Key Points
Strong correlation of NGS-based MRD was observed between paired PB and BM aspirates.
MRD monitoring by blood appears to be an adequate alternative to frequent marrow aspirations in ALL patients receiving cellular therapies.
Abstract
Monitoring of measurable residual disease (MRD) is essential to the management of acute lymphoblastic leukemia (ALL) and is typically performed through repeated bone marrow (BM) assessments. Using a next-generation sequencing (NGS) MRD platform, we performed a prospective observational study evaluating the correlation between peripheral blood (PB) and BM MRD in adults with ALL receiving cellular therapies (hematopoietic cell transplantation [HCT] and chimeric antigen receptor T-cell [CAR-T] therapies). Among the study cohort (N = 69 patients; 126 paired PB/BM samples), we found strong correlation between PB and BM MRD (r = 0.87; P < .001), with a sensitivity and specificity of MRD detection in the PB of 87% and 90%, respectively, relative to MRD in the BM. MRD became detectable in the PB in 100% of patients who subsequently relapsed following HCT, with median time from MRD+ to clinical relapse of 90 days, and in 85% of patients who relapsed following CAR T, with median time from MRD+ to clinical relapse of 60 days. In adult patients with ALL undergoing cellular therapies, we demonstrate strong concordance between NGS-based MRD detected in the PB and BM. Monitoring of ALL MRD in the PB appears to be an adequate alternative to frequent invasive BM evaluations in this clinical setting.
Introduction
Measurable residual disease (MRD) in acute lymphoblastic leukemia (ALL) is a well-established prognostic marker across treatment modalities and therapeutic timepoints and can influence therapeutic decision making.1-4 Assessment of ALL MRD may be performed using multiparameter flow cytometry, allele-specific oligonucleotide polymerase chain reaction, or next-generation sequencing (NGS)-based assays of clonal immunoglobulin and/or T-cell receptor (TCR) loci.5 Although each modality has advantages and limitations, NGS is the most sensitive for ALL MRD detection in the bone marrow (BM) with a sensitivity in the marrow of 10−6,6 is commercially available in the United States and is increasingly used in clinical practice.
A limitation of current MRD methods is the need for repeated BM assessments. We hypothesized that NGS-based MRD detection using the peripheral blood (PB) may serve as a clinically acceptable, more convenient alternative to BM-based MRD assessment. We previously conducted a retrospective analysis of ALL MRD detection using an NGS-based assay in paired PB and BM samples and found general agreement between PB and BM MRD results.7 This current prospective, observational study expands our prior work evaluating the concordance between PB and BM MRD using NGS in a larger cohort of adults with ALL.
Methods
Consecutive patients ≥18 years with B- or T-ALL undergoing hematopoietic cell transplantation (HCT) or chimeric antigen receptor T cell (CAR T) at Stanford University between March 2018 and April 2020 were eligible. This study was approved by the Stanford institutional review board, and all participants provided written informed consent. MRD was performed on paired prospectively collected PB and BM samples at prespecified time points (supplemental Figure 1) and was conducted in real-time at Adaptive Biotechnologies using their clonoSEQ Assay.8 Generally, TCR rearrangements were assessed in patients with B-ALL only if B-cell rearrangements were not identified. Residual disease detected at any level was defined as MRD+; undetectable was considered MRD−. Clinical relapse was defined as the development of ≥5% leukemic blasts, extramedullary leukemia, or the administration of a new therapy for rising MRD.
The primary objective was to compare NGS-based MRD results in the PB and BM. Correlations between log10 values of paired PB/BM NGS results were evaluated using the Pearson correlation coefficient; correlation was evaluated among patients for all time points and in patient subsets of interest. Statistical analyses were performed using SAS version 9.4. L.M. and V.S. analyzed the data.
Results and discussion
Sixty-nine patients were enrolled; 7 (10%) were excluded from analysis because they did not undergo planned therapy (n = 3) or did not have a trackable clonal sequence for NGS MRD assessment (n = 4). Patient and disease characteristics of the study cohort are detailed in supplemental Table 1. Pretreatment clonal rearrangements differed, as expected, between T- and B-ALL: TCR rearrangements were detected in all patients with T-ALL (N = 8) and in 11% of patients with B-ALL; the remainder of patients with B-ALL had immunoglobulin H and/or immunoglobulin κ/λ clones (supplemental Table 2).
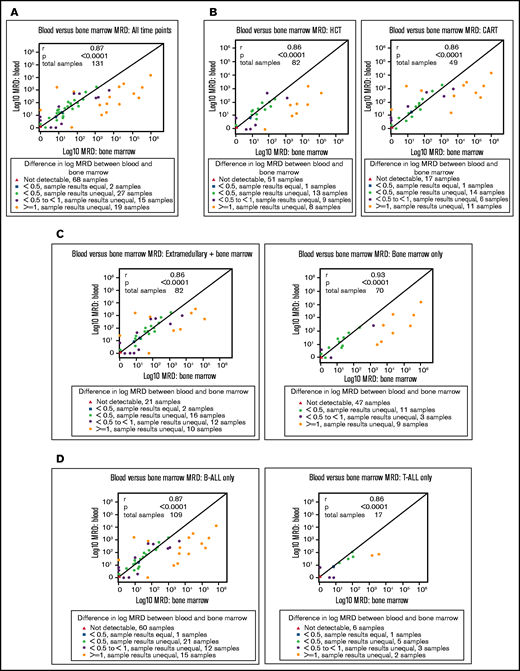
One hundred and twenty-six paired PB/BM samples were obtained for NGS MRD assessment (median, 2; interquartile ratio [IQR], 1-3; paired samples per patient). Among all paired samples, NGS MRD from the PB and BM was highly correlated (r = 0.87; P < .0001) (Figure 1A). Relative to marrow MRD by NGS, the sensitivity, specificity, and positive and negative predictive value of peripheral blood MRD by NGS were: 87% (95% confidence interval [CI], 75-95), 90% (95% CI, 81-96), 87% (95% CI, 76-93), and 90% (95% CI, 82-95), respectively. The PB/BM NGS MRD results were discordant in 14 paired samples (12%): 7 pairs (6%) were MRD+ in PB/MRD− in BM and 7 pairs (6%) were MRD− in PB/MRD+ in BM. We found similar PB/BM MRD correlations among paired samples from HCT (r = 0.85; P < .001) and CAR-T patients (r = 0.87; P < .001) (Figure 1B) and among patients with (r = 0.84; P < .001) and without extramedullary leukemia (r = 0.93; P < .001) (Figure 1C).
Scatterplots and Pearson correlation coefficients of paired PB and BM NGS-based MRD results. (A) Evaluable study cohort (N = 62) including 126 paired PB and BM NGS-based MRD results. (B) Patients undergoing HCT (N = 43) including 81 paired PB and BM results and patients undergoing CAR T (N = 17), including 45 paired PB and BM MRD results. (C) Patients with extramedullary (EM) involvement at any time during leukemia history (N = 27) including 60 paired PB and BM MRD results and patients with only BM involvement (N = 33), including 66 paired PB and BM MRD results.
Scatterplots and Pearson correlation coefficients of paired PB and BM NGS-based MRD results. (A) Evaluable study cohort (N = 62) including 126 paired PB and BM NGS-based MRD results. (B) Patients undergoing HCT (N = 43) including 81 paired PB and BM results and patients undergoing CAR T (N = 17), including 45 paired PB and BM MRD results. (C) Patients with extramedullary (EM) involvement at any time during leukemia history (N = 27) including 60 paired PB and BM MRD results and patients with only BM involvement (N = 33), including 66 paired PB and BM MRD results.
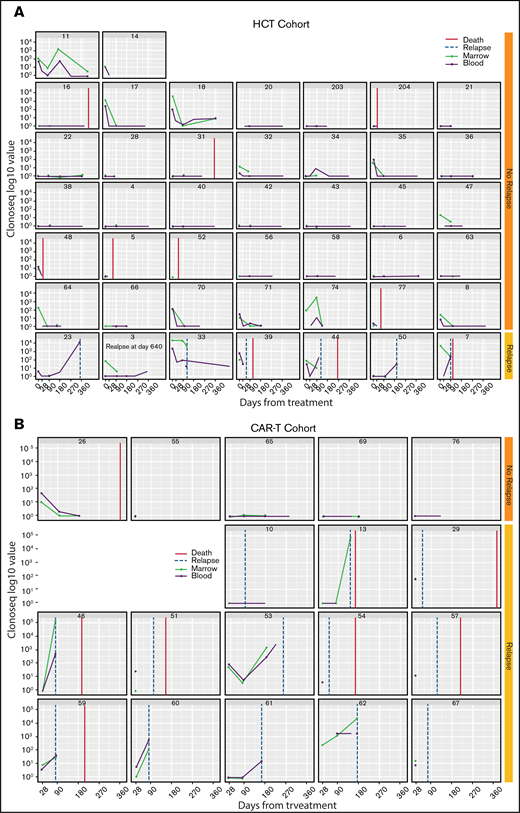
With median follow-up of 341 days (IQR, 196-560), 7 (16%) HCT and 13 (72%) patients with CAR T experienced clinical relapse (Figure 2). All patients who relapsed after HCT had detectable NGS MRD in the PB post-HCT, with median time from first MRD+ result post-HCT to clinical relapse of 90 days (IQR, 59-320). Clinical relapse was averted in 2 patients (Figure 2; patients 74 and 11) by successful MRD-driven withdrawal of immunosuppression without further intervention. Among patients who relapsed following CAR-T, 85% had detectable NGS MRD in the PB post–CAR T, with median time from first MRD+ result post–CAR T to clinical relapse of 60 days (IQR, 50-139).
Individual patient plots demonstrating NGS-based MRD results over time from the PB and BM. Patients receiving HCT (N = 44) (A) and patients receiving CAR T (N = 18) (B). Each dot represents an MRD result; blue represents marrow MRD and green represents peripheral blood MRD. Patients who experienced clinical relapse are noted in the rows next to the yellow relapse indicator; patients who did not experience clinical relapse are noted in the rows next to the orange relapse indicator. Black vertical lines represent time of death.
Individual patient plots demonstrating NGS-based MRD results over time from the PB and BM. Patients receiving HCT (N = 44) (A) and patients receiving CAR T (N = 18) (B). Each dot represents an MRD result; blue represents marrow MRD and green represents peripheral blood MRD. Patients who experienced clinical relapse are noted in the rows next to the yellow relapse indicator; patients who did not experience clinical relapse are noted in the rows next to the orange relapse indicator. Black vertical lines represent time of death.
Assessment of MRD is an essential component of ALL management.2,9,10 Adult ALL routinely undergo MRD evaluations from BM; patients with detectable MRD may undergo frequent repeat BM evaluations, whereas those who achieve MRD− status are often monitored via routine blood counts and clinical history. The use of PB as a source for MRD monitoring in ALL could increase access to MRD testing in patients with ALL, improve patient satisfaction by reducing the need for repeated invasive BM procedures, and facilitate serial monitoring in certain high-risk populations.
In this prospective evaluation of ALL cellular therapy recipients, we found strong concordance between NGS-based MRD of the PB and BM. Further, among 126 paired samples, an equally small number (6%) were MRD+ in the BM and MRD− in the PB, as were MRD+ in the PB and MRD− in the BM (6%). Our findings suggest that PB is an acceptable alternative to BM for NGS-based MRD monitoring following HCT and/or CAR T-cell therapies.
This prospective study is timely because recent retrospective reports demonstrated that PB may function as an adequate substitute for BM in detecting myeloid leukemias at diagnosis (and possibly for MRD) using either flow cytometry or NGS, although blast count and specific clonal mutations may determine utility of PB as an isolated diagnostic tool.11,12 The use of PB sampling for circulating tumor DNA is also of interest in monitoring for residual lymphoma and solid tumors.13-15 Our study population included adults with ALL undergoing cellular therapies with a curative intent, where BM MRD monitoring is performed as a standard of care before and after treatment. Because the attributes of diagnostic assays in leukemia are typically not affected by treatment modality, we expect our results to be generalizable across ALL patients, yet additional confirmatory studies should be undertaken to validate these findings in patients not undergoing cellular therapies. Interestingly, a report by Kotrova and colleagues demonstrated that using real-time quantitative polymerase chain reaction-based MRD, concordance between PB and BM MRD appears tighter in T-ALL than in B-ALL, and suggested that this may be a result of the differential site of leukemia origin (marrow vs thymus).16 Regardless, given the critical and proven role of MRD in ALL, it is incumbent upon us to develop and use less invasive, more accessible, cost-effective methods of disease monitoring.
Although it is routine practice to repeat MRD evaluations in patients with MRD+, patients without residual disease are often followed with blood counts and symptom reporting. In our study, we unexpectedly found disproportionately low and high rates of clinical relapse in the HCT and CAR-T recipients, respectively, thus limiting our power to perform formal statistical analyses regarding the prognostic effects of PB MRD on clinical relapse and survival. However, we found that among the HCT and CAR-T patients who did relapse, MRD was detectable in the peripheral blood after therapy a median of 2 to 3 months before clinical relapse. Further, NGS-based MRD monitoring of the PB following HCT was clinically actionable, enabling immunosuppression withdrawal and subsequent MRD clearance, thus averting clinical relapse.
In summary, we demonstrate that using an NGS-based assay, PB and BM MRD results are highly concordant. In adult patients with ALL undergoing cellular therapies, MRD monitoring of the PB appears to be an adequate alternative to frequent BM aspirations.
Acknowledgments
The authors acknowledge Adaptive Biotechnologies for providing funding support for this study.
Authorship
Contribution: L.M. designed research, performed research, analyzed data, and wrote the paper; D.M. designed research, enrolled subjects, and edited the paper; V.S. designed research, analyzed data, and edited the paper; C.C., I.Y., and S.B. performed research and edited the paper; and J.S., S.A., M.J.F., L.J.J., R.L., E.H.M., R.S.N., A.R.R., S.S., P.S., J.A.S., W.K.W, M.L., and H.T.V. enrolled subjects and edited the paper.
Conflict-of-interest disclosure: L.M. reports research funding from Adaptive Biotechnologies, Servier, Astellas, and Jasper and consulting for Amgen and Pfizer. E.H.M. reports research funding from Orca Bio. R.S.N. reports research funding from Amgen, Kuur, and Magenta; is an equity holder in the public company Magenta; is an equity holder in the private companies BioEclipse and Biosource; and receives honoraria from Uptodate. A.R.R. reports research funding from Pharmcyclics. S.S. reports consultancy for Janssen. P.S. reports research funding from Orca Bio. J.A.S. reports being a current equity holder in private company and membership on an entity's Board of Directors or advisory committees with Jasper. M.L. reports being a member on board or advisory committee for Adaptive, Caelum, Celgene, GSK, Janssen, and Jazz and receiving honoraria from Pfizer. D.B.M. reports consultancies for Kite, Juno-Celgene-GMS, Novartis, Pharmacyclics, and Janssen; research funding from Adaptive Biotechnologies, Juno-Celgene-BMS, Allogene, Novartis, Pharmacyclics, and Miltenyi; membership on board or advisory committees with Kite; travel support from Adaptive, Kite, June-Celgene-BMS, Novartis, Pharmacyclics, and Janssen; and patent and royalty with Pharmacyclics.
Correspondence: Lori Muffly, Stanford University, 300 Pasteur Dr, H0144, Stanford, CA 94305; e-mail: lmuffly@stanford.edu.
References
Author notes
Data sharing statement: For deidentified data requests, please contact: lmuffly@stanford.edu.
The full-text version of this article contains a data supplement.