Key Points
Ischemic stroke is not rare in patients with POEMS syndrome and is an unfavorable prognostic factor for survival.
Abstract
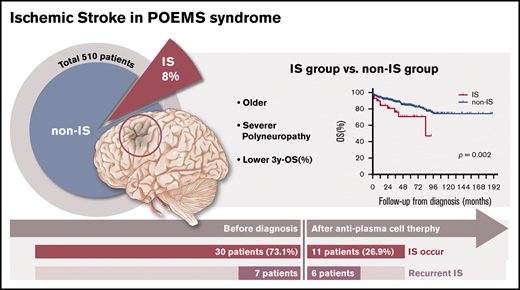
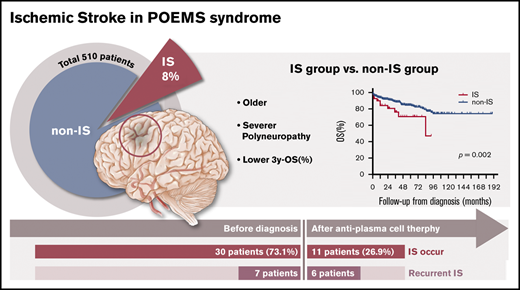
Polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes (POEMS) syndrome is associated with increased risk for ischemic stroke (IS). Because POEMS syndrome is rare, little is known regarding the underlying mechanism and prognosis for IS in patients in whom it occurs. The medical records of patients with POEMS syndrome were screened between January 2018 and January 2000 at Peking Union Medical College Hospital to identify those with IS. The baseline characteristics, IS features, and patient outcomes were analyzed. Forty-one (8.0%) of 510 POEMS patients were documented to have IS. Patients with IS were older, had a higher percentage of Overall Neuropathy Limitation Scale score >4, and had a higher level of fibrinogen compared with those who did not have IS. Ninety-three percent of IS events occurred before or within 3 months after a diagnosis of POEMS. Of 41 occurrences of IS, 29 (46.3%) were multifocal. Recurrent IS was observed in 13 (31.7%) of 41 patients, but not in patients with successful anti-plasma cell therapy. The 3-year overall survival rate in patients with IS was 71.0% and for those without IS, it was 88.5% (P = .002). We showed that 8.0% of POEMS patients had IS, and most IS events occurred in POEMS patients not being treated effectively. Having IS was a predictor of unfavorable prognosis. Early diagnosis, immediate initiation of treatment for POEMS, and control of POEMS syndrome is key to reducing the occurrence of IS, improving survival, and preventing recurrence of IS.
Introduction
Polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes (POEMS) syndrome is a rare paraneoplastic syndrome that results from an underlying plasma cell disorder named by Bardwick et al1 in 1980. Additional important features that are not included in the POEMS acronym are elevated vascular endothelial growth factor (VEGF) levels, Castleman disease, sclerotic bone lesions, extravascular volume overload, thrombocytosis or erythrocytosis, and papilledema.2 Moreover, arterial and/or venous thrombotic events, such as ischemic stroke (IS), myocardial infarction, and Budd-Chiari syndrome, are also observed and seem to be part of the syndrome.2-5 Lesprit et al4 noted that 4 of 20 patients with POEMS syndrome had arterial occlusions. According to Dispenzieri et al,5 18 of 99 patients with POEMS syndrome had 21 thrombotic events, including 10 venous and 11 arterial thromboses. In addition, it has been reported that approximately 10% of patients with POEMS syndrome present with cerebral infarctions, and the suspected etiologies include vascular structural abnormalities leading to vessel dissection and stenosis along with embolism from a proximal source6 ; however, the pathophysiologic mechanism and prognosis of IS in patients with POEMS syndrome are unclear. We retrospectively reviewed the clinical features and long-term outcomes of Chinese patients with POEMS syndrome and IS.
Methods
Patients
Between January 2018 and January 2000, 510 consecutive patients were newly diagnosed with POEMS syndrome at Peking Union Medical College Hospital according to the diagnostic criteria described by Dispenzieri.2 The diagnostic criteria used included 2 mandatory criteria, at least 1 major criterion, and at least 1 minor criterion. The 2 mandatory criteria were polyneuropathy and monoclonal plasma cell proliferative disorder. The major criteria included Castleman disease, sclerotic bone lesions, and increased VEGF levels. The minor criteria included organomegaly, extravascular volume overload, endocrinopathy, skin changes, papilledema, and thrombocytosis or polycythemia.
IS
IS was defined as an episode of acute neurologic dysfunction caused by focal cerebral ischemia based on objective imaging techniques (computed tomography scan or magnetic resonance imaging) and clinical evidence of cerebral focal ischemic injury based on symptoms of any duration. If any patients had IS that preceded any symptom of POEMS syndrome, IS was considered to not be associated with POEMS and that patient was excluded from the study. Recurrent IS was defined by using the same criteria applied for the definition of the index event.7 One neurologist (M.Q.) reviewed the diagnostic criteria used to identify IS patients. Events were classified as unilateral or bilateral, and detailed clinical descriptions for each IS were recorded.
Data collection
The detailed clinical features of POEMS syndrome were assessed at the time of diagnosis, as previously described.8,9 Laboratory data associated with POEMS syndrome were collected, including bone marrow examinations, serum protein electrophoresis, serum and urine immunofixation, and liver and renal function tests (including albumin and serum creatinine). The estimated glomerular filtration rate was calculated by using the Chronic Kidney Disease-Epidemiology Collaboration equation.10,11
Serum VEGF was measured with a human Quantikine ELISA kit (R&D Systems, Minneapolis, MN). A serum VEGF <600 pg/mL was considered normal, as described elsewhere.12,13 The Overall Neuropathy Limitation Scale (ONLS) was used to assess neurologic disability.14 Systolic pulmonary arterial pressure was estimated on the basis of a duplex cardiac ultrasound, and pulmonary hypertension was defined as a systolic pulmonary arterial pressure ≥50 mmHg.15
Patients were divided into low-, intermediate-, and high-risk groups based upon none, one, or more than one of the following findings9 : age >50 years (score 1), pulmonary hypertension (score 1), pleural effusion (score 1), and estimated glomerular filtration rate <30 mL/min/1.73 m2 (score 2).
Treatment and follow-up data were retrieved from the medical records. The last follow-up date was 1 January 2019. Regimens used for treatment included mainly autologous stem cell transplantation (ASCT), lenalidomide and dexamethasone (RD), melphalan and dexamethasone (MD), bortezomib and dexamethasone (BD), and thalidomide and dexamethasone (TD). The choice of treatment was based on the patient’s clinical condition, autonomy, and the treating physician’s judgment.
Hematologic complete remission (CRH) was assessed by immunofixation electrophoresis and free immunoglobulin light chain negativity in both serum and urine. VEGF complete remission (CRV) was defined as a decrease in VEGF to a normal concentration (<600 pg/mL). Neurological response (RN) was defined as a decrease in the ONLS score of at least 1 point.12,16,17
For each IS patient, the Framingham Stroke Risk Profile18 score was completed. Treatment during the acute phase of stroke was rendered by stroke specialists after consulting with hematologists.
Ethical statement
This study was approved by the Clinical Research Ethics Committee of Peking Union Medical Center Hospital (Beijing, China). Because of the retrospective nature of the study, written informed consent was waived by the Ethics Committee.
Statistical analysis
Statistical analysis was performed using SPSS software (version 22.0; IBM, Armonk, NY). Categorical data are expressed as percentages and were compared using the χ2 or Fisher’s exact test. The mean and standard deviation are presented for normally distributed variables, and the median and range are presented for non-normally distributed variables. All P values are 2-sided with a significance level of .05. Survival was assessed by the Kaplan-Meier method and compared by the log-rank test.
Results
Demographic and clinical characteristics
Among all 510 patients, 41 (8.0%) had a history of IS. The demographic and clinical characteristics of the IS and non-IS groups are listed in Table 1. POEMS patients who had IS were older and had a higher percentage of ONLS score >4 compared with non-IS patients. In addition, IS patients had less hepatomegaly but more hypothyroidism and higher serum fibrinogen concentrations. Other demographic and clinical characteristics were identical in the IS and non-IS patients.
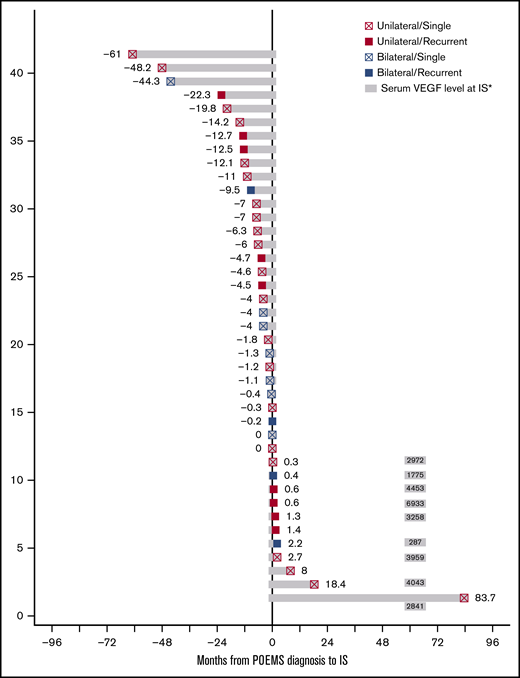
IS evaluation data
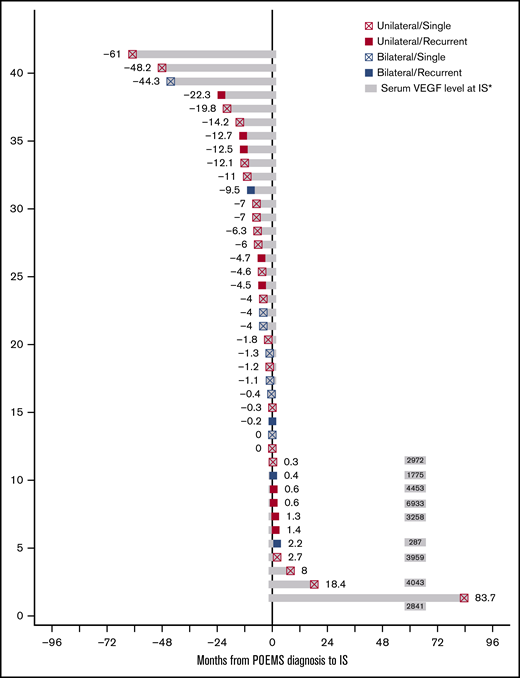
Forty-one patients had 60 episodes of IS. Among the 41 patients, IS occurred in 30 patients (73.1%) before they were diagnosed with POEMS syndrome and occurred concurrently with peripheral neuropathy in 6 patients (14.6%). Eleven patients (26.8%) developed IS after the diagnosis and treatment of POEMS syndrome, including 8 patients within 3 months and 3 patients beyond 3 months after being diagnosed and treated (Figure 1). Serum VEGF levels were measured in 9 patients at the time of an IS event that occurred after they were diagnosed with POEMS, and 8 had increased VEGF levels (Figure 1). Among the 11 patients, 6 developed IS after treatment with the RD regimen and 5 after treatment with a non-RD regimen (3 after ASCT and 2 after MD), which accounted for 3.8% of the RD group and 2.4% of the non-RD group, respectively (P = .400). After 2013, we used aspirin as the primary preventive medicine for IS after diagnosis of POEMS syndrome; however, the incidence of IS after diagnosis was not affected (2.3% before 2013 vs 2.8% after 2013; P = .749).
Time distribution of POEMS-IS patients. *Normal serum VEGF concentration was <600 pg/mL.
Time distribution of POEMS-IS patients. *Normal serum VEGF concentration was <600 pg/mL.
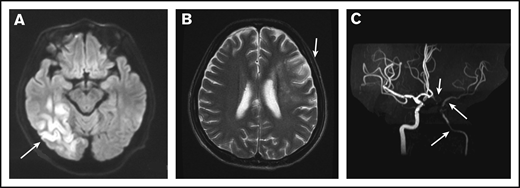
Among 41 IS cases, 19 (46.3%) were multifocal, including 12 bilateral and 7 unilateral. Cerebral vessels were evaluated in only 8 patients via magnetic resonance angiography (MRA) or computed tomography angiography (CTA) (Figure 2A-C). Seven (87.5%) of 8 patients were documented to have cerebral vasculopathy; 3 patients were shown to have multiple and bilateral cerebral artery stenosis or occlusion, including the internal carotid artery, 2 with unilateral internal carotid artery stenosis, 1 with unilateral middle cerebral artery stenosis, and 1 with unilateral posterior cerebral artery stenosis. Cerebral venous sinus thrombosis was demonstrated in 1 patient.
MRI and MRA for a patient with POEMS syndrome and IS. (A) MRI of the brain showed a cerebral infarction of the right temporal occipital lobe (white arrow). (B) A second MRI showed a new focal lesion of cerebral infarction near the left centrum semiovale 1 month later (white arrow). (C) MRA showed severe stenosis of the left intracranial internal carotid artery, left middle cerebral artery, and left anterior artery (white arrows).
MRI and MRA for a patient with POEMS syndrome and IS. (A) MRI of the brain showed a cerebral infarction of the right temporal occipital lobe (white arrow). (B) A second MRI showed a new focal lesion of cerebral infarction near the left centrum semiovale 1 month later (white arrow). (C) MRA showed severe stenosis of the left intracranial internal carotid artery, left middle cerebral artery, and left anterior artery (white arrows).
Recurrent IS was observed in 13 (31.7%) of the 41 POEMS patients, in 7 patients before treatment and in 6 patients during treatment. Eight patients had 2 recurrences, 4 patients had 3 recurrences, and 1 patient had 4 recurrences of IS during the study period. The median interval from first IS to second IS was 1 day (range, 1 day to 17 months). The baseline characteristics of patients with singular versus recurrent IS events are summarized in Table 2. POEMS patients with recurrent IS had a shorter diagnostic interval and a higher platelet count than those with singular IS events; other characteristics were identical. Nine patients with recurrent IS were also screened for inherited or acquired thrombophilia, including deficiencies of antithrombin, protein C, protein S, factor V Leiden, hyperhomocysteinemia, lupus anticoagulant, antiphospholipid antibody, and JAK2V617F mutation, but all test results were negative. MRA was performed in 3 POEMS patients with recurrent IS, and all patients had internal carotid artery stenosis.
Treatment and survival
Two patients (4.9%) received palliative treatment. Among the remaining 39 patients, 15 (38.4%) received RD and 24 (61.5%) received non-RD regimens, including ASCT in 14 (35.9%), MD in 9 (23.0%), and TD in 1 (2.6%). Among the 13 patients with recurrent IS, 5 received ASCT, 5 received RD, and 3 received MD. However, 2 patients had stem cells harvested by high-dose cyclophosphamide mobilization and prepared for ASCT, but they discontinued ASCT and switched to receive BD and RD treatment because of recurrent IS, respectively. The total CRH rate in 24 evaluated IS patients was 54.2%, which was comparable to that for non-IS patients (189 [51.5%] of 367; P = .836). The CRV response and RN were the same between IS and non-IS patients (39.1% vs 53.7%; P = .127; 96.3% vs 93.7%; P = .497). The CRH, CRV, and RN among patients with singular and recurrent IS were not significantly different.
With respect to anti-platelet and anti-coagulation treatments in POEMS IS patients, 34 (82.9%) were treated with single anti-platelet drugs, 4 (9.8%) were treated with both anti-platelet and anti-coagulation therapy, and 3 (7.3%) received dual anti-platelet treatment.
Although anti-platelet or anti-coagulation treatment was used in 13 patients who had IS at the time of diagnosis or after treatment of POEMS syndrome, 7 patients still had recurrent IS. Interestingly, all of those recurrences happened immediately after POEMS was diagnosed (within 3 months); in IS patients who were treated for more than 3 months, no recurrence was identified.
The median follow-up time was 48 months (range, 1-190 months) for all POEMS syndrome patients, 38 months (range, 2-137 months) for IS patients, and 48 months (range, 1-190 months) for non-IS patients. At the time of the last follow-up for patients with POEMS syndrome and IS, 3 patients (7.3%) were lost to follow-up and 11 patients (26.8%) died. Among the deceased patients, 8 died of infections, 2 died of disease progression, and 1 died of secondary malignancy after treatment with RD and ASCT.
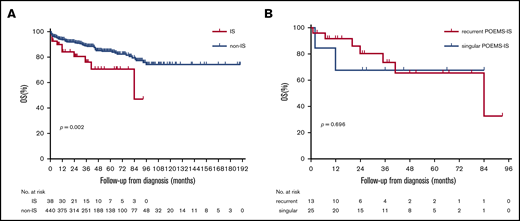
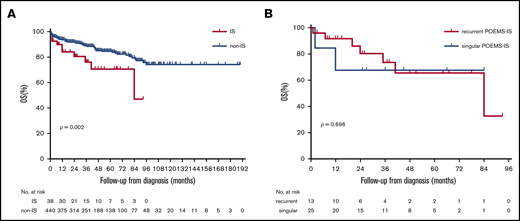
The 3-year overall survival (OS) rates in patients with IS was 71.0% and for those without IS, it was 88.5% (P = .002; Figure 3A). The 3-year OS rates in IS patients with recurrent and singular attacks were similar (67.7% and 73.7%, respectively, P = .696; Figure 3B).
OS in IS patients with POEMS syndrome. (A) Survival in IS and non-IS patients with POEMS syndrome. (B) Survival in IS patients with recurrent and singular attacks.
OS in IS patients with POEMS syndrome. (A) Survival in IS and non-IS patients with POEMS syndrome. (B) Survival in IS patients with recurrent and singular attacks.
Discussion
In this retrospective cohort study, we analyzed 510 consecutive Chinese patients with POEMS syndrome, including 41 patients with comorbid IS. Our study had 3 novel findings. First, we discovered that 8.0% of patients with POEMS syndrome developed IS. Compared with the non-IS group, IS patients were older and had higher ONLS scores. Second, we found that IS in the majority of patients occurred before or immediately after the diagnosis of POEMS syndrome. Approximately one-half of IS occurrences were multifocal and one-third were recurrent. Indeed, to prevent IS recurrence, anti-atherosclerotic drugs may be not sufficient, but anti-plasma cell treatment seems essential. Third, patients with IS had a lower OS compared with non-IS patients.
According to our analysis, 41 patients with POEMS syndrome (8.0%) had IS, which was less than that reported by Dupont et al.6 Although the median age of the patients in the IS group was 7 years older than that of the patients in the non-IS group, the median age was much younger than the typical age range reported in stroke registries for white and Chinese people.19-21 In agreement with other published case series of patients with POEMS syndrome and an IS event,6,22 the frequencies of stroke risk factors such as diabetes mellitus, hypertension, and cardiac arrhythmias occurring in our study were lower than those in the stroke registries,19-21 but the prevalence of multifocal lesions and large vessel stenosis was more common.
The pathophysiologic mechanism underlying IS in patients with POEMS syndrome has not been elucidated. Ninety-three percent (38 of 41) of IS events occurred before or immediately after the diagnosis of POEMS symptoms, suggesting that active disease may be an indicator for IS susceptibility.6 There are several possible explanations for the occurrence of IS in our patients. First, hyperfibrinogenemia in our cohort and in other reports22-26 is believed to trigger a hypercoagulative state. Thrombocytosis,4,6 polycythemia,4,27 bone marrow plasma cell proliferation,6 and high levels of circulating proinflammatory cytokines such as VEGF10,22 have also been reported to increase the risk of IS; however, our study showed that these factors were identical in IS and non-IS patients. Second, large vessel stenosis or occlusions or structural anomalies confirmed by MRA or CTA, especially in patients with no known risk factors for atherosclerosis, is thought to be the cause of stroke. In our study, 7 of 8 patients who underwent MRA had internal carotid artery and/or other proximal intracranial artery stenosis or occlusion, similar to that reported by Dupont et al.6 Yaghi et al28 described 1 patient with POEMS syndrome and recurrent stroke whose temporal artery biopsies were negative for an inflammatory process but showed thickening of blood vessels, which distinguishes vasculopathy from vasculitis and atherosclerosis. Angiogenesis within the adventitia of vessel walls induced by VEGF also plays an important role in the pathogenesis of chronic inflammation of vessel walls.22,29-31
Some case series have reported that POEMS patients with IS die within 2 years after a stroke event.4,25,26,28,32-34 In this study, we noted that the 3-year OS of POEMS patients with IS was approximately 15% lower than that for non-IS patients. Therefore, IS is an unfavorable outcome predictor in patients with POEMS syndrome. Only a minority of IS patients were diagnosed beyond 3 months after initiation of anti-plasma cell treatment, indicating that early diagnosis and treatment of POEMS syndrome may reduce the incidence of IS, potentially reducing mortality.
Recurrent IS in POEMS patients has been described only in case reports consisting of 1 to 2 patients.28,34,35 Our study showed that 31.7% of POEMS patients presented with recurrent IS, which was much higher than IS patients without POEMS syndrome (11.2% in a Chinese study36 and 4.3% to 10.3% in Western studies20,37-41 ). Moreover, although patients with recurrent IS did not have common stroke risks, such as traditional atherosclerotic risk factors, atrial fibrillation, cardiac vegetations, or thrombosis,36-38 they had higher platelet counts than patients with singular IS, and all POEMS patients with recurrent IS who were undergoing MRA had internal carotid artery stenosis, which might partly explain the occurrence of recurrent strokes.38,42 Although recurrent IS increased mortality in IS patients,38,43,44 the OS rates of patients with POEMS syndrome who had either singular and recurrent IS were similar.
With respect to preventing recurrence, our study showed that IS recurred in 53.8% of patients with POEMS syndrome even after anti-thrombotic treatment, indicating that anti-thrombotic therapy is insufficient for POEMS patients with IS, which has been reported by others.4,22,34,35 Previous reports4,22,45-48 have suggested that treatment of POEMS syndrome might be necessary to reduce the risk of IS relapse, and our cohort also showed that none of the patients with POEMS had IS recurrence after successful anti-plasma cell treatment. Therefore, disease control of POEMS syndrome is more important than anti-thrombotic therapy to prevent IS recurrence.
This study had several limitations. First and most important, because of the retrospective nature of the study, it had incomplete data, and denominators kept changing across the results and tables. Second, symptoms of IS such as numbness or muscle weakness are not specific and may easily mislabel POEMS syndrome as a peripheral neuropathy. Because not all patients were screened for cerebrovascular disease, the prevalence of IS among POEMS patients may have been underestimated. Finally, although this study included the most POEMS patients with IS, only 41 patients were analyzed because of the rarity of POEMS IS, thus hampering the credibility of the results.
In conclusion, in this large cohort of patients with POEMS syndrome, we showed that 8.0% of them had IS. Most IS events occurred before or immediately after the diagnosis of POEMS syndrome. IS is a predictor of unfavorable prognosis. Thus, early diagnosis, immediate treatment, and control of POEMS syndrome not only reduce the occurrence of IS and improve survival, but also prevent recurrence of IS.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 81570195) (L.J.), the Foundation for Distinguished Young Physicians of Peking Union Medical College Hospital (Grant No. JQ20150) (L.J.), the CAMS Innovation Fund for Medical Sciences (Grant No. 2016-12M-1-002) (L.J.), and The National Key Research and Development Program of China (Grant No. 2016YFC0901503) (L.J.).
Authorship
Contribution: J.F. designed the study, collected and analyzed the data, and drafted and revised the manuscript; X.-m.G. collected and analyzed the data and drafted and revised the manuscript; H.Z., T.-h.H., C.-l.Z., K.-n.S., L.Z., and X.-x.C. collected data; M.Q. collected and analyzed data; D.-b.Z. designed the study; and J.L. designed the study and drafted and revised the text.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Jian Li, Department of Hematology, Peking Union Medical College Hospital, Peking Union Medical College, Beijing 100730, China; e-mail: lijian@pumch.cn.
References
Author notes
Further anonymized data can be shared by request from Jian Li (lijian@pumch.cn).