Abstract
Preservation of hematopoietic stem and progenitor cell survival is required for recovery from radiation-induced myelosuppression. We recently showed that short-term injection of antiapoptotic cytokine combinations into mice soon after lethal gamma irradiation promoted survival. The present study investigated the hematopoietic response of cynomolgus monkeys to a single dose of stem cell factor, FLT-3 ligand, megakaryocyte growth and development factor, and interleukin-3 in combination (4F, each factor given intravenously at 50 μg/kg) administered 2 hours after 5-Gy gamma irradiation. Treated monkeys (n = 4) experienced no thrombocytopenia. Only 1 in 4 displayed a transient period of neutropenia (neutrophil [ANC] count < 0.5 × 109/L), whereas all irradiated controls (n = 4) experienced neutropenia (5-12 days) and thrombocytopenia (platelet [PLT] count < 20 × 109/L, 5-31 days). Treated animals exhibited an impressive 2-wave PLT response that peaked at days 8 and 22 after total body irradiation (TBI). Areas under the curve (AUC) of PLTs, ANCs, white blood cells (WBCs), and red blood cells (RBCs) between days 0 and 90 were significantly higher in treated animals than in controls. Humeral bone marrow–derived clonogenic activity was significantly spared at 24 hours and 4 days after TBI in treated monkeys. No apparent impairment of the hematopoietic status and stem cell pool, in terms of long-term culture–initiating cells (LTC-ICs) and side population (SP) cells, was observed after 15 months. These results strongly suggest that the 4F cytokine combination, as a single dose regimen, could act as an emergency treatment for nuclear accident or terrorism victims.
Introduction
After the Chernobyl accident, hematopoietic growth factors (HGFs) have been proposed as a substitutive or complementary therapeutic strategy to allogeneic bone marrow (BM) transplantation to rescue lethally irradiated victims.1 The rationale of HGF treatment is the presence of residual hematopoietic stem and progenitor cells (HSPCs) in BM areas after total body irradiation (TBI) due to the constitutive heterogeneity of dose distribution involving notably the attenuation related to body thickness.2,3 These “underexposed” HSPCs represent useful targets in order to accelerate hematopoietic recovery in addition to intrinsic radio-resistant stem cells.4 Numerous studies show the effectiveness of cytokines to stimulate these preserved targets and subsequent neutrophil and platelet recovery in myeloablated animals and humans.5 Granulocyte colony-stimulating factor (G-CSF), granulocyte-macrophage CSF (GM-CSF), and interleukin 3 (IL-3) have been pioneer cytokines whose in vivo evaluation has been largely documented.6-8 Highly active in granulocyte recovery, these molecules exhibit low activity on the megakaryocyte lineage. A second generation of cytokines such as IL-6 and IL-11 was shown to be very active on platelet stimulation.2,9 The search for the megakaryocyte colony-stimulating factor finally led to the discovery of thrombopoietin (TPO)/megakaryocyte growth and development factor (MGDF).10 Other approaches were based on the engineering of modified cytokine receptor agonists and fusion molecules or through the combination of cytokines to obtain multilineage reconstitution.5,7,8,11 As a clinical application of multiple cytokine therapy, G-CSF+MGDF+ erythropoietin in combination were given as a prolonged treatment to the victims of the recent criticality nuclear accident in Tokai Mura.12 However, these victims were grafted with hematopoietic stem cells and the proper therapeutic efficacy of HGF could not be assessed because of the toxicity related to allogeneic transplantation.
Initial therapeutic preclinical schedules were developed to induce a long-term proliferation and differentiation of HSPCs while avoiding interference with an early cytokine burst and a subsequent inflammatory process that follows TBI. Thus, HGFs were administered from the day after myeloablative injury for at least 15 days up to neutrophil and/or platelet recovery. Unfortunately, adverse effects,1 such as proinflammatory activity or immunogenicity might be linked to the duration of such schedules. For example, MGDF has proved to be immunogenic in the clinic after a few repeated injections in healthy volunteers.13 Moreover, the possible exhaustion of stem cell reservoir related to overstimulation of cell cycle machinery is still under debate.14 Consequently, a treatment schedule, based on early and short-term administration of TPO15,16 /MGDF,17 was evaluated in animal models for the sake of avoiding side effects of long-term treatment. An effectiveness like that of prolonged administration was demonstrated against thrombocytopenia, but poor granulopoietic capacity was observed.
