Abstract
We evaluated the clinical characteristics of 41 children with chronic neutropenia based on the quantitative analysis of antineutrophil antibodies in serum by flow cytometry. According to the strength of antineutrophil antibodies, the patients were divided into 3 groups: 12 patients presented negative antibodies, 13 patients showed weak positive antibodies, and 16 patients showed strong positive antibodies. No significant differences were seen in age of diagnosis, severity of neutropenia, and infectious complications associated with neutropenia among the 3 groups. The spontaneous resolution of neutropenia was observed in all patients with negative antibodies and in 22 of 29 patients with positive antibodies. The age of the recovery of neutropenia and the duration until spontaneous resolution of neutropenia were significantly dependent on the antibody strength at the time of diagnosis. These results demonstrate that the quantification of antineutrophil antibodies at the time of diagnosis may be useful in considering the clinical course of chronic neutropenia in childhood.
Introduction
Chronic neutropenia is defined as low absolute neutrophil count (ANC) of less than 1500/μL blood, lasting for at least 6 months.1-3 The pathophysiology of chronic neutropenia in childhood remains unclear because of the heterogeneity of this disorder. Chronic benign neutropenia (CBN) and primary autoimmune neutropenia (AIN) are common forms of neutropenia in infants and early childhood.1-11 Both types of neutropenia have shown similar hematologic findings along with their clinical features. The definitive distinction is the presence or absence of circulating antineutrophil antibodies in serum. Most of these cases actually are considered antineutrophil antibody–mediated neutropenia, because technical difficulties exist in the detection of antineutrophil antibodies.3,4,7 Several methods are used in the detection of serum antineutrophil antibodies.5-8 12-17 However, the specificity and sensitivity of these methods have not been well established. In this study, we have developed a method to semiquantify the strength of antineutrophil antibodies by flow cytometric analysis of the granulocyte indirect immunofluorescence test (GIIFT) by using same donor neutrophils. The results demonstrate the efficacy of the quantification of antineutrophil antibodies at the time of diagnosis and its relevance to the duration of neutropenia.
Study design
Patients
All patients or their sera were referred to our hospital for examining antineutrophil antibodies from June 1995 to October 1999. Forty-one patients were included in this study when their ANC was less than 1500/μL blood for more than 6 months without underlying diseases, a history of drug administration causing neutropenia, or a history of blood transfusions. Approval was obtained from the institutional review board for these studies. Informed consent was provided according to the Declaration of Helsinki. Patients with severe congenital neutropenia, cyclic neutropenia, or alloimmune neutropenia were excluded.
Preparation of monoclonal antibodies to neutrophil-specific antigens and the typing of neutrophils
Human neutrophils were prepared by previously described method.8 Monoclonal antibodies, TAG1, TAG2, and TAG4 that recognize neutrophil-specific antigens, HNA-1 and HNA-2, were originally established. The characteristics of TAG1 and TAG2 were identified by comparing the binding properties of MG38 (Nichirei, Tokyo, Japan), GRM1 (a kind gift from Dr Garrido, Granada University, Granada, Spain), and 3G8 (Pharmingen, San Diego, CA).18,19The binding characteristic of TAG4 was almost identical to that of 7D8 (a generous gift from Dr Stroncek, National Institutes of Health, Bethesda, MD).20,21,22 The genotypes of HNA-1 antigens were determined by using a modification of polymerase chain reaction methods previously reported.23 24
GIIFT and micro-leukocyte agglutination test
GIIFT and micro-leukocyte agglutination test (MLAT) were performed by using a modification of the previously described method.8 In GIIFT, fluorescence isothiocyanate–labeled F(ab′)2 fragments of goat antihuman polyvalent immunoglobulin, immunoglobulin (Ig)G, IgM, and IgA (Tago, Burlingame, CA) were used as the second antibody. The cell suspension was examined by using flow cytometry (FACS Vantage; Becton Dickinson Immunocytometry Systems, San Jose, CA) with 4-W argon ion laser and/or ORTHO CYTRON ABSOLUTE (Ortho-Clinical Diagnostics K.K., Tokyo, Japan) by using a 15-mW argon ion laser.
To avoid variability in the flow cytometric analysis, the same pooled sera from AB-type healthy male subjects and the neutrophils prepared from same donors were used throughout this study. Neutrophils from a FcγRIIIb-deficient donor were used as a control, if necessary. To confirm the specificity of antibodies against target antigens, monoclonal antibody–specific immobilization of granulocyte antigens was performed according to the previously reported method.25 Lymphocyte cytotoxicity test was also performed to exclude the antibodies associated with HLA antigens.
Results and discussion
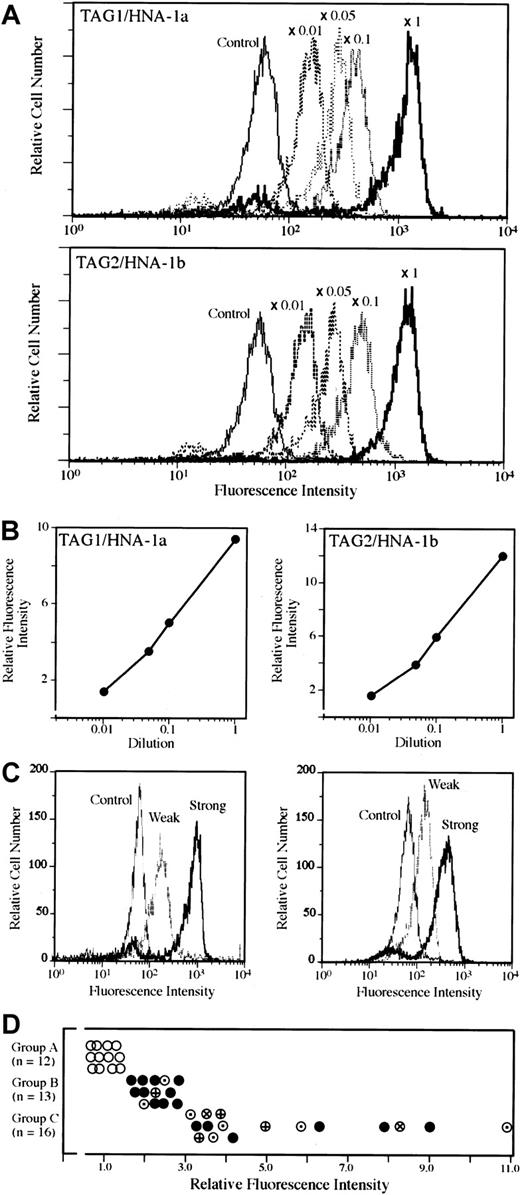
Monoclonal antibodies established by our laboratory, TAG1 or TAG2, reacted with HNA-1a– or HNA-1b–homozygous neutrophils, respectively (Figure1A). The bindings of monoclonal antibodies, TAG1 or TAG2, to the same HNA-1a– or HNA-1b–homozygous donor neutrophils gave rise to almost consistent fluorescence intensity by setting the mean fluorescence channel of the control sample from 50 to 100. The ratio of the mean fluorescence channel of each sample to that of control serum was expressed as relative fluorescence intensity (RFI) to quantify the strength of the antibodies.26 The bindings of antibodies to neutrophils and the RFI of each antibody depended on the concentrations of antibodies (Figure 1B). The representative flow cytometric findings of strongly and weakly positive antibodies to 2 different HNA-1a–homozygous donors are shown in Figure 1C. The data describing the RFI value for each sample were expressed as the mean of the results against 2 or 3 different donors probably possessing the target antigens of the antibody. As shown in Figure 1D, patients were classified into 3 groups based on the RFI value of antineutrophil antibody test in serum at the time of the diagnosis. Eighty-five percent of patients with positive antibodies showed IgG, and the remaining showed IgM antibodies. The distribution of immunoglobulin class did not differ between group B and group C (data not shown). No patients with negative antibodies by flow cytometry showed a positive MLAT in this study.
Representative flow cytometric analysis for detecting antineutrophil antibodies and classification of patients.
All histograms showed the analysis of neutrophils, which were gated electronically in medium to high forward and orthogonal light scatter, and the green fluorescence of this population was collected. Data acquisition and analysis were performed with CellQuest software (Becton Dickinson Immunocytometry Systems) or ORTHO ImmunoCount II software (Ortho Diagnostic Systems). Various concentrations of TAG1 bind to HNA-1a–homozygous neutrophils and those of TAG2 to HNA-1b–homozygous neutrophils (A). The relative fluorescence intensity (RFI) of each concentration of TAG1 or TAG2 is presented (B). The representative flow cytometric findings of weakly positive and strongly positive sera were shown against 2 different HNA-1a–homozygous donors (C). (D) The RFI of negative antibodies was 1.5 or under, whereas that of weakly positive antibodies ranged from 1.6 to 2.9 and that of strongly positive antibodies was 3.0 and above. According to the results of RFI, 41 patients were classified into 3 groups: 12 antibody negative (○), group A), 13 antibody-weakly positive (group B), and 16 antibody-strongly positive (group C). Antibodies specificity in groups B and C are presented as follows: anti–HNA-1a, (●); anti–HNA-1b, (⊕); FcγRIIIb, (⊗); and inconclusive, (⊙).
Representative flow cytometric analysis for detecting antineutrophil antibodies and classification of patients.
All histograms showed the analysis of neutrophils, which were gated electronically in medium to high forward and orthogonal light scatter, and the green fluorescence of this population was collected. Data acquisition and analysis were performed with CellQuest software (Becton Dickinson Immunocytometry Systems) or ORTHO ImmunoCount II software (Ortho Diagnostic Systems). Various concentrations of TAG1 bind to HNA-1a–homozygous neutrophils and those of TAG2 to HNA-1b–homozygous neutrophils (A). The relative fluorescence intensity (RFI) of each concentration of TAG1 or TAG2 is presented (B). The representative flow cytometric findings of weakly positive and strongly positive sera were shown against 2 different HNA-1a–homozygous donors (C). (D) The RFI of negative antibodies was 1.5 or under, whereas that of weakly positive antibodies ranged from 1.6 to 2.9 and that of strongly positive antibodies was 3.0 and above. According to the results of RFI, 41 patients were classified into 3 groups: 12 antibody negative (○), group A), 13 antibody-weakly positive (group B), and 16 antibody-strongly positive (group C). Antibodies specificity in groups B and C are presented as follows: anti–HNA-1a, (●); anti–HNA-1b, (⊕); FcγRIIIb, (⊗); and inconclusive, (⊙).
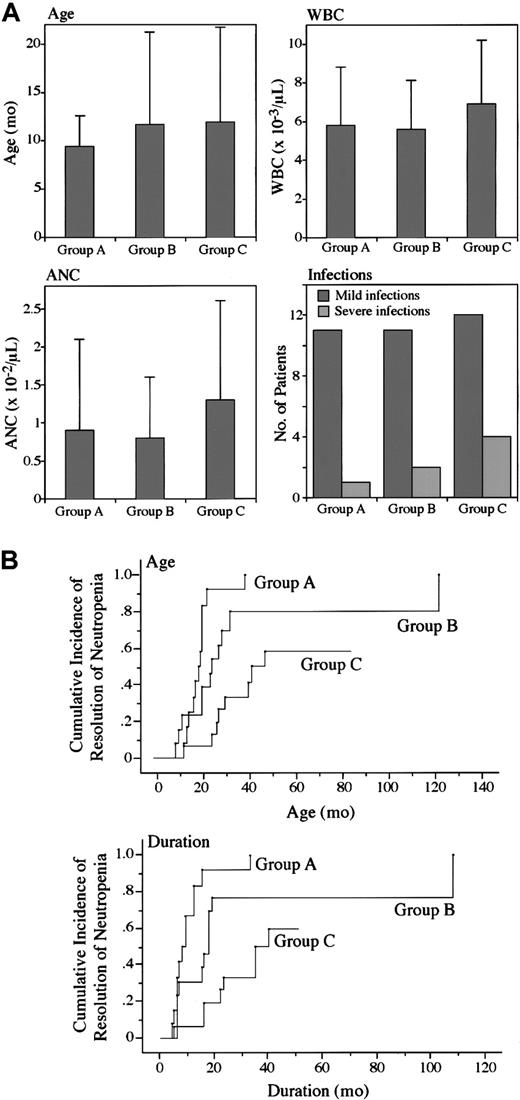
The clinical characteristics of patients in the 3 groups are presented in Figure 2A. There were no significant differences in the age of patients, the severity of leukopenia and neutropenia, and the frequency of infectious complications during the neutropenic period among 3 groups as determined by chi-squared test and Kruskal-Wallis test. These observations suggest that the clinical findings are similar in presentation among patients, irrespective of the results of antineutrophil antibody test. Most children with chronic neutropenia have a benign clinical course because neutropenia often spontaneously resolves.2-7 11 The spontaneous resolution of neutropenia was found up to 40 months of age in all patients of group A. Eleven of 13 patients in group B and 10 of 16 patients in group C showed recovery from neutropenia by July 2001. The clinical prognoses analyzed by the Kaplan-Meier method are presented in Figure2B. When the patients who have shown persistent neutropenia were defined as censor, the age of the recovery of neutropenia and the duration of neutropenia after the first documentation of neutropenia were significantly different among the 3 groups as determined by log-rank test. There were no significant differences in clinical characteristics among immunoglobulin class distribution of antibodies and among different antibody specificity shown in Figure 1D (data not shown).
Clinical characteristics in 3 groups of patients with neutropenia.
The age of diagnosis, white blood cell count, ANC, and the number of infectious episodes were compared among 3 groups (A). Data represent the mean ± SD in the age of diagnosis, white blood cell count, and ANC. The infectious complication showed the number of patients presenting mild or severe infections associated with neutropenia. Cumulative incidence of resolution of neutropenia is presented by age and duration of neutropenia in 3 groups (B). Statistical significance was determined by using the log-rank test. The values of statistical significance are as follows: group A versus group B, P < .05; group B versus group C,P < .05; group A versus group B plus group C,P < .01.
Clinical characteristics in 3 groups of patients with neutropenia.
The age of diagnosis, white blood cell count, ANC, and the number of infectious episodes were compared among 3 groups (A). Data represent the mean ± SD in the age of diagnosis, white blood cell count, and ANC. The infectious complication showed the number of patients presenting mild or severe infections associated with neutropenia. Cumulative incidence of resolution of neutropenia is presented by age and duration of neutropenia in 3 groups (B). Statistical significance was determined by using the log-rank test. The values of statistical significance are as follows: group A versus group B, P < .05; group B versus group C,P < .05; group A versus group B plus group C,P < .01.
CBN and AIN in childhood have presented similar hematologic characteristics. As suggested by several authors, it is likely that most of these cases are actually autoimmune in origin even though antineutrophil antibodies may not always be detected.3,4,7In the present study we introduced FACS analysis for indirect immunofluorescence test using a panel of donor neutrophils, including FcγRIIIb-deficient neutrophils, throughout this study to consistently quantify neutrophil-associated antibodies. Although no apparent differences in clinical and hematologic manifestations existed among the 3 groups of patients classified by the strength of antibodies, the duration of neutropenia after the first documentation of neutropenia is significantly dependent on the strength of the antibodies at the time of diagnosis. The precise mechanism to develop autoantibodies in children with AIN and/or CBN remains unclear. The temporary production of antibodies may result in the spontaneous disappearance of antineutrophil antibodies that preceded the resolution of neutropenia in most cases.2-7 11 It is possible that the primary concentration of antibodies may affect the duration of neutropenia.
It has been reported that some antibodies such as anti–HNA-3a are better detected by agglutination than by GIIFT.15Therefore, the combination of semiquantified GIIFT and agglutination test for detecting antineutrophil antibodies provide information for predicting the clinical course of children with chronic neutropenia. Further, a large prospective study is necessary to demonstrate that measurement of autoantibodies at the time of diagnosis will aid in observations of the natural history of this disorder.
We thank Dr Garrido, Granada University, Granada, Spain, for providing GRM1 and Dr Stroncek, National Institutes of Health, Bethesda, MD, for providing 7D8.
We also thank the following doctors for referring to us the valuable samples from patients with chronic neutropenia: M. Noguchi (Chiba); M. Maeda (Tokyo); M. Yoshida, T. Kudoh, M. Yagi, T. Katoh, M. Fukuda (Nagoya); T. Matsubayashi (Hamamatsu); F. Sofue (Okazaki); Y. Onoue (Itoigawa); H. Toyoda (Tsu); H. Hirata (Tsushima); J. Muroi, M. Naya (Kyoto); T. Sakano (Hiroshima); M. Iga, I. Okafuji (Izumo); A. Iwai (Kagawa); Y. Ishida (Matsuyama); Y. Ishiura, Y. Wakata (Kochi); M. Hirota (Kitakyuushu); and R. Ishihara (Okinawa).
Supported in part by Grants-in-Aid for Scientific Research (C) from the Ministry of Education, Science, Sports and Culture of Japan (M.K. and K.U.).
M.K. and K.N. contributed equally to this study and should both be regarded as first authors.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Masao Kobayashi, Department of Child Health, Hiroshima University Graduate School of Education, 1-1-1 Kagamiyama Higashi-Hiroshima, Hiroshima, 739-8524 Japan; e-mail:masak@hiroshima-u.ac.jp.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal