Key Points
ΔdblGATA mice are resistant to EAE but not due to their lack of eosinophils.
GATA1 regulates numbers of HSPCs in the BM, and the ΔdblGATA mutation causes a functional deficit during inflammation.
Abstract
GATA-binding factor 1 (GATA1) is a transcription factor that governs the development and function of multiple hematopoietic cell lineages. GATA1 is expressed in hematopoietic stem and progenitor cells (HSPCs) and is essential for erythroid lineage commitment; however, whether it plays a role in hematopoietic stem cell (HSC) biology and the development of myeloid cells, and what that role might be, remains unclear. We initially set out to test the role of eosinophils in experimental autoimmune encephalomyelitis (EAE), a model of central nervous system autoimmunity, using mice lacking a double GATA-site (ΔdblGATA), which lacks eosinophils due to the deletion of the dblGATA enhancer to Gata1, which alters its expression. ΔdblGATA mice were resistant to EAE, but not because of a lack of eosinophils, suggesting that these mice have an additional defect. ΔdblGATA mice with EAE had fewer inflammatory myeloid cells than the control mice, suggesting that resistance to EAE is caused by a defect in myeloid cells. Naïve ΔdblGATA mice also showed reduced frequency of CD11b+ myeloid cells in the blood, indicating a defect in myeloid cell production. Examination of HSPCs revealed fewer HSCs and myeloid cell progenitors in the ΔdblGATA bone marrow (BM), and competitive BM chimera experiments showed a reduced capacity of the ΔdblGATA BM to reconstitute immune cells, suggesting that reduced numbers of ΔdblGATA HSPCs cause a functional deficit during inflammation. Taken together, our data show that GATA1 regulates the number of HSPCs and that reduced GATA1 expression due to dblGATA deletion results in a diminished immune response following the inflammatory challenge.
Introduction
GATA-binding factor 1 (GATA1) is a transcription factor that governs the development and function of multiple hematopoietic cell lineages.1 GATA1 was initially implicated in the development of erythroid lineage cells,2,3 but was later found to have functions in eosinophils, mast cells, basophils, conventional dendritic cells (DCs), and monocytes.1,4,5 It has been reported that GATA1 is expressed in hematopoietic stem and progenitor cells (HSPCs),6-8 where it drives erythroid lineage commitment while repressing myeloid lineage commitment.8,9 However, it has also been reported that a mutation in GATA1, which affects its binding to chromatin, reduces the expression of myeloid lineage genes among Lin−CD117+ HSPCs,6 suggesting that GATA1 also promotes the development of myeloid cells. Indeed, GATA1 expression in early hematopoietic progenitors correlates with myeloid lineage gene signatures,10 further supporting the possibility that GATA1 participates in the commitment of early progenitors to the myeloid lineage.
Gata1 expression is regulated by enhancers that direct its cell type–specific expression, including the double GATA-site (dblGATA) enhancer.11 Mice lacking dblGATA (ΔdblGATA) lack eosinophils and have been extensively used to study their role in disease models.12-15 Later, it was discovered that ΔdblGATA mice also have a mild defect in basophils,16 but no additional defects have been described in these mice. However, using a Gata1 bacterial artificial chromosome reporter mouse, it was demonstrated that GATA1 is expressed in Lin−CD117+ hematopoietic progenitors and that the ΔdblGATA mutation reduced GATA1 expression in these cells, but no functional deficit was reported.7 Overall, the function of GATA1 in hematopoietic progenitors and its influence on the immune system remains poorly understood.
We initially used ΔdblGATA mice to test the role of eosinophils in experimental autoimmune encephalomyelitis (EAE) and found that these mice had notably reduced susceptibility to EAE. However, subsequent experiments demonstrated that EAE resistance could not be attributed to the lack of eosinophils, indicating that ΔdblGATA mice have an additional defect. This was surprising, given that the dblGATA enhancer has long been thought to almost exclusively regulate eosinophil development. Further studies revealed that ΔdblGATA mice had fewer infiltrating myeloid cells in the central nervous system (CNS) and peripheral blood during EAE, suggesting that the dblGATA enhancer regulates myeloid cells. Examination of the bone marrow (BM) revealed that ΔdblGATA mice had reduced numbers of hematopoietic stem cells (HSCs) and myeloid lineage progenitors, suggesting that GATA1 regulates their numbers. These data suggest that GATA1 increases immune cell production in the BM by maintaining HSPCs and that reduced GATA1 expression in BM progenitors results in an immune deficit during inflammation.
Materials and methods
Mice
ΔdblGATA (C.129S1(B6)-Gata1tm6Sho/J) mice on a Balb/cJ background and wild-type (WT) Balb/cJ and C57BL/6J mice were obtained from The Jackson Laboratory, whereas PHIL (B6.Cg-Tg(Epo-DTA)#Nal/JleeJ) and NJ.1638 (B6.Cg-Tg(Cd3d-Il5)NJ.1638Nal/JleeJ) mice were obtained from James Lee of Mayo Clinic.
Flow cytometry
The cells were stimulated with phorbol myristate acetate (500 ng/mL; Sigma-Aldrich), ionomycin (50 ng/mL; Sigma-Aldrich), 1 μL/mL BD GolgiPlug (BD Biosciences), and monensin (1 μL/mL, BD Biosciences) for 4 hours at 37°C. Cells were washed, and cell surface antigens were stained for 20 to 30 minutes at 4°C. The cells were washed and fixed with 100 μL of FIX and PERM Cell Fixation & Cell Permeabilization Kit Medium A (Thermo Fisher Scientific) for 20 minutes at room temperature and washed again with fluorescence-activated cell sorting buffer. The cells were permeabilized with FIX and PERM Cell Fixation & Cell Permeabilization Kit Medium B and stained with antibodies against intracellular antigens. The cells were washed twice and analyzed using a BD FACSAria Fusion Flow Cytometer (BD Biosciences). All the antibodies used are listed in supplemental Table 2.
Direct and adoptive EAE
Direct EAE in BALB/cJ mice was induced by immunization with complete Freund’s adjuvant emulsion containing 5 μg/mL heat-killed Mycobacterium tuberculosis (BD Biosciences) and 1 mg/mL PLP180-199 peptide (myelin proteolipid protein; Genscript) by subcutaneous injection of 100 μL of complete Freund’s adjuvant emulsion in each flank. The pertussis toxin was injected (IV administration) on days 0 and 2 after immunization (400 ng per dose). Mice were scored as described.17 For adoptive EAE, WT and ΔdblGATA mice were immunized as described above and euthanized on days 8 to 10 after immunization. Splenocytes were restimulated with 20 μg/mL PLP180-199 and 20 ng/mL murine recombinant interleukin 23 (IL-23) at a density of 5 × 107 cells per well in a 6-well tissue culture plate. After 3.5 days, CD4+ cells were purified using a negative selection magnetic microbead kit (Miltenyi Biotec), and 107 cells were transferred into either WT or ΔdblGATA recipients via tail vein injection in 200 μL of serum-free Iscove modified Dulbecco medium containing 0.2 μg of recombinant murine IL-2 (PeproTech). Adoptive EAE experiments using PHIL and NJ.1638 mice were performed as described,18 following the T helper 17 (Th17) polarization protocol. This study involves the use of mice. All procedures described here were approved by the Thomas Jefferson University Institutional Animal Care and Use Committee.
Eosinophil culture and adoptive transfer
Eosinophils were generated from BM cells as described.19 Cultures were used for experiments on days 14 to 16 after incubation with 10 ng/mL Recombinant Murine GM-CSF (PeproTech) for 24 hours. In addition, 2 × 107 eosinophils were transferred to the recipient EAE animals (IV administration) on days 7 and 9 after immunization for EAE induction.
BM-derived DC (BMDC) and monocyte culture
BM was isolated from the tibia and femurs of mice, and 106 cells per mL were cultured with granulocyte-macrophage colony-stimulating factor (GM-CSF) (50 ng/mL) ± IL-4 (50 ng/mL) for 5 days. On the fourth day, nonadherent cells were collected and replated with GM-CSF ± IL-4. To induce a mature DC phenotype, lipopolysaccharide (LPS) (300 ng/mL) was added for 72 hours. In DC to T cell coculture experiments, 4 × 104 DCs were cocultured with 1.6 × 105 DO11.10 CD4+ T cells and stimulated with OVA323-339 (ovalbumin; 100 ng/mL) peptide for 72 hours. For proliferation assays, the cells were stimulated with 20 μg/mL PLP180-199. After 60 hours, 1 μCurie of [3H]adenine (PerkinElmer) was added to each well. Cells were harvested 72 hours later, and counts per minute were measured in a MicroBeta2 beta counter (PerkinElmer). For monocyte cultures, monocytes were isolated from the BM using CD11b magnetic cell sorting beads (Miltenyi Biotec), followed by fluorescence-activated cell sorting for CD11b+Ly6C+Ly6Glo/− cells, and cultured as described above.
Isolation of immune cells from the CNS
The mice were anesthetized and perfused with 60-mL phosphate-buffered saline (PBS). The spinal cords were flushed from the spinal column with PBS. The brains and spinal cords were pooled and digested in Liberase TM Research Grade (in RPMI 1640 at 0.7 mg/mL; Roche) for 30 minutes at 37°C. The tissue was homogenized and passed through a 100-μm sterile filter, resuspended in 10 mL of 40% 1× Percoll-PBS (90% Percoll, 10% 10× PBS), and centrifuged at 2000 revolutions per minute with no brake at room temperature for 30 minutes. The supernatant was discarded, and the cell pellet was used for further experiments.
BM chimeras
Treosulfan was gifted to our laboratory by Medac GmbH (Germany). The BM was ablated by intraperitoneal injection of treosulfan dissolved in water. Three doses of treosulfan at 2000 mg/kg were administered over 3 consecutive days, and recipient mice were reconstituted with 8 × 106 BM cells (after red blood cell lysis) by tail IV injection. Mice were allowed to reconstitute for at least 8 weeks before use in the experiments.
Library preparation and RNA sequencing analyses
Sequencing libraries were prepared using the TruSeq Stranded Total RNA (Illumina) library preparation kit with high-quality RNA (RNA integrity number >8.7) and 200 ng input RNA. Libraries were assessed for quality using Labchip GX (PerkinElmer) and quantitative polymerase chain reaction (PCR) using the KAPA Library Quantification Kit and the Life Technologies Viia7 Real-Time PCR instrument. Libraries were diluted to 2 nM and sequenced in a paired-end (2 × 100 base pairs), dual-indexed format on HiSeq2500 (Illumina) using High Output V4 Chemistry. RNA sequencing reads were demultiplexed into sample-specific FASTQ files and aligned to the mm10 reference genome using the DRAGEN Genome Pipeline to produce BAM files. BAM files were read in R, and gene counts were obtained using the Rsubread package, producing a feature/gene count matrix. Differential expression analysis was performed using the R/Bioconductor package DESeq2.20 Analysis was performed using standard thresholds and parameters while filtering genes with low mean-normalized counts. Further downstream analysis was performed using the DAVID utility. Differentially expressed genes (P < .05) were entered into the DAVID utility and analyzed for gene ontology and KEGG pathway terms.21,22
Results
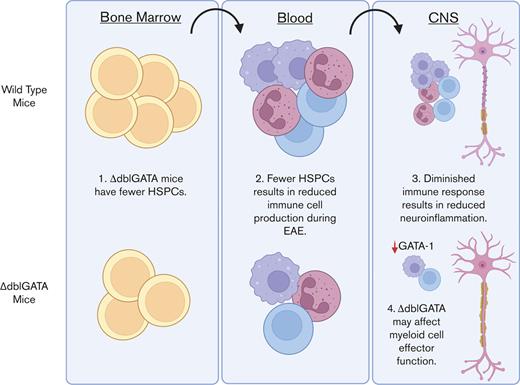
ΔdblGATA mice are resistant to EAE but not owing to the absence of eosinophils
To test whether eosinophils play a role in EAE, we compared WT and ΔdblGATA mice during direct EAE and found that ΔdblGATA mice developed milder clinical disease (Figure 1A-B) with reduced incidence and disease severity (Figure 1C-E). The ΔdblGATA mice had fewer immune cells infiltrating the spinal cords and less demyelination (Figure 1F-G). We also tested their susceptibility to adoptive EAE by transferring CD4+ T cells from PLP180-199–immunized donors to naïve WT and ΔdblGATA recipients. CD4+ T cells derived from either WT or ΔdblGATA donors induced disease in WT recipients, whereas ΔdblGATA recipients were completely resistant to EAE induction, regardless of the T-cell source (Figure 1H-I). These data indicate that the resistance of ΔdblGATA mice to EAE was not due to impaired priming of myelin-specific CD4+ T-cell responses.
ΔdblGATA mice are resistant to EAE. (A) WT and ΔdblGATA mice were immunized for EAE induction. Representative data showing the clinical course from 1 of >5 experiments. Significance was calculated using 2-way analysis of variance (ANOVA). (B) Change in body weight over time. Significance was calculated by comparing the means from each day. (C) Quantification of the maximum clinical score. (D) Weight loss relative to the starting weight on the day of immunization. Significance for maximum clinical score and weight loss were calculated using Student t test. (E) Disease incidence. Significance was calculated using χ2 test. N = 24 to 25 per group in panels C-E. (F) Luxol fast blue (LFB) and hematoxylin and eosin (H&E) staining for myelin in the spinal cord sections. (G) Quantification of inflammation, calculated as percent area of white matter occupied by cell infiltration. N = 2 to 3 per group. (H-I) Adoptive EAE in WT and ΔdblGATA mice. WT and ΔdblGATA mice were immunized with the PLP180-199 peptide, euthanized on day 8 after immunization, and splenic cells were stimulated with the peptide for 3 days in vitro. Then, 107 of purified CD4+ T cells from WT and ΔdblGATA mice were transferred to naïve WT and ΔdblGATA recipients. One of 2 independent repeats is shown. (H) Clinical score. (I) Change in body weight for panel H is shown. Statistical significance for panels H and I was calculated by 2-way ANOVA. Max., maximum.
ΔdblGATA mice are resistant to EAE. (A) WT and ΔdblGATA mice were immunized for EAE induction. Representative data showing the clinical course from 1 of >5 experiments. Significance was calculated using 2-way analysis of variance (ANOVA). (B) Change in body weight over time. Significance was calculated by comparing the means from each day. (C) Quantification of the maximum clinical score. (D) Weight loss relative to the starting weight on the day of immunization. Significance for maximum clinical score and weight loss were calculated using Student t test. (E) Disease incidence. Significance was calculated using χ2 test. N = 24 to 25 per group in panels C-E. (F) Luxol fast blue (LFB) and hematoxylin and eosin (H&E) staining for myelin in the spinal cord sections. (G) Quantification of inflammation, calculated as percent area of white matter occupied by cell infiltration. N = 2 to 3 per group. (H-I) Adoptive EAE in WT and ΔdblGATA mice. WT and ΔdblGATA mice were immunized with the PLP180-199 peptide, euthanized on day 8 after immunization, and splenic cells were stimulated with the peptide for 3 days in vitro. Then, 107 of purified CD4+ T cells from WT and ΔdblGATA mice were transferred to naïve WT and ΔdblGATA recipients. One of 2 independent repeats is shown. (H) Clinical score. (I) Change in body weight for panel H is shown. Statistical significance for panels H and I was calculated by 2-way ANOVA. Max., maximum.
To determine whether the lack of eosinophils causes EAE resistance in ΔdblGATA mice, we attempted to restore their susceptibility to direct EAE by the adoptive transfer of in vitro–generated eosinophils (Figure 2A).19 Eosinophil transfer did not affect EAE development or weight loss (Figure 2B-C), suggesting that eosinophil deficiency does not cause EAE resistance in ΔdblGATA mice. Further experiments with PHIL mice, which also lack eosinophils, but by a mechanism different from that of ΔdblGATA mice,23 yielded similar results, where PHIL and WT mice had similar EAE courses (Figure 2D) and immune cell compositions in the CNS (Figure 2E-G). Moreover, immune cells from the CNS of PHIL and WT mice had a similar capacity to proliferate when stimulated ex vivo with immunizing myelin peptide (Figure 2H). Finally, we tested whether eosinophils played a role in adoptive EAE. Primed myelin-specific CD4+ T cells were transferred to naïve WT, PHIL, NJ.1638, and NJ.1638/PHIL mice. NJ.1638 mice overexpress IL-5,24 resulting in hypereosinophilia,24 whereas NJ.1638/PHIL mice lack eosinophils but retain IL-5 overexpression. As in direct EAE, PHIL mice developed typical disease, whereas NJ.1638 mice developed an attenuated disease course compared with WT mice, but without difference compared with NJ.1638/PHIL mice (Figure 2I), showing that attenuated disease was due to IL-5 overexpression rather than a lack of eosinophils. Taken together, these data demonstrate that eosinophils do not play a significant role in EAE and that the lack of eosinophils is not the cause of EAE resistance in ΔdblGATA mice.
Eosinophils do not contribute to EAE. (A) Flow cytometry overlay of BM-derived eosinophil (Eos) cultures showing double-staining for Siglec-F and CCR3 (blue) and with isotype monoclonal antibodies (red). (B) Adoptive transfer of BM-derived eosinophils. WT and ΔdblGATA mice were immunized for EAE, and 2 × 107 eosinophils were injected IV on days 7 and 9 after immunization into ΔdblGATA mice. (C) Clinical scores and change in body weight are shown. Representative figures from 1 of 2 independent experiments. Significance was calculated by 2-way ANOVA (n = 4 for WT and ΔdblGATA groups; n = 6 for ΔdblGATA and eosinophil group). (D) Clinical course of EAE in WT C57BL6/J and PHIL mice (n = 5 per group). (E) Relative numbers of CD45+ cells isolated from the CNS (brains and spinal cords combined) of WT and PHIL mice. (F) Frequencies of CD11b+ and CD4+ cells within CD45+ cells from the CNS of WT and PHIL mice. (G) Frequencies of Th1 (interferon γ+ [IFN-γ+] IL-17A), Th17 (IL-17A+IFN-γ−), Th1/17 (IFN-γ+IL-17A+), regulatory T cell (Treg) (FoxP3+), and GM-CSF+ T helper cells from the CNS of WT and PHIL mice. (H) Proliferation assay. Mononuclear cells isolated from the CNS of WT and PHIL mice were stimulated for 18 hours with 25 μg/mL MOG35-55 (immunizing peptide) and 1 μCurie per well of [3H]adenine was added for additional 18 hours. Cells were then harvested, and counts per minute (C.P.M.) were measured using beta counter. (I) Clinical scores for adoptive EAE in WT, PHIL, 1638 (IL-5tg), and 1638/PHIL mice. Abs, antibodies; Freq., frequency.
Eosinophils do not contribute to EAE. (A) Flow cytometry overlay of BM-derived eosinophil (Eos) cultures showing double-staining for Siglec-F and CCR3 (blue) and with isotype monoclonal antibodies (red). (B) Adoptive transfer of BM-derived eosinophils. WT and ΔdblGATA mice were immunized for EAE, and 2 × 107 eosinophils were injected IV on days 7 and 9 after immunization into ΔdblGATA mice. (C) Clinical scores and change in body weight are shown. Representative figures from 1 of 2 independent experiments. Significance was calculated by 2-way ANOVA (n = 4 for WT and ΔdblGATA groups; n = 6 for ΔdblGATA and eosinophil group). (D) Clinical course of EAE in WT C57BL6/J and PHIL mice (n = 5 per group). (E) Relative numbers of CD45+ cells isolated from the CNS (brains and spinal cords combined) of WT and PHIL mice. (F) Frequencies of CD11b+ and CD4+ cells within CD45+ cells from the CNS of WT and PHIL mice. (G) Frequencies of Th1 (interferon γ+ [IFN-γ+] IL-17A), Th17 (IL-17A+IFN-γ−), Th1/17 (IFN-γ+IL-17A+), regulatory T cell (Treg) (FoxP3+), and GM-CSF+ T helper cells from the CNS of WT and PHIL mice. (H) Proliferation assay. Mononuclear cells isolated from the CNS of WT and PHIL mice were stimulated for 18 hours with 25 μg/mL MOG35-55 (immunizing peptide) and 1 μCurie per well of [3H]adenine was added for additional 18 hours. Cells were then harvested, and counts per minute (C.P.M.) were measured using beta counter. (I) Clinical scores for adoptive EAE in WT, PHIL, 1638 (IL-5tg), and 1638/PHIL mice. Abs, antibodies; Freq., frequency.
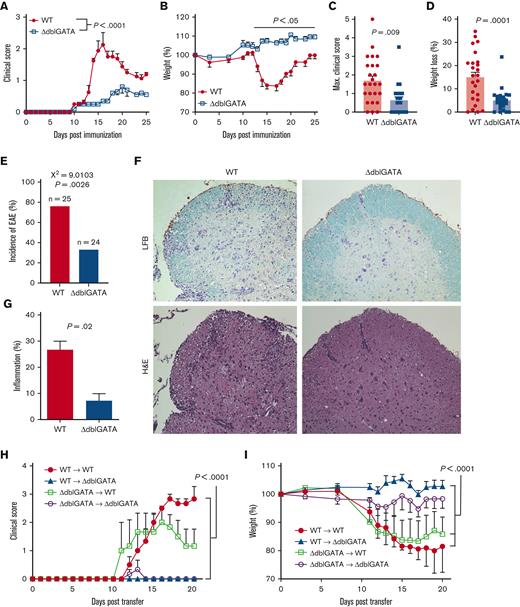
ΔdblGATA mice have reduced numbers of CNS-infiltrating myeloid cells during EAE
We next compared the CNS infiltrates of ΔdblGATA and WT mice during EAE and found fewer CD45+ cells in the CNS of ΔdblGATA mice (Figure 3A). The reduction was mostly due to smaller numbers of CD45hi immune cells from the periphery compared with CD45lo microglia (Figure 3B-C).25 Within the CD45hi population, ΔdblGATA mice exhibited lower frequencies of CD11b+Ly6Chi inflammatory monocytes and CD11b+CD11c+ DCs (Figure 3D). Clustering of flow cytometry data showed that ΔdblGATA mice had fewer MDCs, resulting in fewer cells expressing CD11c, MHC-II, CD80, and CD86 (Figure 3D-E). During EAE, multiple lineages of CCR2+Ly6Chi monocyte-derived cells are present in the CNS, including Arg1+ macrophages and a highly encephalitogenic subset of CXCL9+ monocytes.26 We found that among CCR2+Ly6Chi monocyte-derived cells, both Arg1+ and CXCL9+ subsets were virtually absent in the CNS of ΔdblGATA mice (Figure 3F-G), indicating that multiple monocyte subsets are affected. This coincided with a reduction in the frequencies of pro–IL-1β+ and TNF+ CCR2+Ly6Chi monocytes, and a small increase in IL-10+ monocytes (Figure 3G), suggesting that monocytes had a less proinflammatory phenotype in the CNS of ΔdblGATA mice. Given that IL-1β is critical for the induction of GM-CSF expression by CD4+ T cells,27 we characterized the phenotype of CD4+ T cells and found a reduced frequency of GM-CSF+ T cells in the CNS of ΔdblGATA mice, whereas Th1, Th17, and Treg cells did not differ from that of the WT controls (supplemental Figure 1A). Because GM-CSF is a powerful inducer of monocyte differentiation into MDCs,28 these data align well with our observation that the frequency of MDCs relative to that of monocytes (CD45hiCD11b+Ly6Glo/−Ly6ChiMHC-II−) was reduced in ΔdblGATA mice. Finally, a reduction in myeloid cell numbers in the CNS was concomitant with a reduction in CD11b+ cells among CD45+ peripheral blood mononuclear cells (PBMCs) (supplemental Figure 1B). These data show that ΔdblGATA mice have diminished neuroinflammation, which correlates with reduced myeloid cell numbers in the CNS and peripheral blood.
ΔdblGATA mice have reduced monocyte numbers during EAE. WT and ΔdblGATA mice were immunized for EAE induction. Ten mice per group were initially immunized, and 3 to 4 mice were pooled for each data point when the mice were euthanized on day 16 after immunization. Representative data from 4 experiments are shown. (A) Numbers of CD45+ cells isolated from the CNS (spinal cords and brains combined) of WT and ΔdblGATA mice with EAE. (B) Flow cytometry plots depicting CD45 expression vs side scatter, and quantification of CD45hi and CD45lo cells among the total cells isolated from the CNS. (C) Frequency of CD11b+CD11c+ and CD11b+Ly6Chi cells among the CD45+ cells. (D) t-distributed stochastic neighbor embedding (t-SNE) plots of CD45+ cells. Monocyte-derived DCs (MDCs) were defined as CD45hiCD11b+Ly6Glo/−CD11c+Ly6C+MHC-II+. Undifferentiated monocytes (Mo) were defined as CD45hiCD11b+Ly6Glo/−Ly6ChiMHC-II−. Microglia were defined as CD45loCD11b+. Neutrophils were defined as CD45+CD11b+Ly6G+Ly6Cintermediate. CD4+ cells were defined as CD45hiCD11b−CD4+. Other antigen-presenting cells (APCs) were defined as CD45hiCD11b+Ly6G−MHC-II−Ly6C−. The other CD45+ cells were CD45+CD11b−CD4−CD11c−. (E) Heatmap overlay of CD11c, MHC-II, CD80, and CD86 expression. (F) Flow cytometry plots showing CXCL9 and arginase 1 (Arg1) expression among CD45+Sall1−CD11b+CCR2+Ly6Chi monocytes. (G) Quantification of the frequency of CXCL9+, arginase1+, pro–IL-1β+, TNF+, and IL-10+ cells among CD45+Sall1−CD11b+CCR2+Ly6Chi monocytes. For panels F and G, n = 9 to 10 mice per group. Significance was determined by 2-tailed unpaired Student t test. Error bars are standard error of the mean (SEM). MHC-II, major histocompatibility complex II; TNF, tumor necrosis factor.
ΔdblGATA mice have reduced monocyte numbers during EAE. WT and ΔdblGATA mice were immunized for EAE induction. Ten mice per group were initially immunized, and 3 to 4 mice were pooled for each data point when the mice were euthanized on day 16 after immunization. Representative data from 4 experiments are shown. (A) Numbers of CD45+ cells isolated from the CNS (spinal cords and brains combined) of WT and ΔdblGATA mice with EAE. (B) Flow cytometry plots depicting CD45 expression vs side scatter, and quantification of CD45hi and CD45lo cells among the total cells isolated from the CNS. (C) Frequency of CD11b+CD11c+ and CD11b+Ly6Chi cells among the CD45+ cells. (D) t-distributed stochastic neighbor embedding (t-SNE) plots of CD45+ cells. Monocyte-derived DCs (MDCs) were defined as CD45hiCD11b+Ly6Glo/−CD11c+Ly6C+MHC-II+. Undifferentiated monocytes (Mo) were defined as CD45hiCD11b+Ly6Glo/−Ly6ChiMHC-II−. Microglia were defined as CD45loCD11b+. Neutrophils were defined as CD45+CD11b+Ly6G+Ly6Cintermediate. CD4+ cells were defined as CD45hiCD11b−CD4+. Other antigen-presenting cells (APCs) were defined as CD45hiCD11b+Ly6G−MHC-II−Ly6C−. The other CD45+ cells were CD45+CD11b−CD4−CD11c−. (E) Heatmap overlay of CD11c, MHC-II, CD80, and CD86 expression. (F) Flow cytometry plots showing CXCL9 and arginase 1 (Arg1) expression among CD45+Sall1−CD11b+CCR2+Ly6Chi monocytes. (G) Quantification of the frequency of CXCL9+, arginase1+, pro–IL-1β+, TNF+, and IL-10+ cells among CD45+Sall1−CD11b+CCR2+Ly6Chi monocytes. For panels F and G, n = 9 to 10 mice per group. Significance was determined by 2-tailed unpaired Student t test. Error bars are standard error of the mean (SEM). MHC-II, major histocompatibility complex II; TNF, tumor necrosis factor.
ΔdblGATA mice have impaired priming of myelin-specific T-cell responses in EAE
ΔdblGATA mice had fewer APCs in the CNS at the peak of clinical EAE, prompting us to compare APC function in ΔdblGATA and WT mice. We immunized mice with PLP180-199 peptide and characterized the immune response in the spleen, draining lymph nodes (dLNs), and CNS during the priming phase of EAE. There were fewer CD45+ cells in the dLN of ΔdblGATA mice, including CD11b+ myeloid cells, CD11b+CD11c+ DCs, CD11b+Ly6ChiLy6Glo/− monocytes, and CD4+ T cells (Figure 4A-B). We tested the magnitude of the antigen recall response by stimulating dLN cells with an immunizing peptide and found that cells from ΔdblGATA mice proliferated less, indicating impaired APC function (Figure 4C). Similarly, splenocytes of ΔdblGATA mice had decreased numbers of CD45+ cells and diminished responses to PLP180-199 compared with those of WT controls (Figure 4D-E). In the CNS of ΔdblGATA mice, we observed a decrease in the numbers of infiltrating CD45hi cells (Figure 4F), similar to that observed at the peak of the disease. The reduction in CD45+ cell numbers was primarily due to the loss of CD11b+ myeloid cells, particularly CD11b+CD11c+ DCs and Ly6ChiLy6Glo/− monocytes (Figure 4G). CD11b+CD11c+ DCs from ΔdblGATA mice showed a lower frequency of MHC-IIhi cells (Figure 4H-I) and lower MHC-II expression in CD11b+CD11c+MHC-II+ cells (Figure 4J-K), suggesting impaired APC function. CD80 and CD86 expression by CD11b+CD11c+ DCs of ΔdblGATA and WT mice was similar. These data showed that ΔdblGATA mice had reduced numbers of APCs and weaker myelin-specific T helper cell responses during the priming phase of EAE.
ΔdblGATA mice have defective priming in EAE. WT and ΔdblGATA mice were immunized for EAE induction and euthanized on day 8 after immunization (n = 4-5 per group; 2 independent experiments). (A-C) Analysis of inguinal dLN cells are shown in panels A-C. (A) Total number of CD45+ cells per mouse in inguinal dLNs. (B) Number of CD45+CD11b+, CD45+CD11b+CD11c+, CD11b+Ly6ChiLy6Glo/−, and CD4+ cells. (C) Cells from dLNs were stimulated with 20 μg/mL PLP180-199, and proliferation of cells was measured by [3H]adenine incorporation. (D-E) Analysis of splenocytes. (D) Total number of cells in the spleens of mice with EAE. (E) [3H]adenine incorporation assay for PLP180-199–stimulated splenocytes showing the average proliferation per mouse. (F-K) Analysis of the CNS. (F) Number of CD45hi cells. (G) Number of CD45hiCD11b+, CD45hiCD11b+CD11c+, CD11b+Ly6ChiLy6Glo/−, and CD4+ cells. (H) Representative flow cytometry plots showing MHC-II expression in myeloid DCs present in the CNS of the EAE mice. Gated on CD45hiCD11c+CD11b+ cells. (I) Quantification of the frequency of MHC-IIhi and MHC-IIlo cells among CD45hiCD11b+CD11c+ cells. (J) Histograms normalized to the mode of data depicting MHC-II, CD80, and CD86 expression among CD45hiCD11b+CD11c+ cells. (K) Quantification of the median fluorescent intensity of MHC-II, CD80, and CD86 expression among CD45hiCD11b+CD11c+MHC-II+ cells. Error bars are SEM, and significance was calculated using unpaired Student t test.
ΔdblGATA mice have defective priming in EAE. WT and ΔdblGATA mice were immunized for EAE induction and euthanized on day 8 after immunization (n = 4-5 per group; 2 independent experiments). (A-C) Analysis of inguinal dLN cells are shown in panels A-C. (A) Total number of CD45+ cells per mouse in inguinal dLNs. (B) Number of CD45+CD11b+, CD45+CD11b+CD11c+, CD11b+Ly6ChiLy6Glo/−, and CD4+ cells. (C) Cells from dLNs were stimulated with 20 μg/mL PLP180-199, and proliferation of cells was measured by [3H]adenine incorporation. (D-E) Analysis of splenocytes. (D) Total number of cells in the spleens of mice with EAE. (E) [3H]adenine incorporation assay for PLP180-199–stimulated splenocytes showing the average proliferation per mouse. (F-K) Analysis of the CNS. (F) Number of CD45hi cells. (G) Number of CD45hiCD11b+, CD45hiCD11b+CD11c+, CD11b+Ly6ChiLy6Glo/−, and CD4+ cells. (H) Representative flow cytometry plots showing MHC-II expression in myeloid DCs present in the CNS of the EAE mice. Gated on CD45hiCD11c+CD11b+ cells. (I) Quantification of the frequency of MHC-IIhi and MHC-IIlo cells among CD45hiCD11b+CD11c+ cells. (J) Histograms normalized to the mode of data depicting MHC-II, CD80, and CD86 expression among CD45hiCD11b+CD11c+ cells. (K) Quantification of the median fluorescent intensity of MHC-II, CD80, and CD86 expression among CD45hiCD11b+CD11c+MHC-II+ cells. Error bars are SEM, and significance was calculated using unpaired Student t test.
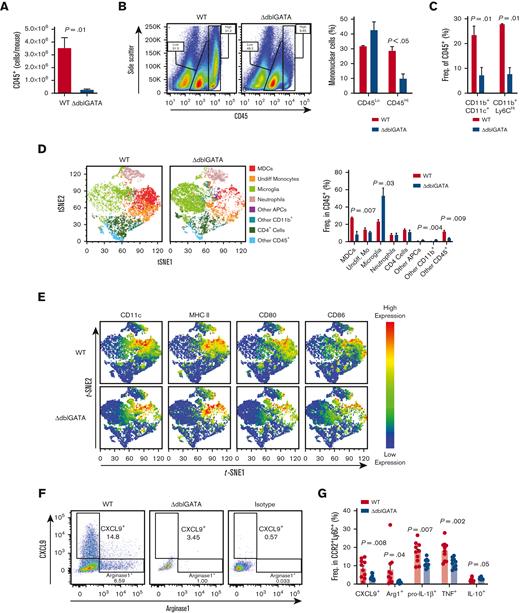
ΔdblGATA monocytes have reduced inflammatory APC phenotype in vivo but not in vitro
The diminished numbers of APCs in the ΔdblGATA mice during EAE may indicate a defect in APC development. To test this hypothesis, we generated BMDC cultures using GM-CSF ± IL-4. Similar to human monocytes,29 IL-4 induced GATA1 expression in murine BMDC cultures (Figure 5A). ΔdblGATA BMDCs showed lower GATA1 expression than WT BMDCs (Figure 5A; supplemental Figure 2A), and flow cytometry analysis revealed fewer CD11b+MHC-IIhi cells in ΔdblGATA cultures (Figure 5B-C). This could be explained by the diminished viability of the developing myeloid cells. However, real-time PCR analysis showed little difference between ΔdblGATA and WT cultures in the expression of the proapoptotic and antiapoptotic molecules caspase-3, Bcl-2, and Bcl-X (supplemental Figure 2B-D). Given that the predominant source of MHC-IIhi cells in GM-CSF/IL-4 BMDC cultures are monocytes,30 we used purified monocytes from WT and ΔdblGATA BM to develop BMDCs and then tested their APC function. Interestingly, WT and ΔdblGATA cultures had similar frequencies of MHC-IIhi cells, suggesting that BMDC differentiation was not affected (Figure 5D). Accordingly, LPS-treated ΔdblGATA and WT BMDCs elicited similar levels of proliferation as OVA323-339 peptide–specific CD4+ T cells from DO11.10 mice (Figure 5E).31 We also found no differences in phagocytosis and antigen processing32 between LPS-treated ΔdblGATA and WT CD11c+ BMDCs (supplemental Figure 2E-F).
MDCs from ΔdblGATA mice have reduced APC phenotype in vivo but not in vitro. (A-C) BM from WT and ΔdblGATA mice was treated with GM-CSF and IL-4 for 5 days. To induce BMDC maturation, the cultures were treated with LPS for an additional 3 days. Data represent the average of 2 independent experiments. (A) GATA1 expression by BMDCs determined by real-time PCR. (B) Flow cytometry plots showing MHC-II and CD11b expression among CD11b+CD11c+ BMDCs. (C) Frequency of MHC-IIhi cells among CD11b+CD11c+ BMDCs. (D) Flow cytometry plots showing MHC-II and CD11b expression among CD11b+CD11c+ MDCs were generated in vitro from CD45+CD11b+Ly6Glo/−Ly6Chi monocytes purified from the BM of WT and ΔdblGATA mice. Histograms overlays (right) of CD80 and CD86 expression from MHC-IIhi and MHC-IIlo cells (left) are depicted. (E) Proliferation of cocultures of LPS-matured MDCs from panel D with DO11.10 CD4+ T cells that were stimulated with OVA323–339 for 72 hours. Proliferation was measured by [3H]adenine incorporation assay. Error bars are SEM and significance was calculated by unpaired Student t test. (F) WT and ΔdblGATA mice were immunized for EAE induction and sacrificed on day 16 after immunization (n = 14-15 per group). CNS mononuclear cells were isolated by Percoll density gradient centrifugation, and cells from 4 to 5 mice were pooled. Monocytes were then highly enriched with CD11b magnetic beads followed by fluorescence-activated cell sorting for CD11b+Ly6ChiLy6Glo/− cells. RNA was isolated, and the transcriptomes of WT and ΔdblGATA monocytes were sequenced (bulk RNA sequencing; n = 3 per group). Differentially expressed genes with adjusted P < .05 were used for pathway analysis using DAVID bioinformatics database. The top 5 significantly enriched pathways using gene ontology and KEGG databases are shown. (G) Heatmap showing differentially expressed genes from the top gene ontology term from panel F. GAPDH, glyceraldehyde-3-phosphate dehydrogenase; Norm., normal.
MDCs from ΔdblGATA mice have reduced APC phenotype in vivo but not in vitro. (A-C) BM from WT and ΔdblGATA mice was treated with GM-CSF and IL-4 for 5 days. To induce BMDC maturation, the cultures were treated with LPS for an additional 3 days. Data represent the average of 2 independent experiments. (A) GATA1 expression by BMDCs determined by real-time PCR. (B) Flow cytometry plots showing MHC-II and CD11b expression among CD11b+CD11c+ BMDCs. (C) Frequency of MHC-IIhi cells among CD11b+CD11c+ BMDCs. (D) Flow cytometry plots showing MHC-II and CD11b expression among CD11b+CD11c+ MDCs were generated in vitro from CD45+CD11b+Ly6Glo/−Ly6Chi monocytes purified from the BM of WT and ΔdblGATA mice. Histograms overlays (right) of CD80 and CD86 expression from MHC-IIhi and MHC-IIlo cells (left) are depicted. (E) Proliferation of cocultures of LPS-matured MDCs from panel D with DO11.10 CD4+ T cells that were stimulated with OVA323–339 for 72 hours. Proliferation was measured by [3H]adenine incorporation assay. Error bars are SEM and significance was calculated by unpaired Student t test. (F) WT and ΔdblGATA mice were immunized for EAE induction and sacrificed on day 16 after immunization (n = 14-15 per group). CNS mononuclear cells were isolated by Percoll density gradient centrifugation, and cells from 4 to 5 mice were pooled. Monocytes were then highly enriched with CD11b magnetic beads followed by fluorescence-activated cell sorting for CD11b+Ly6ChiLy6Glo/− cells. RNA was isolated, and the transcriptomes of WT and ΔdblGATA monocytes were sequenced (bulk RNA sequencing; n = 3 per group). Differentially expressed genes with adjusted P < .05 were used for pathway analysis using DAVID bioinformatics database. The top 5 significantly enriched pathways using gene ontology and KEGG databases are shown. (G) Heatmap showing differentially expressed genes from the top gene ontology term from panel F. GAPDH, glyceraldehyde-3-phosphate dehydrogenase; Norm., normal.
In vitro culture conditions may obscure the differences in the development between ΔdblGATA and WT BMDCs. To address this, we compared the phenotypes of monocytic cells that developed in vivo during inflammation by sequencing the transcriptomes of WT and ΔdblGATA cells from the CNS of mice with EAE. We found 1690 genes that were differentially expressed between WT and ΔdblGATA monocytes (supplemental Table 1). Pathway analysis using the DAVID database21,22 identified the antigen-processing pathway as one of the most significantly enriched pathways between the WT and ΔdblGATA monocytes (Figure 5F). Further examination of the top significantly enriched gene ontology terms showed that genes associated with MHC-II–mediated antigen presentation were significantly downregulated in ΔdblGATA monocytes, consistent with the flow cytometry data (Figure 3D-E). These data further indicated that monocytes cause a deficit in APC function in vivo.
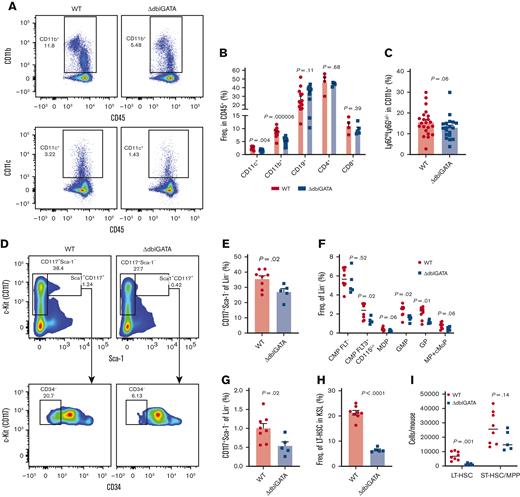
ΔdblGATA mice have reduced numbers of HSCs and MPs
We observed reduced numbers of immune cells in the CNS and secondary lymphoid organs of ΔdblGATA mice with EAE. To test whether these differences also existed in the steady state, we compared the composition of immune cells in the BM, dLN, and spleens of naïve WT and ΔdblGATA mice. In contrast to EAE, the frequencies of the major immune cells (CD11b+, CD11c+, CD19+, CD4+, and CD8+) were similar between WT and ΔdblGATA mice (supplemental Figure 3A-C). However, as in EAE, the frequencies of CD11b+ and CD11c+ cells were reduced in CD45+ PBMCs of ΔdblGATA mice (Figure 6A-B). Notably, the frequency of monocytes among CD11b+ cells was similar in both WT and ΔdblGATA mice (Figure 6C), indicating that the overall frequency of myeloid cells, not only monocytes, was reduced in the blood of the ΔdblGATA mice. The reduced frequency of CD11b+ myeloid cells only in the blood may reflect a reduced rate of their production by BM, which is, nonetheless, in steady state, still sufficient to populate the dLN, spleen, and BM, similar to that in WT mice. To test whether ΔdblGATA mice have a defect in myeloid cell production by the BM, we compared Lin−CD117+ HSPCs in the BM of WT and ΔdblGATA mice. There were multiple differences observed in the hematopoietic progenitor compartment, including a reduction in Lin−CD117+Sca1− cells, which are heavily enriched in myeloid cell progenitors (Figure 6D-E).33 Further subtyping identified a reduced frequency of myeloid cell progenitors in both CMP and GMP subsets (Figure 6F). In addition to reduced numbers of myeloid cell progenitors, ΔdblGATA mice also had reduced Lin−CD117+Sca1+ (LSK) HSCs (Figure 6G). Further subtyping of HSCs showed that this reduction was due to fewer cells with a phenotype consistent with that of LT-HSCs, whereas the numbers of short-term HSCs/multipotent progenitors were only slightly affected (Figure 6H-I). The full gating strategy is shown in supplemental Figure 3D. Taken together, these data indicate that GATA1 maintains HSCs in greater numbers, which then results in more downstream progenitors such as myeloid progenitors (MPs).
ΔdblGATA mice have reduced numbers of HSCs and myeloid cell progenitors. (A) Flow cytometry plots showing frequencies of CD11b+ and CD11c+ cells among CD45+ PBMCs in naïve WT and ΔdblGATA mice. (B) Frequencies of CD11b+, CD11c+, CD19+, CD4+, and CD8+ cells among CD45+ PBMCs. N = 4 to 13 per group. (C) Frequencies of Ly6ChiLy6Glo/− monocytes among CD11b+ PBMCs. N = 19 to 22 per group. (D-I) Quantification of hematopoietic progenitors in the BM of WT and ΔdblGATA mice. N = 5 to 8 per group, compiled from 2 independent experiments. (D) Flow cytometry plots depicting the expression of CD117 and CD34 among lineage negative cells (Lin−; CD3−B220−CD11b−TER119−Gr-1−). (E) Frequencies of CD117+Sca1− cells among Lin− cells. (F) Frequencies of MP populations among Lin− cells. Full gating and population definitions can be found in the supplemental Figure 3. (G) Frequencies of CD117+Sca1+ cells among Lin− cells. (H) Frequencies of long-term HSCs (LT-HSCs) among Lin−CD117+Sca1+ (KSL) cells. (I) Number of LT-HSCs and short-term HSCs/multipotent progenitors per mouse. Significance was determined by a 2-tailed unpaired t test. Error bars are SEM. CMP, common myeloid progenitor; GMP, granulocyte-myeloid progenitor; GP, granulocyte progenitor; MDP, monocyte-dendritic cell progenitor; cMoP, common monocyte progenitor.
ΔdblGATA mice have reduced numbers of HSCs and myeloid cell progenitors. (A) Flow cytometry plots showing frequencies of CD11b+ and CD11c+ cells among CD45+ PBMCs in naïve WT and ΔdblGATA mice. (B) Frequencies of CD11b+, CD11c+, CD19+, CD4+, and CD8+ cells among CD45+ PBMCs. N = 4 to 13 per group. (C) Frequencies of Ly6ChiLy6Glo/− monocytes among CD11b+ PBMCs. N = 19 to 22 per group. (D-I) Quantification of hematopoietic progenitors in the BM of WT and ΔdblGATA mice. N = 5 to 8 per group, compiled from 2 independent experiments. (D) Flow cytometry plots depicting the expression of CD117 and CD34 among lineage negative cells (Lin−; CD3−B220−CD11b−TER119−Gr-1−). (E) Frequencies of CD117+Sca1− cells among Lin− cells. (F) Frequencies of MP populations among Lin− cells. Full gating and population definitions can be found in the supplemental Figure 3. (G) Frequencies of CD117+Sca1+ cells among Lin− cells. (H) Frequencies of long-term HSCs (LT-HSCs) among Lin−CD117+Sca1+ (KSL) cells. (I) Number of LT-HSCs and short-term HSCs/multipotent progenitors per mouse. Significance was determined by a 2-tailed unpaired t test. Error bars are SEM. CMP, common myeloid progenitor; GMP, granulocyte-myeloid progenitor; GP, granulocyte progenitor; MDP, monocyte-dendritic cell progenitor; cMoP, common monocyte progenitor.
ΔdblGATA BM has reduced repopulation potential
The reduced numbers of HSCs in ΔdblGATA mice may result in a functional defect in immune cell production, which is likely to be more pronounced during inflammation. To test this hypothesis, we ablated the BM of CD45.1+ recipient mice with treosulfan, a BM conditioning agent that cannot cross the blood-brain barrier and therefore does not disturb CNS homeostasis.34-36 We then compared the ability of WT and ΔdblGATA BM to reconstitute treosulfan-treated recipients by IV transfer of a 1:1 mixture of WT (CD45.1+) and ΔdblGATA (CD45.2+) BM. Treosulfan-treated mice that received a 1:1 mixture of WT (CD45.1+) and WT (CD45.2+) BM served as controls. After reconstitution, there was a reduced frequency of ΔdblGATA-derived cells in the blood of the naïve mice (supplemental Figure 4). We then immunized mice with EAE to induce proliferative stress in the BM progenitors. Among PBMCs from mixed BM chimeras, the frequency of cells derived from ΔdblGATA BM was reduced when compared with WT cells (Figure 7A-B), resulting in a reduced CD45.2/CD45.1 cell ratio compared with control WT/WT chimera mice (Figure 7C). Examination of CNS-infiltrating immune cells (CD45+Sall1−) revealed a similar trend, with a reduced frequency of cells originating from the ΔdblGATA BM (Figure 7D-E). Notably, there were no differences in the frequencies of WT and ΔdblGATA Ly6C+CCR2+ monocytes in the CNS (Figure 7F-G), indicating that the reduced frequency of monocytes in ΔdblGATA mice with EAE (Figure 3D) was due to the reduced production of immune cells in response to inflammation. Taken together, these data indicate that GATA1 regulates the numbers of hematopoietic progenitors, and loss of the dblGATA enhancer causes a reduction in progenitors, leading to a diminished inflammatory response.
ΔdblGATA BM has reduced repopulation potential. (A) The BM of WT CD45.1+ mice was ablated by intraperitoneal injections of treosulfan, and mice were then IV injected with 8 × 106 BM cells, which were a 1:1 mixture of either WT CD45.1+ plus WT CD45.2+ BM or WT CD45.1+ plus ΔdblGATA CD45.2+ BM. After at least 8 weeks of reconstitution, mice were immunized with PLP180-199 to induce EAE and sacrificed on day 16 after immunization for the analysis of peripheral blood and CNS mononuclear cells. (B-G) Analysis of experiment described in panel A. (B) CD45.1+ and CD45.2+ cells among PBMCs of mixed chimera mice. (C) Frequency of CD45.2+ cells divided by frequency of CD45.1+ cells. (D) CD45.1+ and CD45.2+ cells among CD45+Sall1− (nonmicroglia) cells in the CNS during EAE. (E) Frequency of CD45.2+ cells divided by frequency of CD45.1+ cells. Cells included in analysis were pregated on CD45+Sall1− (CNS-infiltrating immune cells). (F) Ly6ChiCCR2+ monocytes among the gated CD45.1+ or CD45.2+ CD11b+ cells from the CNS. (G) Ratios of frequency of CD45.2+Ly6C+CCR2+ monocytes in CD45.2+CD11b+ cells divided by frequency of CD45.1+Ly6C+CCR2+ monocytes in CD45.1+CD11b+ cells. Significance was determined by 2-tailed t test. Error bars are SEM. N = 11 to 12 mice per group; data were compiled from 2 independent experiments.
ΔdblGATA BM has reduced repopulation potential. (A) The BM of WT CD45.1+ mice was ablated by intraperitoneal injections of treosulfan, and mice were then IV injected with 8 × 106 BM cells, which were a 1:1 mixture of either WT CD45.1+ plus WT CD45.2+ BM or WT CD45.1+ plus ΔdblGATA CD45.2+ BM. After at least 8 weeks of reconstitution, mice were immunized with PLP180-199 to induce EAE and sacrificed on day 16 after immunization for the analysis of peripheral blood and CNS mononuclear cells. (B-G) Analysis of experiment described in panel A. (B) CD45.1+ and CD45.2+ cells among PBMCs of mixed chimera mice. (C) Frequency of CD45.2+ cells divided by frequency of CD45.1+ cells. (D) CD45.1+ and CD45.2+ cells among CD45+Sall1− (nonmicroglia) cells in the CNS during EAE. (E) Frequency of CD45.2+ cells divided by frequency of CD45.1+ cells. Cells included in analysis were pregated on CD45+Sall1− (CNS-infiltrating immune cells). (F) Ly6ChiCCR2+ monocytes among the gated CD45.1+ or CD45.2+ CD11b+ cells from the CNS. (G) Ratios of frequency of CD45.2+Ly6C+CCR2+ monocytes in CD45.2+CD11b+ cells divided by frequency of CD45.1+Ly6C+CCR2+ monocytes in CD45.1+CD11b+ cells. Significance was determined by 2-tailed t test. Error bars are SEM. N = 11 to 12 mice per group; data were compiled from 2 independent experiments.
Discussion
Our findings showed that ΔdblGATA mice were resistant to EAE; however, this was not due to the absence of eosinophils. This suggests that ΔdblGATA mice have an additional unknown defect(s) that substantially affects immune system function, which was unexpected because ΔdblGATA mice have been used as an eosinophil-deficient model for 20 years. The existence of an unknown defect in ΔdblGATA mice raises the possibility that some of the findings in these mice may have been mistakenly attributed to the lack of eosinophils. While searching for additional defects, we found that ΔdblGATA mice developed notably milder neuroinflammation, with far fewer immune cells infiltrating the CNS. The numbers of monocytes and monocyte-derived cells, such as MDCs, were reduced the most, coinciding with the reduced numbers of CD11b+ myeloid cells in the peripheral blood and lymphoid organs. Monocyte-derived cells, such as MDCs, are potent APCs37; they are also the main effector cells that directly inflict damage to the CNS tissue and are thus essential in the immunopathogenesis of EAE.28,38,39 Hence, the reduced number of monocyte-derived cells in the CNS is likely the major contributing factor to the diminished EAE severity observed in ΔdblGATA mice. These data align well with the functions of GATA1 in the development and/or function of myeloid cells, as complete loss of GATA1 results in the accumulation of early MP cells and reductions in the numbers of later progenitors, blood monocytes, and CD11c+ cells in the spleen.4 Knockout of GATA1 in CD11c+ cells also affects DC migration toward CCL21 because of reduced polysialic acid levels on their cell surface.40 ΔdblGATA monocyte/DC might also have a migratory defect, a possibility that remains to be tested.
EAE is predominantly a CD4+ T-cell–driven disease, and diminished T-cell responses due to impaired APC function can result in less neuroinflammation, with fewer immune cells infiltrating the CNS, including fewer monocyte-derived cells.41,42 To determine whether diminished T-cell priming in ΔdblGATA mice causes EAE resistance, we tested their susceptibility to adoptive EAE by transferring primed myelin-specific WT and ΔdblGATA CD4+ T cells to WT or ΔdblGATA recipient mice. However, even the transfer of WT CD4+ T cells could not induce EAE in ΔdblGATA recipient mice, suggesting that they have a defect in inducing and amplifying inflammation, independent of priming pathogenic T-cell responses. The resistance of ΔdblGATA mice to adoptive EAE could be explained by either a defect in APCs that reactivate CD4+ T cells in the CNS43 or the subsequent recruitment and/or function of immune cells in the CNS. To test whether the ΔdblGATA mutation causes a cell-intrinsic defect in APC function, we tested APC function in BMDCs. ΔdblGATA BMDC cultures had fewer CD11c+MHC-IIhi cells and expressed less GATA1 than the control WT cultures, but there were no cell-intrinsic differences in antigen processing or presentation. However, such in vitro data should be interpreted with caution, as culture conditions, such as relatively high GM-CSF concentrations, may distort the physiological functions of the dblGATA enhancer or GATA1. For example, the dblGATA enhancer is required for eosinophil development in vivo, but not in vitro, exemplifying that culture conditions can circumvent the need for the enhancer.44 Concerning the APC function of monocytes, transcriptome sequencing of monocytes from the CNS of mice with EAE showed reduced gene expression for antigen processing and presentation by ΔdblGATA monocytes, indicating that GATA1 affects the development of the proinflammatory phenotype of monocyte-derived cells in a monocyte-intrinsic manner, similar to what has been shown in vitro for human monocytes.5 Alternatively, the less inflammatory phenotype of ΔdblGATA monocytes could be a consequence of monocyte-extrinsic factors, such as the milder inflammatory milieu they encounter in the CNS of ΔdblGATA mice. Nevertheless, our in vitro data suggest that rather than a cell-intrinsic defect in APC function, it is the production of immune cells, including myeloid cells, that is affected in ΔdblGATA mice. Thus, further studies are needed to determine whether the dblGATA enhancer causes a functional difference only in HSPCs, resulting in diminished output of monocytes by the BM, or whether there is also a role for the enhancer, and hence GATA1, in shaping the phenotype of monocyte-derived cells in inflamed tissues.
GATA1 is expressed in HSCs and its expression is controlled by the dblGATA enhancer,7 but the function of GATA1 in HSCs remains poorly understood. Our data suggest that GATA1 increases the numbers of HSCs and in that way also increases immune cell production. In line with this hypothesis, competitive BM reconstitution revealed a reduced capacity of ΔdblGATA BM to repopulate immune cells in the blood in both the steady state and EAE, as well as in the CNS during EAE. Alternatively, GATA1 can control the expansion kinetics of BM cells, rather than the numbers of HSCs. Our characterization of hematopoietic progenitors revealed reduced numbers of LT-HSCs and myeloid cell progenitors in ΔdblGATA BM. Notably, the major immune cell populations in the BM, spleen, and dLNs of naïve ΔdblGATA and WT mice were similar, indicating that the production rate of immune cells in ΔdblGATA mice was sufficient to maintain their normal numbers in a steady state. However, a reduced capacity for the production of immune cells could become apparent when proliferative stress is placed on BM progenitors, such as in the inflammation caused by EAE. The reduced frequency of MPs in the ΔdblGATA BM suggests that a defect in GATA1 expression in HSCs may have downstream consequences for MPs. This concept is supported by the finding that reduced GATA1 expression in a subset of HSCs reduced the expression of myeloid signature genes.6 The molecular pathways whereby GATA1 affects HSCs and the downstream development of HSC-derived progenitor cells involve a complex interplay among multiple transcription factors that is yet to be elucidated.45
ΔdblGATA mice have been used as an eosinophil-deficient model; however, our study demonstrated that findings solely attributed to eosinophil deficiency could be inaccurate because of defects in HSCs and myeloid cell development in these mice. Thus, the findings made with the use of ΔdblGATA mice may need to be reexamined. Overall, our study suggests that GATA1 affects the immune response by regulating multiple stages of hematopoietic development and that altered GATA1 expression in HSPCs could result in resistance to pathologies of autoimmune etiology. Finally, our findings suggest that if methods to modulate GATA1 gene expression are devised, they could have clinical applications for altering immune responses, such as dampening those that are harmful.
Acknowledgments
The authors thank Katherine Regan for editing the manuscript and James Lee for his assistance on this project.
This work was supported by a grant from the National Institute of Allergy and Infectious Diseases, National Institutes of Health (T32 training grant T32AI134646).
Authorship
Contribution: D.H. designed experiments, analyzed data, and wrote the manuscript; B.C. designed experiments and assisted in writing the manuscript; L.L.W.I., M.S.S., E.M., E.K., Z.S., A.B., S.J., and J.R. assisted with experiments; C.V., M.G., and H.H. assisted with RNA sequencing experiments and analysis; and A.R. and G.-X.Z. assisted in manuscript preparation.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bogoljub Ciric, Department of Neurology, Jefferson Hospital for Neuroscience, Thomas Jefferson University, 900 Walnut Street, Suite 300, Philadelphia, PA 19107; e-mail: bogoljub.ciric@jefferson.edu.
References
Author notes
Data are available on request from the corresponding author, Bogoljub Ciric (bogoljub.ciric@jefferson.edu).
The full-text version of this article contains a data supplement.

![Eosinophils do not contribute to EAE. (A) Flow cytometry overlay of BM-derived eosinophil (Eos) cultures showing double-staining for Siglec-F and CCR3 (blue) and with isotype monoclonal antibodies (red). (B) Adoptive transfer of BM-derived eosinophils. WT and ΔdblGATA mice were immunized for EAE, and 2 × 107 eosinophils were injected IV on days 7 and 9 after immunization into ΔdblGATA mice. (C) Clinical scores and change in body weight are shown. Representative figures from 1 of 2 independent experiments. Significance was calculated by 2-way ANOVA (n = 4 for WT and ΔdblGATA groups; n = 6 for ΔdblGATA and eosinophil group). (D) Clinical course of EAE in WT C57BL6/J and PHIL mice (n = 5 per group). (E) Relative numbers of CD45+ cells isolated from the CNS (brains and spinal cords combined) of WT and PHIL mice. (F) Frequencies of CD11b+ and CD4+ cells within CD45+ cells from the CNS of WT and PHIL mice. (G) Frequencies of Th1 (interferon γ+ [IFN-γ+] IL-17A), Th17 (IL-17A+IFN-γ−), Th1/17 (IFN-γ+IL-17A+), regulatory T cell (Treg) (FoxP3+), and GM-CSF+ T helper cells from the CNS of WT and PHIL mice. (H) Proliferation assay. Mononuclear cells isolated from the CNS of WT and PHIL mice were stimulated for 18 hours with 25 μg/mL MOG35-55 (immunizing peptide) and 1 μCurie per well of [3H]adenine was added for additional 18 hours. Cells were then harvested, and counts per minute (C.P.M.) were measured using beta counter. (I) Clinical scores for adoptive EAE in WT, PHIL, 1638 (IL-5tg), and 1638/PHIL mice. Abs, antibodies; Freq., frequency.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/6/23/10.1182_bloodadvances.2022008234/6/m_blooda_adv-2022-008234-gr2.jpeg?Expires=1765931547&Signature=qjvuEA4f2waY07ugQHLnqkWPalwXZTDeNBGTo0VQjQvaaA9EGE842vIt-kAnyZhL9gGFdNFt4qiSOmwgVXHV~ZkU3CWo4qfSaQXnD7ihY3RDp1qdc~eo-kf67e0ahCINxoQ~xd~5Vmxg4MNYjB~xNjvApf3cWW~vbseIA2R4GdLmOUlFZ60aRdBKHz1YlDbRP092A8UupKU-aUgjXQjWzHTZvCVVzU0JOkUj4~jGEyxhfRBDun82HYQO3r~lB0BK6gn~kHGt67Bi6wkDDDArj-7o1~G9EN1dYNuL~zFiDnsc~osbCWwP2EGOrRtk46wYyJRnT3IcqJYX2-n~3YNfiA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![ΔdblGATA mice have defective priming in EAE. WT and ΔdblGATA mice were immunized for EAE induction and euthanized on day 8 after immunization (n = 4-5 per group; 2 independent experiments). (A-C) Analysis of inguinal dLN cells are shown in panels A-C. (A) Total number of CD45+ cells per mouse in inguinal dLNs. (B) Number of CD45+CD11b+, CD45+CD11b+CD11c+, CD11b+Ly6ChiLy6Glo/−, and CD4+ cells. (C) Cells from dLNs were stimulated with 20 μg/mL PLP180-199, and proliferation of cells was measured by [3H]adenine incorporation. (D-E) Analysis of splenocytes. (D) Total number of cells in the spleens of mice with EAE. (E) [3H]adenine incorporation assay for PLP180-199–stimulated splenocytes showing the average proliferation per mouse. (F-K) Analysis of the CNS. (F) Number of CD45hi cells. (G) Number of CD45hiCD11b+, CD45hiCD11b+CD11c+, CD11b+Ly6ChiLy6Glo/−, and CD4+ cells. (H) Representative flow cytometry plots showing MHC-II expression in myeloid DCs present in the CNS of the EAE mice. Gated on CD45hiCD11c+CD11b+ cells. (I) Quantification of the frequency of MHC-IIhi and MHC-IIlo cells among CD45hiCD11b+CD11c+ cells. (J) Histograms normalized to the mode of data depicting MHC-II, CD80, and CD86 expression among CD45hiCD11b+CD11c+ cells. (K) Quantification of the median fluorescent intensity of MHC-II, CD80, and CD86 expression among CD45hiCD11b+CD11c+MHC-II+ cells. Error bars are SEM, and significance was calculated using unpaired Student t test.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/6/23/10.1182_bloodadvances.2022008234/6/m_blooda_adv-2022-008234-gr4.jpeg?Expires=1765931547&Signature=wAr1CXKh4IUcfV3oa6cjFoPIVcsX8W33n0VA-i1znsEkkKMC3ubt4ndBoEhnO1hrcpcO2E8hunMAtfHf2t7xFp5fpjnE3yni4xUl-kvh6Cz5~cAym0QQ0a3iJVIJY8zArQNVXqLyWbthav~4w4lzSnK93MPhtLtURrIS8rQjWV0ieA9cldQXRzGxpjGVOhZt0Mrfehu920NqyD4YXrC3aVV-Sq2DWfDj15bLRZVE2-aMAtg-dPRoilJVfsMPXpoVI6LY~-W491RzgE2SPa0dvufIF4hjBpu~k3379MxyCeismCBvtKP7J8ychEbNDrQfmZ7He3tT2FBg7GTeN1EdmQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![MDCs from ΔdblGATA mice have reduced APC phenotype in vivo but not in vitro. (A-C) BM from WT and ΔdblGATA mice was treated with GM-CSF and IL-4 for 5 days. To induce BMDC maturation, the cultures were treated with LPS for an additional 3 days. Data represent the average of 2 independent experiments. (A) GATA1 expression by BMDCs determined by real-time PCR. (B) Flow cytometry plots showing MHC-II and CD11b expression among CD11b+CD11c+ BMDCs. (C) Frequency of MHC-IIhi cells among CD11b+CD11c+ BMDCs. (D) Flow cytometry plots showing MHC-II and CD11b expression among CD11b+CD11c+ MDCs were generated in vitro from CD45+CD11b+Ly6Glo/−Ly6Chi monocytes purified from the BM of WT and ΔdblGATA mice. Histograms overlays (right) of CD80 and CD86 expression from MHC-IIhi and MHC-IIlo cells (left) are depicted. (E) Proliferation of cocultures of LPS-matured MDCs from panel D with DO11.10 CD4+ T cells that were stimulated with OVA323–339 for 72 hours. Proliferation was measured by [3H]adenine incorporation assay. Error bars are SEM and significance was calculated by unpaired Student t test. (F) WT and ΔdblGATA mice were immunized for EAE induction and sacrificed on day 16 after immunization (n = 14-15 per group). CNS mononuclear cells were isolated by Percoll density gradient centrifugation, and cells from 4 to 5 mice were pooled. Monocytes were then highly enriched with CD11b magnetic beads followed by fluorescence-activated cell sorting for CD11b+Ly6ChiLy6Glo/− cells. RNA was isolated, and the transcriptomes of WT and ΔdblGATA monocytes were sequenced (bulk RNA sequencing; n = 3 per group). Differentially expressed genes with adjusted P < .05 were used for pathway analysis using DAVID bioinformatics database. The top 5 significantly enriched pathways using gene ontology and KEGG databases are shown. (G) Heatmap showing differentially expressed genes from the top gene ontology term from panel F. GAPDH, glyceraldehyde-3-phosphate dehydrogenase; Norm., normal.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/6/23/10.1182_bloodadvances.2022008234/6/m_blooda_adv-2022-008234-gr5.jpeg?Expires=1765931547&Signature=CLwfRRDKixw4EKc2SpKSIE0gNqOkHr1SAHY3h2FI7OtRZw1kkF-DjfN6e9hufcIDLudakonJ5tq3Nc~Vvp1~IfjwiDnJ7~cDhA3rTQuurKiBNqF5pBz8NaXQV2jZ3EdVamFt3pZpavzqHl4nAbTV8P-vdY3~SrbC0NMoCVqV7-apWi21atwpdo3ysfTijPluR6lANC32xNzUiXw5C6gM56pUlWQ612kC47CKbxxl8U5YRukaps1tEa4dcXkpQd-zIQSRxHLm~V2COmc1deq00nzylG4v507~2PPgOTqpSnVKqo6ENeLcBoh0~Cyl0zHl50dVEvSLCduTCSb06UIVTg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)