Abstract
To comparatively assess first-line treatment with fludarabine and 2 anthracycline-containing regimens, namely CAP (cyclophosphamide, doxorubicin plus prednisone) and ChOP (cyclophosphamide, vincristine, prednisone plus doxorubicin), in advanced stages of chronic lymphocytic leukemia (CLL), previously untreated patients with stage B or C CLL were randomly allocated to receive 6 monthly courses of either ChOP, CAP, or fludarabine (FAMP), stratified based on the Binet stages. End points were overall survival, treatment response, and tolerance. From June 1, 1990 to April 15, 1998, 938 patients (651 stage B and 287 stage C) were randomized in 73 centers. Compared to ChOP and FAMP, CAP induced lower overall remission rates (58.2%; ChOP, 71.5%; FAMP; 71.1%; P < .0001 for each), including lower clinical remission rates (CAP, 15.2%; ChOP, 29.6%; FAMP, 40.1%;P = .003). By contrast, median survival time did not differ significantly according to randomization (67, 70, and 69 months in the ChOP, CAP, and FAMP groups, respectively). Incidences of infections (< 5%) and autoimmune hemolytic anemia (< 2%) during the 6 courses were similar in the randomized groups, whereas fludarabine induced, compared to ChOP and CAP, more frequent protracted thrombocytopenia (P = .003) and less frequent nausea-vomiting (P = .003) and hair loss (P < .0001). For patients with stage B and C CLL first-line fludarabine and ChOP regimens both provided similar overall survival and close response rates, and better results than CAP. However, there was an increase in clinical remission rate and a trend toward a better tolerance of fludarabine over ChOP that may influence the choice between these regimens as front-line treatments in patients with CLL.
Introduction
Since 1980, the French Cooperative Group on Chronic Lymphocytic Leukemia (CLL) has conducted 3 multicenter prospective randomized clinical trials in previously untreated patients with CLL in which different therapeutic strategies were designed according to the baseline (A, B, C) Binet stage.1 The 2 first trials showed that a watch and wait policy could be applied to patients with stage A CLL.2 In the advanced forms of CLL (stages B and C), the optimal first-line treatment remains to be established. A clear-cut survival benefit over the COP (cyclophosphamide, vincristine [Oncovin] plus prednisone) of the ChOP regimen (COP plus doxorubicin, 25 mg/m2 intravenously [IV] on day 1) was observed in stage C patients from our first trial.3,4 Thereafter, its benefit in remission rate over chlorambucil was confirmed.5-8 Otherwise, different anthracycline-containing regimens using adriamycin at a higher dose (50 mg/m2 IV day 1) such as POACH (prednisone, vincristine, Ara-C, cyclophosphamide, doxorubicin)9 or CAP (cyclophosphamide, doxorubicin plus prednisone)10 have been reported to be effective in advanced forms of CLL. However, no comparison of these regimens to ChOP has been published.
During the late 1980s, fludarabine (FAMP) emerged as a major drug in CLL and generated tremendous interest. It was first used in patients with progressive and refractory CLL.11-15 It was later reported that fludarabine, either alone or combined with corticosteroids, could achieve high response rates with estimates ranging from 56% in previously treated to 80% in previously untreated patients.16-18 However, except for a multicenter European randomized clinical trial showing a benefit of fludarabine over CAP in terms of the 6-month response rate and progression-free interval in previously treated and untreated CLL patients,19 and a multicenter trial comparing FAMP to chlorambucil,20 no other large randomized trial assessing its efficacy has been conducted.
The current prospective randomized clinical trial was designed in 1990 to compare the effectiveness and tolerance of fludarabine to that of 2 anthracycline-containing regimens in previously untreated patients with stage B and C CLL. We report here the main results of this trial, based on 938 randomized patients with median follow-up of 70 months.
Patients, materials, and methods
Criteria for eligibility
Diagnosis of CLL was established according to the clinical and peripheral blood criteria defined by the International Workshop on CLL (IWCLL).21 Previously untreated stage B and stage C CLL patients, under age 75 years, were eligible for this trial. Those patients with concomitant neoplasm, autoimmune hemolytic anemia (AIHA), or prolymphocytic leukemia were excluded. The Ethics Committee of the Groupe Hospitalier Pitié-Salpêtrière (Paris, France) approved the protocol, and written informed consent was obtained for all patients.
Randomization and treatment schedule
From 73 participating centers, randomization was performed through a centralized telephone assignment procedure stratified by stage. Patients were randomly assigned to receive 6 monthly courses of either (1) ChOP, that is, vincristine IV 1 mg/m2 and doxorubicin IV 25 mg/m2 on day 1, plus cyclophosphamide 300 mg/m2 and prednisone 40 mg/m2 both given orally from day 1 to day 5; (2) CAP, that is, cyclophosphamide 750 mg/m2 IV, doxorubicin 50 mg/m2 IV on day 1 plus prednisone 40 mg/m2 orally from day 1 to day 5; or (3) FAMP, that is, fludarabine phosphate 25 mg/m2 IV daily for 5 days. The procedure was not blinded.
Patients receiving FAMP or CAP with stable or progressive disease after 3 cycles were recommended to switch to CAP or FAMP, respectively. Because the ChOP regimen consisted of lower doxorubicin doses, the 6 scheduled courses were carried out before assessing response; those with stable or progressive disease after 6 courses were then switched to FAMP.
End points
The main end point of the protocol was overall survival from randomization. Disease status after 6 courses or the last course before switching regimens defined a secondary end point. It was assessed by treatment response according to the National Cancer Institute (NCI) recommendation,22 segregating clinical remission, partial remission, and failures (Figure 1). Failure was defined by disease stabilization or progression during treatment or death either related to disease or to treatment toxicity that occurred within the first 12 months after randomization.
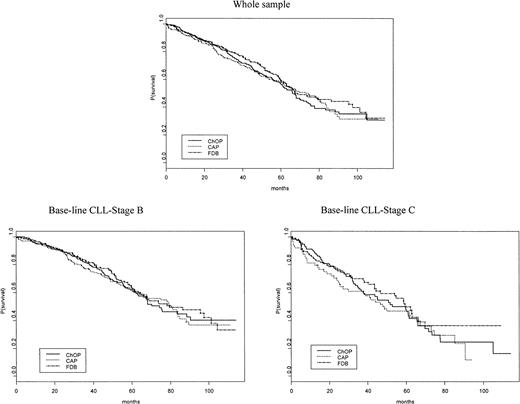
Overall survival.
Overall survival is shown according to randomization (ChOP, CAP, or FAMP) in either baseline Binet stage (B or C).
Overall survival.
Overall survival is shown according to randomization (ChOP, CAP, or FAMP) in either baseline Binet stage (B or C).
In addition, it was recommended to further assess clinical remission through the study in each center of bone marrow infiltration by bone marrow biopsy and by immunophenotypic study of blood lymphocytes based on double-labeling techniques with CD5 and CD19. For patients reaching both histologic remission (ie, absence of bone marrow lymphoid infiltrates) and immunophenotypic remission (ie, < 25% of the peripheral blood B lymphocytes coexpressing CD5/CD19), these investigations were completed by clonotypic reverse transcription-polymerase chain reaction.23 Bone marrow biopsies and immunophenotypic studies were not centrally reviewed. Computed tomograph scans and other imaging procedures, where available, were not taken into account for the staging procedure or the evaluation of response.
Time to progression after remission defined another secondary end point, with progression defined according to the NCI recommendations.22 Finally, time to second-line therapy after remission was also retained as an end point.
Adverse events observed at each course were recorded similarly using detailed case report forms by 2 independent observers in all centers, with grading of the events according to the World Health Organization (WHO) criteria.24
Sample size
Estimation of sample size was based on the method described by George and Desu.25 It was based on a first-type error of 0.05, a second-type error of 0.10 for a one-sided test, and an assumption of treatment benefit given by a 15% increase in 5-year survival with FAMP from 50% with the other regimens. Given the expected accrual of 100 patients per year, it was computed that 300 patients had to be recruited in each randomized group. Five interim analyses were planned. The first interim analysis, performed at January 1, 1996, as the reference date, showed significantly lower response rates and survival with CAP as compared to ChOP or FAMP, with inconclusive results regarding the comparison between ChOP and FAMP. Based on these results, the accrual in the CAP group was stopped on February 9, 1996.
Statistical analysis
Analysis was made on an intent-to-treat basis, using January 1, 2000, as the reference date (fourth interim analysis). Because randomization was stratified on Binet stage, treatment comparison of end points was stratified using Mantel-Haenszel test or stratified Cox model, which also allowed additionally adjusted survival comparison on prognostic or imbalanced covariates; unadjusted and adjusted relative risks of death (RR) with 95% confidence intervals (95CI) were estimated. P values of .05 or less indicated statistical significance. Statistical analysis was performed using the SAS software system (Statistical Analysis System, Cary, NC).
Results
From June 1, 1990 to April 15, 1998, 809 patients, 556 stage B and 253 stage C, from 73 hematology departments were enrolled in the trial; 1022 stage A patients were allocated to a watch and wait policy. Of the 1022 stage A patients, 137 evolved to either stage B (n = 100) or stage C (n = 37) before April 15, 1998, and were randomized into the trial. Five stage B and 3 stage C patients were excluded due to misdiagnosis (2 follicular lymphomas, 1 mantle cell lymphoma, 1 leukemic lymphoma); 3 patients refused treatment; and 1 refused previous treatment. Accordingly, 938 patients were randomized to receive either ChOP (357 patients), CAP (240 patients), or FAMP (341 patients), with 651 stage B patients allocated to either ChOP (n = 240), CAP (n = 175), or FAMP (n = 236) and 287 stage C patients to either ChOP (n = 117), CAP (n = 65), or FAMP (n = 105).
The discontinuation of accrual in the CAP group since February 9, 1996 explains the imbalances in sample sizes. Indeed, accrual in the CAP group was prematurely closed when results of the first interim analysis exhibited significant decreased response rates in the CAP group as compared to the ChOP and FAMP groups. This decision appeared reliable both from statistical and ethical viewpoints. Even though the retained type I error rate was not corrected for 5 interim analyses, the difference in response rates was clinically relevant, so that it appeared unethical to treat further patients with CAP.
Baseline characteristics
The main characteristics of the 938 patients in the 3 treatment groups and according to stage are reported in Table1. Randomization constituted comparable groups on average, except 4 imbalances, either in stage B (spleen involvement more frequently observed in the CAP group) or stage C (less frequent spleen involvement in the CAP group; higher blood lymphocytosis and lower incidence of bulky disease, ie, at least one lymph node with diameter > 4 cm or spleen below the umbilicus, in the ChOP group, as compared to remainder).
Baseline comparison of randomized groups according to stage and treatment
| . | Stage B . | Stage C . | ||||
|---|---|---|---|---|---|---|
| ChOP (n = 240) . | CAP (n = 175) . | FAMP (n = 236) . | ChOP (n = 117) . | CAP (n = 65) . | FAMP (n = 105) . | |
| Age, y (range) | 62 (55-67) | 60 (55-67) | 62 (53-67) | 64 (59-68) | 65 (58-71) | 63 (56-68) |
| Male | 76% | 69% | 74% | 66% | 53% | 69% |
| Involved areas | ||||||
| Cervical | 96% | 95% | 95% | 65% | 73% | 70% |
| Axillary | 94% | 93% | 96% | 62% | 72% | 61% |
| Inguinal | 85% | 78% | 77% | 50% | 53% | 49% |
| Spleen | 52% | 66% | 59% | 75% | 64% | 78% |
| Liver | 12% | 16% | 14% | 15% | 23% | 22% |
| Bulky disease* | 25% | 26% | 24% | 20% | 30% | 33% |
| Hemoglobin (g/L) | 134 (123-143) | 133 (120-143) | 135 (123-145) | 91 (81-101) | 94.5 (82.5-115) | 95 (77-115) |
| Platelets (109/L) | 184 (148-226) | 180 (141-228) | 176 (148-217) | 90 (68-126) | 92.5 (66-125.5) | 88 (71-115) |
| Lymphocytes | ||||||
| Blood (109/L) | 40.7 (19.2-90.2) | 49 (22-90.7) | 50.5 (19-88.3) | 76.3 (31-165) | 59.3 (28-194) | 58.6 (22-111) |
| Medullary (%) | 77 (63-86) | 80 (67-89) | 80 (65-86) | 91 (83-95) | 90 (80.5-94) | 86 (75.5-93.5) |
| . | Stage B . | Stage C . | ||||
|---|---|---|---|---|---|---|
| ChOP (n = 240) . | CAP (n = 175) . | FAMP (n = 236) . | ChOP (n = 117) . | CAP (n = 65) . | FAMP (n = 105) . | |
| Age, y (range) | 62 (55-67) | 60 (55-67) | 62 (53-67) | 64 (59-68) | 65 (58-71) | 63 (56-68) |
| Male | 76% | 69% | 74% | 66% | 53% | 69% |
| Involved areas | ||||||
| Cervical | 96% | 95% | 95% | 65% | 73% | 70% |
| Axillary | 94% | 93% | 96% | 62% | 72% | 61% |
| Inguinal | 85% | 78% | 77% | 50% | 53% | 49% |
| Spleen | 52% | 66% | 59% | 75% | 64% | 78% |
| Liver | 12% | 16% | 14% | 15% | 23% | 22% |
| Bulky disease* | 25% | 26% | 24% | 20% | 30% | 33% |
| Hemoglobin (g/L) | 134 (123-143) | 133 (120-143) | 135 (123-145) | 91 (81-101) | 94.5 (82.5-115) | 95 (77-115) |
| Platelets (109/L) | 184 (148-226) | 180 (141-228) | 176 (148-217) | 90 (68-126) | 92.5 (66-125.5) | 88 (71-115) |
| Lymphocytes | ||||||
| Blood (109/L) | 40.7 (19.2-90.2) | 49 (22-90.7) | 50.5 (19-88.3) | 76.3 (31-165) | 59.3 (28-194) | 58.6 (22-111) |
| Medullary (%) | 77 (63-86) | 80 (67-89) | 80 (65-86) | 91 (83-95) | 90 (80.5-94) | 86 (75.5-93.5) |
Median values (25th-75th percentiles) are given for continuous variables; percentages are reported for categorical variables.
Bulky disease is clinically defined on the basis of at least one lymph node with diameter greater than 4 cm or spleen below the umbilicus or both.
Treatment response at 6 months
Of the 938 randomized patients, 24 (2.6%) did not receive the scheduled chemotherapy (Table 2). Table3 reports the distribution of treatment response according to randomization group and baseline Binet stage and segregating clinical remissions, partial remissions, and failures. The CAP group exhibited the lowest remission rates, notably clinical remission rates (15.2% versus 29.6% in the ChOP group and 40.1% in the FAMP group; P = .003 by the Mantel-Haenszel test). Stratified paired comparisons showed a marked difference of both ChOP and FAMP against CAP in terms of distribution of response and clinical remission (each with P < .0001 by the Mantel-Haenszel test), and of FAMP over ChOP in terms of distribution of response (P = .003) explained by a higher rate of and clinical remission (P = .004). Finally, the global rate (unstratified) of clinical remission was also higher in the FAMP group than that reached with ChOP (P = .004), and CAP (P < .0001).
Protocol follow-up on 938 randomized patients
| . | ChOP, no.* . | CAP, no.† . | FAMP, no.‡ . |
|---|---|---|---|
| Did not receive scheduled chemotherapy as allocated (reason) | 11 | 8 | 5 |
| Early death2-153 | 2 | 1 | 1 |
| Patient refusal | 2 | 1 | 1 |
| Lost to follow-up | 4 | 2 | 2 |
| Stage A improved | 2 | 1 | — |
| Richter syndrome2-155 | 1 | — | 1 |
| Contraindication | — | 3 | — |
| Received 1 or 2 courses of scheduled chemotherapy as allocated (reason) | 2 | 7 | 4 |
| Early death2-153 | 3 | 3 | 3 |
| Therapy ineffective2-153 | 3 | 2 | 2 |
| Toxicity | 2 | — | 1 |
| Lost to follow-up | 1 | — | 1 |
| Patient refusal | |||
| Completed at least 3 courses of scheduled chemotherapy | 335 | 220 | 308 |
| Switches at third to sixth course2-154 | 41 | 56 | 31 |
| . | ChOP, no.* . | CAP, no.† . | FAMP, no.‡ . |
|---|---|---|---|
| Did not receive scheduled chemotherapy as allocated (reason) | 11 | 8 | 5 |
| Early death2-153 | 2 | 1 | 1 |
| Patient refusal | 2 | 1 | 1 |
| Lost to follow-up | 4 | 2 | 2 |
| Stage A improved | 2 | 1 | — |
| Richter syndrome2-155 | 1 | — | 1 |
| Contraindication | — | 3 | — |
| Received 1 or 2 courses of scheduled chemotherapy as allocated (reason) | 2 | 7 | 4 |
| Early death2-153 | 3 | 3 | 3 |
| Therapy ineffective2-153 | 3 | 2 | 2 |
| Toxicity | 2 | — | 1 |
| Lost to follow-up | 1 | — | 1 |
| Patient refusal | |||
| Completed at least 3 courses of scheduled chemotherapy | 335 | 220 | 308 |
| Switches at third to sixth course2-154 | 41 | 56 | 31 |
Total, 357.
Total, 240.
Total, 341.
Early deaths and early stops due to inefficacy were considered as treatment failures.
Diagnosis is based on needle lymph node aspiration and aspect of large cell lymphoma on histologic examination.
Due to treatment inefficacy and thus considered as treatment failures.
Treatment response after 6 courses (or at switch during the 6 courses) according to randomization and baseline stage B or C
| . | ChOP3-150(%) . | CAP3-151 (%) . | FAMP3-152 (%) . |
|---|---|---|---|
| All patients | |||
| Clinical remission | 104 (29.6) | 36 (15.2) | 135 (40.1) |
| Partial remission | 147 (41.9) | 102 (43.0) | 104 (31.0) |
| Failure3-153 | 100 (28.5) | 99 (41.8) | 97 (28.9) |
| Baseline stage B | |||
| Clinical remission | 70 (29.4) | 28 (16.1) | 96 (41.2) |
| Partial remission | 114 (47.9) | 80 (46.0) | 81 (34.8) |
| Failure3-153 | 54 (22.7) | 66 (37.9) | 56 (24.0) |
| Baseline stage C | |||
| Clinical remission | 34 (30.1) | 8 (12.7) | 39 (37.9) |
| Partial remission | 33 (29.2) | 22 (34.9) | 23 (22.3) |
| Failure3-153 | 46 (40.7) | 33 (52.4) | 41 (39.8) |
| . | ChOP3-150(%) . | CAP3-151 (%) . | FAMP3-152 (%) . |
|---|---|---|---|
| All patients | |||
| Clinical remission | 104 (29.6) | 36 (15.2) | 135 (40.1) |
| Partial remission | 147 (41.9) | 102 (43.0) | 104 (31.0) |
| Failure3-153 | 100 (28.5) | 99 (41.8) | 97 (28.9) |
| Baseline stage B | |||
| Clinical remission | 70 (29.4) | 28 (16.1) | 96 (41.2) |
| Partial remission | 114 (47.9) | 80 (46.0) | 81 (34.8) |
| Failure3-153 | 54 (22.7) | 66 (37.9) | 56 (24.0) |
| Baseline stage C | |||
| Clinical remission | 34 (30.1) | 8 (12.7) | 39 (37.9) |
| Partial remission | 33 (29.2) | 22 (34.9) | 23 (22.3) |
| Failure3-153 | 46 (40.7) | 33 (52.4) | 41 (39.8) |
Response was not available in some patients due to loss to follow-up or nonevaluation of response in some untreated patients.
Randomized, n = 357; evaluable, n = 351.
Randomized, n = 240; evaluable, n = 237.
Randomized, n = 341; evaluable, n = 336.
Stabilization, progression, or early death.
To further assess the treatment response of the 275 patients achieving clinical remission, bone marrow histology and blood lymphocyte phenotype were examined concomitantly. Bone marrow histology, assessed in 135 patients, exhibited a normalization in 13 of 42 (31%) patients from the ChOP group, 3 of 19 (16%) in the CAP group, and 15 of 74 (20%) in the FAMP group (P = .31 by the Mantel-Haenszel test). Given the lack of evaluation of bone marrow response in 140 patients in clinical response, and according to the recently published NCI–working group (WG) guidelines,22 these cases could not be assessed as complete remissions. Therefore, in the proportion of patients actually fulfilling the NCI criteria of complete remission were 9%, 2%, and 8% of the ChOP, CAP, and FAMP groups, respectively.
Residual CD5/CD19 lymphocytes, studied in 95 patients in clinical response, exhibited normal values in 14 of 29 (48%) in the ChOP group, 3 of 9 (33%) in the CAP group, and 28 of 57 (49%) in the FAMP group (P = .67 by the Mantel-Haenszel test). Seventy-one patients were assessable for both methods. Complete clearance of bone marrow lymphoid infiltrates and CD5/CD19 lymphocytes from the blood could be substantiated in only 9 patients. In the remaining cases, results are either dissociated (ie, 29 patients have persistent bone marrow infiltration and a normal blood proportion of CD5/CD19 lymphocytes, 7 have persistent CD5/CD19 excess in blood and a normal bone marrow) or indicate persistent abnormal lymphocytes in blood and in bone marrow (26 cases).
Of the 296 failures, 128 switched within the first 6 courses or at the sixth course (Table 2), 41 in the ChOP group (all to FAMP), 56 in the CAP group (all to FAMP but 3 to ChOP), and 31 in the FAMP group (all to CAP but 3 to ChOP). Of the 196 failures observed in the CAP (n = 99) and FAMP (n = 97) groups, 87 were observed after 3 courses and accordingly switched, namely, 56 of 99 (56.6%) in the CAP group and 31 of 97 (31.9%) in the FAMP group. Of the 128 switches, subsequent response was available in 121; response was achieved in 55 patients (45%), including 14 (11%) clinical remissions and 41 partial remissions. In patients switched from ChOP (to FAMP), 6 clinical remissions and 11 partial remissions were observed as compared, respectively, to 6 and 20 from CAP (to FAMP), and 2 and 10 from FAMP (to anthracycline-containing regimens).
Survival
The median follow-up was 70 months. Figure 1 displays the estimated overall survival at the reference date, according to randomization group. Of the 938 patients, 391 died, 140 in the ChOP group (median survival, 67 months), 125 in the CAP group (median survival, 70 months), and 126 in the FAMP group (median survival, 69 months), with 5-year survival rates of 57.3% (95CI, 51.0%-63.6%), 59.8% (95CI, 53.4%-66.2%), and 58.4% (95CI, 51.9%-64.9%), respectively (P = .38 by the log-rank test). Causes of death were mostly related to CLL (299 of 372 of known causes), whatever the treatment group, either ChOP (107 of 136), CAP (97 of 118), or FAMP (95 of 118). Comparison of overall survival stratified on baseline stage, that is, incorporating the baseline stage as a potential source of variability, did not differ between the 3 randomized groups (P = .43 by the likelihood ratio test). Paired comparisons exhibited a trend toward a higher risk of death in the CAP versus FAMP group (RR = 1.22; 95CI, 0.95%-1.57%; P = .11), whereas estimates were close for CAP versus ChOP (RR = 1.10; 95CI, 0.86%-1.40%; P = .44) and FAMP versus ChOP (RR = 0.95; 95CI, 0.84%-1.07%; P = .41). Estimated relative risk of death were slightly erased after adjustment on baseline age, WHO scale, lymphocytosis, and hemoglobin level, as follows: CAP versus FAMP (RR = 1.08; 95CI, 0.84%-1.39%; P = .56), CAP versus ChOP (RR = 1.07; 95CI, 0.84%-1.37%; P = .57), and FAMP versus ChOP (RR = 0.99; 95CI, 0.88%-1.12%;P = .93).
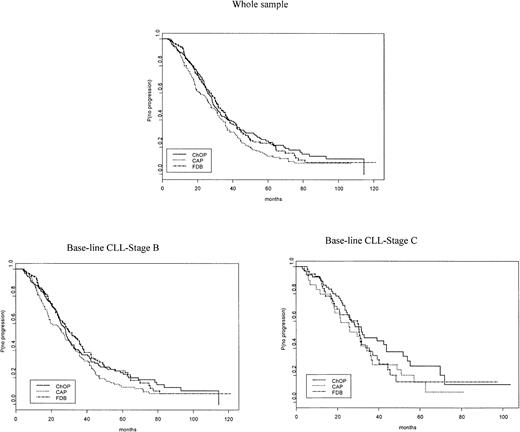
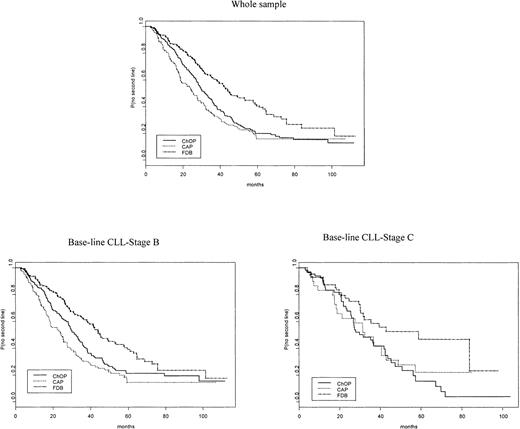
Time to progression, second-line treatment
Of the 628 patients who reached remission either partially (n = 353) or clinically (n = 275), 442 disease progressions were subsequently recorded according to the NCI criteria (Table4). There were slight differences according to randomization group: 166 of 247 in the ChOP group (median time, 29.5 months), 117 of 138 in the CAP group (median time, 27.7 months), and 159 of 239 in the FAMP group (median time, 31.7 months;P = .09; Figure 2). A total of 391 patients received a second-line treatment after remission, but, interestingly, time to second-line therapy was different between randomized groups: 165 of 247 in the ChOP group (median time, 32.2 months), 108 of 138 in the CAP group (median time, 25.7 months), and 118 of 239 in the FAMP group (median time, 45.4 months; P < .0001; Figure 3).
Criteria for treatment response as assessed after (or within) 6 courses
| . | Criterion . |
|---|---|
| Clinical remission | |
| Lymph node, spleen, and liver enlargement (clinical) | Absent |
| Lymphocytosis | < 4.109/L |
| Neutrophils | ≥ 1.5 109/L |
| Platelets | ≥ 100 109/L |
| Hemoglobin level | ≥ 110 g/L |
| Partial remission | |
| Decrease in lymph node, spleen, and liver enlargement | > 50% |
| Decrease in lymphocytosis | > 50% from baseline value |
| Neutrophils | > 1.5 109/L or increased by 50% from baseline value |
| Platelets | > 100 109/L or increased by 50% from baseline value |
| Hemoglobin level | > 110 g/L or increased by 50% from baseline value |
| Stable disease | |
| Response or progression | Absent |
| Progressive disease | |
| Increase in lymph node, spleen, or liver volume | > 50% or new involvement of these organs |
| Increase in lymphocytosis | > 50% from baseline value |
| Neutrophils | < 1.5 109/L or decreased by 50% from baseline value |
| Platelets | < 100 109/L or decreased by 50% from baseline value |
| Hemoglobin level | < 110 g/L or decreased by 50% from baseline value |
| . | Criterion . |
|---|---|
| Clinical remission | |
| Lymph node, spleen, and liver enlargement (clinical) | Absent |
| Lymphocytosis | < 4.109/L |
| Neutrophils | ≥ 1.5 109/L |
| Platelets | ≥ 100 109/L |
| Hemoglobin level | ≥ 110 g/L |
| Partial remission | |
| Decrease in lymph node, spleen, and liver enlargement | > 50% |
| Decrease in lymphocytosis | > 50% from baseline value |
| Neutrophils | > 1.5 109/L or increased by 50% from baseline value |
| Platelets | > 100 109/L or increased by 50% from baseline value |
| Hemoglobin level | > 110 g/L or increased by 50% from baseline value |
| Stable disease | |
| Response or progression | Absent |
| Progressive disease | |
| Increase in lymph node, spleen, or liver volume | > 50% or new involvement of these organs |
| Increase in lymphocytosis | > 50% from baseline value |
| Neutrophils | < 1.5 109/L or decreased by 50% from baseline value |
| Platelets | < 100 109/L or decreased by 50% from baseline value |
| Hemoglobin level | < 110 g/L or decreased by 50% from baseline value |
Disease progression.
Time to disease progression is shown using the IWCLL criteria (Figure1) after remission according to randomization (ChOP, CAP, FAMP) and baseline Binet stage (B or C).
Disease progression.
Time to disease progression is shown using the IWCLL criteria (Figure1) after remission according to randomization (ChOP, CAP, FAMP) and baseline Binet stage (B or C).
Second-line therapy.
Time to second-line therapy in responders is shown, according to randomization (ChOP, CAP, FAMP) and baseline Binet stage (B or C).
Second-line therapy.
Time to second-line therapy in responders is shown, according to randomization (ChOP, CAP, FAMP) and baseline Binet stage (B or C).
Of note, a total of 596 (79%) patients received at least one course of fludarabine over their follow-up, either in the ChOP group (n = 136, 38%), the CAP group (n = 130, 54%), or the FAMP group (n = 336, 99%).
Side effects
Percentages of patients with at least one grade 3 adverse event observed within the first 6 courses of chemotherapy according to the randomization group are reported in Table 5.
Percentages of patients with at least one grade 3 adverse event observed within the first 6 courses of chemotherapy according to randomization group
| . | ChOP5-150 (%) . | CAP5-151(%) . | FAMP5-152 (%) . | P . |
|---|---|---|---|---|
| Biologic events | ||||
| Anemia | 57 (16) | 25 (10) | 57 (18) | .04 |
| AIHA | 3 (1) | 0 | 6 (2) | .07 |
| Neutropenia | 131 (38) | 71 (30) | 122 (38) | .06 |
| Thrombocytopenia5-153 | 29 (8) | 18 (7) | 49 (15) | .003 |
| ALT or AST ≥ twice baseline | 1 (1) | 2 (1) | 4 (1) | .40 |
| Clinical events | ||||
| Hemorrhage | 4 (2) | 0 | 2 (1) | .23 |
| Nausea, vomiting | 6 (1) | 13 (5) | 3 (1) | .003 |
| Alopecia | 54 (16) | 35 (15) | 0 | < .0001 |
| Infection5-155 | 17 (5) | 10 (4) | 16 (5) | .90 |
| Unexplained fever | 0 | 1 (1) | 7 (4) | .05 |
| Cardiac disorder | 2 (1) | 4 (2) | 0 | .04 |
| Neurologic disorder5-154 | 1 (1) | 2 (1) | 0 | .27 |
| Hospitalizations | 66 (19) | 32 (15) | 74 (23) | .06 |
| . | ChOP5-150 (%) . | CAP5-151(%) . | FAMP5-152 (%) . | P . |
|---|---|---|---|---|
| Biologic events | ||||
| Anemia | 57 (16) | 25 (10) | 57 (18) | .04 |
| AIHA | 3 (1) | 0 | 6 (2) | .07 |
| Neutropenia | 131 (38) | 71 (30) | 122 (38) | .06 |
| Thrombocytopenia5-153 | 29 (8) | 18 (7) | 49 (15) | .003 |
| ALT or AST ≥ twice baseline | 1 (1) | 2 (1) | 4 (1) | .40 |
| Clinical events | ||||
| Hemorrhage | 4 (2) | 0 | 2 (1) | .23 |
| Nausea, vomiting | 6 (1) | 13 (5) | 3 (1) | .003 |
| Alopecia | 54 (16) | 35 (15) | 0 | < .0001 |
| Infection5-155 | 17 (5) | 10 (4) | 16 (5) | .90 |
| Unexplained fever | 0 | 1 (1) | 7 (4) | .05 |
| Cardiac disorder | 2 (1) | 4 (2) | 0 | .04 |
| Neurologic disorder5-154 | 1 (1) | 2 (1) | 0 | .27 |
| Hospitalizations | 66 (19) | 32 (15) | 74 (23) | .06 |
ALT indicates alanine aminotransferase; AST, aspartate aminotransferase.
Total, 357.
Total, 240.
Total, 341.
Two patients (one in the ChOP group, one in the FAMP group) discontinued treatment after a single course due to thrombocytopenic purpura.
One patient stopped treatment due to severe pneumonia after one course of CAP.
One patient discontinued treatment due to encephalopathy after one course of CAP.
Twenty treatment-related deaths were reported, including 5 in the ChOP group, 8 in the CAP group, and 7 in the FAMP group. Six of these deaths were due to infection secondary to aplasia, 1 in the ChOP group, 1 in the CAP group, and 4 in the FAMP group.
A total of 130 patients had a positive Coombs test over the follow-up, including 38 AIHA—17 in the ChOP group, 11 in the CAP group, and 10 in the FAMP group (P = .41). AIHA was infrequent during the first 6 scheduled courses, occurring in 3 patients with ChOP and 6 with FAMP. However, AIHA occurred during the follow-up in 29 other patients, 14 in the ChOP arm, 11 in the CAP arm, and 4 in the FAMP arm. Interestingly, 20 of 25 patients from the CAP and ChOP arms developed AIHA after they received FAMP as a subsequent treatment, because of the switch in case of failure with anthracycline regimens or later after recurrence of the disease.
As expected, no alopecia and a lower rate of nausea were observed in the FAMP group as compared to the ChOP and CAP groups. By contrast, there was an increase in cytopenia rates in the FAMP group as compared to the other regimen groups, either in the hemoglobin level (P = .04) or the platelet counts (P = .003).
Discussion
This prospective controlled trial comparing 3 regimens in previously untreated patients with advanced stage CLL is the largest study conducted so far in the literature.
Considering treatment response, fludarabine and ChOP were clearly superior to CAP. This was observed since the first interim analysis of this trial and caused the cessation of accrual in the CAP arm thereafter. Compared to the ChOP regimen, fludarabine provided a similar remission rate, but a higher clinical–partial remission ratio, whatever the baseline stage of the patients. These findings are close to those of previously published trials evaluating fludarabine or anthracycline-containing regimens in cohorts of previously untreated patients: 56% remission with POACH,9 66% with CAP,10,19 70% with ChOP,5,7,8 70% to 77% with fludarabine in comparative trials,19,20,26 and up to 80% in noncomparative ones.27 Otherwise, 2′-chloro-desoxy-adenosine, another purine analogue, exhibited similar remission rates (25% clinical response and 60% partial response rates) in previously untreated CLL patients.28
The reasons accounting for the lower clinical and even partial response rates observed with CAP compared to ChOP are not clear as yet. Comparison between the 2 treatments shows that in the CAP schedule, the dose of Adriamycin is twice and cyclophosphamide is given IV on day 1, whereas the CHOP regimen includes vincristine, and a double dose of cyclophosphamide given orally on 5 consecutive days. This last difference could be more appropriate for CLL treatment if we consider the low proliferative activity of the tumor cells in this disease.
In patients with clinical remission, clearances of bone marrow lymphocytic infiltration and of blood CD5+/CD19+ cells were often dissociated when tested in the same patient. This raises the possibility of categorical types of remission, which confuses the definition of so-called clinical remission. In addition, using a specific clonal probe,23 residual clonal disease could be substantiated at the molecular level in peripheral blood lymphocytes in every patient displaying both a normal bone marrow histology and a normal blood lymphocyte immunophenotype (data not shown). Similar observations have been reported within a group of CLL patients reaching remission after 2′-chloro-desoxy-adenosine courses.29
The differences in remission rates did not translate into differences in survival. This is not surprising because, whatever the randomization group, a majority of included patients received a second and even subsequent treatment lines over the course of their disease, obscuring the interpretation of the survival curves. Similar conclusions were outlined in 2 other large prospective multicenter studies conducted in CLL. In the trial conducted by a US intergroup, fludarabine and chlorambucil were compared in patients with previously untreated stage I to IV B CLL; the response rates and time to progression were clearly improved with fludarabine, but again, and unexpectedly, overall survival curves were similar.20 Another recently published prospective randomized trial comparing 2-chloro-deoxyadenosine plus prednisone with chlorambucil plus prednisone in previously untreated patients also fails to demonstrate a difference in overall survival in patients allocated into these 2 regimens.30
It is of interest to note prolongation of median survival time (79 months for stage B and 58.5 months for stage C CLL patients) as compared with our previous trials.3-6 Whether fludarabine could account in this observation is supported by a trend to a lower and delayed proportion of patients requiring a second-line treatment in the FAMP arm as compared to CAP or ChOP.
In the current trial, patients receiving anthracycline-containing regimens experienced a higher frequency and severity of nausea and vomiting, as well as alopecia and complete hair loss. In contrast, myelosuppression appeared to predominate among patients in the FAMP group. Persistent thrombocytopenia or neutropenia related to fludarabine were observed, sometimes far from the last course, in some patients who concomitantly had a normalized peripheral lymphocyte count. This confounded the staging of treatment response in these patients, given they could not be considered as in remission owing to the used cutoff levels of platelet and neutrophil counts in that definition.
Otherwise, opportunistic infections31-33 and AIHA34,35 have been frequently associated with fludarabine treatment in the case of patients having received previous chemotherapy. By contrast, opportunistic infections were absent and AIHA infrequently recorded during the first 6 treatment courses in our series. This could be related to the fact that FAMP was administered to previously untreated CLL patients.
In summary, fludarabine is not a curative agent for CLL. Nevertheless, when compared to ChOP, fludarabine displays some advantages, including improved tolerance, higher clinical remission rate, and delayed time to retreatment, which can argue for the choice of this drug as a front-line treatment in patients with previously untreated advanced CLL. This should be counterbalanced with the absence of overall survival benefit.
We would like to thank Dominique Meffre and Cécile Dumont-Pavis for their helpful technical assistance.
French Cooperative Group on CLL
Chairman:
J. L. Binet.
Advisory Board: Cl.
Chastang, G. Dighiero, M. Leporrier, Ph. Travade Statistical Center: Département de Biostatistique et Informatique Médicale, Hôpital saint-Louis, Paris. Cl. Chastang, S. Chevret (statisticians); C. Dumont-Pavis, D. Meffre (monitors); S. Gourdain, S. Ballester (secretary).
Investigators (alphabetic order of cities and names of participating physicians):
Alger: N. Boudjerra; Amiens: B. Desablens, J.-F. Claisse; Annecy: D. Martin; Antibes: J.-F. Dor; Avignon: G. Lepeu, A.-M. Touchais; Bayonne: M. Renoux, F. Bauduer; Clichy: J. Brière; Besançon: J.-Y. Cahn, A. Brion, E. Deconninck; Bicêtre: G. Tertian, G. Tchernia, P. D'Oiron; Blois: Ph. Rodon; Bobigny: P. Casassus, N. Vigneron; Bondy: F. Lejeune; Bordeaux: J.F. Eghbali; Brest: J.F. Abgrall; Bruxelles: D. Bron; Caen: M. Leporrier; Cannes: H. Nesman; Châlons sur Sâone: B. Salles; Chambéry: M. Blanc; Clamart; A. Herrera; Clermont-Ferrand: Ph. Travade; Colombes: F. Teillet; Corbeil: A. Devidas; Créteil: M. Diviné; Evreux: H. Bourgeois; Le Havre: F. Durand, W. Godefroy; Laval: D. Jacomy; Lens: D. Dupriez, P. Morel; Libourne: J. Ceccaldi; Lille: B. Cazin; Limoges: D. Bordessoule, D. Preux; Lons-le-Saunier: B. Duvert; Lyon: B. Coiffier, C. Sebban; A. Troncy; Le Mans: Ph. Solal-Celigny, M. Combes; Marseille: A.-M. Stoppa, R. Bouabdallah; Martigues: M. Nezri; Meaux: C. Allard; Metz: B. Christian; Montfermeil: A. Consoli; Montpellier: M. Navarro; Nancy: P. Renaudier, P. Feugier, J-F. Paitel; Nantes: D. Roge, M.-J. Rapp, A. Bataille-Zagury, Y. Le Mevel-Le Pourhiet, M. Hamidou; Nice: J.P. Cassuto, A. Thyss, Ch. Garnier; Nı̂mes: J.-F. Schved, A. Arnaud, J.-C. Gris; Orléans: G. Vaugier, V. Lucas; Perpignan: J. Camo; Paris Bichat: M.-J. Grange; Paris Lariboisière: J.-F. Zini; Paris Pitié-Salpêtrière: J.-L. Binet, K. Maloum; Paris Saint-Antoine: C. Chéron; Paris Saint-Joseph: J.M. James; Paris Saint-Louis: Ch. Gisselbrecht, Y. Najean, P. Brice, J.-P. Fermand; Poitiers: B. Dreyfus, C. Delaunay; Pontoise: M.C. Facquet-Danis, G. Philippe; Reims: B. Pignon, A.-M. Blaise; Rennes: R. Leblay, B. Grosbois, P.Y. Le Prisé, Ch. Ghandour; La Roche sur Yon: A. Maisonneuve; Rouen: D. Lenain, H. Tilly, H. Piguet; Saint Brieuc: I. Yakoub-Agha; Saint-Cloud: F. Turpin, M. Janvier; Saint-Etienne: J. Jaubert; Saint Germain en Laye: Y. Azagury; Sao Paulo: E. Criquet; Saumur: M. Maigre; Tours: C. Linassier, Ph. Colombat; Valenciennes: J.P. Pollet, M. Simon; Vichy: A. Régnier; Villejuif: P. Carde.
Submitted September 12, 2000; accepted June 11, 2001.
Supported by grants from Programme Hospitalier de Recherche Clinique (Ministère de la Santé), Association pour la Recherche Contre le Cancer (no. 6531), Donation Georgelin and Schering SA, France. A complete list of the members of the French Cooperative Group on Chronic Lymphocytic Leukemia is given at the end of this article.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Michel Leporrier, Service d'Hématologie, CHU Caen, Avenue Georges Clémenceau, 14 033 Caen Cedex, France; e-mail: leporrier-m@chu-caen.fr.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal