Clinical observations indicate that elderly people are prone to severe, often lethal infectious diseases induced by novel pathogens. Since the ability to mount primary immune responses relies on the availability of naive T cells, the circulating naive T-cell reservoir was evaluated throughout the human life span. Naive T cells were identified as CD95− T lymphocytes for their phenotypic and functional features. Indeed, the lack of CD95 marker is sufficient to identify a population of naive T cells, as defined by coincidence with previously characterized CD45RA+ CD62L+ T cells. Naive CD95− T cells, as expected, require a costimulatory signal, such as CD28, to optimally proliferate after anti-CD3 stimulation. Cytofluorimetric analysis of circulating T lymphocytes from 120 healthy subjects ranging in age from 18 to 105 years revealed that naive T cells decreased sharply with age. The younger subjects had a naive T-lymphocyte count of 825 ± 48 cells/μL, and the centenarians had a naive T-lymphocyte count of 177 ± 28 cells/μL. Surprisingly, the naive T-cell count was lower in CD8+than in CD4+ subsets at any age, and the oldest individuals were almost completely depleted of circulating naive CD8+ T cells (13 ± 4 cells/μL). Concomitantly, a progressive expansion of CD28− T cells occurs with age, which can be interpreted as a compensatory mechanism. These data provide new insights into age-related T-cell–mediated immunodeficiency and reveal some analogies of T-cell dynamics between advanced aging and human immunodeficiency virus (HIV) infection. In conclusion, the exhaustion of the naive CD8+ T-cell reservoir, which has never been reported before, suggests that this T-cell pool is a major target of the aging process and may define a parameter possibly related to the life span of humans.
Many studies have suggested a correlation between immune function and age-related risk of morbidity and mortality, although the contribution of the immune system to survival and human life span has not been fully elucidated.
Clinical evidence indicates that with advancing age, immune responses against recall antigens may still be conserved,1 but the ability to mount primary immune responses against novel antigens declines significantly.2 The impaired ability to mount immune responses to new antigens may result in a high susceptibility to infectious diseases and may limit the efficacy of vaccination strategies in elderly people. Although several age-related modifications of the immune system have been described so far, no single immune parameter seems to account for this age-related failure.3-6
The immune responses to novel antigens rely on the availability of naive T cells. In order to mount primary responses to new antigens even in advanced age, ie, a long time after the onset of thymic atrophy,7 naive T cells have to survive as long-lived resting cells from the time of their initial release from the thymus. Based on this assumption, the life span of these T cells in humans should reach several decades, especially when considering very old people such as centenarians. Alternatively, it should be hypothesized that in advanced age, naive T cells may still be provided by thymic remnants8-10 and/or by other organs which take over the thymus or by peripheral thymic-independent pathways.11 In any event, the evaluation of a naive T-cell reservoir represents a major task and should give insights into the mechanisms underlying the changes occurring in the immune system with age.
The phenotypic identification of truly naive T cells is still controversial. Several markers have been alternatively proposed for this task. The minimal requirement for the phenotypical definition of naive T cells seems to be the resting state, ie, lack of activation antigens and low-level expression of adhesion molecules.12,13 On the other hand, the most reliable marker to distinguish naive from nonnaive cells should be specifically and irreversibly acquired (or lost) after productive T-cell–receptor (TCR) engagement followed by clonal expansion, but not after exposure to cytokines.14 Until a few years ago, this requirement seemed to be met by CD45 isoforms,15 and indeed these markers have been widely used for this purpose. However, recent findings indicate that the CD45RO isoform can back-revert to CD45RA,16,17 whereas CD45RO can be induced after prolonged exposure to interleukin-2 (IL-2) in vitro.18,19 These data indicate that the distinction between naive and memory T cells, according to CD45 isoforms, is not satisfactory. Recently, double labeling with CD45RA and CD62L was shown to accurately identify naive T cells in HIV-infected subjects,20-22 and currently this double staining procedure may be considered as a standard for the phenotypic assessment of naive T cells in humans.
In this paper we have focused on the CD95 activation antigen (Ag), which is a member of the tumor necrosis factor/nerve growth factor–R (TNF/NGF-R) family.23,24 Most of the literature on CD95 is devoted mainly to cells expressing this molecule. CD95 is expressed on peripheral blood T cells after TCR/CD3 stimulation in vitro.25,26 Moreover, in vivo studies indicate that after antigen stimulation, T cells accumulate within the CD95+subset.27 Furthermore, in adults, CD95 is preferentially expressed by CD45RA−RO+ T cells but not by CD45RA+RO− T cells.27 An increase of CD95+ T cells has been observed in adulthood,28 aging,29-32 and pathological conditions such as HIV infection33 and systemic lupus erythematosus (SLE).34 Thus, CD95 Ag expression might reflect previous or ongoing in vivo antigen-specific activation, and its role in physiological and pathological conditions has been extensively studied. Surprisingly, very little is known regarding lymphocytes that do not express CD95 and their biological role.
We have hypothesized that the absence of CD95 expression could represent a novel tool able to discriminate naive T cells. This possibility was tested according to the above-mentioned and restrictive criteria to distinguish naive from nonnaive T cells in humans. Because the lack of CD95 Ag resulted as a reliable marker of naive T cells, we have evaluated the changes of naive CD95−T cells during aging. Our study demonstrates a decrease of naive T cells within the CD4 subset and an almost complete loss of naive T lymphocytes within the CD8 T-cell subset in old people, particularly in centenarians. This exhaustion of naive T cells within the CD8 T cells could account for the reduced competence to face new intracellular pathogens which occurs during senescence and may define an “immunological clock” which is possibly correlated to the life span of humans.
Materials and methods
Isolations of peripheral blood mononuclear cells and T lymphocytes
Using a sample population of 120 healthy people ranging in age from 18-105 years, peripheral blood mononuclear cells (PBMCs) were obtained by density gradient centrifugation (Ficoll-Hypaque; Sigma, St. Louis, MO) from freshly drawn venous blood. All subjects were in good clinical condition, and those older than 65 years were selected according to the Senieur protocol.35 After washings with phosphate-buffered saline (PBS), the cells were resuspended in RPMI 1640 medium supplemented with 10% fetal calf serum (FCS), 2 mmol/L L-glutamine, 100 μg/mL streptomycin, and 100 units/mL penicillin (complete medium). For proliferation tests, PBMCs were further fractionated into T and non-T cells by a single-step rosetting method using sheep red blood cells. Enriched T cells were further depleted of adherent cells in plastic petri dishes at 37°C, 6% carbon dioxide (CO2). The purity of T-cell preparation, assessed by cytofluorimetric analysis, was greater than 95%. Further isolation of the CD3+CD95− T-lymphocyte subset was obtained by immunoselection using coated beads (Dynabeads M-450; Dynal, Oslo, Norway) with polyclonal sheep antimouse immunoglobulin G (IgG). T lymphocytes were depleted from CD95+ cells by magnetic beads coated with purified anti-CD95 monoclonal antibody (mAb). Isolated CD3+CD95− cells comprised more than 98% CD3+ cells.
Monoclonal antibodies
Purified monoclonal antibody (mAb) anti-CD3 (clone OKT3) was kindly provided by Dr E. G. Engleman (Stanford University, CA). Fluorescein isothiocyanate-conjugated (FITC-conjugated) and phycoerythrin-conjugated (PE-conjugated) mAbs recognizing CD45RA, CD2, CD11a, CD62L, CD69, CD71, or HLA-DR (human leukocyte antigen-DR) were purchased from Becton Dickinson Immunocytometry Systems (San Jose, CA). Purified anti-CD28 mAb was also obtained from Becton Dickinson. FITC-, PE-, or CyChrome-conjugated mAbs directed against CD3, CD4, CD8, CD95, CD28, CD25, or CD44 were obtained from PharMingen (San Diego, CA). The negative controls, of IgG1 or IgG2a isotype and of irrelevant specificity, were purchased from Becton Dickinson and from PharMingen. They were conjugated with either FITC-, PE-, or CyChrome and were used to set the limits of non-specific immunoglobulin cell-binding by cells stained with mAbs conjugated with the homologous fluorochrome.
Immunofluorescence and multiparameter flow cytometric analysis
PBMCs were resuspended in PBS containing 1% FCS, 1% human serum, 10% mouse serum, and 0.01% sodium azide, then stained for 30 minutes on ice with combinations of saturating amounts of fluorochrome-conjugated mAbs. After staining, cells were washed extensively and analyzed. Flow cytometry was performed using a fluorescence-activated fluorcytometer (FACScan, Becton Dickinson). To obtain the percentages and the absolute numbers of different T-cell subsets, we first determined the total number of lymphocytes per μL of peripheral blood (Coulter Counter, Coulter Electronics, Hialeah, FL). PBMCs were stained with FITC-conjugated anti-CD95, PE-conjugated anti-CD4 or anti-CD8, and CyChrome-conjugated anti-CD3. For each sample, data from 104 viable cells were collected and analyzed by flow cytometry, and lymphocytes were identified by characteristic forward angle and side scatter profiles. The percentage of CD3+, CD3+CD4+, and CD3+CD8+ cells among lymphocytes allowed us to obtain the absolute number of total T lymphocytes, CD4 T cells, and CD8 T cells, respectively. Thereafter during analysis, an electronic gate placed on CD3+ cells and the correlated expression of CD4 or CD8 cells versus CD95 cells allowed us to obtain the percentages and calculate the absolute numbers of CD95+ and CD95− cells within CD3+, CD3+CD4+, or CD3+CD8+.
For other subset frequencies, PBMCs were stained with CyChrome-conjugated anti-CD3, anti-CD4, or anti-CD8 mAbs and different combinations of FITC- and PE-conjugated mAbs. To define single subsets we used an acquisition gate of 104 viable cells, uniquely identifying CD3+, CD4+, or (to exclude CD3−CD8+ cells) CD8hiT cells. Quadrants and gates were set based on isotype control mAbs (not shown in the figures). Samples were acquired and analyzed at different times for different donors; thus, given the variation of background intensity, quadrant and gate positions vary among donors. The absolute number of individual CD3, CD4, or CD8 T-cell subpopulations expressing a particular phenotype were calculated by multiplying their percentages derived from FACS gating by the absolute count per μL of each population.
Proliferation assay
For proliferation assays, purified total T cells and isolated CD95− T cells were stimulated with immobilized mAbs as follows. In 96-well round-bottom microtiter plates, either 12.5, 25, or 50 ng/mL anti-CD3 alone or 1 ng/mL anti-CD3 plus 200 ng/mL anti-CD28 were added to PBS. After incubation at room temperature for 90 minutes, the wells were washed with PBS, and 1 × 105 cells were added to 0.2 mL complete medium. Triplicate well cultures were incubated for 3 days, and 0.0185 MBq of3H-thymidine (3H-TdR) was added to each well 18 hours before cell harvesting on glass fiber filter paper. Uptake of3H-TdR was measured in a liquid scintillation counter, and the results were expressed as the mean counts per minute plus or minus standard error of the mean (cpm ± SEM).
Statistical analysis
Comparisons between groups of different ages were done by ANOVA. Changes of percentages and absolute numbers of cells with age were tested by simple regression analysis, and relationships between variables were tested by multiple regression analysis. Statistical analysis was conducted using Statistical Package for Social Sciences for Windows (SPSS, Chicago, IL), and P < .05 was considered significant.
Results
Absence of the CD95 Ag as a marker for the phenotypic identification of CD45RA+CD62L+ naive T cells
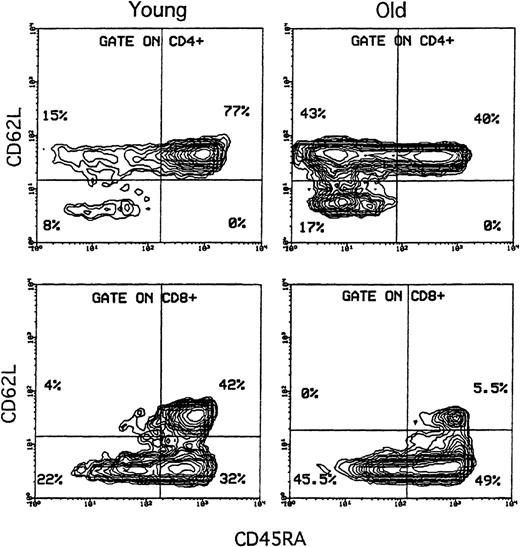
Using flow cytometry, we analyzed freshly isolated PBMCs in 3-color fluorescence with CD45RA and CD62L coexpression (or CD11a, not shown) either with CD4 or CD8 T cells. Evaluation of CD45RA and CD62L coexpression, which may be considered the standard phenotype to define naive T cells, was tested for the first time in donors of different ages. The results in Figure 1, from stainings of a representative 18-year-old and an 80-year-old subject, indicate that double-positive naive T cells were reduced in old subjects (40% versus 77% among CD4+ T cells, and 5.5% versus 42% among CD8+ T cells). Moreover, the percentage of these cells was higher within the CD4 subset than within the CD8 subset in both age groups. Enumeration of circulating naive T cells by this method indicated that old people maintain less naive T cells than was previously reported following staining with the classical marker CD45RA. In fact in both subjects, considering CD45RA+within CD8+ cells, a large subset of CD45RA+ T cells not stained by CD62L was evident (Figure 1).
Evaluation of CD45RA+CD62L+naive T cells in donors of different ages.
Freshly isolated PBMCs were stained with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD45RA, CD62L, and CD4 or CD8. A representative comparison of 5% probability contour plots from a young (18-year-old) and an old (80-year-old) subject is shown. An electronic gate was set on CD4+ or CD8+ T lymphocytes as indicated, and expression of CD45RA (X axis) was correlated to CD62L (Y axis). In both the CD4 and CD8 subsets, CD45RA+CD62L+ (double-positive) naive T cells (upper-right box) were profoundly reduced in the old subject compared with the young subject; within each of these subjects, the percentage of double-positive cells was higher in the CD4 subset than in the CD8 subset. Moreover, within the CD8 T cells, the proportion of CD45RA+CD62L− cells (lower-right box) showed an important age-dependent increase.
Evaluation of CD45RA+CD62L+naive T cells in donors of different ages.
Freshly isolated PBMCs were stained with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD45RA, CD62L, and CD4 or CD8. A representative comparison of 5% probability contour plots from a young (18-year-old) and an old (80-year-old) subject is shown. An electronic gate was set on CD4+ or CD8+ T lymphocytes as indicated, and expression of CD45RA (X axis) was correlated to CD62L (Y axis). In both the CD4 and CD8 subsets, CD45RA+CD62L+ (double-positive) naive T cells (upper-right box) were profoundly reduced in the old subject compared with the young subject; within each of these subjects, the percentage of double-positive cells was higher in the CD4 subset than in the CD8 subset. Moreover, within the CD8 T cells, the proportion of CD45RA+CD62L− cells (lower-right box) showed an important age-dependent increase.
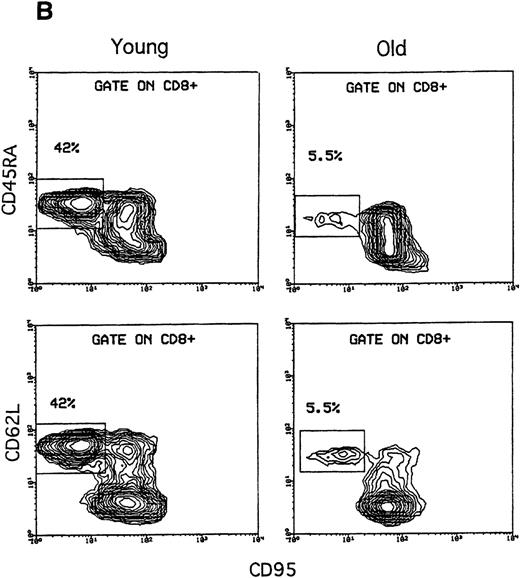
Looking for an alternative single naive T-cell marker, we tested whether, in addition to the lineage markers, staining with CD95 alone could be used instead of CD45RA/CD62L double staining. To this end, using the same subjects, we tested CD95 coexpression with CD45RA and CD62L in CD4 or CD8 subsets (Figure2A and 2B). The results indicated that all CD95− T cells express both CD45RA and CD62L (and low levels of CD11a, not shown). These findings were unequivocal for any donor tested and were detectable both in CD4 and CD8 T-cell subsets (Figure 2A and 2B). Furthermore, because PBMC stainings shown (Figures1, 2, and 3) were obtained from the same representative donors, it must be noted that the percentages of CD95− T cells were substantially coincident with those of the double-positive CD45RA+CD62L+ T cells. These same staining patterns were verified in 10 donors ranging from 18-100 years of age (Table 1). Globally, these results indicate that the absence of CD95 Ag can define putative naive T cells currently identified by double staining with CD45RA and CD62L.
Analysis of CD45RA and CD62L expression versus CD95 expression in both CD4 and CD8 subsets.
Freshly isolated PBMCs were stained with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD95, CD45RA or CD62L, and CD4 or CD8. Analysis of CD45RA and CD62L expressions (Y axis) versus the CD95 expression (X axis) was carried out using lymphocytes from the same donors of Figure 1. (A) Within CD4 T cells, all CD95− cells (square box) were CD45RA+ and CD62L+ in both young and old donors. (B) Similarly, all CD8+CD95− cells (square boxes) were CD45RA+ and CD62L+. It is important to note that in both CD4 and CD8 cells, the percentages of CD95− T cells were substantially identical to those of the double-positive CD45RA+CD62L+ T cells shown in Figure 1.
Analysis of CD45RA and CD62L expression versus CD95 expression in both CD4 and CD8 subsets.
Freshly isolated PBMCs were stained with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD95, CD45RA or CD62L, and CD4 or CD8. Analysis of CD45RA and CD62L expressions (Y axis) versus the CD95 expression (X axis) was carried out using lymphocytes from the same donors of Figure 1. (A) Within CD4 T cells, all CD95− cells (square box) were CD45RA+ and CD62L+ in both young and old donors. (B) Similarly, all CD8+CD95− cells (square boxes) were CD45RA+ and CD62L+. It is important to note that in both CD4 and CD8 cells, the percentages of CD95− T cells were substantially identical to those of the double-positive CD45RA+CD62L+ T cells shown in Figure 1.
Comparison of CD28 expression versus CD95 or CD45RA expression in both CD4 and CD8 T cells.
Freshly isolated PBMCs were stained with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD95 or CD45RA, CD28, and CD4 or CD8. (A) In both the young and old subjects, 5% probability contour plots of CD28 expression (Y axis) versus CD95 expression (X axis) showed that both CD4 and CD8 T cells were made of 3 different subsets: CD95−CD28+ (upper-left boxes), CD95+CD28+ (ungated), and CD95+CD28− (lower boxes). In all stainings, CD28− T cells expressed CD95 at lower intensity than the CD28+CD95+ counterparts. (B) Analysis of CD28 expression (Y axis) versus CD45RA expression (X axis). In both the young and old donors, not all CD45RA+ T cells expressed CD28. Within the CD4+ T cells, all CD45RA+ were CD28+ (upper-right box), whereas in the CD8+ T cells, CD45RA+ T cells comprised both CD28+ (upper-right box) and CD28− T cells (lower-right box). Note that the data were obtained using lymphocytes from the same donors as in Figure 1 and 2.
Comparison of CD28 expression versus CD95 or CD45RA expression in both CD4 and CD8 T cells.
Freshly isolated PBMCs were stained with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD95 or CD45RA, CD28, and CD4 or CD8. (A) In both the young and old subjects, 5% probability contour plots of CD28 expression (Y axis) versus CD95 expression (X axis) showed that both CD4 and CD8 T cells were made of 3 different subsets: CD95−CD28+ (upper-left boxes), CD95+CD28+ (ungated), and CD95+CD28− (lower boxes). In all stainings, CD28− T cells expressed CD95 at lower intensity than the CD28+CD95+ counterparts. (B) Analysis of CD28 expression (Y axis) versus CD45RA expression (X axis). In both the young and old donors, not all CD45RA+ T cells expressed CD28. Within the CD4+ T cells, all CD45RA+ were CD28+ (upper-right box), whereas in the CD8+ T cells, CD45RA+ T cells comprised both CD28+ (upper-right box) and CD28− T cells (lower-right box). Note that the data were obtained using lymphocytes from the same donors as in Figure 1 and 2.
Percentages of CD45RA+CD62L+T cells versus CD95− T cells in donors of different ages
| Donors . | Age . | CD4+ Cells, % . | CD8+ Cells, % . | ||
|---|---|---|---|---|---|
| CD45RA+CD62L+ . | CD95− . | CD45RA+CD62L+ . | CD95− . | ||
| RC | 18 | 77 | 77 | 42 | 42 |
| CA | 20 | 51.3 | 52 | 30 | 30 |
| SS | 21 | 60 | 60 | 41.8 | 41 |
| MA | 59 | 52.7 | 53.2 | 45 | 45.5 |
| MG | 59 | 55.7 | 55 | 35.9 | 34 |
| DSM | 60 | 49.1 | 50.5 | 25.3 | 25 |
| FM | 72 | 63 | 63 | 6.9 | 7 |
| AG | 80 | 40 | 40 | 5.5 | 5.5 |
| DMC | 99 | 21 | 20 | 3 | 3 |
| MC | 100 | 39.1 | 38 | 8 | 7 |
| Donors . | Age . | CD4+ Cells, % . | CD8+ Cells, % . | ||
|---|---|---|---|---|---|
| CD45RA+CD62L+ . | CD95− . | CD45RA+CD62L+ . | CD95− . | ||
| RC | 18 | 77 | 77 | 42 | 42 |
| CA | 20 | 51.3 | 52 | 30 | 30 |
| SS | 21 | 60 | 60 | 41.8 | 41 |
| MA | 59 | 52.7 | 53.2 | 45 | 45.5 |
| MG | 59 | 55.7 | 55 | 35.9 | 34 |
| DSM | 60 | 49.1 | 50.5 | 25.3 | 25 |
| FM | 72 | 63 | 63 | 6.9 | 7 |
| AG | 80 | 40 | 40 | 5.5 | 5.5 |
| DMC | 99 | 21 | 20 | 3 | 3 |
| MC | 100 | 39.1 | 38 | 8 | 7 |
The percentages of CD95− T cells were obtained by staining PBMCs with the following combinations of FITC-, PE-, and CyChrome-conjugated mAbs: CD95, CD4 or CD8, and CD3. The percentages of CD45RA+CD62L+ T cells were obtained by staining PBMCs with CD45RA, CD62L and CD4, or CD8 mAbs. Data from 10 donors, 18-100 years of age, are shown.
To further test if CD95− T cells consist of putative naive T cells, we investigated the phenotype of this T-cell subset by using 3-color flow cytometry analysis. The absence of CD95 activation Ag was specific for resting T cells because early-, intermediate-, and late-activation antigens, such as CD69, CD25, CD71, HLA-DR, and CD45RO, when expressed, were consistently confined among CD95+ T cells (data not shown). Furthermore, adhesion molecules, such as CD2, CD11a, and CD44, were constantly and homogeneously at lower intensity on CD95− T cells than on CD95+ T cells (data not shown).
For clonal expansion, naive T cells need both TCR engagement and costimulatory signals mainly provided by the CD28 Ag on their membrane. Thus, it is expected that naive T cells are CD28+. Indeed, we found that all CD95− T cells bear CD28 Ag, whereas CD95+ T cells comprise both CD28+ and CD28− T cells, and CD28− T cells express CD95 at lower intensity than the CD28+ counterpart (Figure 3A). On the other hand, we found that not all CD45RA+ T cells expressed the CD28 Ag. Indeed, separate analysis of CD4 and CD8 subsets showed that CD45RA+ T cells comprised both CD28− and CD28+ T cells (Figure 3B) within the CD8 subset, whereas in the CD4 subset, all CD45RA+ were CD28+.
In both young and old subjects, the imbalance between the CD4 and CD8 subsets regarding the number of CD45RA+ cells exceeding the CD95− naive cell was due to a subset of the CD8+CD45RA+ T cells not stained by CD28. The proportion of this still uncharacterized T-cell subset, which bears a CD45RA isoform but is no longer defined as naive T cells, augmented heavily among aged people. These results, obtained from the same representative young and old donors, indicated that the imbalance between CD4 and CD8 subsets, as well as an overestimate of naive T cells within the CD8 subset, was due to a subset of CD45RA+(CD62L−) CD28− T cells.
Activation requirement of CD95− T cells is typical of naive T cells
Naive T cells, but not memory or effector T cells, require costimulation to activate and proliferate optimally. We tested the responsiveness of CD95− T cells to stimulation either through the CD3/TCR complex alone or together with a costimulation. To this end we tested the proliferative response of CD95− T cells to increasing doses of anti-CD3 mAb alone or to a combination of submitogenic doses of anti-CD3 plus a costimulation provided by anti-CD28 mAb (Figure4). Unseparated T cells responded to anti-CD3 mAb in a dose-dependent manner, indicating that T cells contain both naive and memory cells. By contrast, CD95− T cells did not proliferate to increasing doses of plastic-bound anti-CD3 mAb without costimulation, and they showed an optimal response only when costimulation was provided. This finding indicates that CD95− T cells are indeed resting cells and supports the hypothesis that they may be unprimed T cells.
Activation requirement of CD95− T cells.
Data are from a representative experiment of 3 similar experiments. T cells showed dose-dependent proliferative responses to immobilized anti-CD3 mAb. On the contrary, purified CD95− T cells did not respond to increasing doses of anti-CD3 mAb alone and showed an optimal proliferation only when costimulated by immobilized anti-CD28 (1 mg/mL) and anti-CD3 mAb.
Activation requirement of CD95− T cells.
Data are from a representative experiment of 3 similar experiments. T cells showed dose-dependent proliferative responses to immobilized anti-CD3 mAb. On the contrary, purified CD95− T cells did not respond to increasing doses of anti-CD3 mAb alone and showed an optimal proliferation only when costimulated by immobilized anti-CD28 (1 mg/mL) and anti-CD3 mAb.
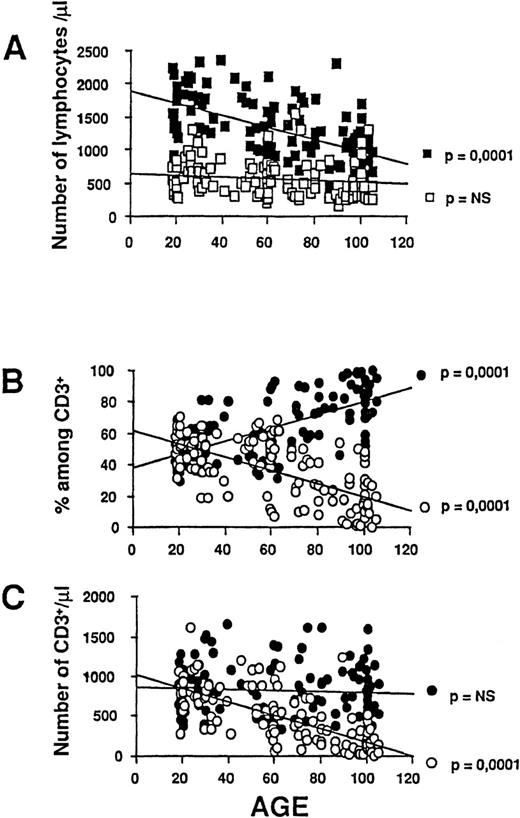
CD95− naive T cells decrease with age
Based on findings that CD95− T cells consist of naive T cells and that there are less CD95− T cells among old donors than young donors, we further investigated their absolute number from young adulthood to the extreme limit of human life. To this end, we analyzed peripheral blood T cells from 120 healthy donors ranging in age from 18-105 years for expression of the CD95 Ag. Confirming previous reports, we found that absolute numbers of total circulating lymphocytes (data not shown), as well as percentages and absolute numbers of CD3+ T lymphocytes, decreased significantly (R = .58, P = .0001) and progressively with age (Figure 5A), whereas non-T lymphocytes remained unchanged (R = .13, P = not significant). Once we plotted CD95− and CD95+ T-cell subsets in the different donor ages, we found a progressive decrease of CD95− T cells, both in percentage (R = .64, P = .0001) and absolute number (R = .72, P = .0001) (Figure 5B and 5C). This age-related reduction was particularly evident in the oldest donors, in whom circulating naive T cells almost disappeared. By contrast, CD95+ T cells symmetrically increased in percentage with age (R = .64, P = .0001) (Figure 5B), but their absolute counts, given the reduction of total lymphocyte absolute number, did not change significantly (R = .065,P = .48) (Figure 5C). Therefore, these changes imply that the most impressive age-related modification within circulating CD3+ T cells consists of a sharp loss of CD95− naive T cells. The trend and the magnitude of the CD95− T-cell decrease are apparently superimposable to that of total T cells, suggesting that the age-related T lymphopenia may largely depend on the marked decrease of this subset.
Effect of age on absolute numbers of T and non-T lymphocytes.
Data from 120 healthy donors, 18-105 years of age, were plotted as individual data points. R and P values were calculated by linear regression analysis. (A) Absolute numbers of T lymphocytes (defined as CD3+, ▪) declined progressively with age, whereas non-T lymphocytes (defined as CD3−, □) remained unchanged. (B, C) The percentages and absolute numbers of circulating CD95− (○) and CD95+ (•) cells among CD3+ T cells were calculated as described in “Materials and methods.” The percentages and absolute numbers of circulating CD95− cells progressively decreased with age, whereas CD95+ cells increased only in percentages but did not significantly change in absolute numbers until the last decades of life.
Effect of age on absolute numbers of T and non-T lymphocytes.
Data from 120 healthy donors, 18-105 years of age, were plotted as individual data points. R and P values were calculated by linear regression analysis. (A) Absolute numbers of T lymphocytes (defined as CD3+, ▪) declined progressively with age, whereas non-T lymphocytes (defined as CD3−, □) remained unchanged. (B, C) The percentages and absolute numbers of circulating CD95− (○) and CD95+ (•) cells among CD3+ T cells were calculated as described in “Materials and methods.” The percentages and absolute numbers of circulating CD95− cells progressively decreased with age, whereas CD95+ cells increased only in percentages but did not significantly change in absolute numbers until the last decades of life.
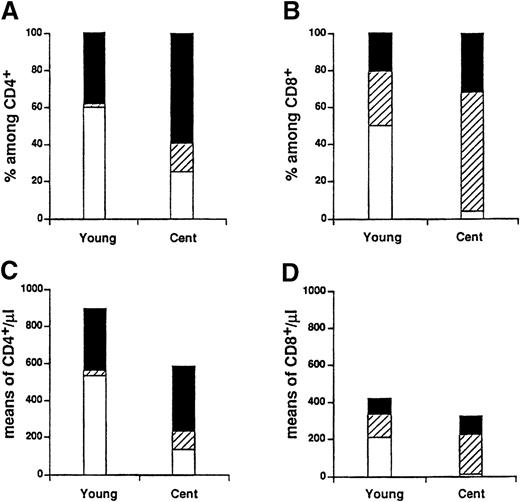
The age-related loss of CD95− T cells was further investigated within CD4 and CD8 T-cell subsets by analyzing a cohort of 71 subjects. The results showed that both percentages (Figure6A and 6B) and absolute numbers (Figure 5C and 5D) of CD95− T cells declined significantly (P = .0001) with age within both CD4 and CD8 T-cell subsets. We also observed that in very old people, CD95− T cells almost disappeared within the CD8 T-cell subset but not within the CD4 T-cell subset. This finding might represent an amplification of an imbalance already present in young adulthood. Indeed the ratio between the number of circulating CD4+CD95− and CD8+CD95− cells was about 2 in young people; the mean plus or minus the standard error of the mean of CD6+CD95− cells was 533 ± 33, whereas CD8+CD95− cells were 213 ± 23 in the older donors. This difference became more evident with age, reaching its peak in centenarians, with a ratio of about 11 (137 ± 24 CD4+CD95− cells versus 13 ± 4 CD8+CD95− cells). Therefore, these data indicate that far advanced age is characterized by a profound reduction of CD4+ circulating naive T cells (Figure 6C) and by an almost complete loss of circulating naive cells within class I–restricted CD8+ T cells (Figure 6D).
Effect of age on CD95 expression on T-cell subsets.
The percentages and absolute numbers of CD95− (○) and CD95+ (•) cells within both CD4 and CD8 T cells were plotted as individual data points from 71 subjects. R andP values were calculated by linear regression analysis. The percentage of CD95− cells decreased with age, and symmetrically the percentages of CD95+ T cells increased with age in both the (A) CD4 subset and the (B) CD8 subset. (C, D) Considering absolute numbers, only CD95−CD4+ and CD95−CD8+ cells significantly declined. In contrast, the CD95+CD4+ and CD95+CD8+ cells did not change.
Effect of age on CD95 expression on T-cell subsets.
The percentages and absolute numbers of CD95− (○) and CD95+ (•) cells within both CD4 and CD8 T cells were plotted as individual data points from 71 subjects. R andP values were calculated by linear regression analysis. The percentage of CD95− cells decreased with age, and symmetrically the percentages of CD95+ T cells increased with age in both the (A) CD4 subset and the (B) CD8 subset. (C, D) Considering absolute numbers, only CD95−CD4+ and CD95−CD8+ cells significantly declined. In contrast, the CD95+CD4+ and CD95+CD8+ cells did not change.
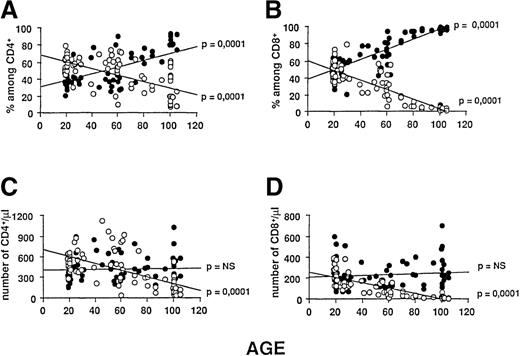
T-cell dynamics in aging: relationship between loss of CD95− and increase of CD28− T cells
The functional and clinical implications of distinct changes in the T-cell compartments suggested that we verify whether the progressive loss of naive T cells, here described, might be related to another profound modification that we recently reported: the expansion of CD28− T cells during aging.36 As previously shown (Figure 3), the reduction of CD95− T cells was associated with an increase of CD28− T cells in the older subjects, and this phenomenon was particularly evident within CD8+ T cells. However, CD95 and CD28 are not mutually exclusive markers, as indicated by the presence of a CD95+CD28+ subset. Thus, we separately analyzed and compared CD4 and CD8 subsets for the expression of the CD95 and CD28 markers among 2 extreme age groups of our study: young subjects (n = 15; 20 ± 0.5 years) and centenarians (n = 15; 100.5 ± 0.3 years). Results showed the relative contribution of CD95+CD28+, CD95+CD28−, and CD95−CD28+ subsets to the composition of total circulating CD4+ and CD8+ T cells (Figure7). When considering only percentages (Figure 7A and 7B) the age-related decrease of CD95−CD28+(P = .0001) was associated with a significant increase (P < .05) with age of both CD95+CD28+ and CD95+CD28− subsets, either within CD4 or CD8 T cells. By contrast, when considering absolute counts (Figure7C and 7D), we found no significant differences in the CD95+CD28+ subsets between young and old subjects, either within CD4 or CD8 T cells (P = .78 andP = .52, respectively), whereas CD95+CD28− T cells increased significantly in both subsets (P = .05 among CD4+T cells, and P = .02 among CD8+ T cells).
Contribution of CD95+CD28+, CD95+CD28−, and CD95−CD28+ to CD4+ or CD8+ T-cell subsets in young subjects compared with centenarians.
Data from 15 young subjects and 15 centenarians represent the means of different cell subpopulations in the 2 groups and were tested by analysis of variance (ANOVA). (A) In both CD4+and CD8+ subsets of centenarians, the percentage reduction of CD95−CD28+ (□) (P = .0001) was mirrored by an increase of CD95+CD28+ (▪) and CD95+CD28− (▨) cells (P < .05 for both). (B) Considering absolute numbers among either CD4 or CD8 T cells, the counts of CD95+CD28+ did not change significantly. Thus, the loss of CD95−CD28+ cells was only associated with an increase of CD95+CD28−cells (P = .05 among CD4+ T cells, andP = .02 among CD8+ T cells).
Contribution of CD95+CD28+, CD95+CD28−, and CD95−CD28+ to CD4+ or CD8+ T-cell subsets in young subjects compared with centenarians.
Data from 15 young subjects and 15 centenarians represent the means of different cell subpopulations in the 2 groups and were tested by analysis of variance (ANOVA). (A) In both CD4+and CD8+ subsets of centenarians, the percentage reduction of CD95−CD28+ (□) (P = .0001) was mirrored by an increase of CD95+CD28+ (▪) and CD95+CD28− (▨) cells (P < .05 for both). (B) Considering absolute numbers among either CD4 or CD8 T cells, the counts of CD95+CD28+ did not change significantly. Thus, the loss of CD95−CD28+ cells was only associated with an increase of CD95+CD28−cells (P = .05 among CD4+ T cells, andP = .02 among CD8+ T cells).
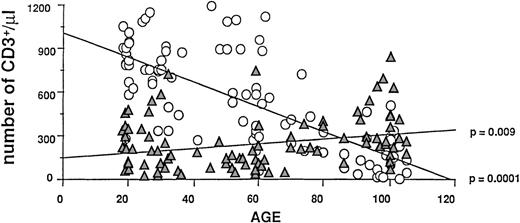
An overall picture of this phenomenon in total CD3+circulating lymphocytes from 96 subjects of different ages is reported in Figure 8. We again found that both subsets statistically changed with age (R = .75 andP = .0001 for CD95−CD28+, andR = .26 and P = .009 for CD95+CD28−), however the magnitude of the CD95−CD28+ T-cell loss was more prominent than the expansion of CD95+CD28−, as shown by the slopes of the 2 regression lines (−8.4 ± 0.7 cells per year for CD95−CD28+ T cells and 1.6 ± 0.6 cells per year for CD95+CD28− T cells). To assess the relationship between CD95−CD28+ and CD95+CD28− T cells and age, we used multiple linear regression analysis. Using CD95−CD28+ as the dependent variable and age and CD95+CD28− as the predictors, we found that the absolute number of CD95−CD28+ was related to both variables (R2 = .58 for the model, P = .0001 for age, and P = .02 for CD95+CD28−T cells). These 2 factors together explained 58% of the variability of CD95−CD28+, but the effect of age was more pronounced than the effect of CD95+CD28− T cells (standardized coefficients: −0.71 versus −0.16). By contrast, we found that the absolute number of CD95+CD28− T cells was weakly related only to CD95−CD28+ (P = .02) and not to age (P = .9). In such a wide age range, more complex relationships may exist between these variables. However, by limiting the multiple linear regression analysis only to people over 55 years of age (n = 52), the statistical findings were virtually identical to those reported above. In conclusion, the T-cell dynamic emerging from these results is that first, aging mainly induces a decrease in the number of CD95−CD28+ T cells, and this in turn is associated with an increase of CD95+CD28− T cells.
Age-related changes of absolute numbers of naive CD95−CD28+ (○) and CD95+CD28− (▴) T cells.
Absolute numbers of CD95− and CD28−T cells among CD3+ cells from 96 donors were plotted as individual data points. R and P values were calculated by linear regression analysis. While CD95− T cells significantly decreased with age, CD28− T cells simultaneously increased.
Age-related changes of absolute numbers of naive CD95−CD28+ (○) and CD95+CD28− (▴) T cells.
Absolute numbers of CD95− and CD28−T cells among CD3+ cells from 96 donors were plotted as individual data points. R and P values were calculated by linear regression analysis. While CD95− T cells significantly decreased with age, CD28− T cells simultaneously increased.
Discussion
In this study we demonstrate that far advanced age is characterized by a profound reduction of circulating naive T cells. These results were obtained by labeling naive T cells with either the CD45RA/CD62L double-staining standard method or the CD95 single-staining method. Both approaches allowed us to recognize an age-dependent naive T-cell depletion that was much more significant than previously estimated by the CD45RA isoform staining method.37 This sharp age-related loss of naive CD95−CD3+ cells paralleled the rate of total T-cell loss (Figure 5), suggesting that the well-known age-related T lymphopenia may largely depend on the marked loss of CD95− naive T cells. A detailed analysis of age-related changes within the CD4 and CD8 subsets showed that naive T-cell reduction was profound in both T-cell subsets, but the reduction was deeper within the CD8+ T cells, where an almost complete loss in the oldest donors was observed. From the data here reported, it appears that the most profound age-related change in the T-cell compartment is the loss of circulating naive CD8+ T cells. The use of markers thus far available has largely underestimated this phenomenon.
Class I–restricted CD8+ T cells play a major role in infectious diseases caused by pathogens living inside cells, and they constitute an important effector arm for immune surveillance against tumors.38 While few studies have found a shortage of naive CD8+ T cells in HIV-infected adults,20-22 most studies on human senescence have neglected the naive CD8 T-cell count as an indicator for evaluating the risk of immune system failure. Infectious diseases, such as influenza and pneumonia, and cancer are major health problems in older people and represent leading causes of death in this population.39 Therefore, naive CD8 T cells constitute an important reservoir, and their shortage could predict lack of protection against novel class I–restricted antigens. Based on our results of the loss of naive T cells within the CD8+compartment, it can be predicted that very old subjects have low protection against infectious diseases, especially viruses, and malignant cells. Moreover, given the direct correlation between the decrease of CD95− T cells and the increase of age, with an almost complete exhaustion in very old subjects such as centenarians, it can also be predicted that a very low number of CD95− T cells correlates with a shorter life expectancy. Although these 2 predictions need to be verified in a perspective study, it must be noted that a high susceptibility to viral infections and a current short life expectancy both characterize far advanced aged people.
A theory on the aging process by F.M. Burnet40 proposed, among other points, that most organs or physiological systems undergo weakening and reduce their physiological reservoirs with aging. However, they “…differ widely in the time needed to use up their quota of cells. Many systems may never approach the limit, but that system, vital to life, which first uses up its quota, will be the chief secondary mediator of aging.”40 Our current results, showing the progressive decline of CD8 naive T cells until exhaustion in centenarians, may fit with this interpretation, and accordingly, we propose that the shortage of CD8 naive T cells may represent a secondary biological clock related to the human life span.
Our results are consistent with most previously published data on the expression of CD95/Fas/Apo-1 by T lymphocytes. Initially, Miyawaki et al28 demonstrated that T lymphocytes from newborns do not bear CD95, whereas percentages of CD95+ T cells increase gradually until 50 years of age. More recently, other studies have confirmed significant increases of CD95 expression with age, either as percentages of T cells29,30 or as intensity of mean fluorescence,31 by comparing a group of aged people versus young controls. Moreover, Aggarwal and Gupta32 found up-regulation of the CD95-CD95L system along with reduced expression of Bcl-2 and increased susceptibility to apoptosis both in CD4 and CD8 T cells from aged donors. Our current study, although focused on the characterization of CD95− T cells, extends those previous results regarding percentages of T cells expressing CD95 well beyond middle age and reports a gradual increase by each decade, until over 100 years of age. On the other hand, the integrate analysis, including for the first time absolute counts, evidenced not simply the well-known increase of CD95+ T-cell percentages, but rather a sharp age-related loss of CD95− T cells paralleling the rate of total T-cell loss.
Somewhat surprisingly, 2 papers41,42 have reported opposing results regarding T-cell expression of CD95. Lechner et al41 found negligible expression of CD95 on freshly isolated T cells at any age, whereas Aspinall et al42described a decrease of percentages and absolute counts of CD95+ T cells both in CD4 and CD8 T cells in a group of 12 older females compared with young controls. The possible explanations for these outlying results are not fully understandable, but in our opinion the divergent classification of CD95+dimT cells, which we characterized as CD28− T cells and which increase with age, may justify at least some of these discrepancies.
Our results indicate that the absence of the CD95 Ag by itself can define putative naive T cells currently identified by a standard double-staining method with CD45RA and CD62L. Therefore, we propose to identify naive T cells phenotypically as CD95− cells. This approach is further supported by the demonstration that CD95− T cells do not express activation antigens, but they express adhesion antigens at low intensity, express CD28 Ag, and have a costimulatory requirement for activation.
The present finding reinforces the notion that naive T-cell frequency cannot be evaluated on the basis of CD45RA expression alone. Indeed, we have shown that physiological aging was coupled by an expansion of a subset of CD95+CD45RA+CD28− T cells paradoxically coexpressing putative markers of virgin and activated cells. The coexpression of CD95 activation Ag in CD45RA+ T cells extends previous findings showing that (1) the CD8+CD45RA+ T-cell subpopulation contains cells with the phenotype of activated T cells expressing high levels of CD11a and CD29 Ags43 and (2) these cells are significantly increasing with age.44 Similarly, it has been shown that the CD8+ T-cell subset contains expanded clones which are very frequent in old donors and are present not only in CD45RO+ T cells but also in CD45RA+ T cells.45 Moreover, our results show that this activated CD8+CD45RA+CD95+ T-cell subset consists of CD28− T cells, which have been extensively studied in humans. CD28− T cells have phenotypic and functional features of terminally differentiated armed effector T lymphocytes,36,46,47 have a telomere length suggestive of a long replicate history,47,48 and contain clonal expansions.49 Taken together, these findings support the notion that CD28− T cells cannot be considered as thymus-derived naive T cells. Accordingly, we propose that staining with CD95 or any other equivalent approach, excluding CD28− T cells, is required whenever an expansion of CD28− T cells occurs. Consequently, the interpretation of previous findings about CD45RA stainings in clinical settings, characterized by an expansion of CD28− T cells including viral infection (HIV, cytomegalovirus, Epstein-Barr virus, etc.) and/or chronic inflammatory diseases (rheumatoid arthritis, SLE, etc.), should be reconsidered.
To date, CD28− T cells have been described only in humans, and their origin is still controversial. They may be generated, as such, from extra-thymic lymphopoiesis, or alternatively, they may derive from loss of the CD28 molecule by thymus-derived T cells. As shown here and in a previous report,36 aging is associated with expansion of CD28− effector T cells. By using multiple linear regression fitting, we show that during the aging process, there is a significant correlation between CD28− expansion and CD95−reduction. In particular, the hypothesis emerging from our results is that aging induces, in the first place, a decrease in the number of CD95−CD28+ T cells, and this in turn is associated with an increase of CD95+CD28−T cells, which could represent a compensatory mechanism of the immune system.
Some recent studies on T-cell regeneration in different clinical settings in humans have similarly shown that thymic lymphopoiesis is severely limited in adults, and thymic-independent expansion of a mature T-cell population may represent the primary pathway by which T cells are regenerated.7,11,50,51 Notably, several distinctions have been observed between CD8+ and CD4+ T cells. In patients undergoing intensive chemotherapy, Mackall et al50 described that CD8+ T cells recover more rapidly than CD4+ T cells, but there is a prolonged alteration in the composition of the CD8+ subset, with a predominance of CD8+CD28− cells. Consistently, a longitudinal study demonstrated that in HIV+patients at different stages of the disease, variations of CD8+CD28− T cells inversely correlated with CD4+ and CD8+CD28+ T cells.52 This suggests that in these patients, CD3+ T-cell homeostasis is maintained by the continuous production of CD8+CD28− T cells.52 Moreover, in HIV-infected patients, Gorochov et al53 found no significant enhancement of the CD8+ T-cell Vβ repertoire after highly active antiretroviral therapy. Reminiscent of what is seen after toxic insults from chemotherapy, irradiation, or infections such as HIV, we hypothesize that during aging, when the ability to replenish the naive pool via thymopoiesis is reduced, the immune system tries to compensate for the progressive loss of naive T cells by increasing thymic-independent pathways, such as the peripheral expansion of mature CD28− T cells, especially within the CD8+ subset.
Taken together, these age-dependent changes in the T-cell subpopulations indicate that advanced age, per se, is a condition characterized by lack of adaptive immune response to new intracellular pathogens. These changes also strongly support the notion that aging shares similarities with persistent and chronic stimulatory conditions of the immune system by infectious agents such as HIV. In particular, the progressive loss of naive T cells within the CD8+subset,20-22,54 the expansion of CD8+CD28− T cells,52 as well as the restriction in the CD8+ T-cell repertoire53 55 suggest a typical perturbation of the CD8+ T-cell subset that occurs in both HIV disease and advanced aging. The mechanisms underlying the CD8+ naive T-cell loss in aging, as well as in HIV disease, may be unique or reflect common immunoregulatory processes that HIV could accelerate.
In any event, we are suggesting that the loss of naive T cells, particularly within the CD8+ T-cell compartment, represents a hallmark of immunosenescence as well as some immunodeficiencies and could provide a useful biomarker in both conditions.
Acknowledgment
We thank Lucia Orlando for her excellent technical assistance.
Supported by grant 9806171821-003 from MURST (Ministry for University & Scientific Research, Rome, Italy); grant for the project “Predictive Molecular Markers of Osteoporosis,” Ministry of Health, Rome, Italy; and grant 1998/99 from Foundation of the Cassa di Risparmio, Bank of Parma and Piacenza, Parma, Italy.
F.F.F. and R.V. contributed equally to this work. F.F.F. is currently affiliated with the Division of Medical Oncology, Maugeri Foundation Medical Center,Loc. Cravino, Pavia, Italy.
Submitted August 13, 1999; accepted December 30, 1999.
Reprints:Paolo Sansoni, Department of Internal Medicine and Biomedical Sciences, University of Parma, via Gramsci 14, 43100, Parma, Italy; e-mail: immunopr@ipruniv.cce.unipr.it.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal