The inability to undergo apoptosis is a crucial mechanism of multidrug resistance in acute myeloid leukemia (AML), and the analysis of mitochondrial apoptotic proteins may represent a significant prognostic tool to predict outcome. Bcl-2 and Bax oncoproteins were evaluated in 255 de novo AML patients (pts) by flow cytometry using an anti–bcl-2 monoclonal antibody (MoAb) and an anti-bax MoAb. The results were expressed as an index (bax/bcl-2) obtained by dividing bax mean fluorescence intensity (MFI) and bcl-2 MFI. Lower bax/bcl-2 ratio was associated with French-American-British (FAB) M0-M1 classes (P = .000 01) and CD34 more than 20% (P < .000 01). There were striking inverse correlations between CD34 or CD117 MFI and bax/bcl-2 values (r = −.40, P < .000 001 andr = −.29, P = .000 002), confirming that immaturity is consistent with this index. Moreover, lower bax/bcl-2 levels were correlated with poor-risk cytogenetics (P = .0002). A significant higher complete remission (CR) rate was found in pts with higher bax/bcl-2 levels (79% versus 45%; P = .000 01). Also, both a longer overall survival (OS) and disease-free survival (DFS) were observed in pts with higher bax/bcl-2 levels (P = .000 01 and = .019). Noteworthy, bax/bcl-2 levels accurately predicted the clinical response and outcome of pts with normal or unknown cytogenetics. Indeed, within this subset of 147 pts, higher bax/bcl-2 ratio was significantly associated both with a higher CR rate (86% versus 42%;P < .000 01) and a longer OS (P = .0016). The independent prognostic value of bax/bcl-2 ratio was confirmed in multivariate analysis. Therefore, mitochondrial oncoproteins, such as bcl-2 and bax, represent both sensitive indicators of clinical outcome and potential targets of novel proapoptotic molecules in order to circumvent chemoresistance.
Introduction
The primary cause of treatment failures in acute myeloid leukemia (AML) is the emergence of multidrug resistance.1-3 Common mechanisms of resistant disease are defects in apoptotic pathways. Apoptosis is ultimately executed by caspases that operate both through the receptor-mediated pathway containing members of the tumor necrosis factor (TNF) family of death receptors4,5 and the mitochondrial-mediated pathway involving cytochrome c release from the mitochondria.6,7Defects in the receptor- or mitochondrial-mediated pathway may give important prognostic information in AML, allowing risk stratification of the patients (pts). The mitochondrial-mediated pathway of apoptosis is regulated by the bcl-2 family of antiapoptotic (bcl-2, bcl-xl, mcl-1) and proapoptotic proteins (bax, bad, and bak), and bcl-2 inhibits apoptosis by interacting and forming inactivating heterodimers with bax/bak.8 Overexpression of bcl-2 has been associated with drug resistance in hematologic malignancies,9,10 whereas a high bax level was found to be a good prognostic indicator in AML.11 It has been suggested that the bax/bcl-2 ratio may be more important than either promoter alone in determining apoptosis.12 However, conventional techniques, such as immunocytochemistry and Western blot, cannot provide reliable quantitative information and are inadequate for calculating the bax/bcl-2 ratio.11 Flow cytometry may be particularly well suited both for the precise, semiquantitative measurement of bcl-2 and bax oncoprotein expression and for the estimation of cellular heterogeneity that is frequently found in AML.9 11 In fact, the binding of the anti–bcl-2 or bax monoclonal antibody (MoAb) to leukemic cells is variable, which makes it difficult to define 2 groups, one positive and one negative. On the basis of these observations, we investigated the presence of bcl-2 and bax proteins within a large series of 255 newly diagnosed AML cases, using the mean fluorescence intensities rather than the percentages. Therefore, in our study, the use of a more sensitive, quantitative flow cytometric method allowed us to assess the strong and independent clinical significance of bax/bcl-2 ratio.
Materials and methods
Immunophenotyping
Double-color immunofluorescence analysis of surface antigens was performed by using combinations of phycoerythrin (PE) and fluorescein isothiocyanate (FITC) conjugate MoAbs, as previously described.15 Results were obtained by gating the appropriate “blast gate” using side scatter (SSC) versus forward light scatter (FSC) and examining the associated FITC and PE expression. We used MoAbs against CD33 (My9-PE), CD13 (My7-PE), CD14 (My4-PE) obtained from Beckman Coulter (Hialeah, FL) and MoAbs anti-CD15 (LeuM1-FITC), anti-CD34 (HPCA-2 PE), anti-CD117 (CD117 PE), anti-CD2 (Leu5b-FITC), anti-CD7 (Leu9-FITC), anti-CD3 (Leu4-FITC), anti-CD10 (Calla-FITC), anti-CD19 (Leu12-FITC), anti–HLA-DR (HLA-DR PE), anti-CD61 (CD61-FITC), all purchased from Becton Dickinson (Mountain View, CA). Mononuclear cell fractions were separated from heparinized BM samples by Ficoll-Hypaque gradient centrifugation (Sigma, St Louis, MO). All samples contained at least 80% of blasts. Cells (1 × 107/mL) were incubated at 4°C for 30 minutes with the MoAbs at saturation concentrations and washed twice with phosphate-buffered saline (PBS). Analysis was carried out on an Epics XL flow cytometer (Beckman Coulter). The positivity was expressed as a percentage with cutoff 20% over the corresponding isotypic control.
CD34 and CD117 expressions were also evaluated in 221 pts as mean fluorescence intensities (MFIs), calculated as the ratio of CD34 or CD117 MoAb mean/negative control mean. Both CD34 percentages and MFI values were determined on the blast cells identified using FSC/SSC gating.
Intracytoplasmic and nuclear stains on cytospin preparations included terminal deoxynucleotidyl transferase; cytoplasmic CD3 (cCD3), CD22 (cCD22), and CD13 (cCD13), as well as and myeloperoxidase (MPO), as previously described.15 Immunofluorescence was evaluated by optical examination using a Zeiss microscope equipped with an epifluorescence set, a barrier filter set for blue fluorescence, and a ×100 phase contrast objective (Zeiss, Göttingen, Germany).
Cytogenetic analysis
Karyotype analysis was performed on aspirated BM cells by using standard G-banding techniques to stain metaphase preparations obtained from unstimulated cultures, as previously described.16Chromosome abnormalities were analyzed separately and according to prognostic groups, using a modification of the Chicago classification in which a normal karyotype, t(8;21), abnormal (16) were considered intermediate/favorable (int/fav) risk category, whereas complex patterns, hyperploid or polyploid karyotypes, numerical or structural deletions of chromosome 5 or 7, trisomy 8, t(9;22), 11q23 rearrangements, and other chromosome abnormalities were pooled together as poor-risk category.17 A successful karyotype analysis was obtained in 187 presentation samples.
Bcl-2 and bax expression
Bcl-2 and bax oncoproteins were evaluated by flow cytometry using the following 2 MoAbs: (1) Anti–human bcl-2 clone 124 FITC-conjugated MoAb (Dako, Glostrup, Denmark) is an immunoglobulin G1 (IgG1) that reacts specifically with bcl-2 oncoprotein associated with mitochondria, smooth endoplasmic reticulum, and perinuclear membrane18; (2) anti-bax clone Ab-2 (Oncogene, Cambridge, MA) is an IgG1 that recognizes bax, normally localized to the cytoplasm, but translocating rapidly to the mitochondria after the induction of an apoptotic signal.19 For multiparameter analysis of bcl-2 and bax combined with myeloid antigens, mononuclear cells were first incubated with CD13 and/or CD33 PE-conjugated MoAbs for 30 minutes at 4°C. Subsequently the cells, washed twice in PBS, were fixed and permeabilized in 2 steps: first in 3.5% paraphormaldeyde/PBS and then in 50% cold acetone/PBS. All samples were then incubated at 4°C for 30 minutes with either 10 μL anti–bcl-2 FITC or 20 μL unconjugated anti-bax. For bax, cells were further incubated at 4°C for 30 minutes with 100 μL FITC-conjugated F(ab)2 fragment of goat antimouse immunoglobulin (dilution 1:50; Dako, Glostrup, Denmark). Negative controls were performed by incubating cells with nonspecific isotype IgG1 antibodies. In 52 pts with AML T-residual lymphocytes identified by CD3 PE-conjugate MoAb and treated with bcl-2 and bax MoAbs were used as another negative control. KG-1 and HL-60 cell lines were used as positive controls for this study. Analysis was carried out by flow cytometry (Epics XL; Coulter). The results were obtained by gating blast cells by using SSC versus FSC and examining bcl-2 and bax expressions on CD13/CD33+ blast cells (Figure 1).
Flow cytometric histograms of bcl-2 and bax expressions on 3 AML samples.
AML cases were analyzed by flow cytometry after exposure to anti-CD33 PE and anti–bcl-2 FITC or bax MoAbs, as described. (A) Bivariate histogram FSC/SSC with “blast gate” on leukemic cells and IgG1 isotype-negative controls for bcl-2 (B) or bax (C) and CD33 MoAbs from “blast gate.” Bcl-2 (Di, Ei, Fi) and bax (Gi, Hi, Ii) were evaluated on the CD33+ cells segregated by “AML cells” gate in 3 AML cases. Bcl-2 (Dii, Eii, Fii) or bax (Gii, Hii, Iii) univariate histograms, conditioned on “AML cells” gate, show the distribution of fluorescence, reported as arithmetic means (M).
Flow cytometric histograms of bcl-2 and bax expressions on 3 AML samples.
AML cases were analyzed by flow cytometry after exposure to anti-CD33 PE and anti–bcl-2 FITC or bax MoAbs, as described. (A) Bivariate histogram FSC/SSC with “blast gate” on leukemic cells and IgG1 isotype-negative controls for bcl-2 (B) or bax (C) and CD33 MoAbs from “blast gate.” Bcl-2 (Di, Ei, Fi) and bax (Gi, Hi, Ii) were evaluated on the CD33+ cells segregated by “AML cells” gate in 3 AML cases. Bcl-2 (Dii, Eii, Fii) or bax (Gii, Hii, Iii) univariate histograms, conditioned on “AML cells” gate, show the distribution of fluorescence, reported as arithmetic means (M).
Bcl-2 and bax proteins were evaluated as relative mean fluorescence intensities (MFIs), calculated as the ratio of bcl-2 or bax MoAbs mean/negative control mean. The results were expressed as an index (bax/bcl-2), obtained by dividing MFI bax and MFI bcl-2. The threshold was set at the bax/bcl-2 median value higher than 0.3 (range, 0.01-6.0), taking into account BM immature progenitors from healthy donors as negative controls and reference cell lines (KG-1 and HL-60) as positive controls. We tried to set empirically various cutoff points for bax/bcl-2 index, and the selected threshold was sufficient to severely affect complete response and survival, identifying accurately pts at poor prognosis. Moreover, we applied a discriminant function analysis based on the squared Mahalanobis distances of each case from its group centroids (bax/bcl-2). The correct percentage (observed classification versus predicted classification) was more than 80% for this variable.
Statistical analysis
The relationships of bax/bcl-2 values to age or karyotype were assessed by Mann-Whitney test. Correlations between bax/bcl-2 index and FAB classification or white blood cell (WBC) counts or CD34 percentages or the complete remission (CR) rate were based on chi-square or 2-tailed Fisher exact test. Overall survival (OS), disease-free survival (DFS), and relapse-free survival curves were plotted according to the Kaplan-Meier method. Survival was measured from the date of diagnosis to the date of death or last follow-up. DFS was calculated from the date of CR until relapse. All the pts who underwent autologous or allogeneic transplantation were censored at the time of BM or peripheral blood stem cell (PBSC) infusion. For comparison of OS or DFS patterns of 2 or more groups, the log-rank test was applied. The variables for which univariate analysis had shown a significant association were studied in multivariate analysis. A logistic regression model was used to assess the independent effect of covariables, treated as dichotomous, on the CR, whereas Cox proportional hazards regression model was used to evaluate OS and DFS.
Results
Patients
Approval for this study was obtained from the institutional review board. Informed consent was provided according to the Declaration of Helsinki. Criteria for inclusion in this study were (1) diagnosis of AML other than acute promyelocytic leukemia (APL), because pts with APL were entered into a different protocol; and (2) eligibility for intensive chemotherapy. We studied 255 newly diagnosed AML cases, admitted at our unit, between 1995 and 2001, as shown in Table1.
The pts had a median age of 63 years (range, 18-80 years) with a performance status of 2 or less (World Health Organization [WHO] grading system). The population studied included 116 pts aged younger than 60 and 139 pts older than 60. The first group was treated according to the European Organization of Research and Treatment of Cancer and Gruppo Italiano Malattie Ematologiche Maligne dell'Adulto (EORTC/GIMEMA) AML-10 and AML-12 randomized trials, based, as induction scheme, on the triple association of cytarabine, etoposide, and an anthracycline (daunorubicin or idarubicin or mitoxantrone). Pts with an HLA-compatible sibling were allografted whenever eligible, whereas the others were randomly assigned to receive peripheral or BM stem cell transplantation.20 21 Pts older than 60 were entered into the EORTC/GIMEMA AML-13 randomized trial. These pts received mitoxantrone, etoposide, and cytarabine as induction therapy. On achievement of CR, pts were randomly assigned to receive either an intravenous (idarubicin, etoposide, and cytarabine) or an oral (idarubicin, etoposide, and subcutaneously administered cytarabine) consolidation program. Fifty-one patients were transplanted (40 patients with an autologous transplant and 11 patients with an allogeneic transplant) and censored at the time of BM or PBSC infusion.
Characteristics of bax/bcl-2 ratio in AML
The MFI of staining with anti–bcl-2 FITC MoAb (18.9 ± 17.3) and anti-bax MoAb (5.6 ± 6.7) in AMLs shifted between CD34+ cell means of normal BM (12.2 ± 11.5 and 4.4 ± 3.2, respectively) and HL-60 cell line means (24.6 ± 8.2 and 6.8 ± 3.1, respectively). Higher bcl-2 MFI median values were found within FAB M0-M1-M6 subgroups, whereas higher bax MFI median values characterized FAB M2-M4-M5 pts, as shown in Table2.
The CD34+ small percentages (1%-5%) of immature progenitors in 50 BM specimens from healthy donors were used as a control group for bax/bcl-2 index: in all cases, bax/bcl-2 ratio values, obtained by flow cytometry, were always higher than 0.3 (range, 0.5-8.5). The CD3+ T lymphocytes within 52 AML samples showed also bax/bcl-2 ratio values higher than 0.3 (range, 0.4-6.1). With this cutoff point, 51% (130 of 255) of the pts, showing bax/bcl-2 ratio less than 0.3, were considered as positive. No relevant association was found between bax/bcl-2 ratio and age (Table3). Lower than 0.3 bax/bcl-2 index was significantly associated both with the immature FAB M0-M1 subtypes (P = .000 01, Table 4), higher than 100 × 109/L white blood cell (WBC) count (P = .01, Table 4) and CD34 more than 20% (P < .000 01, Table 4). Moreover, lower bax/bcl-2 ratio levels were significantly related to poor risk cytogenetics (P = .0002, Table 3). There were also highly significant inverse correlations between bax/bcl-2 ratio values and CD34 MFI (r = −.40, P < .000 001) or CD117 MFI (r = −.29, P = .000 002), confirming that this index is consistent with a stem cell-like feature in AML.
Prognostic value of bax/bcl-2 index
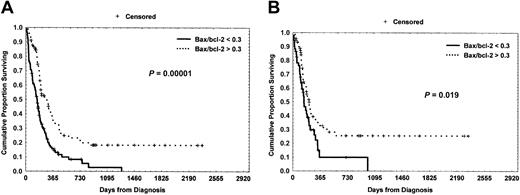
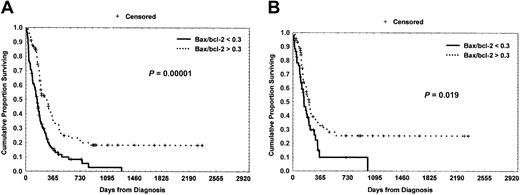
A significant higher complete remission (CR) rate was found in pts with higher bax/bcl-2 index (79% versus 45%;P = .000 01, Table 1). Also, both a longer overall survival (OS) and disease-free survival (DFS) were observed in pts with higher bax/bcl-2 index (18% [confidence interval (CI), 10-38] versus 0% at 4 years; P = .000 01 and 26% [CI, 14-45] versus 0% at 4 years; P = .019, Figure 2A-B).
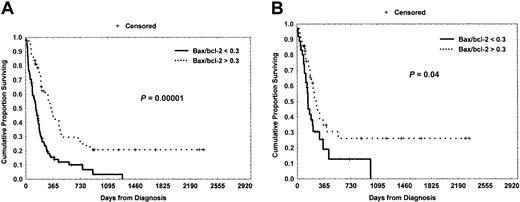
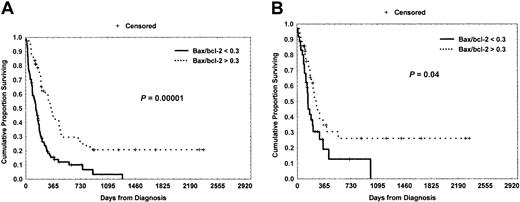
However, there was no significant difference between CD34+(> 20%) and CD34− (< 20%) pts with regard to CR (P = .06), OS (P = .4), and DFS (P = .8). However, lower bax/bcl-2 ratio was capable of clearly identifying pts at poorer prognosis within the CD34+ subgroup (n = 150 pts; 42% versus 81%,P = .000 03 for CR; 3% versus 21% at 3 years,P = .000 01 for OS, Figure3A and 0% versus 26% at 3 years,P = .04 for DFS, Figure 3B).
Overall survival (OS) and disease-free survival (DFS) curves based on bax/bcl-2 ratio levels.
(A) Kaplan-Meier plot comparing survival based on the detection of more than 0.3 bax/bcl-2 ratio or less than 0.3 bax/bcl-2 ratio. More than 0.3 bax/bcl-2 pts experienced a significantly longer OS (P = .000 01). (B) AML pts with bax/bcl-2 ratio more than 0.3 showed a significant longer DFS as compared with pts with lower than 0.3 (P = .019).
Overall survival (OS) and disease-free survival (DFS) curves based on bax/bcl-2 ratio levels.
(A) Kaplan-Meier plot comparing survival based on the detection of more than 0.3 bax/bcl-2 ratio or less than 0.3 bax/bcl-2 ratio. More than 0.3 bax/bcl-2 pts experienced a significantly longer OS (P = .000 01). (B) AML pts with bax/bcl-2 ratio more than 0.3 showed a significant longer DFS as compared with pts with lower than 0.3 (P = .019).
Overall survival (OS) and disease-free survival (DFS) curves based on bax/bcl-2 ratio within the CD34+ subset.
Lower than 0.3 bax/bcl-2 ratio retained its striking poor prognostic effect with regard to OS (A) (P = .000 01) and DFS (B) (P = .04).
Overall survival (OS) and disease-free survival (DFS) curves based on bax/bcl-2 ratio within the CD34+ subset.
Lower than 0.3 bax/bcl-2 ratio retained its striking poor prognostic effect with regard to OS (A) (P = .000 01) and DFS (B) (P = .04).
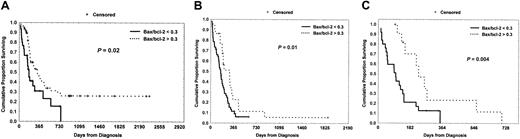
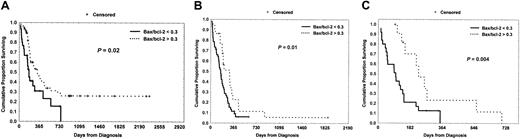
Interestingly, lower bax/bcl-2 ratio retained its adverse prognostic significance both within int/fav cytogenetics subgroup (n = 94 pts; 70% versus 94%, P = .002 for CR and 0% versus 26% at 2 years, P = .02 for OS, Figure4A) and poor cytogenetics class (n = 93 pts; 11% versus 23% at 1 year, P = .01 for OS, Figure4B, and 21% versus 70% at 6 months, P = .004 for DFS, Figure 4C).
Overall survival (OS) and disease-free survival (DFS) curves based on bax/bcl-2 ratio levels within the int/fav and poor-risk cytogenetics subgroups.
(A) The significant difference between less than 0.3 and more than 0.3 bax/bcl-2 ratios was maintained within the int/fav cytogenetics class with regard to overall survival (P = .02). Within the poor-risk cytogenetics category, pts with lower bax/bcl-2 ratio levels showed a less favorable outcome than those with higher bax/bcl-2 levels with regard to OS (B) (P = .01) and DFS (C) (P = .004).
Overall survival (OS) and disease-free survival (DFS) curves based on bax/bcl-2 ratio levels within the int/fav and poor-risk cytogenetics subgroups.
(A) The significant difference between less than 0.3 and more than 0.3 bax/bcl-2 ratios was maintained within the int/fav cytogenetics class with regard to overall survival (P = .02). Within the poor-risk cytogenetics category, pts with lower bax/bcl-2 ratio levels showed a less favorable outcome than those with higher bax/bcl-2 levels with regard to OS (B) (P = .01) and DFS (C) (P = .004).
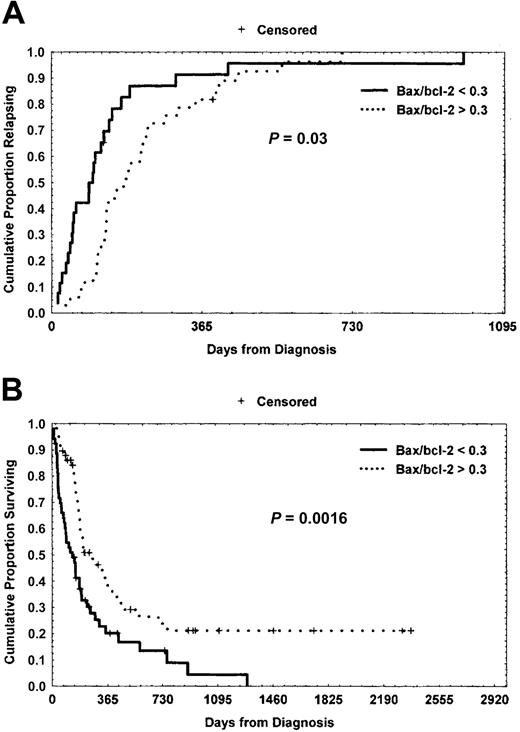
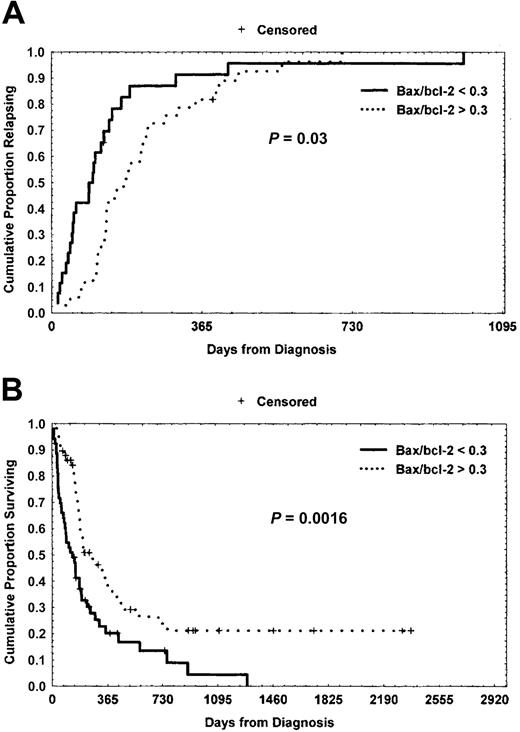
Furthermore, lower bax/bcl-2 ratio was closely associated with a shorter time to relapse (4 ± 3.6 months versus 7 ± 6.3 months;P = .03, Figure 5A). Noteworthy, bax/bcl-2 levels accurately predicted the clinical response and outcome of pts with normal (79 of 255) or unknown cytogenetics (68 of 255). Indeed, within this subset of 147 pts, higher bax/bcl-2 ratio was significantly associated both with a higher CR rate (86% versus 42%; P < .000 01) and a longer OS (21% versus 0% at 4 years; P = .0016, Figure 5B).
Relapse-free survival (RFS) and overall survival (OS) curves within normal/unknown cytogenetics subset based on bax/bcl-2 ratio levels.
(A) Kaplan-Meier plot comparing bax/bcl-2 ratio values with relapse-free survival. The difference between bax/bcl-2 ratio less than 0.3 group and bax/bcl-2 ratio more than 0.3 group was statistically significant (P = .03). (B) With regard to OS, the significant difference between less than 0.3 bax/bcl-2 ratio and more than 0.3 bax/bcl-2 ratio cases was maintained within the normal/unknown cytogenetics subset (P = .0016).
Relapse-free survival (RFS) and overall survival (OS) curves within normal/unknown cytogenetics subset based on bax/bcl-2 ratio levels.
(A) Kaplan-Meier plot comparing bax/bcl-2 ratio values with relapse-free survival. The difference between bax/bcl-2 ratio less than 0.3 group and bax/bcl-2 ratio more than 0.3 group was statistically significant (P = .03). (B) With regard to OS, the significant difference between less than 0.3 bax/bcl-2 ratio and more than 0.3 bax/bcl-2 ratio cases was maintained within the normal/unknown cytogenetics subset (P = .0016).
In a logistic multivariate regression analysis of CR, bax/bcl-2 ratio was confirmed in being a significant independent prognostic factor (odds ratio, 3.3; CI, 1.3-8.4; P = .013). Finally, using a multivariate Cox regression analysis both of OS and DFS, bax/bcl-2 mortality hazard ratios were 8.7 for OS (P = .003) and 5.5 for DFS (P = .019), respectively (Tables 5 and 6).
Discussion
Lower bax/bcl-2 ratio is consistent with immaturity and a worse cytogenetic pattern in AML
The biologic basis of drug resistance and relapse in AML is not well understood, and prognoses are still largely based on descriptive parameters. Several lines of evidence indicate that apoptosis plays a role in response to chemotherapy, suggesting an association between therapy-induced apoptosis and therapeutic efficacy in AML.22 Increasing evidence suggests that specific genetic alterations may abrogate apoptotic responses in myeloid tumorigenesis. High bcl-2 or low bax protein expression may contribute to leukemogenesis and drug resistance.9,23 The mechanisms linking these molecules to drug resistance have been experimentally addressed in AML by Banker et al.24 In this study, most AML samples showed less treatment-associated apoptosis, suggesting that apoptotic responses to the therapeutic agents may be attenuated. All AML samples with the highest bcl-2–positive fractions showed low apoptosis. Moreover, the relative expression of proapoptotic and antiapoptotic proteins25 has been shown to provide an indication of chemosensitivity in solid tumors.26 We hypothesized that bcl-2 measured in conjunction with bax would provide valuable information on the intrinsic chemosensitivity of AML, as reflected by the clinical response to treatment. Besides, among the polypeptides that are structurally and functionally related to bcl-2, Mcl-1 has been identified. The Mcl-1 gene encodes a 36-kD polypeptide with a carboxyl terminal domain that is 35% identical to bcl-2.27 Overexpression studies have revealed that Mcl-1 delays apoptosis induced by etoposide in myeloid leukemia cells28 and exhibits high levels at the time of leukemic relapse in AML.29 The antiapoptotic effects of bcl-2 and Mcl-1 are opposed by a number of proapoptotic bcl-2 family members, such as bax and bak. As it is well known, bcl-2 and Mcl-1 have the ability to form heterodimers with Bax, a 22-kD polypeptide, neutralizing its effect. This results in a diminished ability of the cell to undergo apoptosis.25 It has been demonstrated that, in chronic lymphocytic leukemia (CLL) cells, the conformational changes of bax and bak are among the early steps in the induction of cell death.30 Besides, after dimethyl sulfoxide (DMSO) treatment, HL-60 cells died via apoptosis, and the levels of the apoptosis effector proteins bak and bad were enhanced, whereas there was a slight down-regulation of the apoptosis suppressor protein bcl-2.31 Moreover, in myelodysplastic syndromes, a higher expression of proapoptotic proteins, such as bak, bad, and bcl-xs, was associated with a longer survival and a decreased risk of leukemic transformation.32 Our present study performed in a large series of patients identifies a distinct AML subset (130 pts), expressing lower than 0.3 bax/bcl-2 ratio, characterized by immaturity (higher CD34 and CD117 levels) and by a poor karyotype. The use of a quantitative flow cytometric method based both on bcl-2 and bax mean fluorescence intensities and their ratio allowed us to precisely define its biologic and clinical potentiality. In fact, the quantitation of fluorescence intensity seems technically adequate and useful for a more correct evaluation of clinical and prognostic correlations, as previously demonstrated.33Moreover, Ong et al11 observed that immunocytochemical techniques were both inadequate for calculating the bax/bcl-2 ratio and unable to find any significant correlation between this ratio and outcome parameters. All our AML cases were found to be bcl-2 positive, probably because of a more sensitive technical approach by direct immunofluorescence, as observed also by other researchers.10 Concerning the FAB classification, our data demonstrated significantly higher bax/bcl-2 ratio values in monocytic AMLs (M4 and M5), because of a lower bcl-2 MFI. This finding is in contrast to the report of Campos et al9 who found a significantly higher percentage of bcl-2–positive cells in these FAB subtypes. However, our results confirm other observations of higher bcl-2 expression in more immature cells34 and in immature AMLs.10,35 The prognostic value of bax/bcl-2 ratio may be also due to a correlation of bcl-2 with maturation. In fact, this ratio was found to be low in our CD34+ AML cases (P < .000 01), as observed by others.35,36 Besides, CD34 MFI values were significantly correlated with bax/bcl-2 ratio (r = −.40,P < .000 001). Moreover, a significant correlation was found between higher bcl-2 expression (MFI > 14) and coexpression of the CD34 antigen, further suggesting that the higher bcl-2 expression is more evident in less differentiated AMLs.10 These findings could contribute to the prognostic relevance of bax/bcl-2 ratio, because CD34+ AMLs are considered to have an unfavorable outcome.35,37 On the contrary, despite the strict correlation between CD34 expression and bax/bcl-2 ratio, in our experience CD34 alone did not show any clinical significance with regard to CR, OS, and DFS in univariate analysis. In addition, the strong inverse correlation between bax/bcl-2 ratio and MFI CD117 values (P = .000 002) in our cases confirms the link between this index and maturation pathways, because CD117 is expressed by myeloid precursor cells38 and its activation prevents apoptosis.39 Besides, a lower bax/bcl-2 ratio was able to identify clearly pts at unfavorable prognosis within the CD34+ subset (Figure 3), demonstrating that its strong independent prognostic value is bound not only to immaturity but also probably to a disregulation of the apoptotic pathways. Furthermore, bax/bcl-2 ratio was found to be expressed at lower levels in our poor-risk cytogenetics AML subset (P = .0002), as corroborated also by other studies.35,40 From literature, it is well known that chromosomal translocations associated with specific subtypes of acute leukemia result in the rearrangement of a variety of transcription factor genes. These resulting hybrid genes encode chimeric or aberrantly expressed proteins that may contribute to malignant transformation via the suppression of apoptosis. Banker et al24 observed that some karyotypic abnormalities, such as t(15;17), del(7), and t(9;11), exhibited lower basal apoptosis in AML. On the contrary, other researchers10 11 showed that the bcl-2 expression (bcl-2 mRNA, bcl-2/bax ratio, or bcl-2 MFI) did not correlate to prognostic groups defined by karyotype.
Clinical significance of bax/bcl-2 ratio
From a clinical point of view, higher bax/bcl-2 ratio was significantly correlated with a higher CR rate (Table 1), longer time to relapse (Figure 5A), and a longer OS and DFS (Figure 2A-B). Accordingly, Campos et al9 demonstrated that AML pts with high levels of bcl-2 expression by immunofluorescent staining had a CR rate of 29% versus an 85% CR rate in pts with low levels. Likewise, high levels of bcl-2 translated into decreased OS. Bcl-2 remained an important predictor of survival in multivariate analysis over other known prognostic markers, including age and WBC count of more than 30. Besides, increased levels of bax expression by immunocytochemical analysis correlated with improved rates of OS in a study of 56 pts with de novo AML.11 On the contrary, a study of 165 pts with newly diagnosed AML41 reported that levels of bax expression by immunoblotting did not correlate with response to induction chemotherapy or survival. However, in the same study, high ratios of bcl-2 to bax protein conferred a poor prognosis with decreased rates of CR and OS. Moreover, there was a significant correlation between bcl-2-to-bax expression ratio and clinical response (P < .005) in 14 AML pts examined by using an immunophosphatase staining method.12 Along these lines, it has been demonstrated that the ratio of bcl-2 to bax correlates inversely with the sensitivity of B-cell chronic lymphocytic leukemia (B-CLL) cells to cytotoxic drugs in vitro.42 Therefore, the prognostic discrimination offered by the ratio of the proteins is greater than the bcl-2 levels alone. Also in our hands, the use of a more sensitive, quantitative method, eg, quantitative flow cytometry, allowed us to realize the clinical prognostic potential value of this ratio, as demonstrated by our clinical results. Moreover, lower bax/bcl-2 ratio retained its unfavorable prognostic value both within int/fav and poor cytogenetic classes with regard to CR, OS, and DFS (Figure 4). In myelodysplastic syndromes (MDSs) and AML secondary to MDS, bax/bcl-2 ratio was inversely correlated with both the International Prognostic Scoring System (IPI) score and cytogenetics: the highest levels were observed in pts with low IPI score and/or good risk cytogenetics.43 Andreeff et al44 reported an unexpectedly poor survival rate associated with low bcl-2 in a group of AML pts with unfavorable cytogenetics. These preliminary data were confirmed by Kornblau et al41 who demonstrated that AML pts with a lower bcl-2/bax ratio had an inferior response rate to induction therapy (35% versus 78%, P = .0006) and an inferior survival outcome (median survival, 11 versus 53 weeks,P = .000 02). On the contrary, we found that a low bax/bcl-2 ratio predicted a poor outcome also within the unfavorable cytogenetic class. The explanation for this discrepancy may be in the particular karyotypic abnormalities, such as del(7), complex karyotypes, and 11q23 translocations, notoriously inhibiting apoptosis24 45 and very frequently found in our poor-risk cytogenetics subgroup. Furthermore, we found that bax/bcl-2 ratio maintained its strong prognostic significance with regard to CR (P < .000 01) and OS (P = .0016) also within AML pts with normal or unknown cytogenetics. These data suggested that cytogenetics and bax/bcl-2 ratio were independent predictors of response and survival. In multivariate analysis a low bax/bcl-2 ratio confirmed its worse significant effect on the outcomes.
In conclusion, this biologic ratio is feasible and reliable through flow cytometric methods46 and is a potentially useful prognostic indicator for tailoring the intensity of treatment. Its striking prognostic effect confirms the key role of mitochondrial apoptotic proteins, such as bcl-2 and bax, both in chemosensitivity and in future strategies for overcoming multidrug resistance in AML.
Prepublished online as Blood First Edition Paper, November 7, 2002; DOI 10.1182/blood-2002- 06-1714.
Supported in part by MURST, Programmi di ricerca di interesse nazionale 2000.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Giovanni Del Poeta, Cattedra e Divisione Ematologia, Università “Tor Vergata,” Ospedale S. Eugenio, P. le Umanesimo, 10, 00144 Roma, Italy; e-mail:g.delpoeta@tin.it.