Key Points
Patients with APL treated with ATRA-ATO reported better long-term quality of life outcomes than patients treated with chemotherapy.
Late comorbidity and health problem prevalence was similar between patients with APL previously treated with ATRA-ATO or chemotherapy.
Abstract
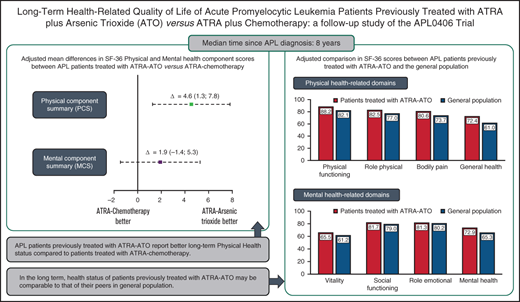
The main objective of this study was to compare the long-term health-related quality of life of patients with acute promyelocytic leukemia (APL) treated with all-trans retinoic acid (ATRA) plus arsenic trioxide (ATO) vs ATRA plus standard chemotherapy. Patients previously enrolled in the randomized controlled trial APL0406 were considered eligible for this follow-up study. The following patient-reported outcome measures were used: the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core30 (EORTC QLQ-C30), the EORTC Quality of Life Questionnaire Chemotherapy-Induced Peripheral Neuropathy 20 (QLQ-CIPN20), and the Short Form Health Survey 36 (SF-36). The prevalence of late comorbidities and health problems was also assessed. The clinical significance of differences was evaluated based on predefined thresholds. A total of 161 of 232 potentially eligible patients were analyzed, of whom 83 were treated with ATRA-ATO and 78 were treated with ATRA chemotherapy. The median time since diagnosis of the study sample was 8 years. The 2 largest clinically meaningful differences in the EORTC QLQ-C30 were observed for role functioning (Δ = 8.4; 95% confidence interval [CI], 0.5 to 16.3) and dyspnea (Δ = −8.5; 95% CI, −16.4 to −0.7), favoring patients treated with ATRA-ATO. With regard to the SF-36 results, a clinically relevant better physical component score (Δ = 4.6; 95% CI, 1.3 to 7.8) was observed in patients treated with ATRA-ATO, but this was not the case for the mental component score. The 2 groups showed similar profiles in the scores of the EORTC QLQ-CIPN20 scales and in the prevalence of late comorbidities. Overall, our findings suggest that the greater and more sustained antileukemic efficacy of ATRA-ATO is also associated with better long-term patient-reported outcomes than ATRA chemotherapy. This study was registered at www.clinicaltrials.gov as #NCT03096496.
Introduction
Acute promyelocytic leukemia (APL) is a rare subtype of acute myeloid leukemia (AML) characterized by distinctive morphological, biologic, and clinical features. The hallmark of the disease is the chromosomal translocation t(15;17) leading to the production of PML-RARA, a fusion oncogene that has a repressor role.1 The course of APL has dramatically improved from a fatal form of leukemia to a curable disease with the use of the vitamin A derivative all-trans retinoic acid (ATRA) in conjunction with anthracycline-based chemotherapies,2,3 which has been the standard of care until recently. Further treatment advances in APL have resulted from the introduction of arsenic trioxide (ATO) in combination with ATRA therapy.
Mainly based on results from 2 phase 3 randomized controlled trials (RCTs) comparing first-line ATO-ATRA vs ATRA chemotherapy in patients with APL, that is, AML174 and APL0406,5,6 ATO was granted regulatory approval and is now included in international treatment recommendations.7 We previously reported efficacy results of the APL0406 RCT,5,6 which indicated that after a median follow-up of 40.6 months, the event-free survival and overall survival at 50 months for patients treated with ATRA-ATO vs ATRA chemotherapy were 97.3 vs 80%, and 99.2% vs 92.6%, respectively.6 A recent analysis of this study further confirmed the survival advantages of ATRA-ATO therapy.8
Given the importance of the patient’s perspective on the impact of therapy during drug development process,9 health-related quality of life (HRQoL) was included as a secondary end point in the APL0406 trial protocol, which stipulated 2 HRQoL assessments during the on-treatment period (ie, after induction and after the third consolidation course). The results of this short-term HRQoL evaluation showed clinically meaningful differences in fatigue severity, favoring patients treated with ATRA-ATO vs ATRA chemotherapy after the initial induction therapy, and no HRQoL differences after the third consolidation course.10 However, the effects of ATO therapy on patients’ HRQoL are largely unknown and, to the best of our knowledge, no comparative data exist with regard to the long-term HRQoL of patients treated with ATRA-ATO vs those treated with ATRA and standard chemotherapy.
Therefore, we performed a follow-up study to assess long-term HRQoL and late effects in patients previously enrolled in the APL0406 RCT6 to more comprehensively understand the benefits and risks of ATO therapy in APL patients.
Patients and methods
Study design and patients
Eligible patients for the current long-term follow-up study were all those enrolled in the Italian-German APL0406 phase 3 RCT, who were in first molecular complete remission after third consolidation treatment (N = 232).6 Details on the design and main clinical efficacy results of the APL0406 RCT were previously reported.5,6
The research protocol of the current study (ie, APL0816) was specifically developed to assess long-term survivorship issues in former APL0406 patients after the end of treatment. The corresponding schedule of HRQoL assessments in the 2 protocols is depicted in supplemental Figure 1. The APL0816 protocol stipulated that investigators had to invite eligible patients to participate at their earliest convenience (in any case, after having received local ethical approval), when meeting him or her in the hospital during a follow-up visit or, alternatively, via a mailed invitation. Consenting patients were given a survey booklet, including patient-reported outcome (PRO) questionnaires, with the request to complete it at home. All data were then analyzed at GIMEMA Data Center, Rome, Italy, by linking information obtained from the survey booklets with clinical and laboratory data already available in the main RCT database.6 To ensure a uniform approach to recruitment procedures across all centers, standard operating procedures detailing how to engage patients were included in the study protocol.
The main objective of the current APL0816 survivorship study was to assess cross-sectional HRQoL differences between patients formerly assigned to either treatment arm in the APL0406 RCT. Two longer term PRO assessments were planned in the APL0816 protocol to also address other specific APL survivorship issues, and data collection is ongoing; the corresponding results will be published in the future.
This study was conducted in accordance with the Declaration of Helsinki and was approved by all Ethics Committees of each participating center. All patients provided written informed consent.
PRO assessment
The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core30 (EORTC QLQ-C30) (version 3) was used to assess HRQoL.11 This validated questionnaire consists of 5 functioning scales: physical, role, emotional, cognitive, and social; 3 symptom scales: fatigue, nausea/vomiting, and pain; 6 single-item scales: dyspnea, sleep disturbance, appetite loss, constipation, diarrhea, and financial difficulties; and the global health status/quality of life scale. The items were scaled and scored using the recommended EORTC procedures.12 This questionnaire was successfully used in our previous analysis10 and in other studies with patients with other types of acute leukemias.13 Based on previous data indicating differences between groups in neurotoxicity, mainly in terms of the prevalence of peripheral nerve neuropathy (ie, higher in the group of patients treated with ATRA-ATO), the EORTC Quality of Life Questionnaire Chemotherapy-Induced Peripheral Neuropathy 20 (QLQ-CIPN20) questionnaire was also used.14 This validated questionnaire consists of 20 items assessing peripheral neuropathic side effects of chemotherapy in cancer patients and includes 3 subscales assessing sensory (9 items), motor (8 items), and autonomic (3 items) symptoms and functioning.14
Health status was assessed with the well-validated Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36)15 (version 1), which consists of 36 items yielding 8 scales: physical functioning, role limitations because of physical problems, bodily pain, general health perceptions, vitality, social functioning, role limitations from emotional problems, and mental health. From a weighted combination of these 8 scales, 2 higher order component scores, 1 for physical health, that is, the physical component score (PCS) and 1 for mental health, that is, the mental component score (MCS), were also calculated.16 This questionnaire was found to be sensitive in capturing health status changes in previous long-term follow-up studies with patients with hematologic malignancies.17
Assessment of comorbidities and health problems
Considering the importance of collecting data on long-term complications and problems of current APL-directed therapy,18 we also examined comorbidity and late health problems using a survey of 23 items adapted from the validated Self-Administered Comorbidity Questionnaire19 and from a previous survey used by Messerer and colleagues to investigate late effects of AML.20 Patients were asked to rate the presence of these problems as developed during the previous 12 months from current study entry, and answers were categorized as yes or no.
Statistical methods
All HRQoL outcomes were compared between 2 groups of patients defined by previous randomly assigned treatments received for APL: ATRA-ATO vs ATRA chemotherapy. Based on previous findings4,10 and clinical considerations, the following scales of the EORTC QLQ-C30 were prespecified in the APL 0816 protocol as the main HRQoL scales for cross-sectional exploratory comparisons: role functioning, cognitive functioning, and fatigue. We summarized the main characteristics of patients with APL at study entry overall and by treatment group, using frequencies, proportions, medians, and interquartile ranges, depending on the type of variable. To detect possible confounders of between-group HRQoL comparisons, we assessed possible systematic differences in main characteristics between patients from either treatment arm by Fisher’s exact, χ2, or Wilcoxon-Mann-Whitney tests, depending on the type of variable. We considered multivariable linear regression analysis to assess mean differences between treatment groups for each scale, adjusting for possible confounders. In any case, as prespecified in this long-term follow-up study protocol, each regression model had to include the time since APL0406 RCT protocol completion as independent variable, the rationale being the different duration of previous treatment between arms.5
The clinical significance of the adjusted mean differences was evaluated according to previously published criteria, which define the minimal important difference.21 For the EORTC QLQ-C30 questionnaire, we used the scale-specific thresholds reported by Cocks and colleagues,22 whereas for the EORTC QLQ-CIPN20 questionnaire, we used the half-a-standard deviation threshold rule.23 With regard to the SF-36 questionnaire, we considered a minimal important difference a difference of 8 points in the corresponding 8 scales24 and 2 points for the 2 higher order component scores (ie, PCS and MCS).25,26
For descriptive purposes, we reported the prevalence of specific self-reported comorbidities, assessed by items adapted from the Self-Administered Comorbidity Questionnaire19 and from Messerer and colleagues.20 We also performed adjusted comparisons of the health status of patients with APL previously treated with ATRA-ATO with the general population (GP). For this purpose, we computed the mean differences in the SF-36 scores, between ATRA-ATO patients and adult subjects without cancer from the GP27 who were previously matched to ATRA-ATO patients by an optimal full matching procedure based on sex and age.
To assess the robustness and generalizability of our findings, we compared the main characteristics of patients included in our analyses vs those who could not be enrolled in this follow-up study to examine possible selection bias.28 All statistical tests were 2-sided with type I error α = 0.05. Because of the exploratory nature of cross-sectional comparisons between arms in the 3 main scales, we did not adjust for multiple testing. Also, all findings from the remaining analyses were considered descriptive and no formal statistical tests were performed.29 All analyses were performed using SAS statistical software, version 9.4.
Results
Patient characteristics
Between April 2017 and January 2020, 162 patients (of the 232 potentially eligible) were enrolled from 54 centers in this long-term follow-up study. For 1 patient treated with ATRA-ATO, the HRQoL questionnaire was not available; therefore, all analyses were based on 161 patients. A detailed flowchart of the patients considered for this study is reported in supplemental Figure 2.
The median age of the 161 patients analyzed was 55.2 years with an interquartile range (IQR) from 45 to 66.2 years, and the median time since diagnosis was 8 years (IQR, 6.6, 9.1). Given the different treatment RCT schemas, the median time since APL0406 protocol completion was shorter (P < .001) for patients treated with ATRA chemotherapy (5.9 years; IQR, 3.6, 6.8) than for those treated with ATRA-ATO (7.3 years; IQR, 6.3, 8.5). However, no statistically significant differences were detected between treatment groups with regard to key variables, including APL disease characteristics at diagnosis (eg, the risk level, P = .334). Further characteristics of patients with APL analyzed, overall and by type of previous treatment (ATRA-ATO vs ATRA chemotherapy) are reported in Table 1. In addition, no statistically significant differences were found in selected key variables between patients who could not be approached to participate for any reason (N = 70) and those who were considered in the current analysis (Table 2).
Main characteristics of long-term patients with APL by previous treatment arm
| Variables . | Overall (n = 161) . | ATRA plus arsenic trioxide (n = 83) . | ATRA plus chemotherapy (n = 78) . | P value . |
|---|---|---|---|---|
| Age at study entry, y | .450 | |||
| Mean (SD) | 54.2 (14.6) | 53.4 (14.7) | 55.1 (14.5) | |
| Median (IQR) | 55.2 (45.0-66.2) | 53.5 (40.8-66.9) | 55.7 (46.0-66.2) | |
| Sex, n (%) | .875 | |||
| Male | 79 (49.1) | 40 (48.2) | 39 (50.0) | |
| Female | 82 (50.9) | 43 (51.8) | 39 (50.0) | |
| Time since diagnosis, y | .800 | |||
| Mean (SD) | 7.8 (1.6) | 7.9 (1.5) | 7.8 (1.7) | |
| Median (IQR) | 8.0 (6.6-9.1) | 7.8 (6.9-9.2) | 8.1 (6.2-9.1) | |
| Number of comorbidities, n (%) | .311 | |||
| 0 | 35 (21.7) | 18 (21.7) | 17 (21.8) | |
| 1 | 35 (21.7) | 22 (26.5) | 13 (16.7) | |
| ≥2 | 91 (56.6) | 43 (51.8) | 48 (61.5) | |
| Received additional treatment of APL | .089 | |||
| No | 151 (94.4) | 81 (97.6) | 70 (90.9) | |
| Yes | 9 (5.6) | 2 (2.4) | 7 (9.1) | |
| Missing | 1 (.) | 0 (.) | 1 (.) | |
| Most recent RT-PCR PML-RAR alfa test, n (%) | .193 | |||
| Negative | 130 (96.3) | 68 (98.6) | 62 (93.9) | |
| Positive | 5 (3.7) | 1 (1.4) | 4 (6.1) | |
| Missing | 26 (.) | 14 (.) | 12 (.) | |
| Variables at APL diagnosis | ||||
| WBC count, ×109/L | .097 | |||
| Mean (SD) | 2.1 (2.2) | 2.4 (2.5) | 1.8 (1.8) | |
| Median (IQR) | 1.2 (0.8-2.3) | 1.4 (0.9-2.6) | 1.2 (0.7-1.8) | |
| Platelet count, ×109/L | .392 | |||
| Mean (SD) | 50.3 (45.2) | 53.9 (47.0) | 46.6 (43.2) | |
| Median (IQR) | 34.0 (18.0-64.0) | 36.5 (18.0-83.5) | 32.0 (18.0-58.0) | |
| Hemoglobin count, g/dL | .553 | |||
| Mean (SD) | 9.5 (2.1) | 9.7 (2.1) | 9.4 (2.1) | |
| Median (IQR) | 9.2 (8.3-11.0) | 9.2 (8.5-11.1) | 9.2 (8.0-11.0) | |
| Risk level, n (%) | .334 | |||
| Low | 68 (43.3) | 38 (47.5) | 30 (39.0) | |
| Intermediate | 89 (56.7) | 42 (52.5) | 47 (61.0) | |
| Missing | 4 (.) | 3 (.) | 1 (.) |
| Variables . | Overall (n = 161) . | ATRA plus arsenic trioxide (n = 83) . | ATRA plus chemotherapy (n = 78) . | P value . |
|---|---|---|---|---|
| Age at study entry, y | .450 | |||
| Mean (SD) | 54.2 (14.6) | 53.4 (14.7) | 55.1 (14.5) | |
| Median (IQR) | 55.2 (45.0-66.2) | 53.5 (40.8-66.9) | 55.7 (46.0-66.2) | |
| Sex, n (%) | .875 | |||
| Male | 79 (49.1) | 40 (48.2) | 39 (50.0) | |
| Female | 82 (50.9) | 43 (51.8) | 39 (50.0) | |
| Time since diagnosis, y | .800 | |||
| Mean (SD) | 7.8 (1.6) | 7.9 (1.5) | 7.8 (1.7) | |
| Median (IQR) | 8.0 (6.6-9.1) | 7.8 (6.9-9.2) | 8.1 (6.2-9.1) | |
| Number of comorbidities, n (%) | .311 | |||
| 0 | 35 (21.7) | 18 (21.7) | 17 (21.8) | |
| 1 | 35 (21.7) | 22 (26.5) | 13 (16.7) | |
| ≥2 | 91 (56.6) | 43 (51.8) | 48 (61.5) | |
| Received additional treatment of APL | .089 | |||
| No | 151 (94.4) | 81 (97.6) | 70 (90.9) | |
| Yes | 9 (5.6) | 2 (2.4) | 7 (9.1) | |
| Missing | 1 (.) | 0 (.) | 1 (.) | |
| Most recent RT-PCR PML-RAR alfa test, n (%) | .193 | |||
| Negative | 130 (96.3) | 68 (98.6) | 62 (93.9) | |
| Positive | 5 (3.7) | 1 (1.4) | 4 (6.1) | |
| Missing | 26 (.) | 14 (.) | 12 (.) | |
| Variables at APL diagnosis | ||||
| WBC count, ×109/L | .097 | |||
| Mean (SD) | 2.1 (2.2) | 2.4 (2.5) | 1.8 (1.8) | |
| Median (IQR) | 1.2 (0.8-2.3) | 1.4 (0.9-2.6) | 1.2 (0.7-1.8) | |
| Platelet count, ×109/L | .392 | |||
| Mean (SD) | 50.3 (45.2) | 53.9 (47.0) | 46.6 (43.2) | |
| Median (IQR) | 34.0 (18.0-64.0) | 36.5 (18.0-83.5) | 32.0 (18.0-58.0) | |
| Hemoglobin count, g/dL | .553 | |||
| Mean (SD) | 9.5 (2.1) | 9.7 (2.1) | 9.4 (2.1) | |
| Median (IQR) | 9.2 (8.3-11.0) | 9.2 (8.5-11.1) | 9.2 (8.0-11.0) | |
| Risk level, n (%) | .334 | |||
| Low | 68 (43.3) | 38 (47.5) | 30 (39.0) | |
| Intermediate | 89 (56.7) | 42 (52.5) | 47 (61.0) | |
| Missing | 4 (.) | 3 (.) | 1 (.) |
RT-PCR, reverse transcriptase polymerase chain reaction; SD, standard deviation; WBC, white blood cell.
Main characteristics of patients with APL enrolled in this follow-up study compared with those who could not be enrolled for any reason
| Variables at APL diagnosis . | Patients with APL analyzed in current study (n = 161) . | Patients with APL not enrolled in this study (n = 70) . | P value . |
|---|---|---|---|
| Age at diagnosis, y | .075 | ||
| Mean (SD) | 46.4 (14.4) | 42.6 (14.8) | |
| Median (IQR) | 47.0 (36.7-57.7) | 41.9 (29.4-55.7) | |
| Sex, n (%) | 1 | ||
| Male | 79 (49.1) | 34 (48.6) | |
| Female | 82 (50.9) | 36 (51.4) | |
| Randomization arm, n (%) | .320 | ||
| ATRA-ATO | 83 (51.5) | 31 (44.3) | |
| ATRA chemotherapy | 78 (48.5) | 39 (55.7) | |
| WBC count, ×109/L) | .059 | ||
| Mean (SD) | 2.1 (2.2) | 2.4 (2.1) | |
| Median (IQR) | 1.2 (0.8-2.3) | 1.7 (1.0-3.0) | |
| Platelet count, ×109/L) | .705 | ||
| Mean (SD) | 50.3 (45.2) | 46.5 (41.6) | |
| Median (IQR) | 34.0 (18.0-64.0) | 32.0 (19.0-53.0) | |
| Hemoglobin level, g/dL | .552 | ||
| Mean (SD) | 9.5 (2.1) | 9.3 (2.0) | |
| Median (IQR) | 9.2 (8.3-11.0) | 9.2 (8.0-11.1) | |
| Risk level, n (%) | 1 | ||
| Low | 68 (43.3) | 30 (42.9) | |
| Intermediate | 89 (56.7) | 40 (57.1) | |
| Missing | 4 (.) | 0 (.) |
| Variables at APL diagnosis . | Patients with APL analyzed in current study (n = 161) . | Patients with APL not enrolled in this study (n = 70) . | P value . |
|---|---|---|---|
| Age at diagnosis, y | .075 | ||
| Mean (SD) | 46.4 (14.4) | 42.6 (14.8) | |
| Median (IQR) | 47.0 (36.7-57.7) | 41.9 (29.4-55.7) | |
| Sex, n (%) | 1 | ||
| Male | 79 (49.1) | 34 (48.6) | |
| Female | 82 (50.9) | 36 (51.4) | |
| Randomization arm, n (%) | .320 | ||
| ATRA-ATO | 83 (51.5) | 31 (44.3) | |
| ATRA chemotherapy | 78 (48.5) | 39 (55.7) | |
| WBC count, ×109/L) | .059 | ||
| Mean (SD) | 2.1 (2.2) | 2.4 (2.1) | |
| Median (IQR) | 1.2 (0.8-2.3) | 1.7 (1.0-3.0) | |
| Platelet count, ×109/L) | .705 | ||
| Mean (SD) | 50.3 (45.2) | 46.5 (41.6) | |
| Median (IQR) | 34.0 (18.0-64.0) | 32.0 (19.0-53.0) | |
| Hemoglobin level, g/dL | .552 | ||
| Mean (SD) | 9.5 (2.1) | 9.3 (2.0) | |
| Median (IQR) | 9.2 (8.3-11.0) | 9.2 (8.0-11.1) | |
| Risk level, n (%) | 1 | ||
| Low | 68 (43.3) | 30 (42.9) | |
| Intermediate | 89 (56.7) | 40 (57.1) | |
| Missing | 4 (.) | 0 (.) |
HRQoL and chemotherapy-induced peripheral neuropathy differences between treatment groups
The results of the 3 HRQoL main scales indicated a statistically and clinically meaningful difference, favoring patients treated with ATRA-ATO for role functioning (Δ = 8.4; 95% confidence interval [CI], 0.5 to 16.3; P = .037). With regard to the other 2 main scales, cognitive functioning (Δ = 4.9; 95% CI, −3.6 to 13.4; P = .257), and fatigue (Δ = −5.4; 95% CI, −14.3 to 3.5; P = .235) also showed clinically relevant (albeit not statistically significant) differences, favoring patients treated with ATRA-ATO.
With regard to the remaining HRQoL scales, it was found that patients treated with ATRA-ATO also reported a clinically meaningful lower severity of dyspnea (Δ = −8.5; 95% CI, −16.4 to −0.7) than patients treated with ATRA chemotherapy. Other clinically relevant differences favoring patients treated with ATRA-ATO were observed for global QoL (Δ = 6.1; 95% CI, −1.4 to 13.5), physical functioning (Δ = 5.9; 95% CI, −0.2 to 12.0), and pain (Δ = −8.2, 95% CI, −17.1 to 0.7) (Figure 1).
Adjusted mean differences in HRQoL profile by the EORTC QLQ-C30 questionnaire between patients with APL previously treated with ATRA-ATO vs ATRA chemotherapy. The figure represents differences in mean scores and corresponding 95% CIs, adjusted for time since protocol completion, of functional and global QoL scales (A) and symptom scales (B) from the EORTC QLQ-C30 questionnaire between long-term APL survivors previously treated with ATRA plus arsenic trioxide or ATRA plus chemotherapy. For descriptive purposes, the mean difference scores and corresponding 95% CIs of the symptom scales were multiplied by −1. Positive differences in functional and symptom scales indicate better outcomes in the ATRA plus arsenic trioxide arm than in the ATRA plus chemotherapy arm. A red circle indicates a clinically relevant difference.
Adjusted mean differences in HRQoL profile by the EORTC QLQ-C30 questionnaire between patients with APL previously treated with ATRA-ATO vs ATRA chemotherapy. The figure represents differences in mean scores and corresponding 95% CIs, adjusted for time since protocol completion, of functional and global QoL scales (A) and symptom scales (B) from the EORTC QLQ-C30 questionnaire between long-term APL survivors previously treated with ATRA plus arsenic trioxide or ATRA plus chemotherapy. For descriptive purposes, the mean difference scores and corresponding 95% CIs of the symptom scales were multiplied by −1. Positive differences in functional and symptom scales indicate better outcomes in the ATRA plus arsenic trioxide arm than in the ATRA plus chemotherapy arm. A red circle indicates a clinically relevant difference.
Other results of the EORTC QLQ-C30 and the EORTC QLQ-CIPN20 questionnaires were similar in the 2 treatment groups. Further details are reported in Figure 1 and supplemental Figure 3.
Differences in physical and mental health status between treatment groups
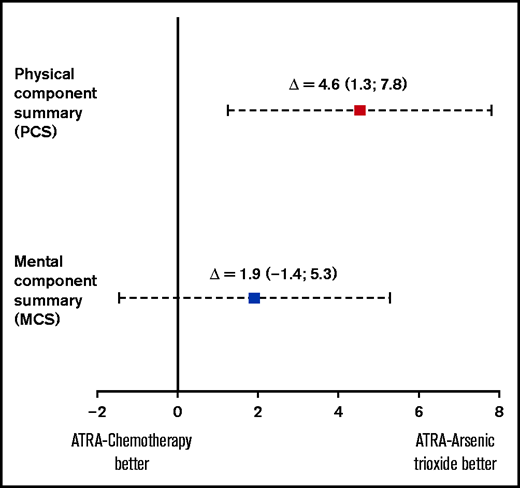
Clinically meaningful differences favoring patients treated with ATRA-ATO were observed for the following individual SF-36 scales: physical functioning (Δ = 13.2; 95% CI, 5.0 to 21.3), role physical (Δ = 12.9; 95% CI, −0.1 to 25.8), and role emotional (Δ = 11; 95% CI, −1.7 to 23.6) (Figure 2). Inspection of differences between groups in the PCS and MCS revealed a clinically meaningful difference for the PCS, favoring patients treated with ATRA-ATO (Δ = 4.6; 95% CI, 1.3 to 7.8). The difference between groups with regard to the MCS was not clinically relevant (Δ = 1.9; 95% CI, −1.4 to 5.3) (Figure 3).
Adjusted mean differences in physical and mental health-related domains by the SF-36 questionnaire between patients with APL previously treated with ATRA-ATO vs ATRA chemotherapy. The figure represents the differences in mean scores and corresponding 95% CIs, adjusted for time since protocol completion, of physical (A) and mental health-related scales (B) from the SF-36 questionnaire between long-term APL survivors previously treated with ATRA plus arsenic trioxide or ATRA plus chemotherapy. A positive difference in all scales indicates better outcomes in the ATRA plus arsenic trioxide arm than in the ATRA plus chemotherapy arm. A red circle indicates a clinically relevant difference.
Adjusted mean differences in physical and mental health-related domains by the SF-36 questionnaire between patients with APL previously treated with ATRA-ATO vs ATRA chemotherapy. The figure represents the differences in mean scores and corresponding 95% CIs, adjusted for time since protocol completion, of physical (A) and mental health-related scales (B) from the SF-36 questionnaire between long-term APL survivors previously treated with ATRA plus arsenic trioxide or ATRA plus chemotherapy. A positive difference in all scales indicates better outcomes in the ATRA plus arsenic trioxide arm than in the ATRA plus chemotherapy arm. A red circle indicates a clinically relevant difference.
Adjusted mean differences in SF-36 physical and mental health component scores between patients with APL previously treated with ATRA-ATO vs ATRA chemotherapy. The figure represents the differences in mean scores and corresponding 95% CIs, adjusted for time since protocol completion, of physical (A) and mental component summary scales (B) from the SF-36 questionnaire between long-term APL survivors previously treated with ATRA plus arsenic trioxide or ATRA plus chemotherapy. A positive difference in all scales indicates better outcomes in the ATRA plus arsenic trioxide arm than in the ATRA plus chemotherapy arm. A red square indicates a clinically relevant difference.
Adjusted mean differences in SF-36 physical and mental health component scores between patients with APL previously treated with ATRA-ATO vs ATRA chemotherapy. The figure represents the differences in mean scores and corresponding 95% CIs, adjusted for time since protocol completion, of physical (A) and mental component summary scales (B) from the SF-36 questionnaire between long-term APL survivors previously treated with ATRA plus arsenic trioxide or ATRA plus chemotherapy. A positive difference in all scales indicates better outcomes in the ATRA plus arsenic trioxide arm than in the ATRA plus chemotherapy arm. A red square indicates a clinically relevant difference.
Long-term comorbidities and health problems
At least 10% of the overall APL population reported problems with hypertension (32.9%), impaired vision (29.8%), back pain (29.2%), osteoarthritis (18%), depression (15.5%), allergies (14.9%), impaired hearing (14.3%), and thyroid disorders (10.6%).
Seventy-eight percent of patients in each group (ATRA-ATO and ATRA chemotherapy) reported at least 1 comorbid condition. Hypertension was the most frequent problem in both groups, being reported by 30.1% and 35.9% of patients treated with ATRA-ATO and ATRA chemotherapy, respectively. The prevalence of individual comorbidities and health problems was broadly similar between groups. Details are reported in Table 3.
Prevalence of long-term comorbidities and health problems in patients with APL, overall and by previous randomization group (ATRA-ATO vs ATRA chemotherapy)
| Variable . | Total (N = 161) n (%) . | ATRA-ATO (N = 83) n (%) . | ATRA chemotherapy (N = 78) n (%) . |
|---|---|---|---|
| Hypertension | 53 (32.9) | 25 (30.1) | 28 (35.9) |
| Impaired vision | 48 (29.8) | 20 (24.1) | 28 (35.9) |
| Back pain | 47 (29.2) | 25 (30.1) | 22 (28.2) |
| Osteoarthritis, degenerative arthritis | 29 (18.0) | 13 (15.7) | 16 (20.5) |
| Depression | 25 (15.5) | 12 (14.5) | 13 (16.7) |
| Allergies | 24 (14.9) | 11 (13.3) | 13 (16.7) |
| Impaired hearing | 23 (14.3) | 12 (14.5) | 11 (14.1) |
| Thyroid disorders | 17 (10.6) | 7 (8.4) | 10 (12.8) |
| Lung disease | 15 (9.3) | 7 (8.4) | 8 (10.3) |
| Rheumatoid arthritis | 14 (8.7) | 7 (8.4) | 7 (9.0) |
| Diabetes | 11 (6.8) | 4 (4.8) | 7 (9.0) |
| Cataract surgery | 11 (6.8) | 7 (8.4) | 4 (5.1) |
| Gut disease other than u lcer or stomach disease | 10 (6.2) | 4 (4.8) | 6 (7.7) |
| Ulcer or stomach disease | 9 (5.6) | 5 (6.0) | 4 (5.1) |
| Chronic skin disorders | 9 (5.6) | 6 (7.2) | 3 (3.9) |
| Anemia or other blood disease | 9 (5.6) | 3 (3.6) | 6 (7.7) |
| Congestive heart failure | 8 (5.0) | 6 (7.2) | 2 (2.6) |
| Chronic genitourinary diseases | 8 (5.0) | 3 (3.6) | 5 (6.4) |
| Impaired extremities | 7 (4.4) | 3 (3.6) | 4 (5.1) |
| Coronary heart disease | 6 (3.7) | 3 (3.6) | 3 (3.9) |
| Liver disease | 4 (2.5) | 2 (2.4) | 2 (2.6) |
| Hormonal disorders | 4 (2.5) | 0 (0) | 4 (5.1) |
| Kidney disease | 1 (0.6) | 1 (1.2) | 0 (0) |
| Variable . | Total (N = 161) n (%) . | ATRA-ATO (N = 83) n (%) . | ATRA chemotherapy (N = 78) n (%) . |
|---|---|---|---|
| Hypertension | 53 (32.9) | 25 (30.1) | 28 (35.9) |
| Impaired vision | 48 (29.8) | 20 (24.1) | 28 (35.9) |
| Back pain | 47 (29.2) | 25 (30.1) | 22 (28.2) |
| Osteoarthritis, degenerative arthritis | 29 (18.0) | 13 (15.7) | 16 (20.5) |
| Depression | 25 (15.5) | 12 (14.5) | 13 (16.7) |
| Allergies | 24 (14.9) | 11 (13.3) | 13 (16.7) |
| Impaired hearing | 23 (14.3) | 12 (14.5) | 11 (14.1) |
| Thyroid disorders | 17 (10.6) | 7 (8.4) | 10 (12.8) |
| Lung disease | 15 (9.3) | 7 (8.4) | 8 (10.3) |
| Rheumatoid arthritis | 14 (8.7) | 7 (8.4) | 7 (9.0) |
| Diabetes | 11 (6.8) | 4 (4.8) | 7 (9.0) |
| Cataract surgery | 11 (6.8) | 7 (8.4) | 4 (5.1) |
| Gut disease other than u lcer or stomach disease | 10 (6.2) | 4 (4.8) | 6 (7.7) |
| Ulcer or stomach disease | 9 (5.6) | 5 (6.0) | 4 (5.1) |
| Chronic skin disorders | 9 (5.6) | 6 (7.2) | 3 (3.9) |
| Anemia or other blood disease | 9 (5.6) | 3 (3.6) | 6 (7.7) |
| Congestive heart failure | 8 (5.0) | 6 (7.2) | 2 (2.6) |
| Chronic genitourinary diseases | 8 (5.0) | 3 (3.6) | 5 (6.4) |
| Impaired extremities | 7 (4.4) | 3 (3.6) | 4 (5.1) |
| Coronary heart disease | 6 (3.7) | 3 (3.6) | 3 (3.9) |
| Liver disease | 4 (2.5) | 2 (2.4) | 2 (2.6) |
| Hormonal disorders | 4 (2.5) | 0 (0) | 4 (5.1) |
| Kidney disease | 1 (0.6) | 1 (1.2) | 0 (0) |
Descriptive comparison of the physical and mental health status profiles of patients treated with ATRA-ATO with the general population
Adjusted mean score differences for the 8 physical and mental health-related SF-36 scales, between APL patients and matched subjects without cancer from the GP, are presented in Figure 4. The health status profile of patients with APL was similar to that of their peers from the general population, and a clinically meaningful better general health status perception (Δ = 11.4; 95% CI, 6.5 to 16.4) was also observed in patients with APL.
Adjusted mean differences in SF-36 scores between patients with APL previously treated with ATRA-ATO and the general population. Patients with APL and subjects from the general population had been previously matched by the propensity scores estimated on age and sex. *Clinically relevant difference.
Adjusted mean differences in SF-36 scores between patients with APL previously treated with ATRA-ATO and the general population. Patients with APL and subjects from the general population had been previously matched by the propensity scores estimated on age and sex. *Clinically relevant difference.
Discussion
We have shown that after a median time since diagnosis of 8 years, patients with APL treated with ATRA-ATO report fewer limitations in daily life activities (role functioning of the EORTC QLQ-C30) and better physical health status (PCS of the SF-36) than patients treated with ATRA and chemotherapy. Also, our additional descriptive analysis, indicated that the health status profile of patients with APL previously treated with ATRA-ATO, is broadly comparable with that of their peers, without cancer, in the general population.
Our result of a better role functioning as measured by the EORTC QLQ-C30 for patients treated with ATRA-ATO is partly corroborated by a previous RCT with a 2-year HRQoL follow-up.4 Burnett and colleagues4 analyzed 156 patients with APL (of whom 80 and 76 received ATRA-ATO and ATRA-idarubicin, respectively) using the EORTC QLQ-C30 and found a statistically significantly better role functioning for patients treated with ATRA-ATO.4 However, based on the negative results of their primary study outcome (ie, the global QoL scale), they concluded that no HRQoL improvement was seen for patients treated with ATRA-ATO. It is difficult to compare our results with their findings4 because they also included high-risk patients with APL, and their HRQoL follow-up was substantially shorter than in our study. Furthermore, patients treated with ATRA chemotherapy in the AML17 trial did not receive maintenance therapy, as our patients did according to the RCT treatment schema.6 Indeed, our findings of a clinically meaningfully worse physical condition and higher limitations in daily life activities for patients treated with ATRA chemotherapy may possibly be explained by their prolonged maintenance treatment.
Zhu and colleagues30 included an HRQoL assessment in a single-arm study of 112 patients with APL treated with ATRA-ATO with a 12-year follow-up and concluded that they reported a “good” quality of life. Notably, the authors reported a mean score on the global QoL scale of the EORTC QLQ-C30, which was very similar to that observed in our study for patients treated with ATRA-ATO (data not shown). However, this report was published in a Letter format, and very little information was provided on HRQoL methodology and outcomes, thereby hampering any further comparison with our results.30
An important consideration in interpreting our data is the route of ATO administration (ie, IV), which may have somehow mitigated its potential long-term HRQoL advantages over traditional chemotherapy. Although there were a number of clinically relevant better functional and symptom outcomes favoring patients treated with ATRA-ATO, these outcomes were often of small magnitude. Additionally, the absence of a prolonged maintenance therapy in the ATRA-ATO arm did not translate into evident better mental health outcomes for patients treated with ATRA-ATO. Therefore, whether more substantial HRQoL benefits may be obtained with oral formulations of ATO is an important research question to be elucidated in future studies.
In an effort to develop an oral powder capsule formulation of ATO (ie, ORH-2014) for the Western market, Ravandi and colleagues31 have recently shown that this is safe and effective, and the authors speculated that it can also improve patients’ HRQoL. An oral formulation of ATO is currently only available for the Chinese market, and a recent RCT phase 3 study has shown that this is not inferior to IV ATRA-ATO for the treatment of patients with nonhigh-risk APL.32 Some very preliminary data on the potential HRQoL advantages of oral ATO have been published in a brief research letter including 20 Chinese APL patients with a median follow-up of 14 months, which concluded that HRQoL was rated by patients as nearly normal.33
Considering the importance of collecting long-term data to better understand the long-term risk profile of frontline ATO therapy in patients with APL,18 we also examined the prevalence of late comorbidities and health problems and found no major difference between treatment groups. Despite previous data indicating a different toxicity profile during treatment, for example, with patients treated with ATRA-ATO reporting higher liver problems and QTc prolongation and patients treated with ATRA chemotherapy experiencing higher gastrointestinal toxicities and cardiac function abnormalities,6 our findings suggest that they do not translate into a different proportion of late health problems and comorbidities between the 2 groups. Additionally, we observed similar results in patient-reported peripheral neuropathy (as measured by the QLQ-CIPN20) between groups, despite a greater proportion of patients treated with ATRA-ATO reporting neurotoxicity (mainly consisting of reversible peripheral nerve neuropathy) during consolidation.6 The prevalence we observed for some key problems, such as hypertension, impaired vision, allergies, diabetes, and thyroid disorders, was similar to that reported by Messerer and colleagues in a cohort of patients with AML with a very similar median follow-up of that in our study.20
Our study has limitations. We did not include an HRQoL questionnaire specific for patients with AML/APL, thereby possibly limiting a more comprehensive evaluation of the impact of therapy. However, probably because of the historical lack of PRO research in AML, we note that the HRQoL measures specifically developed for patients with AML have only been published over the past few months.34,35 Given the known association between anthracyclines and cardiotoxicity,18 we also acknowledge that the addition of instrumental examinations of cardiac function could have helped to better understand the observed differences between groups in the reporting of dyspnea severity. Finally, the relatively low sample size precluded further analyses by specific patient subgroups, and we also note that our results should not be interpreted as confirmatory.
This study also has key strengths. Despite the challenges of including PROs in leukemia trials,36 we were able to document the first and largest long-term HRQoL comparative data on the impact of ATO therapy (ie, chemotherapy-free) vs a chemotherapy approach in patients with APL. Additionally, our sensitivity analysis on the characteristics of patients who could not be invited to participate in this follow-up study provides confidence in the generalizability of the study findings to the overall trial population. Finally, our patients were recruited across more than 50 centers from 2 countries, thereby enhancing the generalizability of the study results.
In conclusion, our results further support the use of IV ATRA-ATO as a first-line therapy in nonhigh-risk patients with APL by suggesting that they report a better long-term physical health status and fewer limitations in daily life activities than patients previously treated with standard chemotherapy. Our findings also suggest that, in the long term, the health status of patients with APL previously treated with ATRA-ATO may be comparable to that of the general population.
Acknowledgments
The authors are grateful to all patients who participated in this study and thank all local investigators and research staff of all participating centers within the GIMEMA, AMLSG, and SAL study groups. The authors are also grateful to Paola Mosconi from the Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Italy, for her support in getting access to the SF-36 Italian validation data.
Authorship
Contribution: F.E., U.P., and M.V. provided the concept and design; U.P., M.B., P.C., P.S., E.D.B., E.B., F.A., L.L., O.F., V.M., S.D., R.F.S., L.M., M.F., W.F., G.B., N.S.F., M.B., K.M., and M.T.V. provided study material or patients; F.E., U.P., M.B., F.C., P.C., P.S., E.D.B., E.B., F.A., L.L., O.F., V.M., S.D., R.F.S., L.M., M.F., W.F., G.B., N.S.F., M.B., K.M., and M.T.V. collected and assembled data; F.E., U.P., M.B., F.C., M.T.V., and M.V. undertook data analysis and interpretation; F.C. and F.E. provided statistical analysis; and all authors wrote the manuscript; provided final approval of the manuscript, and are accountable for all aspects of the work.
Conflict-of-interest disclosure: F.E. reports consultancy for Abbvie, Amgen, Janssen, Orsenix, and Takeda and a research grant (to his institution) from Amgen, outside the submitted work; he also reports research support from TEVA and Lundbeck (to his institution) during the conduct of the study. U.P. reports research support from TEVA. E.B. is a consultant for Amgen and Celgene, outside the submitted work. M.V. reports personal fees from Amgen, Millennium Pharmaceuticals Inc., Celgene, Janssen, Novartis, and Incyte, outside the submitted work.
Correspondence: Fabio Efficace, Health Outcomes Research Unit, Italian Group for Adult Hematologic Diseases (GIMEMA), GIMEMA Data Center, Via Benevento, 6, 00161 Rome, Italy; e-mail: f.efficace@gimema.it.
References
Author notes
For data sharing, contact the corresponding author: f.efficace@gimema.it.
The full-text version of this article contains a data supplement.