary, cardiac, dental, orthopedic, ophthalmologic, and growth and development. Dual-energy X-ray absorptiometry (DEXA) scans were performed on a Lunar DPX-Alpha (Madison, WI) or Hologic QDR-4500 (Bedford, MA) machine. Pulmonary function studies were performed on a SenorMedics Model 2200 or 6200 (Yorba Linda, CA) for patients when they became older than 6 years of age. Growth was evaluated by annual reports of height measurements and height standard deviation (SD) scores calculated as height minus mean height for age and sex divided by the SD of height for age and sex. Periodic evaluation of hormonal deficiency included measurements of the growth hormone (GH), thyroxine (T4), thyroid stimulation hormone (TSH) in all ages of patients; luteinizing hormone (LH), follicle stimulating hormone (FSH), and estradiol in girls older than 10 years of age; and testosterone in boys older than 10 years of age. Spontaneous nocturnal and clonidine-stimulated GH secretions were measured to detect GH deficiency. Neuropsychologic development was evaluated by using Full Scale Intelligence Quotient (FSIQ) tests appropriate for the age of the patient at testing.38,39
For statistical methods, Cox regression models were used to assess the association of various pretransplantation factors with the hazard of failure appropriate to various time-to-event endpoints, including overall survival, disease-free survival, and chronic GVHD. Logistic regression was used to assess the association of the same pretransplantation factors with the probability of grades II to IV acute GVHD, and linear regression was used for time to engraftment. Kaplan-Meier estimates were used to summarize estimates of overall and disease-free survival,40 and cumulative incidence estimates were used to summarize relapse, nonrelapse mortality, and chronic GVHD.41 The pretransplantation factors examined for association with the various endpoints included cytogenetic risk (high-risk versus others), phase of disease (first complete remission [CR1] versus beyond CR1 versus relapse), patient sex, patient and donor CMV serostatus, and type of donor (matched sibling versus nonsibling relative versus unrelated). All reported P values are 2-sided, and those estimated from regression models were derived from the Wald test. No adjustments were made for multiple comparisons.
Results
Patient characteristics at diagnosis and transplantation
Patient characteristics at the time of diagnosis are shown in Table 1, and the characteristics at time of transplantation are shown in Table 2. Overall the median age at transplantation was 15 months (range, 6.1-67.1 months), and the median time from diagnosis to transplantation was 7.1 months (range, 2.7-58.9 months). The median time from diagnosis to transplantation for the 17 patients in CR1 was 5.6 months (range, 2.7-8.1 months). Among the 17 patients in CR1, 8 (47%) were aged 6 months or younger at diagnosis, 12 (71%) had initial WBC of greater than 50 × 109/L, and 15 (88%) had t(11q23) cytogenetic abnormality, the MLL gene rearrangement, or both. Central nervous system disease was present at diagnosis in 4 (17%) of 24 patients who received transplants in remission (2 patients in CR1 and 2 patients in CR2/3) and in 5 (31%) of 16 patients who received transplants in relapse. In addition, 3 of the patients in CR1 also had a history of significant leukemia cutis, 1 of the patients in CR1 had a cutaneous orbital mass that was treated with 900 cGy radiotherapy prior to referral for HC transplantation, and 2 of the patients who received transplants in relapse had CNS disease presenting at the time of relapse. One of those patients received 18 Gy cranial irradiation prior to referral for transplantation, and the second patient received 10.0 Gy to the fontal lobe mass immediately prior to transplantation.
The transplantation preparative regimen included TBI for all except 1 patient in CR3 who received busulfan and CY. Two patients received a preparative regimen that included cytosine arabinoside and CY plus 12.0 Gy TBI fractionated over 6 days, 23 patients received CY and 13.20 to 14.40 Gy TBI fractionated over 4 days, and 13 patients received CY plus 15.75 Gy TBI fractionated over 7 days. The donors included an HLA-matched sibling for 8 patients, 1-antigen–mismatched family member for 7 patients, a 2-antigen–mismatched parent for 4 patients, a 3-antigen–mismatched parent for 5, a matched unrelated donor for 14 patients, and a mismatched unrelated donor for 2 patients.
Engraftment
Thirty-nine of the 40 patients achieved a sustained granulocyte count greater than 0.5 × 109/L at a median of 18 days (range, 8-31 days) after transplantation. One patient died on day 27 of severe veno-occlusive disease (VOD) with a granulocyte count below 400 × 109/L. The univariate analysis suggested that risk factors associated with delayed engraftment included transplantation from a nonsibling relative or transplantation in relapse. Patients who received transplants in relapse engrafted an average of 3.2 days later than patients who received transplants in CR1 (P = .10). Patients who received transplants from a nonsibling relative engrafted an average of 4.7 days later than patients who received transplants from a matched-sibling donor (P = .05). The multiple linear regression model confirmed that patients who received transplants from a nonsibling donor engrafted an average of 4.3 days later than patients who received transplants from a matchedsibling or unrelated donor (P = .01) (Tables 3 and 4).
Acute and chronic GVHD
Acute GVHD was assessed in 39 of the 40 patients (1 patient who died on day 27 was not considered evaluable). Twenty-four (62%; 95% confidence interval [CI], 45%-77%) of the 39 evaluable patients developed grades II to III acute GVHD (17 grade II, 7 grade III). No patient developed grade IV acute GVHD. Patients who were CMV positive were more likely to develop grades II to III acute GVHD compared with CMV-negative patients (unadjusted odds ratio [OR] = 6.0; 95% CI, 1.1-32.6; P = .04). The odds of developing grades II to III acute GVHD among patients who received transplants from a matched-sibling donor were 0.3 times that among patients who received transplants from an alternative donor (95% CI, 0.1-1.4; P = .13). In a multivariable logistic regression model, patients who were CMV seropositive had an increased odds ratio of 13.0 (95% CI, 1.3-126.8; P = .03) compared with CMV-negative patients, while those who received transplants from a matched-sibling donor had a decreased odds ratio of grades II to III acute GVHD compared with alternate donors (OR = 0.1; 95% CI, 0.01-1.1; P = .06) (Tables 3 and 4).
Clinically extensive chronic GVHD developed in 7 patients, leading to an estimated 2-year probability of 17.5% (95% CI, 6%-29%) for all patients. Among the 28 patients who survived without relapse beyond day 80, the estimated 2-year probability of clinical extensive chronic GVHD was 24% (95% CI, 9%-40%). The 7 patients who developed clinically extensive chronic GVHD received transplants from an HLA 2- to 3-antigen–mismatched parent (n = 3), 1-antigen–mismatched unrelated donor (n = 1), 1-antigen–mismatched unrelated cord blood donor (n = 1), and matched unrelated donor (n = 2). Among these 7, 4 patients were in CR1, 1 was in CR2, and 2 were in relapse. All patients with extensive chronic GVHD required therapy with corticosteroids and other immunosuppressive agents from 9 to 27 months.
An additional 5 patients developed limited chronic GVHD that did not require immunosuppressive therapy. These 5 patients received transplants from an HLA-identical sibling (n = 1), a 1-antigen–mismatched relative (n = 1), and matched unrelated donor (n = 3). The overall estimated 2-year probability of chronic GVHD was 30% (95% CI, 16%-44%) among all patients and 41% (95% CI, 23%-59%) among patients who survived without relapse beyond day 80. Patients who received transplants from a matched-sibling donor had a suggestively lower hazard of clinical chronic GVHD compared with those who received transplants from a nonsibling or unrelated donor (hazard ratio [HR] = 0.2; 95% CI, 0.02-1.20; P = .07).
Nonrelapse death
Seven patients died between day 23 and 54 of causes not related to recurrent leukemia. The cause of death for 3 patients was VOD (1 in second remission and 2 in relapse). Two patients died of pulmonary hemorrhage (1 in CR1 and 1 in relapse), and 2 died of viral pneumonia (1 in CR1 and 1 in relapse).
Relapse
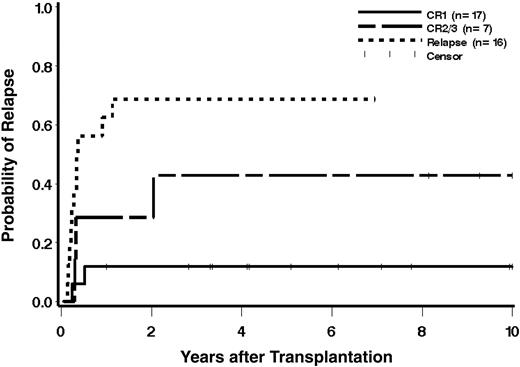
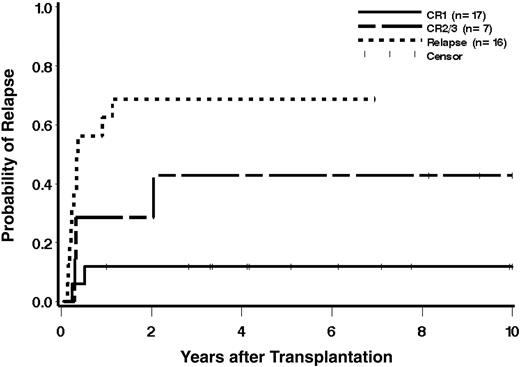
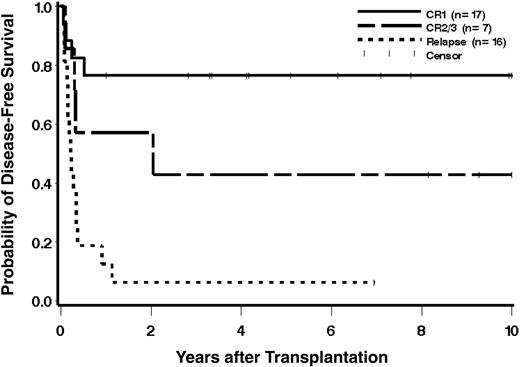
Sixteen patients relapsed at a median of 114 days (range, 51-746 days) after transplantation. The estimated 1-year probability of relapse was 35% (95% CI, 20%-50%) and 3-year probability of 40% (95% CI, 25%-56%). The estimated probability of relapse at 1 year according to phase of disease at transplantation was 12% (2 relapses among 17 patients), 43% (3 relapses among 7 patients), and 69% (11 relapses among 16 patients), respectively, for patients with CR1, CR2/3, and relapse (Figure 1). All 16 patients who relapsed after HC transplantation died of progressive disease.
Cumulative incidence estimates of the probability of relapse according to phase of disease at transplantation. Patients alive without relapse beyond 10 years (at 13.5 and 17.0 years) and 1 patient who received a transplant in CR2/3 alive without relapse beyond 10 years (at 11.6 years) are indicated as censored observations at 10 years.
Cumulative incidence estimates of the probability of relapse according to phase of disease at transplantation. Patients alive without relapse beyond 10 years (at 13.5 and 17.0 years) and 1 patient who received a transplant in CR2/3 alive without relapse beyond 10 years (at 11.6 years) are indicated as censored observations at 10 years.
Patients who received transplants beyond CR1 had a suggestively increased hazard of relapse compared with patients who received transplants in CR1 (HR = 4.4; 95% CI, 0.7-26.1; P = .11), and patients who received transplants in relapse had a statistically significantly increased hazard of relapse compared with the CR1 group (HR = 15.5; 95% CI, 3.3-71.9; P = .001). Patients who received transplants from a nonsibling donor had a hazard 2.7 times that of patients who received transplants from a matched-sibling or unrelated donor (95% CI, 1.0-7.3, P = .05). However, once stage of disease is accounted for, the association between donor and outcome is diminished (HR = 2.0, P = .17). Having high-risk cytogenetics was not statistically significantly associated with development of recurrent leukemia.
Overall and event-free survival
Overall, 17 of 40 patients survive with a median follow-up of 7 years (range, 1-17 years). One of the 12 patients who had extramedullary disease survives, but 5 died of relapse and 6 died of nonrelapse complications. The estimated probabilities of survival at 1 year and 3 years are 53.0% (95% CI, 37.0%-68.0%) and 50.0% (95% CI, 34.3%-65.4%), respectively. Patients who received transplants beyond CR1 had a hazard of death 2.6 times that of patients who received transplants in CR1, although the difference was not statistically significant (95% CI, 0.6-10.3, P = .18). Patients who received transplants in relapse had a statistically significantly increased hazard compared with those who received transplants in CR1 (HR = 8.1; 95% CI, 2.6-25.1; P = .001). Patients who received transplants from a nonsibling donor had an increased hazard of death compared with patients who received transplants from a matched-sibling donor (HR = 4.6; 95% CI, 1.3-16.3; P = .02), and patients who received transplants from an unrelated donor had a higher hazard of death relative to matched-sibling patients, but the difference was not statistically significant (HR = 1.6; 95% CI, 0.4-6.2; P = .49). Among 24 patients who received transplants in CR, 8 of 9 who received transplants from URDs survive.
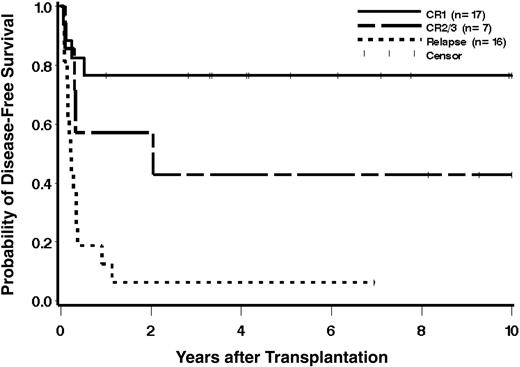
The 1-year and 3-year estimates of disease-free survival (DFS) are 47.5% (95% CI, 32.0%-63.0%) and 42.2% (95% CI, 26.8%-57.6%), respectively. The 3-year DFS estimates according to phase of disease were 76%, 43%, and 6% for patients who received transplants in CR1, in CR2/3, and in relapse, respectively (Figure 2). Only 1 of the 12 patients with extramedullary disease survives with 5 dying of relapse and 6 dying of transplantation complications.
Cumulative incidence estimates of the probability of disease-free survival according to phase of disease at transplantation. Patients alive without relapse beyond 10 years (at 13.5 and 17.0 years) and 1 patient who received a transplant in CR 2/3 alive without relapse beyond 10 years (at 11.6 years) are indicated as censored observations at 10 years.
Cumulative incidence estimates of the probability of disease-free survival according to phase of disease at transplantation. Patients alive without relapse beyond 10 years (at 13.5 and 17.0 years) and 1 patient who received a transplant in CR 2/3 alive without relapse beyond 10 years (at 11.6 years) are indicated as censored observations at 10 years.
Fourteen of 26 patients with high-risk cytogenetics received transplants in CR1 and 11 survive without disease, 1 died of recurrent leukemia, and 2 died of transplantation complications. One of the 3 who received a transplant in CR2/3 and none of the 8 who received transplants in relapse survive.
Long-term side effects
Seventeen patients survived disease free for more than 1 year after transplantation. Long-term side effects were evaluated in those 17 patients at a time when they were 6.1 years (range, 1.0-17.0 years) after transplantation. Sixteen patients had not received cranial irradiation other than that given with the TBI, and 1 had received 900 cGy orbital irradiation for extramedullary disease.
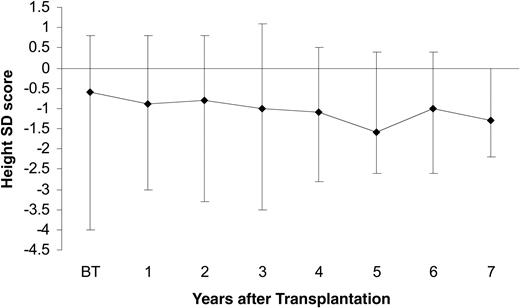
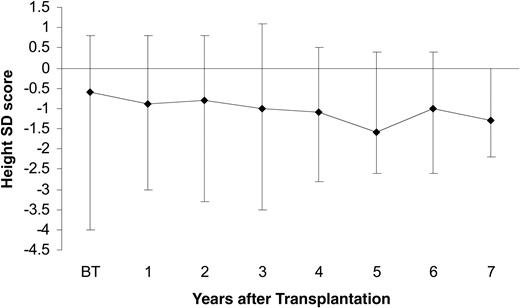
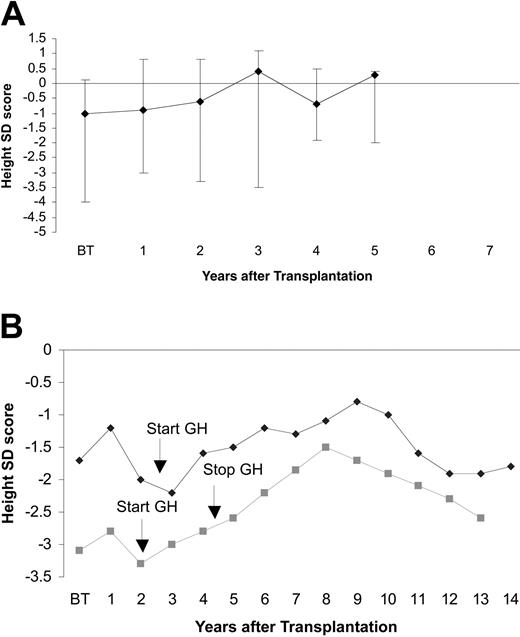
Growth. Height data were available for 19 patients. Median height standard deviation (SD) scores for 17 patients in Figure 3 shows that with increasing time after transplantation the median height SD scores declined gradually and fell below -1 SD at 3 years, and by 7 years the median height was -1.3 (-2.2 to 0.0) SD. GH production was evaluated in 14 patients at 1 or more years after transplantation. Twelve of these 14 patients had biochemical GH deficiency as evidenced by low secretion of spontaneous GH and subnormal stimulated GH values, but only 2 had developed growth failure, requiring GH therapy. Figure 4A shows the growth rates without GH therapy and Figure 4B shows the growth rates for the 2 patients receiving GH therapy.
Height standard deviation (SD) scores after transplantation for 19 patients surviving for longer than 1 year. Bars represent the height SD range. Line connects the median height at each time point. BT indicates before transplantation.
Height standard deviation (SD) scores after transplantation for 19 patients surviving for longer than 1 year. Bars represent the height SD range. Line connects the median height at each time point. BT indicates before transplantation.
Height SD score for patients with growth hormone deficiency and those treated with growth hormone supplemental therapy. (A) Height SD score for 12 patients with growth hormone deficiency. Bars represent height SD range. Line connects the median height at each time point. (B) Height SD scores for 2 patients who have been treated with growth hormone supplemental therapy.
Height SD score for patients with growth hormone deficiency and those treated with growth hormone supplemental therapy. (A) Height SD score for 12 patients with growth hormone deficiency. Bars represent height SD range. Line connects the median height at each time point. (B) Height SD scores for 2 patients who have been treated with growth hormone supplemental therapy.
Thyroid. Thyroid function studies with T4 and TSH were available for 18 patients. Five of these 18 developed compensated hypothyroidism with elevated TSH levels and normal T4 levels at a median of 4.2 years (range, 1.6-10.9 years) after transplantation. In 3 patients, spontaneous reversion to normal thyroid function occurred 1 to 2 years after abnormal function was discovered, but 2 patients continue to have compensated hypothyroidism. One patient is being treated with thyroid hormone and the other is not. No case of overt hypothyroidism has been observed. One patient with normal thyroid function tests developed a benign follicular adenoma at 9 years after transplantation that was treated with a total thyroidectomy with subsequent thyroid hormone supplementation.
Diabetes. One patient developed type 2 diabetes at 9.7 years after transplantation, requiring insulin. One patient was found to have an abnormal glucose tolerance test.
Pubertal development. Fifteen patients are younger than 12 years and hence are prepubertal. Four patients, currently older than 12 years, were evaluated for pubertal development. Of the 4 patients, 1 boy had normal pubertal development, 1 boy and 1 girl had early pubertal development that was classified by the pediatric endocrinologist as precocious puberty, and data are not available for 1 girl. The girl with precocious puberty is being treated with leuprolide acetate (Lupron).
Cataract. Six of 19 patients evaluated have developed mild subcapsular cataracts at a median follow-up of 5.6 years (range, 2.7-10.8 years) after transplantation. No patient required surgical removal of the cataracts. There were no other ophthalmologic complications.
Pulmonary function. All 10 patients who had pulmonary function tests performed were older than 6 years, and all study results demonstrated normal lung function at a median follow-up of 5.5 years (range, 2.5-10.8 years) after transplantation. No obstructive or restrictive disease has been observed. Three of these 10 patients had diffusing lung capacity for carbon monoxide (DLCO) measured that was normal in 2 and low (61%) in 1 patient. All 3 patients were asymptomatic.
Dental development. Eight patients had panographic dental radiographs of the teeth, 7 of which demonstrated abnormal findings, including small palate, missing secondary tooth buds, short roots on the primary teeth, small primary teeth, or pointed or otherwise abnormally shaped teeth. One of those children received orthodontic corrective therapy.
Bone. Bone mineral density studies have been performed for 7 patients older than 5 years. Four patients had osteopenia by DEXA scan with a median z score of -1.48 (-1.1 to -1.53) at the median time of 3.5 years (range, 1.0-6.1 years) after transplantation. No patient developed osteoporosis, none had a fracture occur, and none has avascular necrosis. Two patients developed osteochondroma, exostosis, or both of the left humerus, ulna, and digits.
Neuropsychiatric development. Assessments for neurodevelopment following transplantation were performed on 16 patients. One of 16 patients had a developmental delay at the time of transplantation as a result of extreme prematurity (26-week gestation) and mild cerebral palsy. Among the remaining 15 patients, 3 had normal development, 4 were average to slightly delayed in gross and fine-motor skills, 1 had developmental delay in gross and fine-motor skills, 6 had speech delay mostly mild to moderate, and 1 had developmental delay in both motor skills and language. IQ data were available for 4 patients. The mean (± SD) FSIQ, Verbal IQ, and Performance IQ scores were 103.8 (± 13.59), 106.5 (± 14.87), and 100.8 (± 10.83), respectively, at the median time of 2.2 years after transplantation and at the median age of 4.4 years.
Second HCT
Three patients, who received transplants in second CR (n = 1) or in relapse (n = 2), received second HCT for recurrent disease at 314, 413, and 816 days after first transplantation, respectively. All 3 patients received HCT from matched sibling donor and achieved another remission, but all 3 subsequently died of relapse at 2.5, 2.7, and 2.8 years after second transplantation.
Discussion
Despite marked advances in survival for childhood ALL, the outcomes for infants treated with conventional chemotherapy are significantly worse than for older children.10,12 Although reports of treatment using an intensive multiagent chemotherapy appear to result in improved survival for infants with ALL, the outcomes of most clinical trials are still unsatisfactory with overall event-free survival ranging between 23% and 40%.3,10-12,21,42-44 The present report demonstrates that it is possible to achieve an excellent DFS if patients are treated with myeloablative TBI-containing preparative regimen and HC transplantation in first remission. Infants who received HCT in first remission had significantly better survival and a significantly lower rate of relapse compared with infants who received transplants in relapse. Moreover, the dismal outcome of infant ALL with 11q23 abnormalities seen with chemotherapy approaches was not appreciated in the current study in which high-risk cytogenetic abnormalities were not significantly associated with DFS or relapse, although the power to detect such associations is limited by the number of events observed.
The present report represents the largest study evaluating the outcome of allogeneic HC transplantation for infants with ALL reported to date. Some small studies have observed encouraging outcomes for the infants with ALL using HC transplantation.17 Hilden et al7 suggested the possible role of allogeneic transplantation in the treatment of infant ALL, reporting that 3 of 8 patients who received allogeneic transplant survived. Pirich et al17 reported 7 infants with ALL who received allogeneic HCT following TBI, etoposide, and CY whereby 4 survived. Others have reported varying results using a non-TBI preparative regimen for a small number of infants.16-20 A Japanese group recently reported an event-free survival of 64.4% for 29 patients who received allogeneic transplants in first remission.45 These patients received the transplant at a median of 5 months from diagnosis from umbilical cord blood donors (n = 23) or family member marrow or peripheral blood stem cell donors (n = 6) following either a busulfan (n = 13) or TBI (n = 15) based preparative regimen.45 Marco et al18 noted that patients who received transplants earlier than 4 months after remission induction had a significantly better prognosis than those receiving transplants at later times. In the current series of patients, median time from diagnosis to transplantation for those in first remission was 5 months and hence not different from the Japanese series of patients.
Some series report disappointing outcomes for the infants with ALL who receive HCT. Chessells et al3 reported all 3 infants with ALL enrolled in cooperative group (Medical Research Council) studies died following HC transplantation. Children's Cancer Group found that only 2 of 12 patients who received transplants survived.12 Pui et al9,21 analyzed results of cooperative group and individual transplantation center data for patients with the 11q23 abnormality. Among the patients reported were 28 infants who received an HCT, whereby results indicated that infants had event-free survival of 19% ± 3% and that those given matched sibling marrow or marrow from an unrelated donor had outcomes that were not significantly different from those receiving chemotherapy.9,21 Pui et al also noted that any transplantation resulted in significantly worse outcome than those receiving chemotherapy. The reasons for this are not entirely clear as the patients were a median of 5 months between diagnosis and transplantation. No information was provided regarding the transplantation preparative regimen used, which may be a very important factor in the observed 50% incidence of recurrent leukemia among the patients who received transplants in the Pui et al21 report. The phase of the patient's disease, remission, or relapse at time of transplantation is also not included in the Pui et al21 report. It is well known that patients who receive transplants while in first remission have outcomes superior to those who receive transplants in later remissions or relapse. The present report demonstrates superior disease-free survival for infants who received transplants in first remission as compared with later remissions or relapse.
The present report demonstrates that the outcome for infants who received transplants in relapse is dismal, as has been previously shown.22 Our study confirms that reported by others who have demonstrated that phase of disease is the most important factor determining outcome after HC transplantation.19,22 In our series, the major cause of failure was relapse of disease. Sixteen of 40 patients relapsed after transplantation with the highest relapse incidence occurring in patients with advanced disease at time of transplantation. These data suggest that best results are obtained when the HC transplantation is performed while the patient is in remission.
The 11q23 abnormalities associated with rearrangements of the MLL gene are very common in infant ALL, and infants with 11q23 abnormality have poor outcomes.5-9 In our series, 76% of patients with evaluable cytogenetics had the MLL rearrangement, 56% of which received transplants in CR1. Analyses demonstrated that the presence of the MLL gene rearrangement was not significantly associated with poor outcome after transplantation as has been suggested by others, although the power to detect such differences is limited.9,21 Among 14 patients who received transplants in CR1 with 11q23 or MLL gene rearrangement, only 1 has relapsed and died. Among the remaining 13 patients, 2 died of pneumonia and 11 survive a median of 4 years after transplantation (range, 1-13 years) with a 3-year DFS estimate for this group of patients of 73%.
The TBI-containing conditioning regimen is widely used in HC transplantation for childhood ALL. The present study demonstrates that severe devastating late effects have not been observed when the only cranial irradiation was 13.20 to 15.75 Gy administered as fractionated TBI. The observations in the current study are in contrast to the late effects reported by Leung et al46 in which 75% of 34 infants had significant neurocognitive deficits and subnormal growth rates that were attributed to the 10 to more than 20 Gy cranial or cranial/spinal irradiation administered to most infants as part of their nontransplantation treatment regimens. It is tempting to speculate that the lack of severe devastating late effects among the infants in the present study may suggest a dose-response effect on the effect of irradiation to the young developing brain. To avoid long-term late effects as a result of radiotherapy administered to young children, several investigators have used non–TBI-conditioning regimens before HC transplantation for infant ALL, but outcomes have varied. The reports of these infants who received non-TBI preparative regimens unfortunately provide no details regarding late effects.16-20 In the present study, all surviving patients received a fractionated TBI-containing conditioning regimen and have not developed significant neurocognitive or growth deficits or any other late effects different from that expected for all children given TBI and HC transplantation.19,47,48
Our study suggests that HC transplantation can improve the survival for infants with ALL and should be considered for infants with MLL gene rearrangement early in the course of disease when patients are in CR1.
Prepublished online as Blood First Edition Paper, January 6, 2005; DOI 10.1182/blood-2004-08-3312.
Supported in part by National Institutes of Health (grants no. CA-18029).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.