Abstract
Thrombocytosis is occasionally seen in patients with carcinomas and has been assumed to be attributable to interleukin-6 or granulocyte-macrophage colony-stimulating factor produced by carcinoma cells. In this study, we clarified whether thrombopoietin (TPO) is involved in carcinoma-associated thrombocytosis. Expression of TPO mRNA was observed in the majority of 27 carcinoma cell lines as determined by reverse transcriptase-polymerase chain reaction (RT-PCR). There were 6 PCR products differing in size; sequence analysis showed the full-length TPO mRNA (TPO-1), 12- and 116-bp deleted variants (TPO-2 and TPO-3, respectively), and 3 novel isoforms (197- and 128-bp deleted forms and a 60-bp insert form of TPO-3; named TPO-4, TPO-5, and TPO-6, respectively). Of 27 lines, 24 expressed TPO-1 mRNA with various other isoforms. Culture supernatants of COS-1 cells transfected with TPO-5 or TPO-6 cDNA did not promote the proliferation of TPO-responsive cells, whereas Western blot analysis on the cell lysates demonstrated TPO-5 but not TPO-6 protein, suggesting poor extracellular secretion (TPO-5) or poor protein synthesis (TPO-6). TPO protein was detected in 10-fold concentrated culture supernatants of cells of these carcinoma lines, with a median concentration of 0.38 fmol/mL as evaluated by enzyme-linked immunosorbent assay. High blood TPO levels were observed with a median value of 3.46 fmol/mL (range, 0.34 to 8.67 fmol/mL) in patients with advanced carcinomas associated with thrombocytosis. These results indicate that thrombocytosis in patients with carcinomas might be caused, at least in part, by TPO produced by carcinoma cells.
THROMBOCYTOSIS IS occasionally seen in patients with carcinomas.1-3 The cause of malignancy-associated thrombocytosis has been assumed to be attributable to interleukin-6 (IL-6),4 which potently promotes megakaryocyte maturation and induces platelet production (megakaryocyte potentiating [Meg-Pot] activity),5,6although the cellular source of IL-6 may be different from patient to patient, being carcinoma cells, bystander cells, or both. In our previous study on 14 patients with tumors producing colony-stimulating factor (CSF), IL-6 produced by tumors was shown to be responsible for the thrombocytosis.7 When the type of CSF produced was granulocyte-macrophage colony-stimulating factor (GM-CSF), thrombocytosis was caused by the megakaryocyte colony-stimulating factor (Meg-CSF) activity of GM-CSF and the Meg-Pot activity of GM-CSF plus IL-6.7 In our additional series of patients with CSF-producing tumors, the semisolid culture of normal bone marrow cells with plasmas from patients with tumors producing granulocyte colony-stimulating factor (G-CSF) occasionally generated small megakaryocytic colonies in addition to granulocytic colonies (unpublished data). This fact suggested the presence of Meg-CSF activity in the plasmas examined, because neither G-CSF nor IL-6 induces megakaryocytic colonies in vitro. Furthermore, Estrov et al8 showed that thrombocytosis in patients with metastatic cancer was not totally attributable to IL-6 or GM-CSF and subsequently suggested the presence of unidentified thrombopoietic activity in plasmas from these patients.
In recent years, thrombopoietin (TPO), the c-mpl ligand, was cloned from several species.9-14 TPO has both Meg-CSF and Meg-Pot activity in vitro.15 It stimulates platelet production in vivo in mice and markedly increases the number of megakaryocytes in the spleen and bone marrow.16 TPO mRNA is expressed primarily in the liver and, to a lesser degree, kidney, smooth muscle, spleen, and bone marrow.9,10,12,17 Regarding malignant tumors, constitutive TPO mRNA expression has been demonstrated in a human hepatoma cell line (HepG2)18 and a number of leukemic cell lines.19 However, there has been no report regarding TPO production by human carcinomas other than HepG2 and HEK20cells. In addition, the relationship between thrombocytosis and TPO production by malignant cells has not been studied, although TPO production by tumor cells was suspected in patients with hepatoblastoma associated with thrombocytosis.21
To date, 3 different forms of human TPO mRNA have been identified from the liver, ie, full-length mRNA and its 2 alternative spliced forms.22 The alternative forms lack 12 and 116 bp in exon 6.22 The 2 isoforms may correspond to murine TPO isoforms, TPO-2 and TPO-3, respectively.23,24 In addition, TPO-4 has been identified in mice24 but not in humans. In this study, we determined the expression of TPO mRNA by human carcinoma cell lines producing or not producing CSF using reverse transcriptase-polymerase chain reaction (RT-PCR). Most of these cell lines expressed TPO-1, TPO-2, and TPO-3 mRNAs, and novel isoforms (TPO-4, TPO-5, and TPO-6) were identified in some lines. Furthermore, we examined the biological activity of TPO-5 and TPO-6 proteins. TPO protein was detected in the culture supernatants of carcinoma cells as evaluated by enzyme-linked immunosorbent assay (ELISA). We also examined the relationship between blood TPO levels and platelet counts in patients with advanced carcinomas.
MATERIALS AND METHODS
Human carcinoma cell lines.
Twenty-seven cell lines from human carcinomas were tested. KHC287 (lung cancer),7,25 Lu-Y1 (lung),7 UT-M1 (uterus),7 HTC/C3 (thyroid),26 ST-Y1 (stomach; unpublished data), and ES-O (esophagus; unpublished data) were established in our institution. CHU-2 (oral cavity),27T24 (urinary bladder),28 Lu65 (lung),29 Lu99 (lung),30 SK-HEP-1 (liver),31 HeLa (uterus), PC-3 (lung),32 A-549 (lung),33 ABC-1 (lung),34 Lc-1sq (lung),35 LK-2 (lung), RERF-LC-MS (lung), RERF-LC-OK (lung), and VMRC-LCD (lung) were provided by the Japanese Cancer Research Resources Bank (Osaka, Japan). HepG2 (liver)36 was obtained from the American Type Culture Collection (Rockville, MD). HLC-1 (lung)37 and HL111783 (lung) were provided by the Riken Cell Bank (Tsukuba, Japan). Sq-19 (lung), 86-2 (lung),38LK-79 (lung), and 11-18 (lung) were provided by the Research Institute for Tuberculosis and Cancer, Tohoku University (Sendai, Japan). All of the lung carcinoma cell lines were established from non–small-cell lung carcinomas. Of the 27 cell lines, KHC287,7Lu-Y1,7 UT-M1,7 HTC/C3,7 ST-Y1, ES-O, CHU-2,39 T24,39 Lu65,25 Lu99, and SK-HEP-1 produce G-CSF or GM-CSF (HTC/C3) and IL-6, being regulated by coproduced IL-1. A-549, RERF-LC-MS, RERF-LC-OK, PC-3, Sq-19, 86-2, 11-18, and HepG2 do not produce IL-1 and produce G-CSF and IL-6 only when they are cultured with exogenous IL-1.40 41
Cell culture and culture supernatant.
All cells were cultured in RPMI 1640 (Nissui, Tokyo, Japan) containing 10% fetal calf serum (GIBCO, Grand Island, NY) at an initial cell density of 2 × 105/mL. After 48 hours, culture supernatants were collected, concentrated 10-fold by ultrafiltration using a PM-10 membrane (Amicon, Tokyo, Japan), and kept frozen (−20°C) until use. In some experiments, recombinant human IL-1α was added at the initiation of culture at a concentration of 4 ng/mL. IL-1α was provided by Dainippon Pharmaceutical Co (Osaka, Japan).
RNA extraction, RT-PCR, and nested-PCR.
After 48 hours of incubation, cells were harvested and total RNA was extracted using TRIzol (GIBCO) by a modification of the acid phenol method. One microgram of total RNA was reverse transcribed by Superscript II (GIBCO) in a reaction volume of 10 μL [50 mmol/L Tris-HCl, 75 mmol/L KCl, 3 mmol/L MgCl2, 10 mmol/L dithiothreitol (DTT), 1.25 mmol/L oligo(dT), 1 mmol/L dNTPs, and 100 U RTase]. Reverse transcription was performed for 10 minutes at 30°C and for 60 minutes at 42°C. PCR and nested-PCR reactions were performed in a reaction volume of 25 μL (1 μL of cDNA pool or PCR products, 10 mmol/L Tris-HCl, 50 mmol/L KCl, 1.5 mmol/L MgCl2, 0.1% TritonX-100, 0.2 mmol/L dNTPs, 0.4 μmol/L sense and antisense primers, and 0.5 U rTaq DNA polymerase [Toyobo, Osaka, Japan]). Primers used for PCR and nested-PCR are shown in Fig 1 and Table 1. First-strand cDNA pool (PCR) or PCR product (nested-PCR) was amplified for 35 cycles using the GeneAmp PCR System 2400 (Perkin Elmer, Norwalk, CT). To determine the existence of an isoform that corresponds to mouse TPO-4, we fractionated the RT-PCR products (primers S3 and A3) at approximately 450 to 500 bp by electrophoresis and then performed the second PCR using a set of S7 and A2 primers. The amplification procedure consisted of denaturation at 94°C for 30 seconds; annealing at 62°C (primers S3 and A3), 65°C (S7 and A2), or 63°C (S2 and A4) for 30 seconds; and extension at 72°C for 30 seconds.
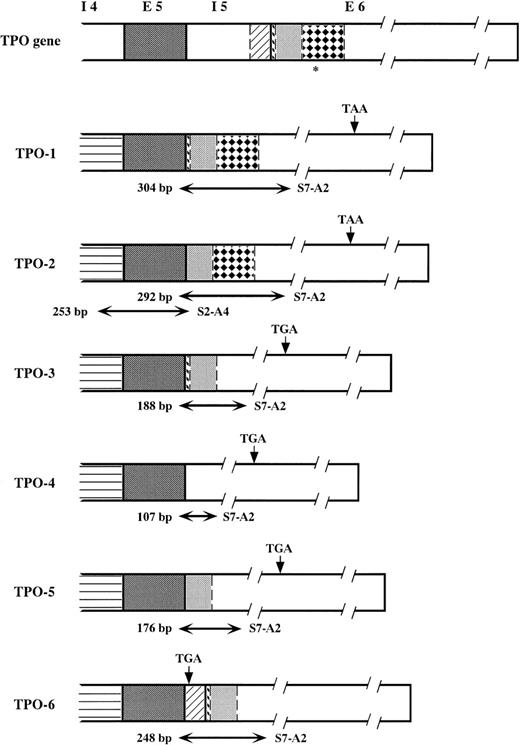
A schematic of the human TPO gene from intron 4 to exon 6 and mRNA isoforms. Corresponding portions exhibit the same patterns. TPO-1, TPO-2, and TPO-3 were reported previously. TPO-4, TPO-5, and TPO-6 are newly identified forms. TPO-3, TPO-4, and TPO-5 possess a stop codon that is different from that of TPO-1 and TPO-2 due to the frameshift. TPO-6 contains another stop codon in the inserted sequence that is part of intron 5, which is not spliced out. *End of the erythropoietin-like domain. Horizontal arrows show the regions amplified by RT-nested PCR. The sizes of the PCR products and the sets of primers used are written beside the arrows.
A schematic of the human TPO gene from intron 4 to exon 6 and mRNA isoforms. Corresponding portions exhibit the same patterns. TPO-1, TPO-2, and TPO-3 were reported previously. TPO-4, TPO-5, and TPO-6 are newly identified forms. TPO-3, TPO-4, and TPO-5 possess a stop codon that is different from that of TPO-1 and TPO-2 due to the frameshift. TPO-6 contains another stop codon in the inserted sequence that is part of intron 5, which is not spliced out. *End of the erythropoietin-like domain. Horizontal arrows show the regions amplified by RT-nested PCR. The sizes of the PCR products and the sets of primers used are written beside the arrows.
PCR Primers and the TPO Isoforms Amplified
| 5′ Primers . | 3′ Primers . | Type of Isoform . | Size of PCR Product (bp) . |
|---|---|---|---|
| S3: 5′-TCCTAACTGCAAGGCTAACG-3′ | A3: 5′-AGGGACCTGGAGGTTTGGTT-3′ | ||
| S7: 5′-TGCAGAGCCTCCTTGGAACC-3′ | A2: 5′-CTGAATCCCTGCTGCCACTT-3′ | TPO-1 | 304 |
| TPO-2 | 292 | ||
| TPO-3 | 188 | ||
| TPO-4 | 107 | ||
| TPO-5 | 176 | ||
| TPO-6 | 223 | ||
| S2: 5′-TTCACCCTTTGCCTACACCT-3′ | A4: 5′-GCTGTGGTCCTGCCCTGGGT-3′ | TPO-2 | 253 |
| 5′ Primers . | 3′ Primers . | Type of Isoform . | Size of PCR Product (bp) . |
|---|---|---|---|
| S3: 5′-TCCTAACTGCAAGGCTAACG-3′ | A3: 5′-AGGGACCTGGAGGTTTGGTT-3′ | ||
| S7: 5′-TGCAGAGCCTCCTTGGAACC-3′ | A2: 5′-CTGAATCCCTGCTGCCACTT-3′ | TPO-1 | 304 |
| TPO-2 | 292 | ||
| TPO-3 | 188 | ||
| TPO-4 | 107 | ||
| TPO-5 | 176 | ||
| TPO-6 | 223 | ||
| S2: 5′-TTCACCCTTTGCCTACACCT-3′ | A4: 5′-GCTGTGGTCCTGCCCTGGGT-3′ | TPO-2 | 253 |
S3 and A3 primers were used for the first PCR of the cDNA pool. Combinations of S7-A2 and S2-A4 primers were used for the second PCR (nested-PCR) of the first PCR products.
Sequencing of PCR products.
Representative PCR products were electrophoresed in a 4% agarose gel and separated to single bands. The isolated bands were sequenced directly or after subcloning into pGEM-T vector (Promega, Madison, WI) by Dye Deoxy terminator cycle sequencing, using a 373A DNA sequencer (Applied Biosystems, Foster City, CA). The results were confirmed by reading both DNA strands.
Construction of expression vectors for TPO-5 and TPO-6.
PCR product of S9 (5′-GGAGCCACGCCAGCCAGACA-3′) and A1 (5′-TCCAACAATCCAGAAGTGGT-3′) using the UT-M1 cDNA as a template were subcloned into pGEM-T plasmid (pGEM-T/TPOS9A1). PCR products of S10 (5′-CCCTGCAGAGCCTCCTTGGA-3′) and A6 (5′-GGGCTTTGGGTTTCAGGAGA-3′) using the same cDNA were electrophoresed, and the band corresponding to the 3′ half of the coding region of TPO-5 was purified. pGEM-T/TPOS9A1 was digested withPst I and HincII and then ligated with the purified S10/A6 product digested with Pst I and Rsa I, resulting in a construction of pGEM-T/TPO-5. pGEM-T/TPO-6 plasmid was constructed with the PCR product of S9 and A10 (5′-CTCAGGCCTCCCTTGTCTGGGTTC-3′) and then subcloned into pGEM-T vector. Sequence analyses were performed to confirm that these plasmids contained the entire coding regions of these TPO isoforms.
Expression of the hexahistidine (His)-tagged TPO-1, TPO-5, and TPO-6.
TPO-1, TPO-5, and TPO-6 cDNAs were regenerated by PCR using the subcloned cDNAs to introduce an EcoRI site at the 5′ end and a His residue and Not I site at the 3′ end. Each PCR product was digested with EcoRI and Not I and subcloned into pEF18S vector derived from pEFneo,42 a mammalian expression vector containing the elongation factor 1 (EF1) promoter and the SV40 polyadenylation signal. The resulting expression vectors (pEF18S-hTPO-1/His, pEF18S-hTPO-5/His, and pEF18S-hTPO-6/His) were transiently transfected into COS-1 cells using the diethyl aminoethyl (DEAE)-Dextran method. After 3 days of culture, the conditioned medium was collected, sterilized by filtration, and subjected to a TPO-dependent cell proliferation assay, as described below. The expression levels of TPO were determined by Western blot analysis. His-tagged TPOs in the culture supernatants and cell lysates of COS-1 cells were first purified and concentrated by a Ni-NTA resin column (QIAGEN Inc, Valentica, CA). The purified materials were immunoprecipitated with the Ni-NTA resin, and the precipitates were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), transferred onto a polyvinilidene difluoride membrane (Millipore, Bedford, MA), and probed with anti-His(C-term) antibody (Invitrogen, Carlsbad, CA). Antibody reactions were detected by an enhanced chemiluminescence (ECL) method according to the manufacturer’s instructions (Amersham, Arlington Heights, IL).
Bioassay of TPO.
The in vitro biological activity of the His-tagged TPO-1, TPO-5, and TPO-6 were determined using FDCP-hMp15 cells,43 which were genetically engineered to express human c-mpl constitutively. The cells were cultured with serially diluted culture supernatants of COS-1 cells that expressed TPO-1, TPO-5, or TPO-6 in 200 μL of Iscove’s modified Dulbecco’s medium (GIBCO) supplemented with 10% fetal calf serum in a 96-well tissue culutre plate (2.5 × 103cells/well) for 3 days at 37°C. Each concentration was tested in duplicate. Cell growth was determined by a colorimetric assay using a tetrazolium salt, WST-1 (Dojindo Laboratories, Kumamoto, Japan).44
ELISA.
TPO concentrations in the culture supernatants of cells from each cell line were measured in triplicate using an ELISA kit devised by Tahara et al45 46 in the Pharmaceutical Research Laboratory, Kirin Brewery Co (Takasaki, Japan). The lower limit of detection for TPO both in the human plasma and the culture supernatant was 0.2 fmol/mL. Stem cell factor (SCF) concentrations in the culture supernatants were measured by use of an ELISA kit (Amersham). The lower limit of detection for SCF was 31.3 pg/mL.
Patients with advanced carcinomas.
Citrated plasmas were obtained with informed consent from patients with advanced carcinomas associated with thrombocytosis more than 500 × 109/L. TPO concentrations in the plasmas were determined with the same ELISA kit. Patients with infection, palpable spleen, or abnormal blood pictures, such as leukoerythroblastosis, giant platelets, or circulating megakaryocytes, were excluded in this study. As a control, TPO concentrations in the plasmas from patients with advanced carcinomas without thrombocytosis (<370 × 109/L) were measured.
Statistical analysis.
The differences in the plasma TPO concentrations were analyzed using the Wilcoxon signed rank test.
RESULTS
Expression of TPO mRNA and sequencing of PCR products.
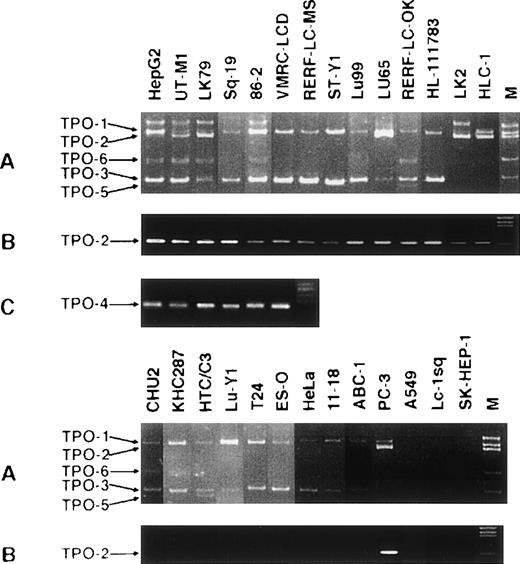
TPO mRNA expression by carcinoma cells was investigated using RT-PCR and nested-PCR. There were 6 bands observed at 304, 292, 188, 176, and 248 bp (Fig 2A) and 1 band at 107 bp (Fig 2C) using a set of S7 and A2 primers. By sequencing each band, the latter 5 were shown to be parts of the full-length TPO (TPO-1) mRNA, ie, 12-bp (position 397 to 408), 116-bp (478 to 593), and 128-bp (397 to 408, 478 to 593) deleted forms in exon 6, a 60-bp insert form between exon 5 and 6 in combination with the 116-bp (478 to 593) deletion in exon 6, and a 197-bp (397 to 593) deleted form in exon 6. The former 2 variant mRNAs correspond to previously reported human and mouse isoforms of TPO (TPO-2 and TPO-3, respectively)22 23and the latter 3 are novel forms (TPO-5, TPO-6, and TPO-4; Fig 1). Because the band representing TPO-2 was weak for many of the cell lines, we constructed another set of primers (S2 and A4) that specifically amplify TPO-2 (Fig 2B). Table2 summarizes the TPO mRNAs expressed by carcinoma cells. Of the 27 cell lines examined, 24 lines expressed TPO-1 mRNA, 15 expressed TPO-2, 23 expressed TPO-3, 6 expressed TPO-4, 7 expressed TPO-5, and 9 expressed TPO-6. Expression of TPO mRNA was not correlated with the production of IL-1, IL-6, G-CSF, or GM-CSF by the carcinoma cells examined. In addition, TPO mRNA expression was not correlated with the origin of the carcinomas or the histological subtype of lung carcinomas.
TPO mRNA isoforms detected by RT-nested PCR. (A and B). Total RNA was reverse-transcribed and the first PCR (primer set S3 and A3) was performed. PCR products were subjected to nested-PCR using a set of S7 and A2 primers for TPO-1, TPO-2, TPO-3, TPO-5, and TPO-6 (A) or a set of S2 and A4 primers for TPO-2 (B). (C) Approximately 450 to 500 bp of the first PCR products was fractionated by electrophoresis, and then the second PCR using a set of S7 and A2 primers for TPO-4 was performed.
TPO mRNA isoforms detected by RT-nested PCR. (A and B). Total RNA was reverse-transcribed and the first PCR (primer set S3 and A3) was performed. PCR products were subjected to nested-PCR using a set of S7 and A2 primers for TPO-1, TPO-2, TPO-3, TPO-5, and TPO-6 (A) or a set of S2 and A4 primers for TPO-2 (B). (C) Approximately 450 to 500 bp of the first PCR products was fractionated by electrophoresis, and then the second PCR using a set of S7 and A2 primers for TPO-4 was performed.
Expression of TPO mRNA Isoforms in Carcinoma Cells
| Cell Line . | Isoforms Detected . |
|---|---|
| HepG2 | 1-6 |
| UT-M1 | 1-6 |
| LK-79 | 1-6 |
| Sq-19 | 1-4 |
| 86-2 | 1-4, 6 |
| VMRC-LCD | 1-4, 6 |
| RERF-LC-MS | 1-3, 6 |
| ST-Y1 | 1-3 |
| Lu99 | 1-3 |
| Lu65 | 1-3 |
| RERF-LC-OK | 1-3, 5, 6 |
| HL111783 | 1-3 |
| LK-2 | 1-3 |
| HLC-1 | 1-3 |
| CHU-2 | 1, 3, 5, 6 |
| KHC287 | 1, 3, 5, 6 |
| HTC/C3 | 1, 3, 5 |
| Lu-Y1 | 1, 3 |
| T24 | 1, 3 |
| ES-O | 1, 3 |
| HeLa | 1, 3 |
| 11-18 | 1, 3 |
| ABC-1 | 1, 3 |
| PC-3 | 1, 2 |
| A-549 | Undetectable |
| Lc-1sq | Undetectable |
| SK-HEP-1 | Undetectable |
| Cell Line . | Isoforms Detected . |
|---|---|
| HepG2 | 1-6 |
| UT-M1 | 1-6 |
| LK-79 | 1-6 |
| Sq-19 | 1-4 |
| 86-2 | 1-4, 6 |
| VMRC-LCD | 1-4, 6 |
| RERF-LC-MS | 1-3, 6 |
| ST-Y1 | 1-3 |
| Lu99 | 1-3 |
| Lu65 | 1-3 |
| RERF-LC-OK | 1-3, 5, 6 |
| HL111783 | 1-3 |
| LK-2 | 1-3 |
| HLC-1 | 1-3 |
| CHU-2 | 1, 3, 5, 6 |
| KHC287 | 1, 3, 5, 6 |
| HTC/C3 | 1, 3, 5 |
| Lu-Y1 | 1, 3 |
| T24 | 1, 3 |
| ES-O | 1, 3 |
| HeLa | 1, 3 |
| 11-18 | 1, 3 |
| ABC-1 | 1, 3 |
| PC-3 | 1, 2 |
| A-549 | Undetectable |
| Lc-1sq | Undetectable |
| SK-HEP-1 | Undetectable |
TPO isoforms detected as shown in Fig 2 are summarized.
Biological activity of TPO-5 and TPO-6 proteins.
As shown in Table 3, culture supernatants of COS-1 cells transfected with TPO-5 or TPO-6 cDNA did not promote the proliferation of TPO-responsive FDCP-hMp15 cells, whereas a culture supernatant of COS-1 cells that expressed TPO-1 stimulated the growth of FDCP-hMp15 cells in a dose-dependent manner.
Biological Activity of Human TPO Isoforms
| TPO Isoforms . | % of Culture Supernants Added . | ||||
|---|---|---|---|---|---|
| 50 . | 10 . | 2 . | 0.40 . | 0.08 . | |
| TPO-1 | 0.953 | 1.155 | 0.871 | 0.489 | 0.260 |
| TPO-5 | 0.243 | 0.292 | 0.248 | 0.250 | 0.248 |
| TPO-6 | 0.232 | 0.258 | 0.252 | 0.250 | 0.254 |
| Medium | 0.236 | ND | ND | ND | ND |
| TPO Isoforms . | % of Culture Supernants Added . | ||||
|---|---|---|---|---|---|
| 50 . | 10 . | 2 . | 0.40 . | 0.08 . | |
| TPO-1 | 0.953 | 1.155 | 0.871 | 0.489 | 0.260 |
| TPO-5 | 0.243 | 0.292 | 0.248 | 0.250 | 0.248 |
| TPO-6 | 0.232 | 0.258 | 0.252 | 0.250 | 0.254 |
| Medium | 0.236 | ND | ND | ND | ND |
Data are shown as the absorbance at 450 nm in a colorimetric assay. Culture supernatants from COS-1 cells that expressed each TPO isoform were added in duplicate to the culture of FDCP-hMp15 cells at varying concentrations and were tested for the ability to stimulate the cell growth as described in Materials and Methods.
Abbreviation: ND, not done.
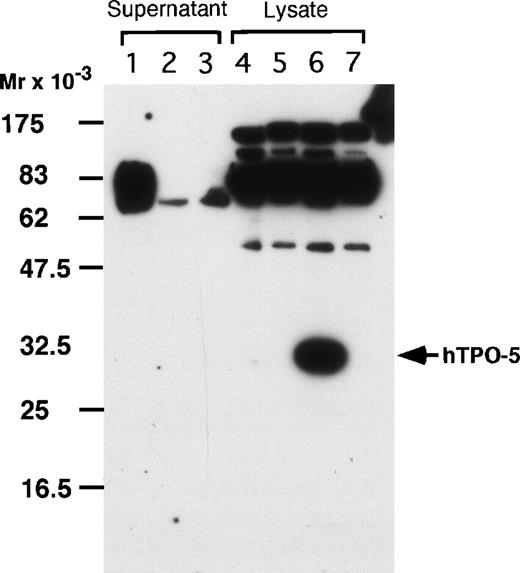
Western blot analysis.
Western blot analysis was performed on immunoprecipitated His-tagged TPOs both in the culture supernatants and cell lysates of COS-1 cells transfected with TPO cDNAs. As shown in Fig 3, only TPO-1 protein was detected in the culture supernatants. On the other hand, in the cell lysates, TPO-5 protein as well as that of TPO-1, but not TPO-6 protein, was demonstrated. Similar results were obtained when anti-TPO polyclonal antibody was used as a probe (data not shown).
His-tagged TPOs in the culture supernatants and cell lysates of COS-1 cells were adsorbed on a Ni-NTA resin column. The eluates were precipitated with the Ni-NTA resin, and the precipitates proteins were separated by SDS-PAGE and probed with anti-His(C-term) antibody. Lanes 1 and 5, TPO-1; lanes 2 and 6, TPO-5; lanes 3 and 7, TPO-6; lane 4, untransfected COS-1 cells. In lane 5, the band corresponding to TPO-1 appears to be masked by nonspecific bands.
His-tagged TPOs in the culture supernatants and cell lysates of COS-1 cells were adsorbed on a Ni-NTA resin column. The eluates were precipitated with the Ni-NTA resin, and the precipitates proteins were separated by SDS-PAGE and probed with anti-His(C-term) antibody. Lanes 1 and 5, TPO-1; lanes 2 and 6, TPO-5; lanes 3 and 7, TPO-6; lane 4, untransfected COS-1 cells. In lane 5, the band corresponding to TPO-1 appears to be masked by nonspecific bands.
Detection of TPO and SCF proteins by ELISA.
We chose representative cell lines classified based on the intensity of TPO-1 PCR bands (Fig 2A). TPO protein was detected in 10-fold concentrated culture supernatants of the cells in 8 of 10 cell lines tested, with a median concentration of 0.38 fmol/mL, ranging from 0.24 to 5.86 fmol/mL (Table 4). A hepatoma cell line (HepG2) showed a high level of TPO production. IL-1α exogenously added to the culture did not enhance the TPO production by any of the cell lines examined. The SCF levels were determined in the culture supernatants of T24, UT-M1, 86-2, LK-79, and VMRC-LCD cells and were found to be 82.0, 85.3, 84.8, less than 31.3, and less than 31.3 pg/mL, respectively.
Concentrations of TPO in the Culture Supernatants of Carcinoma Cells
| Cell Line . | Concentration of TPO (fmol/mL) . | |
|---|---|---|
| IL-1α (−) . | IL-1α (+)4-150 . | |
| T24 | 0.34 ± 0.05 | 0.28 ± 0.08 |
| HepG2 | 5.86 ± 0.44 | 5.38 ± 0.54 |
| UT-M1 | 0.44 ± 0.14 | 0.34 ± 0.06 |
| RERF-LC-MS | 0.25 ± 0.06 | 0.29 ± 0.07 |
| 86-2 | 0.24 ± 0.05 | 0.33 ± 0.08 |
| LK-79 | 0.29 ± 0.05 | 0.28 ± 0.06 |
| LU65 | 0.41 ± 0.12 | 0.53 ± 0.14 |
| VMRC-LCD | 0.78 ± 0.18 | 0.89 ± 0.14 |
| SK-HEP-1 | <0.20 | ND |
| Lc-1sq | <0.20 | ND |
| FCS | <0.20 | ND |
| RPMI/10% FCS | <0.20 | ND |
| Cell Line . | Concentration of TPO (fmol/mL) . | |
|---|---|---|
| IL-1α (−) . | IL-1α (+)4-150 . | |
| T24 | 0.34 ± 0.05 | 0.28 ± 0.08 |
| HepG2 | 5.86 ± 0.44 | 5.38 ± 0.54 |
| UT-M1 | 0.44 ± 0.14 | 0.34 ± 0.06 |
| RERF-LC-MS | 0.25 ± 0.06 | 0.29 ± 0.07 |
| 86-2 | 0.24 ± 0.05 | 0.33 ± 0.08 |
| LK-79 | 0.29 ± 0.05 | 0.28 ± 0.06 |
| LU65 | 0.41 ± 0.12 | 0.53 ± 0.14 |
| VMRC-LCD | 0.78 ± 0.18 | 0.89 ± 0.14 |
| SK-HEP-1 | <0.20 | ND |
| Lc-1sq | <0.20 | ND |
| FCS | <0.20 | ND |
| RPMI/10% FCS | <0.20 | ND |
Cells from each cell line were cultured at an initial cell density of 2 × 105/mL. At 48 hours of culture, supernatants were collected and concentrated 10-fold by ultrafiltration. The TPO assay was performed in triplicate in all cell lines examined. The data show TPO concentrations in each 10-fold concentrated supernatant. The lower limit of detection for TPO was 0.2 fmol/mL.
Abbreviation: ND, not done.
One hundred units per milliliter of IL-1α (4 ng/mL) was added at the initiation of culture.
Blood TPO levels in patients with advanced carcinomas with or without thrombocytosis.
In Table 5, clinical and laboratory findings and plasma TPO concentrations in individual patients are shown. The plasma TPO concentrations in patients with thrombocytosis were 3.46 ± 2.02 fmol/mL (mean ± SD, n = 13) and were significantly (P = .0003) higher than those in patients without thrombocytosis (0.91 ± 0.57 fmol/mL, n = 14). These blood TPO levels in cancer patients with thrombocytosis were comparable to those reported in patients with hepatoblastoma associated with thrombocytosis.21 The plasma TPO levels in patients without thrombocytosis were slightly higher than those in healthy volunteers (0.40 ± 0.28 fmol/mL, n = 99); however, the difference was not statistically significant.
Blood TPO Levels and Laboratory Data in Patients With Advanced Carcinomas With or Without Thrombocytosis
| Patient No. . | Age/ Sex . | Tumor . | Plasma TPO (fmol/mL) . | Platelet (×109/L) . | WBC (×109/L) . | Neutrophil (%) . | Hb (g/dL) . | CRP (mg/dL) . |
|---|---|---|---|---|---|---|---|---|
| 1 | 63/M | Stomach, carcinomatous pleuritis | 1.84 | 654 | 16.0 | 91 | 8.9 | 4.3 |
| 2 | 62/F | Lung, carcinomatous pleuritis | 3.18 | 600 | 9.5 | 59 | 11.4 | 3.4 |
| 3 | 47/F | Uterus | 8.67 | 798 | 11.1 | 83 | 9.9 | 4.4 |
| 4 | 59/F | Uterus | 4.20 | 712 | 12.6 | 54 | 12.6 | 0.4 |
| 5 | 58/M | Esophagus, multiple lymph node metastasis | 4.98 | 523 | 10.5 | 83 | 10.5 | 13.1 |
| 6 | 58/M | Esophagus, multiple lymph node metastasis | 0.34 | 550 | 13.4 | 81 | 13.4 | 4.7 |
| 7 | 58/M | Liver | 3.59 | 695 | 17.2 | 92 | 10.6 | 15.5 |
| 8 | 60/M | Stomach, multiple lymph node metastasis | 3.02 | 782 | 12.0 | 61 | 15.4 | 0.3 |
| 9 | 62/F | Gall bladder, multiple liver metastasis | 3.28 | 701 | 9.4 | 56 | 11.0 | 2.7 |
| 10 | 57/M | Larynx, multiple lung metastasis | 3.50 | 659 | 10.8 | 89 | 10.2 | 6.1 |
| 11 | 57/F | Uterus | 1.03 | 624 | 6.8 | 71 | 11.5 | 1.2 |
| 12 | 47/F | Breast, multiple bone metastasis | 4.10 | 587 | 9.3 | 58 | 8.5 | 8.9 |
| 13 | 47/M | Kidney, lung metastasis | 3.27 | 995 | 4.6 | 61 | 10.1 | 1.6 |
| 14 | 51/F | Uterus | 0.57 | 258 | 7.0 | 52 | 14.3 | 0.3 |
| 15 | 56/M | Kidney | 0.21 | 193 | 5.0 | 41 | 11.3 | 0.3 |
| 16 | 72/M | Lung, carcinomatous pleuritis | 0.88 | 358 | 12.1 | 68 | 12.8 | 4.5 |
| 17 | 69/M | Lung, carcinomatous pleuritis | 0.21 | 180 | 11.6 | 42 | 11.1 | 0.5 |
| 18 | 65/M | Lung, lymph node metastasis | 1.06 | 139 | 4.5 | 62 | 11.8 | 0.5 |
| 19 | 61/F | Stomach | 0.30 | 229 | 6.7 | 39 | 13.9 | 0 |
| 20 | 75/F | Colon, multiple lung metastasis | 1.70 | 243 | 4.6 | 70 | 11.5 | 0 |
| 21 | 59/M | Esophagus | 1.78 | 253 | 4.5 | 56 | 10.5 | 0.4 |
| 22 | 71/F | Stomach | 0.63 | 243 | 4.1 | 40 | 9.8 | 0 |
| 23 | 69/F | Rectum | 1.27 | 140 | 2.6 | 45 | 10.1 | 0.1 |
| 24 | 69/M | Bile duct, multiple liver metastasis | 1.47 | 174 | 6.0 | 68 | 13.2 | 1.4 |
| 25 | 74/F | Stomach, multiple liver metastasis | 1.64 | 307 | 7.5 | 66 | 10.8 | 4.2 |
| 26 | 80/F | Stomach | 0.34 | 225 | 5.7 | 59 | 10.1 | 0.5 |
| 27 | 77/F | Duodenum, liver metastasis | 0.66 | 179 | 4.7 | 77 | 9.8 | 0.9 |
| Patient No. . | Age/ Sex . | Tumor . | Plasma TPO (fmol/mL) . | Platelet (×109/L) . | WBC (×109/L) . | Neutrophil (%) . | Hb (g/dL) . | CRP (mg/dL) . |
|---|---|---|---|---|---|---|---|---|
| 1 | 63/M | Stomach, carcinomatous pleuritis | 1.84 | 654 | 16.0 | 91 | 8.9 | 4.3 |
| 2 | 62/F | Lung, carcinomatous pleuritis | 3.18 | 600 | 9.5 | 59 | 11.4 | 3.4 |
| 3 | 47/F | Uterus | 8.67 | 798 | 11.1 | 83 | 9.9 | 4.4 |
| 4 | 59/F | Uterus | 4.20 | 712 | 12.6 | 54 | 12.6 | 0.4 |
| 5 | 58/M | Esophagus, multiple lymph node metastasis | 4.98 | 523 | 10.5 | 83 | 10.5 | 13.1 |
| 6 | 58/M | Esophagus, multiple lymph node metastasis | 0.34 | 550 | 13.4 | 81 | 13.4 | 4.7 |
| 7 | 58/M | Liver | 3.59 | 695 | 17.2 | 92 | 10.6 | 15.5 |
| 8 | 60/M | Stomach, multiple lymph node metastasis | 3.02 | 782 | 12.0 | 61 | 15.4 | 0.3 |
| 9 | 62/F | Gall bladder, multiple liver metastasis | 3.28 | 701 | 9.4 | 56 | 11.0 | 2.7 |
| 10 | 57/M | Larynx, multiple lung metastasis | 3.50 | 659 | 10.8 | 89 | 10.2 | 6.1 |
| 11 | 57/F | Uterus | 1.03 | 624 | 6.8 | 71 | 11.5 | 1.2 |
| 12 | 47/F | Breast, multiple bone metastasis | 4.10 | 587 | 9.3 | 58 | 8.5 | 8.9 |
| 13 | 47/M | Kidney, lung metastasis | 3.27 | 995 | 4.6 | 61 | 10.1 | 1.6 |
| 14 | 51/F | Uterus | 0.57 | 258 | 7.0 | 52 | 14.3 | 0.3 |
| 15 | 56/M | Kidney | 0.21 | 193 | 5.0 | 41 | 11.3 | 0.3 |
| 16 | 72/M | Lung, carcinomatous pleuritis | 0.88 | 358 | 12.1 | 68 | 12.8 | 4.5 |
| 17 | 69/M | Lung, carcinomatous pleuritis | 0.21 | 180 | 11.6 | 42 | 11.1 | 0.5 |
| 18 | 65/M | Lung, lymph node metastasis | 1.06 | 139 | 4.5 | 62 | 11.8 | 0.5 |
| 19 | 61/F | Stomach | 0.30 | 229 | 6.7 | 39 | 13.9 | 0 |
| 20 | 75/F | Colon, multiple lung metastasis | 1.70 | 243 | 4.6 | 70 | 11.5 | 0 |
| 21 | 59/M | Esophagus | 1.78 | 253 | 4.5 | 56 | 10.5 | 0.4 |
| 22 | 71/F | Stomach | 0.63 | 243 | 4.1 | 40 | 9.8 | 0 |
| 23 | 69/F | Rectum | 1.27 | 140 | 2.6 | 45 | 10.1 | 0.1 |
| 24 | 69/M | Bile duct, multiple liver metastasis | 1.47 | 174 | 6.0 | 68 | 13.2 | 1.4 |
| 25 | 74/F | Stomach, multiple liver metastasis | 1.64 | 307 | 7.5 | 66 | 10.8 | 4.2 |
| 26 | 80/F | Stomach | 0.34 | 225 | 5.7 | 59 | 10.1 | 0.5 |
| 27 | 77/F | Duodenum, liver metastasis | 0.66 | 179 | 4.7 | 77 | 9.8 | 0.9 |
In each patient, TPO concentration in the citrated plasma was measured by an ELISA kit. The lower limits of detection for TPO was 0.2 fmol/mL. The plasma TPO concentrations in healthy volunteers were 0.40 ± 0.28 fmol/mL (mean ± SD, n = 99). The laboratory data are from the samples simultaneously obtained for TPO determination. The normal range of platelet count was 150 to 370 × 109/L. The normal range of CRP was less than 0.5 mg/dL. From patient no. 5, ES-O cell line was established (see Materials and Methods).
Abbreviations: Hb, hemoglobin; CRP, C-reactive protein.
DISCUSSION
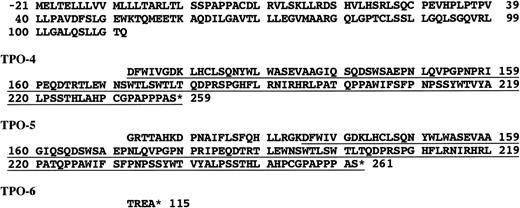
In this study, we demonstrated TPO production by carcinoma cells originating from various tumors both at the mRNA and protein levels. Regarding the isoforms of TPO mRNA, we identified 3 novel isoforms (TPO-4, TPO-5, and TPO-6) as well as previously reported forms (TPO-1, TPO-2, and TPO-3). TPO-3, TPO-4, and TPO-5 yield frameshifts and TPO-6 contains a stop codon in the inserted sequence (Figs 1 and 4). Regarding biological activity of TPO-5 and TPO-6, culture supernatants of COS-1 cells transfected with TPO-5 or TPO-6 cDNA did not stimulate the growth of TPO-responsive cells. Western blot analysis showed no detectable protein of TPO-5 or TPO-6 in the culture supernatants of transfected COS-1 cells, whereas the analysis demonstrated TPO-5 but not TPO-6 protein in cell lysates of the COS-1 cells. These results suggest poor extracellular secretion of TPO-5 protein and poor protein synthesis of TPO-6. Therefore, biological activity of TPO-5 and TPO-6 remains unclear and to be examined. However, it has been reported in humans that the biological activity of TPO isoforms is abolished if the truncation extends into the region that shares homology with the erythropoietin (EPO) mRNA (EPO-like domain).47 The EPO-like domain (amino acid residues 1-154) activates mpl and the structure of the domain is supposed to be stabilized by disulfide bonds between cysteins 1 and 4 and cysteins 2 and 3. Replacement of either cystein 1 or 4 completely abrogates biological activity.48 In TPO-5, the position of cystein 4 is changed from 151 to 145 due to frameshift. This may prevent cysteins 1 and 4 to form the bonds. TPO-6 lacks cystein 4 because of the stop codon in the insert between exons 5 and 6 (Figs 1 and 4). These findings suggest poor biological activity of TPO-5 and TPO-6, although the possibility that these isoforms, especially TPO-5, act as a membrane-bound ligand for mpl still remains. Regarding the activity of TPO-4, mouse TPO-4 protein has comparable biological activity to TPO-1 and the apparently low activity of TPO-449 results from the poor extracellular secretion of the truncated protein.50 Therefore, human TPO-4 should be characterized with respect to its thrombopoietic activity.
Deduced amino acid sequences of TPO-4, TPO-5, and TPO-6. 5′ terminal sequences down to Gln-111 are common with TPO-1 (top). TPO-4 and TPO-5 contain the same sequence derived due to the frameshift (underlined).
Deduced amino acid sequences of TPO-4, TPO-5, and TPO-6. 5′ terminal sequences down to Gln-111 are common with TPO-1 (top). TPO-4 and TPO-5 contain the same sequence derived due to the frameshift (underlined).
It has been reported that the level of TPO mRNA expression in the liver or kidney is unchanged, regardless of the platelet count.24Therefore, it is assumed that the blood TPO level is regulated by platelets expressing abundant TPO receptors that absorb TPO.51,52 On the other hand, the cytokine regulation of TPO production is poorly understood. Only 1 study regarding this was performed using a human hepatoma cell line HepG2; however, all cytokines tested did not have any effect on the TPO mRNA expression by this cell line.18 In the present study, exogenously added proinflammatory cytokine, IL-1α, which is a potent inducer of IL-6, IL-8, G-CSF, or GM-CSF in normal macrophages or in some carcinomas,39 40 did not affect the TPO production by the carcinoma cells examined. Furthermore, TPO production was not correlated with the production of IL-1α, IL-6, or CSFs by these carcinoma cells. Therefore, TPO production in carcinomas may be independent of the expression of these cytokines. Thus, it would be very interesting and important to identify regulatory factors for TPO production.
In the present study, the amount of TPO produced by carcinoma cells, except for HepG2 cells, appears to be minute. Higher levels of production of TPO by HepG2 may reflect the potency of normal hepatocytes with respect to the production of TPO. Several reports have described marked thrombocytosis in patients with hepatocellular carcinomas21,53,54; however, TPO production by tumor cells was not determined. On the other hand, even for a relatively low level of production, the amount of TPO may not be negligible when a patient has a high tumor burden. Indeed, in this study, we observed high blood TPO levels in almost all patients with advanced carcinomas associated with thrombocytosis greater than 500 × 109/mL. Whereas blood TPO levels in patients with advanced carcinomas without thrombocytosis were almost equal to those in healthy controls, these results indicate that TPO is involved in the carcinoma-associated thrombocytosis, although the exact contribution of TPO produced by carcinomas to the thrombocytosis remains to be determined. We also detected SCF in the culture supernatants in 3 of 5 TPO-producing cell lines examined. SCF acts synergistically with TPO in the proliferation of megakaryocyte progenitors.52 55 Therefore, the action of TPO may be amplified by SCF produced by tumors in some patients. This appears to further support the hypothesis of TPO-induced thrombocytosis in carcinoma patients.
In conclusion, some carcinomas produce TPO that might be involved, in part, in the carcinoma-associated thrombocytosis. However, the cause of thrombocytosis is rather complicated, because certain carcinomas produce multiple cytokines that exhibit Meg-Pot and/or Meg-CSF activities, such as SCF, IL-6, IL-11, and GM-CSF, as well as TPO. Indeed, in this study, blood TPO levels were not correlated with platelet counts in cancer patients with thrombocytosis. This fact suggests that other thrombopoietic factors were involved besides TPO in the thrombocytosis in these cancer patients. Thus, further studies are required to clarify the exact roles of individual cytokines in carcinoma-associated thrombocytosis.
ACKNOWLEDGMENT
The authors are grateful to Kyoko Tanaka and Eiko Yamashita (Kobe City General Hospital, Kobe, Japan) for preparing plasmas from patients with carcinomas.
Supported in part by the Sasaki Foundation for the Promotion of Leukemia Research, by the Smoking Research Foundation, and by the Kobe City Foundation for the Promotion of Medical Research (to T.T.).
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Takayuki Takahashi, MD, Department of Hematology and Clinical Immunology, Kobe City General Hospital, 4-6 Minatojima Nakamachi, Chuo-ku, Kobe 650-0046, Japan.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal