Key Points
Carfilzomib+dexamethasone (Kd) had significantly higher renal overall and complete response vs bortezomib+dex (Vd) in a real-world study.
In a combined Kd+Vd analysis, renal responders had significantly longer overall survival and time to next treatment vs renal nonresponders.
Abstract
In the phase 3 ENDEAVOR study, carfilzomib-dexamethasone (Kd) improved survival over bortezomib-dexamethasone (Vd) in patients with relapsed or refractory multiple myeloma (RRMM), regardless of baseline renal function. This real-world study compared renal response in patients with RRMM (1-3 prior lines) and renal impairment (estimated glomerular filtration rate ≤50 mL/min) treated with Kd vs Vd. Electronic medical records data from the Oncology Services Comprehensive Electronic Records database were assessed (from January 2012 through February 2018). Time to renal response (defined according to International Myeloma Working Group criteria) was evaluated using the Kaplan-Meier method and log-rank test. Incidence rate ratios (IRRs) and 95% confidence intervals (CIs) were calculated for renal overall response (ROR) and renal complete response (RCR) using Cox proportional hazard models adjusted for baseline covariates. Included were 543 Kd-treated and 1005 Vd-treated patients. In line 2 (2L), compared with Vd, Kd achieved significantly higher ROR (51.4% vs 39.6%; P < .0001) and RCR (26.6% vs 22.2%; P = .0229). After baseline covariate adjustment, 2L patients receiving Kd vs Vd were 45% more likely to achieve ROR (IRR, 1.45; 95% CI, 1.18-1.78), and 68% were more likely to achieve RCR (IRR, 1.68; 95% CI, 1.24-2.28). The renal response benefit with Kd remained consistent in 2L to line 4 (4L). In a combined analysis of patients receiving Kd and Vd (2L and 2L-4L), renal responders had longer overall survival and time to next treatment than renal nonresponders. These results demonstrate improved real-world effectiveness of Kd over Vd in RRMM renal rescue, and the positive association between renal response and improved survival.
Introduction
Moderate to severe renal impairment is a common clinicopathological feature of multiple myeloma (MM), with renal impairment (serum creatinine, ≥2 mg/dL) occurring in ∼17% to 19% of patients with MM at diagnosis.1,2 A variety of factors can contribute to renal failure in MM, including hypercalcemia, dehydration, and acute tubular necrosis.3 The major cause of MM-associated renal failure involves the precipitation of monoclonal light chains that block renal tubules and result in myeloma cast nephropathy.3 Renal impairment is associated with poor prognosis and early death in patients with MM1,4 and can also complicate drug dosing and limit treatment options. In an analysis of >3000 patients with newly diagnosed MM in the United Kingdom, infection and renal failure were the main direct causes of early mortality, with renal failure being present in 28% of early deaths.4
Proteasome inhibitors have substantially improved the survival of patients with MM, including those with renal impairment.5,6 Bortezomib is currently a standard of treatment of patients with MM with renal impairment,7 and has been shown to improve survival, clinical response, and renal function in these patients.8-12 Carfilzomib, a second-generation proteasome inhibitor, has been approved in the United States for the treatment of relapsed or refractory MM (RRMM) in combination with lenalidomide plus dexamethasone or with dexamethasone alone.13 In a post hoc exploratory subgroup analysis of the head-to-head phase 3 ENDEAVOR trial, carfilzomib (56 mg/m2 twice weekly) and dexamethasone (Kd56) demonstrated progression-free survival (PFS) and overall survival (OS) improvements over bortezomib and dexamethasone (Vd) in patients with RRMM, regardless of their baseline renal function.14
There is currently a lack of data regarding real-world effectiveness of carfilzomib vs bortezomib in renal rescue in patients with RRMM. This study was conducted to describe and compare renal response rates in patients with RRMM and renal impairment treated with carfilzomib-dexamethasone (Kd) vs Vd by using electronic medical record (EMR) data from United States oncology clinics.
Methods
Study design
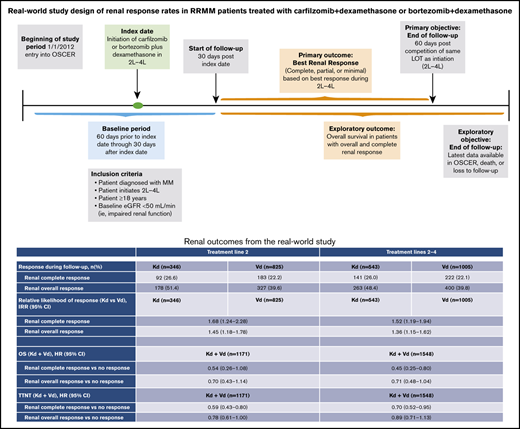
The Oncology Services Comprehensive Electronic Records (OSCER) database15 contains EMR data from oncology and hematology outpatient clinics affiliated with communities and hospitals in the United States. Inclusion criteria included a diagnosis of MM (International Classification of Diseases [ICD]-9: 203.x; ICD-10: C90.x); age ≥18 years at diagnosis; at least 2 visits to an OSCER clinic from January 2012 up to February 2018; initiation of Kd or Vd treatment as line 2 (2L), 3 (3L), or 4 (4L) with ≥30 days of follow-up after the index date; and baseline renal impairment (estimated glomerular filtration rate [eGFR] ≤50 mL/min from the most recent baseline serum creatinine measurement). The index date was defined as the date of Kd or Vd initiation, and the baseline period was from 60 days before the index date through 30 days after the index date. Patient and disease characteristics were assessed at baseline. Two cohorts of interest were identified for analysis, including the 2L and 2L to 4L (2L-4L) patient groups (Figure 1).
Study design. eGFR, estimated glomerular filtration rate; LOT, line of therapy.
Study design. eGFR, estimated glomerular filtration rate; LOT, line of therapy.
Outcomes
The primary outcome was best renal response during follow-up, with results analyzed for both the 2L and 2L-4L groups. Renal response was defined according to the International Myeloma Working Group (IMWG) criteria,7 as follows: (1) renal overall response (ROR): best response of minor response or better; (2) renal complete response (RCR): baseline eGFR <50 mL/min per 1.73 m2 and best posttreatment eGFR ≥60 mL/min; (3) renal partial response (RPR): baseline eGFR <15 mL/min per 1.73 m2 and best posttreatment eGFR 30-59 mL/min; (4) renal minor response (RMR): baseline eGFR <15 mL/min per 1.73 m2 and best posttreatment eGFR 15 to 29 mL/min or baseline eGFR 15 to 29 mL/min and best posttreatment eGFR 30 to 59 mL/min; and (5) renal no response (RNR): baseline eGFR <50 mL/min per 1.73 m2 and no improvement to >50 mL/min per 1.73 m2 after treatment. The follow-up period for best renal response was defined as 30 days after the index date to death, loss to follow-up, or 60 days after completion of the same line of treatment. An additional analysis was performed in patients with the most severe renal impairment, defined as patients with baseline renal function <15 mL/min per 1.73 m2.
In a combined secondary analysis of patients receiving Kd and Vd, OS and time to next treatment (TTNT) were compared between groups defined by depth of renal response (RCR vs RNR, RPR+RMR vs RNR, and ROR vs RNR). The follow-up period for the combined analyses extended from initiation of the treatment line to loss to follow-up, death, or event.
Statistical analyses
In the 2L and 2L-4L groups, baseline characteristics of patients in the Kd and Vd treatment arms were compared using P values based on the χ2 test for categorical variables and the t test and Wilcoxon rank-sum test for continuous variables, a nonparametric test for comparing the distribution of nonnormally distributed samples.
In Kd- and Vd-treated patients, time to renal response was evaluated and compared using the Kaplan-Meier method and log-rank test. Incidence rate ratios (IRRs) and 95% confidence intervals (CIs) were calculated for ROR and RCR using multivariate Cox proportional hazard models adjusted for baseline covariates (demographics, Eastern Cooperative Oncology Group [ECOG] Performance Status [PS], International Staging System [ISS] stage, renal function, frontline bortezomib [1L], time from MM diagnosis to initiation of treatment line, use of IV bisphosphonates, and serum calcium, serum free light-chain ratio, serum lactate dehydrogenase, and whole-blood hemoglobin measurements). These covariates were included in the models because they were deemed to be potential confounders. Missing baseline values were estimated using the standard Rubin method for multiple imputation.16
In the combined analysis of patients treated with Kd or Vd, OS and TTNT were estimated by the Kaplan-Meier method, and nonadjusted comparisons between treatment arms were made by using the log-rank test. Hazard ratios (HRs) and their 95% CIs were calculated with a Cox model adjusted for the baseline covariates.
Results
This study included a total of 543 Kd-treated patients and 1005 Vd-treated patients in the 2L-4L group; of these, 346 (64%) patients in the Kd group and 825 (82%) patients in the Vd group received 2L treatment. Baseline characteristics were generally similar between Kd and Vd treatment groups in the 2L-4L group, with no difference in baseline eGFR stages (Table 1). At MM diagnosis, Kd-treated patients were younger, with a greater percentage of Kd- vs Vd-treated patients (27.3% vs 21.1%; P = .0062) being <65 years of age. The median time from diagnosis to treatment line initiation was 17.1 months in Kd-treated patients and 16.1 months in Vd-treated patients. In the Kd- and Vd-treated groups, respectively, 46.8% and 38.0% of patients had an ECOG PS score of 0 to 1, 18.6% and 11.3% had ECOG PS score of ≥2, and 34.6% and 50.6% had missing ECOG data. In the Kd and Vd groups, respectively, 9.8% and 14.3% of patients had an ISS score of 1, 17.1% and 17.7% of patients had an ISS score of 2, and 23.0% and 20.1% of patients had an ISS score of 3.
In the 2L group, median (interquartile range [IQR]) treatment duration was 6.0 months (3-14) for Kd and 6.0 months (4-10) for Vd. In the 2L-4L treatment group, these values were 4.4 months (2.3-8.3) for Kd and 4.3 months (2.1-8.3) for Vd. In the Kd and Vd groups, median follow-up (IQR) at 2L was 7.6 (5-14) and 10.4 (5-22) months and 7.6 (5-14) and at 2L-4L, 10.3 (5-22) months, respectively.
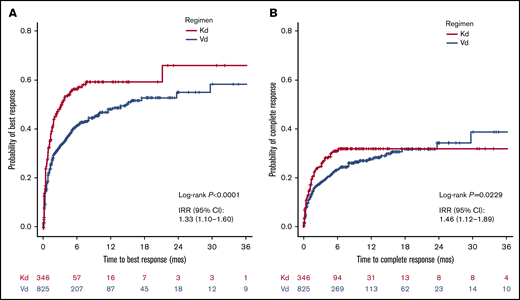
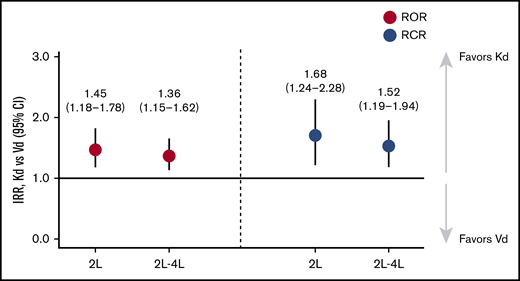
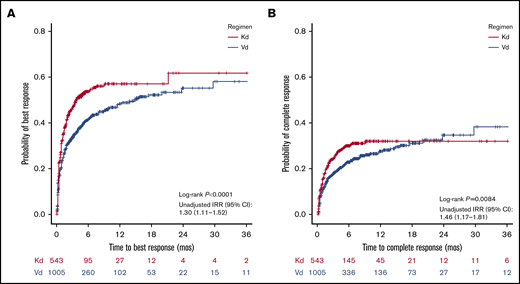
In both univariate and multivariate adjusted analyses, patients treated with Kd at 2L demonstrated significantly better outcomes than those treated with Vd, for both ROR (51.4% vs 39.6%; log-rank P < .0001; IRR, 1.45; 95% CI, 1.18-1.78) and RCR (26.6% vs 22.2%; log-rank P = .0229; IRR, 1.68; 95% CI, 1.24-2.28; Table 2; Figures 2 and 3). A similar pattern was observed in 2L-4L (ROR, 48.4% vs 39.8%; log-rank P < .0001; IRR,1.36; 95% CI, 1.15-1.62; RCR, 26.0% vs 22.1%; log-rank P = .0084; IRR, 1.52; 95% CI, 1.19-1.94; Table 2; Figures 3 and 4). Consistent results were observed among 3L and 4L patients (supplemental Figures 1 and 2) and for 2L patients with the most severe baseline renal impairment (eGFR <15 mL/min per 1.73 m2; supplemental Figure 3).
Relative likelihood of ROR and RCR in Kd-treated vs Vd-treated patients. IRRs and 95% CIs were calculated for ROR and RCR, using multivariate Cox proportional hazard models adjusted for the following baseline covariates: age, sex, race, ECOG PS, ISS stage, baseline renal function, bortezomib use in the first line, time from MM diagnosis to treatment line initiation, use of IV bisphosphonates, and baseline measurements of serum calcium, serum free light-chain ratio, LDH, and whole-blood hemoglobin.
Relative likelihood of ROR and RCR in Kd-treated vs Vd-treated patients. IRRs and 95% CIs were calculated for ROR and RCR, using multivariate Cox proportional hazard models adjusted for the following baseline covariates: age, sex, race, ECOG PS, ISS stage, baseline renal function, bortezomib use in the first line, time from MM diagnosis to treatment line initiation, use of IV bisphosphonates, and baseline measurements of serum calcium, serum free light-chain ratio, LDH, and whole-blood hemoglobin.
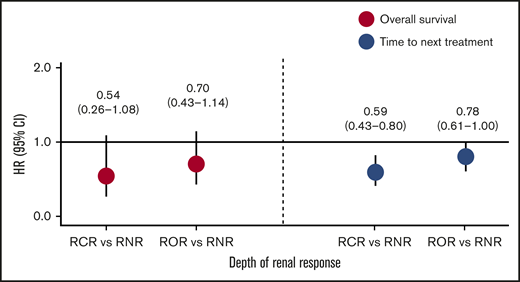
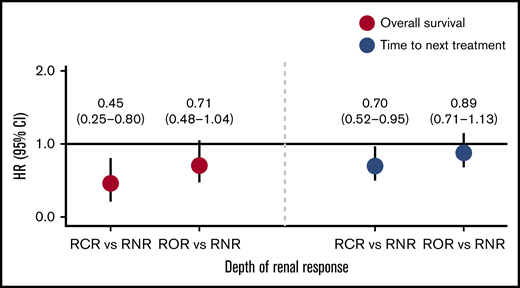
Baseline patient characteristics for a pooled analysis of Kd- and Vd-treated patients categorized by depth of renal response are shown in Table 3 for patients in the 2L group and in Table 4 for patients in the 2L-4L group. Renal responders tended to be younger, to be at a lower ISS stage, and to have higher free light-chain ratios and lactate dehydrogenase (LDH), than patients with no renal response. When we examined OS and TTNT by depth of renal response in those patients, we found that, at 2L, responders had longer OS and TTNT than renal nonresponders (Figure 5). Patients who achieved RCR had a 46% lower risk of death (HR, 0.54; 95% CI, 0.26-1.08) and patients who achieved ROR had a 30% lower risk of death (HR, 0.70; 95% CI, 0.43-1.14) than patients who did not achieve a renal response. Patients who achieved RCR were 41% less likely (HR, 0.59; 95% CI, 0.43-0.80) and patients who achieved ROR were 22% less likely (HR, 0.78; 95% CI, 0.61-1.00) to need a subsequent line of therapy, than were patients who did not achieve a renal response. Similarly, renal responders had longer OS and TTNT than renal nonresponders when lines 2 to 4 were combined (Figure 6). Patients who achieved RCR had a 55% lower risk of death (HR 0.45; 95% CI, 0.25-0.80), and patients who achieved ROR had a 29% lower risk of death (HR, 0.71; 95% CI, 0.48-1.04) than patients who did not achieve a renal response. Patients who achieved RCR were 30% less likely (HR, 0.70; 95% CI, 0.52-0.95) and patients who achieved ROR were 11% less likely (HR, 0.89; 95% CI, 0.71-1.13) to need a subsequent line of therapy than were patients who did not achieve a renal response.
Cox model for OS and TTNT by depth of renal response. HR and 95% CI of combined Kd- and Vd-treated population at 2L.
Cox model for OS and TTNT by depth of renal response. HR and 95% CI of combined Kd- and Vd-treated population at 2L.
Cox model for OS and TTNT by depth of renal response. HR and 95% CI of combined Kd- and Vd-treated population at 2L-4L.
Cox model for OS and TTNT by depth of renal response. HR and 95% CI of combined Kd- and Vd-treated population at 2L-4L.
Discussion
Our study is the first, to our knowledge, to investigate the real-world effectiveness of Kd and Vd in renal rescue of patients with RRMM. Using OSCER, one of the most complete oncology EMR databases available, we found that patients with RRMM who had baseline renal impairment treated with Kd had significantly higher rates of overall and complete renal response and were more likely to have a renal response, than patients treated with Vd. In addition, both OS and TTNT were longer in renal responders than in renal nonresponders in a combined analysis of patients treated with Kd and Vd at 2L.
Our study findings are consistent with those observed in the randomized controlled trial ENDEAVOR among patients with RRMM and varying degrees of renal impairment and further demonstrates the superior efficacy of Kd over Vd in real-world clinical practice settings.14 In our analysis, after adjustment for potential baseline confounders, a patient treated with Kd at 2L was more likely to experience RCR than was a patient treated with Vd at 2L; results were similar in patients treated with Kd vs Vd at 2L-4L. Similarly, in the ENDEAVOR trial, a higher proportion of Kd56- than Vd-treated patients experienced RCR (15.3% vs 14.1%; supplemental Table 2), although the difference did not meet the cutoff for statistical significance specified in the study.14 There was also a consistent PFS and OS benefit of Kd56 vs Vd treatment across all levels of renal function, including severe renal impairment (creatinine clearance, ≥15 to <50 mL/min), with the lowest HR for OS.
This benefit was most apparent in patients who achieved RCR. Clinical trials have demonstrated an association between renal response and clinical outcomes in patients with MM who have renal impairment. In the combined Kd56 and Vd subgroup analysis in ENDEAVOR, complete renal responders had a longer median PFS (14.1 vs 9.4 months) and OS (35.3 vs 29.7 months) compared with renal nonresponders (supplemental Table 2).14 Among newly diagnosed patients with MM with renal impairment, a single-center analysis demonstrated a longer median OS in patients who achieved renal response than in those who did not (56 vs 33 months; P = .006).17 In addition, in an analysis of patients with MM who survived at least 1 month, patients with a renal response had a higher 1-year survival rate than did the renal nonresponders (82% vs 54%), and those who achieved both a renal and disease response had a better outcome (92% alive at 1 year) than those who had neither a renal nor a disease response (40% alive at 1 year).8 In our combined analysis of patients treated with Kd and Vd at 2L and 2L-4L, patients who achieved a renal response had improved OS and TTNT than those who did not.
We observed a consistent benefit of carfilzomib, whether used at first relapse or after 2 to 3 lines of therapy in patients with RRMM and renal impairment. Similarly, in a subgroup analysis of patients with RRMM and various degrees of renal impairment from ENDEAVOR, there were consistent PFS and OS benefits with Kd56 vs Vd, regardless of the number of prior lines of therapy (1 or 2-3 lines). These benefits were observed across all renal subgroups (creatinine clearance, ≥15 to <50 mL/min, 50 to <80 mL/min, and ≥80 mL/min).14
Our study results are compelling, given the importance of having effective MM therapies available at first relapse as well as after multiple lines of treatment, as patients are living longer with MM.18 Deep responses to treatment at first relapse are important for extended survival, and therapies that can improve renal efficacy to maximize efficacy are critical. For patients with MM who have undergone multiple lines of treatment, each line of therapy is associated with an increased risk of comorbidities or disease-related complications, as well as shorter response rates.19,20 Thus, as patients advance in therapy, it is important to have options that can improve renal function. In addition, there is an unmet need for effective MM therapies for patients with severe renal impairment, because these patients are often excluded from MM clinical trials.21-23 Our study results suggest that treatment with Kd can help address this need. Currently, the IMWG recommends bortezomib-based regimens for the management of myeloma-related renal impairment (grade A).7 Our results, together with the efficacy data for renally impaired MM patients from ENDEAVOR,14 suggest that treatment guidelines should include carfilzomib as a recommended treatment option for patients with MM and renal impairment.
There were some limitations associated with this study. As expected with structured electronic health records data, we observed an incomplete ascertainment of antitumor response, transplantation history, baseline comorbidities, and use of concomitant medication in the OSCER database. Kd-treated patients were younger on average than Vd-treated patients, and bortezomib-based therapies were the most common 1L regimens for both Kd- and Vd-treated patients. However, after adjustment for differences in age and 1L bortezomib use, Kd was still associated with superior renal response in both the 2L and the combined 2L-4L cohorts.
The results of this study demonstrate the real-world effectiveness of carfilzomib-based therapy in renal rescue for patients with RRMM. Our findings suggest a consistent clinical benefit of carfilzomib over bortezomib in patients with MM with various degrees of renal impairment.
Because permission for data sharing was not obtained from all participating partners, the patient-level data set used in this study will not be shared. The institutional review board of each oncology practice approved collaboration to provide data for the OSCER database. Per the United States framework for retrospective noninterventional studies, informed patient consent was waived. Individual patient-level data were protected against breach of confidentiality, consistent with the final Health Insurance Portability and Accountability Act Security Rule from the United States Department of Health and Human Services.
Acknowledgments
Medical writing assistance was provided by Sachi Yim and Andrew Gomes of BlueMomentum, an Ashfield Company, part of UDG Healthcare, plc.
This study was supported by research funding from Amgen Inc. Medical writing assistance was funded by Amgen Inc.
Authorship
Contribution: A.F. was involved in the conception and design of the study; all authors were involved in the analysis and interpretation of data; and all authors participated in the writing of the manuscript and approved the final version before submission.
Conflict-of-interest disclosure: S.K. reports membership on the board of directors or advisory committees for, and research funding from AbbVie, Celgene, Janssen, and KITE. A.F. reports employment with and equity ownership in Amgen Inc. R.N. reports consultancy for and research funding from Amgen Inc, Bristol-Myers Squibb (BMS), Janssen, Celgene, and Takeda. S.J. reports participation in the speakers’ bureau for the Multiple Myeloma Research Foundation and Medicom and consultancy for Novartis, Merck, BMS, and Celgene. R.B. reports consultancy for Sandoz and Pfizer; participation in the speakers’ bureau for AbbVie, Genentech, Amgen Inc, and AstraZeneca; and research funding from Genentech, Amgen Inc, BMS, and AstraZeneca. N.R. reports consultancy for Celgene, Janssen, Merck, Takeda, BMS, and Amgen, Inc.; research funding from AstraZeneca; and honoraria from Research to Practice and Medscape.
Correspondence: Shaji Kumar, Mayo Clinic, 200 1st St SW, Rochester, MN 55905; e-mail: kumar.shaji@mayo.edu.
References
Author notes
The full-text version of this article contains a data supplement.