We recently tested the effectiveness of the early and short-term administration of a combination of 4 cytokines including 3 early-acting factors.18 Using TPO as a thrombopoietic molecule, implementing stem cell factor (SCF) and FLT-3 ligand (FL) as survival factors and using IL-3 for its granulopoietic contribution, we speculated that this combination of 4 cytokines (4F) used soon after TBI could abrogate the period of pancytopenia. Based on previous in vitro studies,19-21 our goal was to counteract HSPC cell death in vivo and then initiate their proliferation and differentiation. We previously reported the capacity of 4F to rescue lethally irradiated mice (8 Gy gamma) from hematopoietic death with a persistent benefit regarding long-term survival.18 Moreover, we demonstrated that 4F effectiveness was related to the early protection against radiation-induced (RI) apoptosis at the HSPC level.
The purpose of the present study was 2-fold: first, assessing the capacity of a single dose of the 4F combination (SCF+FL+ MGDF+IL-3) to counteract myelosuppression in monkeys that were irradiated at 5-Gy 60Co gamma TBI, which results in a profound pancytopenia for 3 weeks; second, evaluating the long-term consequences of treatment. We demonstrated that treated monkeys experienced no thrombocytopenia and only 1 in 4 displayed a transient period of neutropenia, whereas all irradiated controls experienced an intense phase of neutropenia (5-12 days) and thrombocytopenia (5-31 days). The most striking effect was a 2-wave platelet (PLT) response in treated animals, which peaked at day (D) 8 and D22 after TBI. Humeral BM–derived total clonogenic activity proved to be significantly spared at 24 hours and 4 days after TBI in treated monkeys. No apparent decrease in stem cell reserve was observed one year after radiation.
Materials and methods
Animals
Adult male cynomolgus monkeys (Macaca fascicularis) weighing 7 ± 2kg were housed at the CRSSA (Centre de Recherches du Service de Santé des Armées)–accredited animal facility in individual cages in holding rooms equipped with a reverse-filtered air barrier (10 air changes per hour 100% fresh air) and full-spectrum light (8:00 am to 8:00 pm) and conditioned to 23°C with a relative humidity of 60%. Animals were fed with commercial primate chow supplemented with fresh fruit and were provided with tap water ad libitum. Housing and experiments were approved by the French Army Ethics Committee in accordance with European rules and regulations. Biologic samples collection and animal management were carried out under general anesthesia with ketamine (Imalgene, Myrial, Lyon, France; 10 mg/kg intramuscular).
Irradiation
Anesthetized monkeys (N = 9) placed in a restraining chair were exposed to a global unilateral front irradiation with a 60Co gamma source at a total midline tissue dose of 5 Gy (measured in air at the anterior iliac crest level) with a dose rate of 20 cGy/minute. Dosimetry was performed using 0.3-cm3 ionizing chambers and thermoluminescent aluminum oxide dosimeters.
Cytokines
Recombinant human (rh) SCF, rhFL, and rhIL-3 (R&D Systems, Abingdon, United Kingdom) were used. Pegylated recombinant human MGDF (Peg-rHuMGDF) was kindly supplied by Kirin Breweries Co, Ltd (Tokyo, Japan).
Study design
Eight monkeys were irradiated at day 0 (D0) and randomly assigned to either control group (n = 4) or 4F-treated group (n = 4). Two hours (h) after TBI, the animals received single, 5-mL intravenous injections of either 4F (50 μg/kg of each cytokine) or saline diluent. The dose and the schedule of single administration were based on a previous mouse study18 and other works dealing with the evaluation of Peg-rHuMGDF17 or pegylated recombinant murine MGDF alone.22 Both short-term and long-term hematopoietic recovery was then studied.
In addition to the main study design, the PLT response to a second MGDF injection was evaluated in 4F-treated animals one year after TBI. Furthermore, 2 other animals were enrolled to study the multiple cytokine pharmacokinetic pattern in steady-state conditions. One of them (Z 966) was irradiated after a 3-month washout period and given a second 4F injection 2 hours after TBI in order to compare the pharmacokinetics before and after irradiation.
Clinical support
Animals were transfused with fresh whole blood irradiated with a 20-Gy dose (60Co gamma irradiation) when the platelet count was less than 20 × 109/L or the hematocrit less than 20%. An antimicrobial regimen (ampicillin 50 mg/kg/d and gentamycin 1.5 mg/kg/d) was provided during the neutropenia period (neutrophil [ANC] count < 0.5 × 109/L).
Pharmacokinetic analysis
The pharmacokinetics of SCF, FL, Peg-rHuMGDF, and IL-3 were determined in normal (n = 2) and irradiated (n = 5) animals after intravenous bolus (50 μg/kg of each cytokine). Concentrations in plasma were measured using procedures (R&D Systems) by ELISA (enzyme-linked immunosorbent assay). The ELISA used murine antihuman cytokine monoclonal antibodies (Abs) and anti-TPO Abs cross react with Peg-rHuMGDF. Detection thresholds were 9 pg/mL (SCF), 7 pg/mL (FL), 15 pg/mL (TPO), and 7.4 pg/mL (IL-3). The following parameters were determined: elimination half-life (expressed in hours [h]), plasmatic clearance (mL/h/kg), initial volume of central compartment Vc and volume of distribution during elimination phase Vd (ng/mL), mean area under the plasma concentration-time curves (AUC in μg/mL/h) using the PK Solutions 2.0 Software (SRS, Montrose, CO).
Evaluation of neutralizing anti-MGDF Abs
We looked for anti-MGDF Abs in the plasma of all treated animals by ELISA using Nunc MaxiSorp plates (Dutscher, Brumath, France) coated with MGDF (10 μg/mL in phosphate-buffered saline [PBS]) as capture antigen and alkaline phosphatase–conjugated antihuman immunoglobulin G (IgG) or IgM mouse Ab (Sigma, Saint Quentin Fallavier, France) as a revelation reagent.
Hematopoietic evaluations
Peripheral blood. Peripheral blood (PB) was obtained from the saphenous vein to assay complete blood and differential cell counts (Pentra 120 analyzer; ABX, Montpellier, France; and May-Grünwald Giemsa stain, Sigma). CD34+ cells were quantified in the blood by flow cytometry (XL analyzer; Beckmann Coulter, Villepinte, France) using a monoclonal Ab anti-CD34 (clone 563; BD Biosciences, Le Pont de Claix, France). Short-term recovery was defined as the time for ANC count to reach 0.5 × 109/L and the PLT count to reach 20 × 109/L. The duration of anemia was defined as the time when hemoglobin (Hb) level was lower than 100 g/L (10 g/dL). Mid- and long-term reconstitution was estimated from the AUC of the white blood cell (WBC), ANC, lymphocyte (LY), PLT, and red blood cell (RBC) counts from D0 to D90 and D0 to D450 after TBI, respectively, based on trapezoid area calculations.
Bone marrow. Approximately 5 mL of heparinized-BM was aspirated from the humerus and posterior iliac crest of anesthetized monkeys before TBI and then at 6 hours, 24 hours, 4 days, 42 days, and 450 days after TBI. These BM areas were chosen to evaluate the dose distribution heterogeneity related to unilateral front TBI. Indeed, humeral level represents BM sites that were overexposed to radiation compared with posterior iliac crest (PIC). Low-density (1.070 g/cm3) mononuclear cells (MNCs) were separated and cultured for colony-forming units (CFUs; granulocyte macrophage CFUs [CFU-GMs], erythroid burst-forming units [BFU-Es], granulocyte-erythrocyte-megakaryocyte-macrophage CFUs [CFU-GEMMs], megakaryocyte CFUs [CFU-MKs]) evaluation in a methylcellulose short-term culture (RTM-Mabio, Tourcoing, France). Colonies were scored at day 14 and expressed in CFUs for 1 × 105 MNCs plated.
Long-term culture–initiating cells (LTC-ICs) were assessed 450 days after TBI. LTC-ICs were developed by seeding humeral BM MNCs onto irradiated (20 Gy) preformed murine MS-5 stromal cells that were cultured as a feeder layer. CD34+ cell percentage was determined on MNCs as described for PB samples. The following MNC dilutions containing 5, 50, 500, and 5000 CD34+ cells per well of 96-well microplates (32 replicates per dilution step) were tested. After 5 weeks, methylcellulose medium was added in each well to perform clonogenic assays as described in the previous paragraph. A well was scored positive for LTC-ICs if at least one colony was identified. To evaluate the stem cell reservoir, we quantified the BM side population (SP) cells, which have been reported to represent a rare population of very immature stem cells.23 SP cells have been defined by their capacity to efflux Hoechst 33342 dye, which can be mostly inhibited by the addition of Verapamil. SP cells can be characterized using flow cytometry as Hoechst 33342low cells. BM cells were depleted of erythrocytes by hypotonic lysis. After 2 washes in PBS (Gibco Life Technologies, Cergy Pontoise, France), cells were resuspended in prewarmed Hoechst staining solution, with or without Verapamil (100 μM/L; Sigma) at 1 × 106 cells/mL. Hoechst staining was conducted in Iscove modified Dulbecco medium (Gibco) supplemented with 2% fetal calf serum (FCS), 10 mM/L HEPES (4-(2-Hydroxyethyl)-1-piperazineethanesulfonic acid), and 5 μg/mL Hoechst 33342 (Sigma) at 37°C for 2 hours. Hoechst dye was excited at 351 nm by UV laser. Its fluorescence was detected at 2 wavelengths using 424/44 (Hoechst blue) and 630/22 (Hoechst red) band pass filters. Dead cells were excluded based on propidium iodide staining (5 μg/mL; Sigma). Cytometric analysis was performed on FACS Vantage SE (BD Biosciences). To determine SP cells percentage, acquisition was run on 1 × 106 cells. BM was collected from 5 untreated unirradiated animals in order to assess baseline SP values.
Evaluation of inflammatory markers
RI inflammatory reaction was evaluated by measuring C-reactive protein (CRP), fibrinogen, haptoglobin, orosomucoid, transferrin, and apolipoproteins A1 and B (Hitachi 704 analyzer; Roche Diagnostics, Meylan, France) before irradiation at D1, D4, D6, D8, D15, D20, D30 after TBI and then once a month up to D450.
Statistical analysis
Results are expressed as means ± SD. The nonparametric Mann and Whitney U test was used to test the significance between the 2 groups regarding major parameters at each experimental time. The Wilcoxon matched pairs test was used for clonogenicity gradient study. Poisson statistics for the single-hit model were applied to determine the frequency of LTC-ICs. The latter parameter was calculated by using the maximum likelihood estimator.24
Results
Biologic response of 5-Gy gamma irradiated animals
Five-gray gamma unilateral TBI mainly induces a hematopoietic syndrome. Owing to the clinical support provided (ie, antibiotics and blood transfusion), this irradiation dose constitutes a high sublethal dose that is compatible with long-term follow-up. Monkeys exhibited a transient phase of reduced food intake without obvious signs of gastrointestinal damage (eg, absence of diarrhea). Necropsies carried out on historic 5-Gy–irradiated animals revealed no meaningful abnormalities, in particular no extensive focuses of fibrosis. Biochemical parameters evaluation accounted for a transient, moderate RI inflammatory process in both groups. Thus, CRP increased early (on average 98 ± 38 mg/L at D1) and returned to the baseline value (2.24 ± 1.7 mg/L) by D4. It was not followed by a fibrinogen level increase. The 4F administration did not augment the inflammatory response. All biochemical parameters under evaluation stayed within a normal range throughout the duration of this 450-day study. In particular, no biologic impairment of liver or kidney function was detected in either group.
In irradiated monkeys, a single 4F administration stimulates PB cell recovery and BM hematopoietic activity
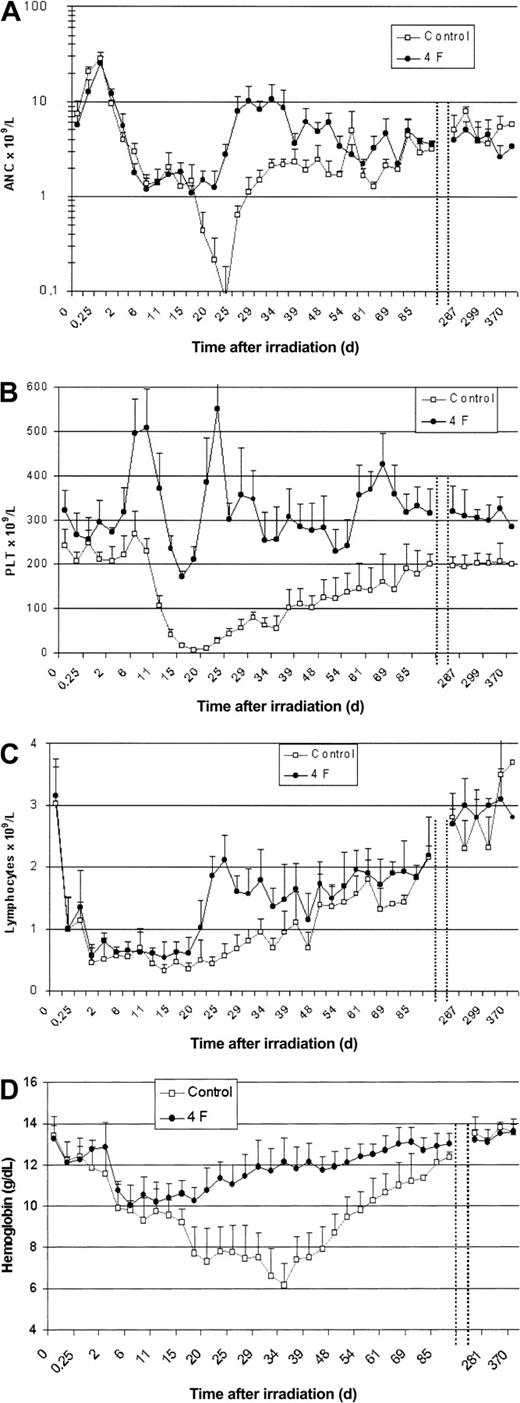
Neutrophil recovery. Three of 4 treated monkeys exhibited no period of leukopenia or neutropenia (Figure 1A). However, all control animals showed a phase of neutropenia (ANC count < 0.5 × 109/L, 9 ± 2.5 days) with an average time to baseline neutrophil recovery of 68 ± 30 days as shown in Table 1. The AUC analysis of leukocyte and neutrophil cell counts from D0 to D90 shows a significantly improved reconstitution in the 4F group in comparison with the control group (Table 2). No significant difference in long-term reconstitution was observed.
Irradiated animals and 4F administration. Effect of 4F administration on (A) neutrophils (ANC), (B) platelets (PLT), (C) lymphocytes, and (D) hemoglobin in 5 Gy total body 60Co gamma irradiated animals. Animals were given a single intravenous injection of 4F combination (50 μg/kg of each cytokine, n = 4) or saline diluent (n = 4). The data represent mean values ± SD. For better visualization, values of hematologic parameters are not represented from D90 to D260.
Irradiated animals and 4F administration. Effect of 4F administration on (A) neutrophils (ANC), (B) platelets (PLT), (C) lymphocytes, and (D) hemoglobin in 5 Gy total body 60Co gamma irradiated animals. Animals were given a single intravenous injection of 4F combination (50 μg/kg of each cytokine, n = 4) or saline diluent (n = 4). The data represent mean values ± SD. For better visualization, values of hematologic parameters are not represented from D90 to D260.
Platelet recovery. Only animals in the control group exhibited a prolonged phase of thrombocytopenia (PLT < 20 × 109/L, 13.2 ± 10.5 days; PLT < 50 × 109/L, 23.5 ± 20 days) with an average time to baseline PLT recovery of 85 ±20 days. However, the thrombocyte count increased after all animals in the treated group received a 4F injection. The count peaked twice at D8 and D22 (Figure 1B). The AUC analysis of the PLT count from D0 to D90 shows significantly improved reconstitution in the 4F group in comparison to the controls. As for long-term reconstitution, no significant difference was observed between groups.
Lymphocyte recovery. The 4F animals exhibited a significantly shorter period of lymphopenia (Figure 1C) than controls (P = .04). However, according to the LY AUC analysis from D0 to D90, no difference in lymphocyte recovery was observed between groups.
RBC production and transfusion requirements. A very short period of anemia was observed in treated animals (6.2 ± 6 days) allowing for blood transfusion independence (Figure 1D). However, the control monkeys exhibited a prolonged period of anemia (45.2 ± 13.6 days) and received around 1 to 3 blood units. The AUC analysis of RBC counts and Hb levels showed a significantly improved short-term recovery in the treated group (P < .05 for both parameters); no significant difference in long-term recovery was observed between groups.
PB CD34+cell evaluation. The statistical analysis showed significantly higher CD34+ cell peak values in treated animals (P = .02) than in control animals (Table 3). The increased circulation of immature cells accounts for the greater recovery level in the 4F group. Moreover, this recovery occurred much sooner in these animals (P = .02).
Bone marrow–derived CD34+cells and clonogenic activity. Results of clonogenicity are presented in Tables 4 and 5 for the humeral and PIC BM, respectively. At the humeral level, the clonogenic activity (CFU-GM + BFU-E + CFU-GEMM) was tremendously reduced in control animals the first few days after TBI (1 ± 1.1 CFU and 1 ± 1.4 CFU at D1 and D3/D4, or 0.4% of baseline value). In the treated group, the reduction of HSPC cell death and subsequent stimulation after 4F injection accounted for significantly higher clonogenic activity in humeral BM versus controls (P = .02) at D1 and D3/D4 (12.3 ± 7 CFU and 36 ± 12 CFU, or 7.5% and 22% of the baseline values, respectively). At D42, proliferation increased in humeral and PIC BM of controls but progenitor cell counts did not reach a steady-state value until 15 months. By contrast, treated animals recovered more efficiently. For example, regarding PIC BM, treated monkeys displayed higher clonogenicity at D42 (CFU-GM were significantly higher: 34.3 ± 11 colonies versus 13.3 ± 3.9 in controls, or 36.9% of the baseline versus 5%; P = .02). No exhaustion of clonogenic cells was observed after 15 months in either group. In particular, treated animals exhibited an augmentation of committed progenitors: CFU-GMs, BFU-Es, and CFU-MKs. From the baseline values of 73 ± 27 colonies, CFU-MKs reached 61 ± 18 at D42 and 134 ± 75 at D450. As for controls, CFU-MKs reached similar values at D450 (128 ± 55 colonies).
When comparing matched humeral and PIC BM activities, a gradient of clonogenicity was observed in favor of PIC in control animals at D1 and D3/D4 (P < .02). Intriguingly, a reversed gradient was assessed from D42 to D450 (P = .03). No gradient was observed in treated animals at any time.
CFU-GEMMs (Table 4) and LTC-ICs (Table 6) that were evaluated at 450 days after TBI from humeral BM showed no apparent impairment of the stem cell pool in either irradiated group. Thus, 4F animals displayed 0.8 ± 0.28 LTC-ICs for 1 × 105 MNCs versus 1.42 ± 0.49 LTC-ICs for 1 × 105 MNCs in irradiated controls; in comparison, LTC-IC number ranged from 0.52 to 3.94 LTC-ICs for 1 × 105 MNCs in untreated unirradiated animals. In the latter, the LTC-IC frequency (relative to CD34+ cells) ranged from 1:2040 to 1:480. No significant differences in LTC-IC frequency or number was seen between treated and control groups.
Humeral BM SP cells (number for 1 × 105 MNCs; Table 7) were evaluated in 4F animals (89.3 ± 49.5; n = 4) 15 months after TBI in comparison with irradiated (137 ± 54; n = 4) and unirradiated (85.3 ± 50.2; n = 5) controls. At this time, no significant difference in SP cell number was observed between these 3 groups.
Pharmacokinetics of SCF, FL, MGDF, and IL-3 administered in combination to normal and irradiated animals
Plasma levels of all cytokines injected were measured over 24 hours after intravenous injection in unirradiated (n = 2) and irradiated monkeys (n = 5) as shown in Table 8. In all animals Peg-rHuMGDF was the cytokine to reach the highest plasma concentrations. Plasma concentrations at 24 hours for SCF, FL, and MGDF (Table 7) were higher than baseline values (SCF, 0.6 ng/mL; FL, 0.1 ng/mL; MGDF, < detection threshold on average), showing a sustained exposure of the organism to these cytokines.
Response to a second administration of Peg-MGDF
Given that Peg-rHuMGDF has been reported to be potentially immunogenic, we looked for the possible production of neutralizing anti-MGDF antibodies after 4F administration and we also evaluated PLT response and possible immunogenicity after a second MGDF injection, administered 1 year after irradiation (in 3 animals of the 4F group: N318, P423 and K811). No Ab was detected after either the multiple cytokine injection or the second MGDF injection. Compared with respective baseline PLT counts, 4F and MGDF induced PLT peaks corresponding to the following respective increases: 31% and 173% [N318]; 50% and 121% [P423]; 98% and 212% [K811]. After the peak induced by the second MGDF injection, PLT counts returned to normal and remained stable over the 6 months afterward.
Moreover, the animal Z966 was enrolled to compare 4F pharmacokinetic parameters before and after irradiation. This monkey received a first 4F injection in steady-state conditions, was irradiated 3 months later, and received a second 4F injection 2 hours after TBI. In this animal, we detected anti-MGDF Ab after the second dose (titers of 1:20 at D10 and 1:80 at D20) accompanied by severe thrombocytopenia.
Discussion
Here, we examined the capacity of a combination of 4 antiapoptotic cytokines (4F) administered as an early and single injection into sublethally irradiated monkeys to promote multilineage hematopoietic recovery. This work was based on a mouse study showing the ability of 4F (each cytokine given at 50 μg/kg) to rescue lethally irradiated mice (8 Gy gamma) from hematopoietic death.18 It was also based on other mouse studies that evaluated the hematopoietic effects of a single injection of TPO15,16 or Peg-rHuMGDF17 after irradiation. We have also brought forth evidence in nonhuman primate models showing that 4F effectiveness is related to early protection from RI apoptosis at the HSPC level both in vitro20 and in vivo.18
In monkeys, we observed that there was a clear benefit in terms of short-term hematologic recovery. The period of neutropenia and thrombopenia was abrogated in treated animals. The most striking effect was focused on thrombopoiesis as characterized by 2 PLT waves centered on D8 and D22 after TBI, emerging from a sustained thrombopoietic activity. Accordingly, PLT counts always remained above 1.2 × 109/L in treated monkeys, as assessed by significantly augmented D0 to D90 AUC for PLTs. The day-8 wave would be related to the intrinsic megakaryopoietic activity of MGDF, in combination with the 3 other cytokines; as to the day-22 wave, 4F could strengthen the latent potential of residual megakaryoblats. This could be in accordance with the abortive rise in blood cells observed in victims irradiated at doses from 2 to 4 Gy.25 This kind of 2-wave increase in PLT count was not observed in mice exposed to carboplatin26 or in 5-Gy–irradiated monkeys27 given PEG-rHuMGDF or TPO alone, respectively; in the latter 2 cases however, treatment was administered at D1 as a single dose26 or from D1 as a prolonged treatment.27 The 4F combination abrogated neutropenia in 3 animals, which is consistent with Neelis et al's study on 6-Gy irradiated mice.15 Granulopoiesis was stimulated in particular between D20 and D40 in all treated monkeys versus controls, and D0 to D90 AUC for WBCs and polymorphonuclear leukocytes (PMNs) were significantly augmented in the 4F group. In monkeys given a single dose of TPO 24 hours after 5-Gy TBI,28 the subsequent administration of G-CSF or GM-CSF from D1 to D14, was necessary to improve neutrophil recovery. In addition, an early lymphocyte count recovery was observed in the 4F group between D20 and D40, which could be the consequence of the protection of intrathymic or BM lymphoid progenitors and/or of the peripheral expansion of mature lymphocytes amplified by 4F. Indeed, SCF and FL have been reported to synergize in vitro with IL-7 for lymphocyte expansion.29 RBC recovery quickly improved as seen by D0 to D90's AUC. This accounts for transfusion independence, which is consistent with erythroid progenitor stimulation induced by TPO30 and confirms Neelis et al's studies.15,27,28 Finally, the earlier and higher increase in PB CD34+ cell count in the 4F group relative to controls is also an indication of greater hematopoietic activity.31
The benefit observed at the PB cell level stems from the early preservation of BM clonogenic activity. In our early single 4F treatment we showed that in treated animals there were detectable BM CFU levels at D1 in the humerus and PIC that appeared to have increased at D3/D4, whereas CFU values were depressed in the humerus of controls at these times. In our model of unilateral radiation exposure, physical dosimetry demonstrates the existence of a gradient of absorbed dose, that is an attenuation of 50%, between entrance (thorax) and exit (back; ie, CIP) sides of gamma ray flow. In accordance with that, the comparison of matched humeral and PIC clonogenic activities reveals a “gradient of clonogenic activity” in BM territories of control animals at day 1 and D3/D4 in favor of PIC. Intriguingly, a reversed gradient was observed in controls in favor of the humerus at D42 that persisted at day 450. In fact, the depleted humeral hematopoietic niches may have been recolonized from underexposed areas in control animals through a process involving an increased cytokine production from stromal environment.32 As for treated animals, no gradient of clonogenic activity was detected whatever the time. This apparent homogeneous recovery could be related to 4F stimulation of ubiquitous radioresistant progenitor cells.4 Moreover, bystander and abscopal effects33 based on the cross-talk between initially damaged cells and other cells, involving soluble factor release and protein exfoliation on shed vesicles,34 which leads to the extension of damage to distant tissues, could be implicated in the slower BM recovery in controls compared with treated animals.
As for possible mid-term and long-term side effects, exhaustion of the stem cell reservoir after HGF administration is still under discussion. In fact, published data suggests possible exhaustion in the case of prolonged G-CSF or GM-CSF administration35-37 after multiple doses of cytotoxic agents were used. In our study, a single injection of cytokines was chosen in order to reduce putative side effects, including stem cell impairment. The BM clonogenic activity and the stem cell pool were evaluated 15 months after treatment. BM clonogenicity was not impaired (including CFU-MK) in either group when compared with baseline values. LTC-ICs and SP cells could be quantified in both irradiated groups within respective normal ranges. Furthermore MGDF readministration one year after TBI in 3 animals resulted in high levels of PLT production 8 days later on average. This reflects good megakaryopoiesis functionality. While we cannot exclude an effect on stem cell reserve, our results with a single 4F treatment are consistent with a lack of effect on the stem cell reservoir.
Peg-rHuMGDF safety is currently being debated since an adverse immunogenic effect has been reported. Cases of persistent thrombocytopenia were reported in patients who received multiple doses of Peg-rHuMGDF.38 This toxicity was due to the production of autoAbs to MGDF that cross-reacted with and neutralized endogenous TPO.13 However, the same authors published that no production of anti-TPO Abs was observed in 46 healthy apheresis donors given a single subcutaneous injection of Peg-rHUMGDF in order to collect PLTs.39 Here, we reported the safety of a single administration of Peg-rHuMGDF combined with 3 other cytokines in myelosuppressed monkeys, as evidenced over a 15-month follow-up. Moreover, 4F-treated animals did not develop an immunogenic response with a second MGDF administration performed after stable hematopoietic recovery. In fact, only one monkey produced neutralizing Abs leading to severe thrombocytopenia; this animal had previously been sensitized to MGDF as a nonmyeloablated subject. TPO/MGDF molecules should be optimized owing to the development of derived thrombopoietic factors deprived of antigenic activity such as pegylated peptide TPO receptor agonist40 or nonpeptidyl receptor agonist.
Based on the pharmacokinetic study, effective plasma concentrations could be sustained up to 15 hours for each cytokine after a single intravenous administration of 4F. This is compatible with the aim to mitigate the early RI apoptotic process. If one considers the plasma levels reached, one can wonder what further benefit a second 4F injection 24 hours after TBI would offer. However one cannot rule out that a 2-injection treatment would be beneficial toward higher doses of radiation.
In conclusion, different growth factor combinations have been reported to be effective in reducing the duration of cytopenia following irradiation.41 The present monkey study shows that a single 4F administration is effective in managing a 5-Gy gamma radiation dose that is close to the lethal dose 50% per 60 days for humans and nonhuman primates, according to the literature.42 Regarding prolonged stem cell stress that would result from protracted exposure or combined internal contamination, further investigation should address the relevance of the emergency antiapoptotic cytokine therapy. Moreover, whether the 4F combination could reduce HSPC apoptosis and rescue monkeys after exposure to higher radiation doses remains to be determined. Indeed, a severe inflammatory process would develop in more deeply irradiated monkeys as documented after 7- to 10-Gy TBI (F.H. and M.D., unpublished observations, April 2003) by a prolonged increase of CRP (up to 250 mg/L) and fibrinogen (up to 6.5 g/L) plasma levels. As this led to a multiorgan failure syndrome, multiple cytokine treatments should be optimized to also mitigate extrahematologic toxicity. This mitigation could result from direct effects on stromal cells and tissue-restricted stem cells or might involve mobilization of pluripotent stem cells that would home to damaged tissues under attraction by specific local factors. This strategy would be in accordance with the multiple tissue distribution of grafted mesenchymal stem cells observed by Thierry et al43 in irradiated monkeys 3 months after TBI. This would also be consistent with the myocardial regeneration observed after cytokine treatment in animal models of myocardial infarction.44 In severely irradiated victims a sequential cytokine treatment consisting of antiapoptotic factors followed by colony-stimulating factors could be proposed. The emergency multiple cytokine regimen presented here could also be applied as part of cell therapy treatment.
Prepublished online as Blood First Edition Paper, October 2, 2003; DOI 10.1182/blood-2003-05-1400.
Supported by a grant from EDF (Electricité de France).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are grateful to Dr H. Miyazaki from Kirin Breweries Co Ltd for kindly providing Peg-rHuMGDF. We thank H. Chaussard, M. Fonteneau, D. Bois, D. Coulon, and D. Maitre for their technical assistance in animal care.