Key Points
Patients with MM after CP have inferior survival compared with patients with MM after BP.
Patients with MM tend to present symptoms at relapse similar to those at diagnosis.
Abstract
Almost all patients with multiple myeloma (MM) eventually relapse, either asymptomatically or with end-organ damage. However, it remains unclear whether initiating therapy at the time of biochemical progression (BP) improves the outcomes compared with initiating therapy at the clinical progression (CP) stage. Here, we retrospectively assessed 1347 patients with relapsed MM. Most progressions were BP (60.4%); 39.6% had CP. The most prevalent symptoms at relapse were new or evolving bone disease (80.9%), anemia (38.0%), and renal failure (12.7%). Patients with BP had longer median time from second-line treatment to the next treatment compared with patients who had CP (17.0 vs 9.6 months; P < .001) as well as longer median overall survival from first relapse (59.4 vs 26.2 months; P < .001). Male sex (odds ratio [OR], 1.49; 95% confidence interval [CI], 1.02-2.18; P = .04), plasma cell labeling index ≥2% (OR, 1.58; 95% CI, 1.02-2.45; P = .04), and extramedullary disease at diagnosis (OR, 1.84; 95% CI, 1.08-3.13; P = .03) were associated with higher risk of CP, whereas very good partial remission or better had decreased risk of CP (OR, 0.62; 95% CI, 0.43-0.91; P = .02). To conclude, patients with CP have inferior postprogression outcomes compared with patients who have BP. Patients with deeper response to first-line therapy are less likely to develop CP. The presence of a specific CRAB (C, hypercalcemia; R, renal failure; A, anemia; B, bone disease) symptom at diagnosis predicts for the development of similar CRAB symptoms at relapse.
Introduction
Multiple myeloma (MM) is the second most common hematologic malignancy, originating from clonal plasma cells.1 Even with current approaches, MM remains incurable, and eventually nearly all patients relapse after first-line therapy. At relapse, patients may present with increasing serum and/or urine monoclonal protein alone (biochemical progression [BP]) or may present with clinical features suggestive of progression including CRAB (C, hypercalcemia; R, renal failure; A, anemia; B, bone disease) symptoms; more specifically, those symptoms are hypercalcemia, renal insufficiency, anemia that cannot be attributed to another cause, new or evolving bone lesions, and/or soft tissue plasmacytomas, but they may not meet the criteria for BP.2 BP precedes clinical progression (CP) by a median of 5.1 months (range, 2-24 months).3 Approximately one quarter of patients, even when they are closely monitored during complete remission (CR), can develop unanticipated CP with end organ damage.4 Conversely, some patients present with indolent, asymptomatic BP that might not be treated for a long time.2 Recognizing and understanding different progression patterns is crucial not only to better understand the disease biology but also for counseling the patient and implementing salvage therapy, especially in the BP phase.
The true prevalence of different patterns of progression and its clinical significance to the outcome is not well understood, because clinical trial data from patients’ relapse characteristics vary from study to study on account of different enrollment criteria.5,6 Previously published data suggested that the clinical features at relapse occur in ∼45% of the studied populations, and some data suggested that postprogression survival tends to be worse in patients with CP than in those with BP.3,4,7-9 However, most of the studies were based on data from trials with selected treatment options or the study included a small group of patients.
To better understand different progression patterns and their impact on survival outcomes, we designed a retrospective study of patients with relapsed MM from our institutional database. The primary objective was to describe the prevalence and outcome of BP vs CP in a real-world setting as well as the occurrence of different CRAB symptoms at diagnosis and at relapse and their relationship. We also aimed to determine whether any of the baseline characteristics at diagnosis could be predictive of the relapse pattern.
Methods
Case selection
We retrospectively assessed patients with relapsed MM who were observed at Mayo Clinic Rochester and who were initially diagnosed between February 15, 2001, and December 15, 2018. The cohort included patients age 18 years or older diagnosed with MM with at least 1 disease relapse that required an additional line of treatment and who had a known pattern of relapse. Exclusion criteria included continued first remission at most recent follow-up or insufficient data to determine the pattern of relapse.
To be classified in the CP group, patients were required to have evidence of CRAB symptoms according to International Myeloma Working Group (IMWG; increase ≥50% in size or new plasmacytomas or bone lesions, hypercalcemia ≥11.5 mg/dL, decrease in hemoglobin ≥2 g/dL or to ≥10 g/dL, increase in serum creatinine ≥2 mg/dL, or hyperviscosity).10 For this study, aggressive relapse was considered when the patient presented with new extramedullary disease (EMD), plasma cell leukemia (PCL), or hyperviscosity requiring plasmapheresis at the time of relapse. EMD was defined as new soft tissue plasmacytomas diagnosed at the time of relapse, either contiguous or noncontiguous with a bony structure. Bone lesions were detected using a positron emission tomography–computed tomography (PET-CT) scan, magnetic resonance imaging, CT scan or skeletal survey. BP was defined as an increase in serum or urine monoclonal protein leading to initiation of a new line of therapy without meeting criteria for CP. In our institution, there is a general consensus for starting treatment according to IMWG recommendations (CRAB symptoms or significant increase in monoclonal protein if the patient remains asymptomatic); however, the timing of second-line treatment might have been influenced to some extent by specific clinical context and patient preferences. Patients who met criteria for both BP and CP were included in the CP group.
We collected clinical and laboratory data at diagnosis and data on treatment regimens, progression, second progression, and overall survival (OS). Disease response was assessed using IMWG criteria and included CR, very good partial response (VGPR), partial response, stable disease, and progressive disease.11 OS was defined as the time from diagnosis or first progression to last follow-up or death, as required for the specific analysis. Time to next treatment (TTNT) was defined as the time between initiation of second- and third-line therapy, and this variable was available for 1239 patients. Patients who had not progressed to a subsequent line of therapy were censored at the date of last follow-up or at death. High-risk fluorescence in situ hybridization (FISH) has been defined as the presence of deletion 17p/TP53 mutation and/or translocation t(4;14), t(14;16), or t(14;20).12 Immunomodulatory drugs (IMiDs) include thalidomide, lenalidomide, and pomalidomide; proteasome inhibitors (PIs) include bortezomib, carfilzomib, and ixazomib. Novel agents were defined as lenalidomide, pomalidomide, bortezomib, next-generation PIs, and daratumumab. All patients authorized use of their medical record data for research.13 The study was approved by the Mayo Clinic Institutional Review Board and was conducted in accordance with the Declaration of Helsinki.
Statistical analysis
Data are expressed as mean (± standard deviation) or median (interquartile range) as appropriate. The Shapiro-Wilk test was used to assess conformity with a normal distribution. The continuous variables were compared between 2 groups by using Student t test for independent groups for mean values and Mann-Whitney U test for distribution. Categorical variables were analyzed using the χ2 test or Fisher’s exact test as appropriate. For the survival analysis, the Kaplan-Meier method was used to generate survival curves, which were then compared using the log-rank test. The median follow-up was calculated by using the reverse Kaplan-Meier method. Cox proportional hazards regression was used to fit univariable and multivariable-adjusted survival models, the results of which are reported as hazard ratios with 95% confidence intervals (CIs). A P value of ≤.1 in a simple logistic regression model was used as the entry criterion for the multivariable models. Odds ratios in multivariable models were adjusted for age and sex. Two-sided P values <.05 were considered statistically significant. Statistical analysis was performed with STATISTICA 12.0 (StatSoft, Tulsa, OK).
Results
Baseline characteristics
Patients’ baseline characteristics are presented in Table 1. Overall, 1347 patients were included in the final analysis. Median age at time of diagnosis was 62.9 years, and 59.6% of the patients were males. Median age at relapse was 65.2 years. The median time from diagnosis to first relapse was 22.8 months and was shorter by a median of 2.9 months in the CP group compared with the BP group. Except for stage from the International Staging System (ISS), patients in the CP group were more likely to have high-risk features at MM diagnosis, including high-risk FISH, elevated lactate dehydrogenase, and EMD. Patients in the CP group more often had non-secretory disease and hypercalcemia at baseline compared with patients in the BP group.
More than 82% of patients were treated with novel agents, including more than 21% of patients who were exposed to both PI- and IMiD-based therapy (supplemental Table 1). Patients with BP were more often treated with novel agents (85.4% vs 77.7%) and more often received lenalidomide-based maintenance treatment (15.6% vs 10.7%) compared with patients in the CP group. Almost half the studied population underwent first-line autologous stem cell transplantation (ASCT), which was more often performed in the BP group than in the CP group (50.8% vs 42.9%). Regarding response to treatment, patients in the BP group achieved VGPR or better to the first-line therapy more often than those in the CP group (59.9% vs 52.9%), but the percentage of patients who achieved CR was similar between the groups. Relapse on either primary therapy or maintenance therapy was noted in more than 42% of patients and was more prevalent in the CP group than in the BP group (45.7% vs 39.9%). After relapse, 40.3% of patients were treated with IMiD-based therapy, 27.7% with a PI-based regimen, and 22.7% with PI plus IMiD–based treatment. More patients in the BP group received IMiD-based therapy compared with patients in the CP group (42.8% vs 36.5%), whereas more patients in the CP group received PI plus IMID–based therapy compared with patients in the BP group (26.0% vs 20.6%). Almost 15% of patients underwent ASCT during second remission; there was no significant difference between the BP and CP groups.
Patterns of progression
Overall, 813 patients (60.4%) experienced BP, and 534 (39.6%) had CP, including 94 patients (6.9%) with an aggressive form of relapse (Table 2). Nearly 60% of patients were diagnosed with relapsed MM during or after 2013, and the remaining patients were diagnosed with relapse between 2004 and 2012. Among patients with CP, different CRAB symptoms occurred at the time of relapse, with the most prevalent being new or evolving bone disease (80.9%), followed by anemia (38.0%), and renal failure (12.7%). Hypercalcemia occurred in 6.6% of patients with CP at the time of relapse. Seventy-two patients (13.5%) presented with >1 of the CRAB symptoms at relapse.
Interestingly, patients with a specific CRAB symptom at diagnosis tended to relapse with the same symptom (eg, patients with hypercalcemia at diagnosis had higher chances of presenting with hypercalcemia at first relapse compared with patients who did not have hypercalcemia at diagnosis; Table 3). Moreover, patients with anemia at diagnosis had a higher prevalence of renal insufficiency but a lower likelihood of new bone disease at first relapse, and patients with bone disease at diagnosis had lower prevalence of renal insufficiency and anemia at first relapse.
Survival
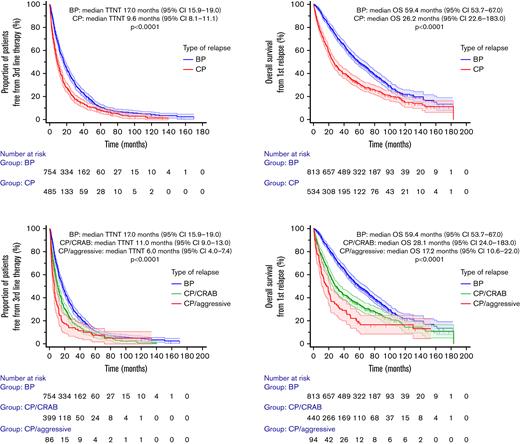
The median follow-up was 10.7 years (95% CI, 10.1-11.2 years). The median OS from diagnosis was 76.0 months (95% CI, 70.6-81.0 months); median OS from diagnosis for the CP group was 56.1 months (95% CI, 48.2-62.9 months) and for the BP group, it was 93.4 months (95% CI, 85.3-103.2 months; P < .001). For the whole group, the median TTNT from second-line therapy was 13.7 months (95% CI, 12.4-15.3 months), and median OS from first relapse was 46.6 months (95% CI, 42.9-183.0 months); the Kaplan-Meier curves are shown in Figure 1. Patients with CP had shorter median TTNT from second-line therapy compared with patients who had BP (9.6 vs 17.0 months; P < .001) as well as shorter median OS from first relapse (26.2 vs 59.4 months; P < .001). Among patients with CP, those presenting with aggressive vs CRAB features at relapse had a significantly shorter median TTNT from second-line therapy (6.0 vs 11.0 months; P < .001) and OS from first relapse (17.2 vs 28.1 months; P < .001).
TTNT from 2nd line treatment and OS from 1st relapse estimates in 1347 treated patients with MM stratified by pattern of relapse into BP and CP or into biochemical progression and CP with CRAB symptoms and aggressive form of CP (CP/aggressive). CI, confidence interval.
TTNT from 2nd line treatment and OS from 1st relapse estimates in 1347 treated patients with MM stratified by pattern of relapse into BP and CP or into biochemical progression and CP with CRAB symptoms and aggressive form of CP (CP/aggressive). CI, confidence interval.
The differences in survival between the BP and CP groups were also present after excluding patients with the non-secretory type of disease. In this subgroup of 1300 patients, the TTNT from second-line therapy was 17.0 months for the BP group and 9.6 months for the CP group (P < .001), whereas OS from first relapse was 59.2 months for the BP group and 26.2 months for the CP group (P < .001).
By using a multivariable-adjusted Cox proportional hazards model, CP (vs BP) was a predictor of shorter TTNT from the start of second-line therapy, along with ISS stage III, high-risk FISH at diagnosis, and relapse while receiving primary or maintenance treatment, whereas the use of first-line ASCT was a predictor of longer TTNT from the start of second-line therapy (Table 4). CP was also a predictor of shorter OS from first relapse, along with age younger than 65 years, male sex, ISS stage III, high-risk FISH at diagnosis, EMD at diagnosis, and relapse while receiving primary or maintenance treatment.
Factors associated with CP
On multivariable logistic regression models, several parameters were associated with increased risk of developing CP (Table 5). Male sex, PCL index ≥2%, and EMD at diagnosis were associated with a higher risk of CP, whereas achieving VGPR or better after first-line treatment was associated with a decreased risk of CP.
Discussion
This study compares different patterns of first relapse in a large group of patients with MM who were treated in a real-world setting. CP accounted for almost 40% of progressions, with new bone disease and anemia being the most common presentations. Relapse with clinical features predisposes to a worse OS and postprogression survival than BP, as expected. Patients with male sex, PCL index ≥2%, and EMD at diagnosis were at higher risk of developing CP, whereas patients who achieved deeper response to first-line treatment were at lower risk of developing CP. Finally, the presence of CRAB symptoms at diagnosis increased the risk of developing the same CRAB symptom at first relapse. Patients with aggressive relapse—PCL, EMD, or hyperviscosity requiring plasmapheresis—exhibit substantially worse postprogression survival compared with the rest of the studied group, which means that this group of patients with MM had a high need for novel, more effective therapies.
Several previous studies have been focusing on the prevalence and prognostic significance of different relapse patterns. Such studies included mostly patients treated with older agents and after ASCT, and the landscape of relapse patterns was heterogenous.14-16 Based on a newer post hoc analysis from MM-020 and MM-015 trials, Rosenberg et al8 have shown that the prevalence of CRAB symptoms at relapse reached almost 44% of the studied population (n = 1243) and was associated with worse post-progression progression-free survival (PFS) and OS (median OS from first relapse for the CP group was 23.2 months). Nonetheless, the study population was limited to patients who were ineligible for transplantation and were treated with IMiD-based therapies only (ie, patients were PI-naïve). In a Spanish study by Fernández de Larrea et al9 on 211 patients who underwent ASCT, about half had asymptomatic relapse, and they had longer OS (median OS, 6.5 years) than patients with symptomatic relapse (median OS, 4.2 years). Lopez et al3 studied different patterns of relapse in a smaller group of elderly patients (n = 145) from the GEM05MAS65 trial (patients who were ineligible for transplantation were treated with bortezomib plus prednisone plus either melphalan or thalidomide).
It has been shown that clinical and aggressive relapse (severe renal insufficiency, PCL, EMD) were the most common types of relapse (57% and 22%, respectively). The more aggressive type of relapse had the worst postprogression survival; median OS in the CP group was 18.1 months, and median OS in the aggressive group was 7.6 months. Chakraborty et al7 reported data from standard clinical practice on 252 patients. Most of them received novel agents, 26% underwent ASCT, and 47% experienced CP. Patients with CP without EMD exhibited median postprogression OS of 19.2 months, and patients with CP with EMD had a post-progression OS of 10.2 months. In another small, real-world study by Katodritou et al,17 the efficacy of lenalidomide-dexamethasone as second-line treatment was evaluated; 32% of 207 patients had CP, and patients treated during CP had shorter postprogression PFS than patients with BP. Of note, a sub-analysis of the Endeavor study showed that the stage of implementing treatment for relapsed MM (asymptomatic vs symptomatic) also influences the results, because patients with asymptomatic relapse had better PFS and OS.18
In comparison with the previously mentioned studies, our study showed that the prevalence of CP was slightly lower (39.6%), and the postprogression survivals were better (median OS, 28.1 months for patients with CP who had CRAB symptoms; median OS for patients with CP who had aggressive relapse was 16.6 months). The latter might be explained by lower median age in our study and also by the fact that in our population, more patients had been treated with a combination of novel agents and first-line ASCT (50%). Therefore, our data provide important input on the role of different relapse characteristics based on a population of patients more reflective of a real-world standard patient with MM. The information on pattern of relapse should be an important parameter in stratifying patients at relapse and should be included in the randomization and analysis process in clinical trials, especially trials that include patients with MM who have relapsed.
In our study, patients relapsed mostly with new bone disease, followed by anemia and renal insufficiency; hypercalcemia was the least frequent symptom. Similar results were obtained by Chakraborty et al7 and Fernández de Larrea et al.9 On the contrary, in the study by Rosenberg et al,8 the most common CRAB symptoms at relapse were anemia and renal insufficiency; only 15% had new bone disease. Such differences might originate from a very specific design aspect of the trials included in the analysis. Nonetheless, the differences between real-world data and data derived from clinical trials are significant, and they need to be taken into account when incorporating clinical trial data into clinical decision making.6
Interestingly, we were able to show that baseline CRAB symptoms increase the risk of developing the same CRAB symptoms at first relapse. This association is seen in clinical practice and has already been confirmed in a Spanish study that showed correlation between renal insufficiency and hypercalcemia at diagnosis and at relapse.9 The predilection for developing a specific CRAB symptom is known to be associated with specific cytogenetic MM subtype19 and indicates the pivotal role of primary disease biology.
Regarding the aggressive forms of relapse, our study is consistent with results from previous publications. Even in the era of novel drugs, new EMD is associated with shorter survival at both diagnosis and relapse.20,21 Similarly, secondary PCL and hyperviscosity syndrome portend poor survival.22,23
Of note, we showed that in comparison with BP, more CP occurred while patients were receiving primary or maintenance treatment. Moreover, worse postprogression TTNT and OS were predicted by relapse when patients were receiving primary or maintenance treatment. This is an important finding that reflects the current tendency to implement continuous treatment strategies; it also reflects the fact that disease that relapsed during treatment might have more drug-resistant and aggressive biological characteristics and that such a relapse (whether BP or CP) should be handled more cautiously.
We observed that patients with VGPR or better were less likely to develop CP. That might be a result of the fact that the disease is biologically less aggressive in patients who achieved good response to treatment. However, the observation period in our study was limited, and the exact status of response was unknown (CR vs stringent CR vs minimal residual disease negativity); we also have not analyzed many patients treated in the first line with a combination of at least three drugs and ASCT. In view of the observation that patients with CRs have greater mutational load,24 we might expect slightly different results in the future with more effective treatment.
Our study has some limitations. This was a retrospective study that lacked protocol standardization, including the frequency of follow-up and tests for progression and CRAB symptoms. Next, the imaging technique was not consistent throughout the study, and skeletal survey (with lower sensitivity in detecting osteolytic lesions) was also used, especially during the earlier time periods. Patients who were inaccurately suspected of having BP because of the lack of imaging and who were included in the BP group may have a negative impact on survival, but this should not have affected the overall findings. Complete longitudinal data on monoclonal protein evaluations during first remission have not been collected; therefore, the study does not answer the question of whether the occurrence of CP could have been predicted and mitigated by starting treatment earlier, because the precise proportion of patients who had a BP was unknown.
One of the important questions in the field is the timing of treatment of relapsed disease, at the time of BP or when clinical signs and symptoms develop, an approach that is being studied in the setting of smoldering MM. Given the shorter time to second-line therapy in the CP group in our study, it is likely that at least a proportion of these patients have a distinct biology that predisposes to progression with clinical features rather than increasing M spike values. We also acknowledge that early initiation of treatment may not alter the survival of all patients and that we need to better determine the characteristics of patients who will benefit from early treatment. These issues can be answered only in a carefully designed prospective study, and we hope the data presented here will help form the framework for developing such a trial in the near future.
In conclusion, patients with clinical features at relapse have a worse overall and postprogression survival than patients who relapsed solely biochemically. Approximately half of CP presented while the patient was receiving active treatment, which suggests that even closely monitored patients may develop CRAB features at relapse. Factors that help predict the occurrence of CP include male sex, PCL index ≥2%, and EMD at diagnosis. Patients with deeper response to first-line treatment are less likely to develop CP, once again highlighting the need for deep responses for first-line therapy, especially in those with high-risk features at baseline. Patients tend to present CRAB criteria at relapse similar to what they present at diagnosis.
Authorship
Contribution: S.G.-M. and S.K.K. collected and analyzed the data, wrote the first draft, and approved the final version of the manuscript; A.V., S.V.R., P.K., A.D., M.Q.L., M.A.G., F.K.B., S.R.H., D.D., T.K., W.G., R.W., E.M., N.L., M.B., A.F., M.H., Y.L.H., and R.A.K. managed patients, revised the manuscript critically, and approved the final version of the manuscript.
Conflict-of-interest disclosure: P.K. received research funding from Takeda Pharmaceuticals, Sanofi, Karyopharm Therapeutics, GlaxoSmithKline, Regeneron Pharmaceuticals, Ichnos Sciences, and Amgen and served as a consultant for Sanofi, Pharmacyclics, BeiGene, Cellectar Biosciences, and Karyopharm Therapeutics. A.D. served as a consultant for and received research funding from Janssen, received research funding from Takeda Pharmaceuticals, Alnylam Pharmaceuticals, and Pfizer, and served as a consultant for Oncopeptides and Sorrento Therapeutics. M.A.G. served on the advisory board for Ionis Pharmaceuticals, served as a consultant for Akcea Therapeutics, Alnylam Pharmaceuticals, and Prothena, served on the data safety and monitoring committee for AbbVie and Celgene, received honoraria from Akcea Therapeutics, Ambry Genetics, Amgen, Celgene, Janssen Biotech, Karyopharm Therapeutics, Pfizer (to the institution), Sanofi, and Genzyme, and has stock options with Aurora BioPharma. D.D. served as a consultant for Alexion Pharmaceuticals, Apellis Pharmaceuticals, GlaxoSmithKline, Sanofi, and Janssen and received research funding from Novartis. S.K. served as a consultant for and received research funding from Bristol Myers Squibb, Amgen, and Roche-Genentech, served as a consultant for, received research funding from, and was on the board of directors or advisory committees for AbbVie, Takeda Pharmaceuticals, Janssen, Kite Pharma, and AstraZeneca, received research funding from Teneobio, CARsgen Therapeutics, Merck, Novartis, and Sanofi, served as a consultant for BeiGene, Oncopeptides, and Bluebird Bio, served as a consultant for and received honoraria from Antengene, and served on the board of directors or advisory committee for and received research funding from Adaptive Biotechnologies and Celgene. The remaining authors declare no competing financial interests.
Correspondence: Shaji K. Kumar, Division of Hematology, Mayo Clinic Rochester, 200 First St SW, Rochester, MN 55905; e-mail: kumar.shaji@mayo.edu.
References
Author notes
For original data, please contact Shaji K. Kumar (kumar.shaji@mayo.edu) or Sarah Goldman-Mazur (goldman-mazur.sarah@mayo.edu).
The full-text version of this article contains a data supplement.