Abstract
Most primitive hematopoietic progenitor cells reside in vivo within the G0/G1 phase of the cell cycle. By simultaneous DNA/RNA staining it is possible to distinguish G0 and G1 states and to isolate cells in defined phases of the cell cycle. We report here the use of cell cycle fractionation to separate human mobilized peripheral blood (MPB) CD34+ cells capable of repopulating the bone marrow (BM) of non-obese diabetic/severe combined immune-deficient (NOD/SCID) mice. In freshly isolated MPB, repopulating cells were predominant within the G0 phase, because transplantation of CD34+cells residing in G0 (G0CD34+) resulted on average in a 16.6- ± 3.2-fold higher BM chimerism than infusion of equal numbers of CD34+ cells isolated in G1. We then investigated the effect of ex vivo cell cycle progression, in the absence of cell division, on engraftment capacity. Freshly isolated G0CD34+ cells were activated by interleukin-3 (IL-3), stem cell factor (SCF), and flt3-ligand (FL) for a 36-hour incubation period during which a fraction of cells progressed from G0 into G1 but did not complete a cell cycle. The repopulating capacity of stimulated cells was markedly diminished compared with that of unmanipulated G0CD34+ cells. Cells that remained in G0 during the 36-hour incubation period and those that traversed into G1 were sorted and assayed separately in NOD/SCID recipients. The repopulating ability of cells remaining in G0 was insignificantly reduced compared with that of unstimulated G0CD34+ cells. On the contrary, CD34+ cells traversing from G0 into G1 were largely depleted of repopulating capacity. Similar results were obtained when G0CD34+ cells were activated by the combination of thrombopoietin-SCF-FL. These studies provide direct evidence of the quiescent nature of cells capable of repopulating the BM of NOD/SCID mice. Furthermore, these data also demonstrate that G0-G1 progression in vitro is associated with a decrease in engraftment capacity.
© 1998 by The American Society of Hematology.
IN VITRO MANIPULATION of hematopoietic stem cells (HSC) has been the focus of numerous studies. Two main objectives have been under evaluation: HSC expansion and somatic gene therapy. The use of expanded grafts would in theory speed up the hematological recovery after HSC transplantation and/or allow for the use of small HSC collections, such as cord blood samples.1 Information collected from ex vivo expansion studies is also critical to design gene transfer protocols, because retroviral transduction requires in vitro cycling of the target cells.2 3
In defining strategies for HSC expansion or gene therapy, a decisive factor to consider is the responsiveness of the most primitive cells to cytokine stimulation in vitro. This is largely dependent on the cell cycle status of the target cells, as cycling cells will be able to respond quickly to mitogenic factors, whereas more quiescent cells will not.4-7 In addition, cell cycle activation may have a negative effect on the engraftment capability. Studies in murine models have documented an engraftment defect of stimulated HSC: in vitro HSC activation by various combinations of hematopoietic growth factors resulted in a decrease of in vivo repopulating ability, compared with unmanipulated marrow.8-10 Consistent with these results were data acquired in our laboratory by PKH membrane cell tracking11 that demonstrated the superiority of quiescent cells over proliferating cells in rescuing lethally irradiated recipients. In another report, evidence was presented that not only in vitro stimulation, but also in vivo HSC cycling, as observed after 5-fluorouracil (5-FU) treatment, resulted in transient alterations in the functional state of HSC, leading to an engraftment defect.12
In humans, experimental studies examining the impact of cell cycle status on engraftment capacity have been unattainable due to the absence of an in vivo model of human HSC. Xenotransplant models have been recently developed which can address this question, most notably the in vivo severe combined immune-deficient (SCID) mouse repopulating cell (SRC) assay.13 In this model, human HSC intravenously injected into immunodeficient recipients home to the bone marrow and are able to proliferate to a large extent and differentiate into various lineages.14 15 High levels of chimerism are especially achieved with the non-obese diabetic/SCID (NOD/SCID) strain, which was used in the present study.
To investigate the relationship of cell cycle status with the engraftment capability of human hematopoietic cells, we took advantage of a new method of cell cycle analysis and fractionation recently developed in our laboratory.16-18 Conventional cell cycle analysis using DNA dyes classifies cells in the G0/G1 phase as noncycling cells and cells in the S/G2+M phase as cycling cells. This approach is of limited utility when applied to the characterization of the cell cycle status of human hematopoietic cells, because more than 85% of bone marrow (BM) CD34+ cells and almost all of mobilized peripheral blood (MPB) CD34+ cells are in the G0/G1 phase. Simultaneous DNA/RNA staining with Hoechst 33342 (Hst) and Pyronin Y (PY) allows for further fractionation of the G0/G1 phase. Using this procedure, we have been able to isolate viable CD34+ cells in the G0 or G1 phase of the cell cycle and examine their properties in vitro.16G0CD34+ cells respond slowly to cell cycle activation in cytokine-driven liquid culture, whereas G1CD34+ cells proliferate immediately when exposed to the same conditions.18 In addition, we have shown by in vitro assays that the functional heterogeneity of human CD34+ cells is correlated with their position within the G0/G1 phase, with the G0compartment being enriched in primitive hematopoietic cells.17 In the present study, we have used Hst/PY staining to analyze the NOD/SCID repopulating ability of MPB human CD34+ cells isolated in G0 or G1. Two main questions were addressed. First, by determining the repopulating activity of freshly isolated CD34+ cells in G0 or in G1, we assessed the cell cycle status of putative stem cells. Second, the effect of cell cycle activation on engraftment capability was investigated by transplanting animals with CD34+ cells initially isolated in G0 and then stimulated to progress into G1 by in vitro exposure to cytokines.
MATERIALS AND METHODS
Mice.
NOD/LtSz-scid/scid (NOD/SCID)19 animals were kindly provided by Dr Leonard Shultz (Jackson Laboratory, Bar Harbor, ME). Mice were housed in microisolators under pathogen-free conditions and received autoclaved food and acidified water ad libitum. Animal experiments were performed in accordance with institutional guidelines approved by the Animal Care Committee of the Indiana University School of Medicine.
Human cells.
BM and MPB samples were obtained from healthy adult volunteers according to the guidelines established by the Human Investigation Committee of the Indiana University School of Medicine. Mobilization was achieved by daily granulocyte colony-stimulating factor (G-CSF) administration at 5 μg/kg (maximum, 480 μg/d) for 4 consecutive days. MPB cells were collected by apheresis on day 5. MPB CD34+ cells were isolated by immunomagnetic selection using a large scale Isolex 300i system (Baxter Healthcare, Irvine, CA) as per the manufacturer’s instructions. CD34+ cell purity in the selected product always exceeded 95%. In one experiment, BM cells instead of MPB cells were used. BM cells were pooled from 5 normal donors and selected with the same procedure. CD34+ cell purity of this BM collection was 86%.
Cell cycle fractionation with Hst and Pyronin Y.
Fresh or cultured CD34+ cells were resuspended at 5 × 106 cells/mL in a 1 μg/mL solution of Hst (Molecular Probes, Eugene, OR) in Hst buffer. Hst buffer consisted of Hanks Balanced Salt Solution (HBSS; Biowhittaker, Walkersville, MD), 20 mmol/L HEPES (Biowhittaker), 1 g/L glucose, and 10% fetal calf serum (FCS; Hyclone, Logan, UT). After incubation at 37°C for 45 minutes, PY (Sigma, St Louis, MO), prepared in Hst Buffer, was added at a final concentration of 1 μg/mL and cells were further incubated for another 45 minutes at 37°C. Cells were washed once, resuspended in Hst buffer, and sorted on a FACStar Plus equipped with an argon laser providing the 488 nm excitation for PY and a krypton laser providing the 350 nm excitation for Hst. PY signal was selected with a 575 ± 13 nm bandpass filter and Hst was detected with a 424 ± 22 nm bandpass filter. Sorting windows were constructed as depicted in Fig 1. Cells were kept on ice during sorting to minimize dye leaking and were protected from light. Viability of sorted cells always exceeded 98%. No toxic effect of Hst/PY staining on cell proliferation, colony formation, long-term culture-initiating cell (LTC-IC) frequency and NOD/SCID repopulating activity was detected (data not shown).
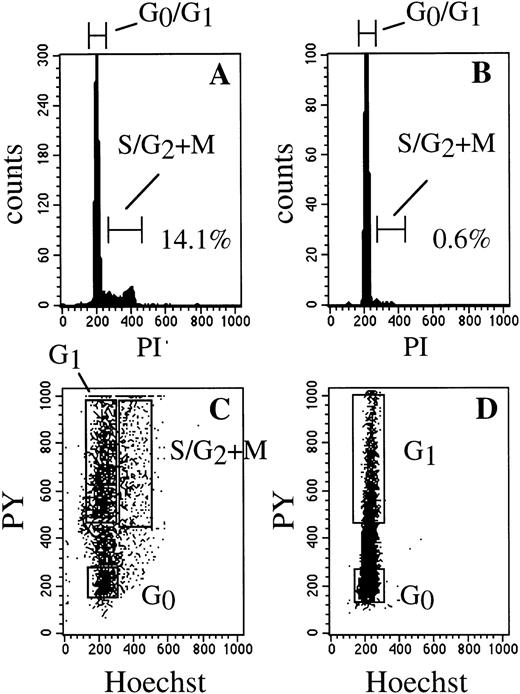
Single- and dual-parameter cell cycle analysis of BM and MPB CD34+ cells. DNA histogram of BM (A) and MPB (B) CD34+ cells, respectively, showing the relative absence of replicating progenitor cells in MPB. Simultaneous DNA/RNA staining with Hst and PY, identifying G0 and G1 regions in similar samples of BM (C) and MPB (D) CD34+ cells.
Single- and dual-parameter cell cycle analysis of BM and MPB CD34+ cells. DNA histogram of BM (A) and MPB (B) CD34+ cells, respectively, showing the relative absence of replicating progenitor cells in MPB. Simultaneous DNA/RNA staining with Hst and PY, identifying G0 and G1 regions in similar samples of BM (C) and MPB (D) CD34+ cells.
High resolution cell cycle analysis.
Cells were analyzed for Ki-67 expression and DNA content as recently described by Jordan et al,20 with minor modification. Cells were washed and resuspended in 1 mL phosphate-buffered saline (PBS) + 0.4% formaldehyde. After 30 minutes at 4°C, 1 mL of PBS + 0.2% Triton X-100 was added and cells were left overnight at 4°C. Cells were then washed twice in PBS + 1% bovine serum albumin (BSA) and stained with fluorescein isothiocyanate (FITC)-conjugated anti-Ki-67 (clone MIB-1; Immunotech, Westbrook, ME) for 60 minutes at 4°C. Isotype controls were stained in parallel. Finally, cells were washed and resuspended in PBS + 1% BSA containing 5 μg/mL 7-aminoactinomycin-D (7-AAD; Sigma). After 3 hours of incubation on ice, samples were run on a FACScan flow cytometer (BDIS, San Jose, CA) using FL-1 and FL-3 channels for Ki-67 and 7-AAD, respectively.
Human progenitor cell assay.
Human CD34+ cells were assayed in 1.3% methylcellulose, 30% FCS, 100 ng/mL stem cell factor (SCF), 10 ng/mL interleukin-3 (IL-3), 10 ng/mL IL-6, 5 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF), and 2 U/mL erythropoietin (EPO) suspended in Iscove’s modified Dulbecco’s medium (IMDM). When unseparated BM cells from NOD/SCID recipient mice were used, IL-6 was omitted to avoid the growth of murine progenitors.14 21The selectivity of the assay for human progenitors was confirmed by polymerase chain reaction (PCR) detection of human β-globin gene in individual colonies (see below). Hematopoietic colonies were scored after 2 weeks according to standard criteria.
LTC-IC assay by limiting dilution analysis.
M2-10B4 cells,22 obtained from the American Type Culture Collection (Rockville, MD), were used to establish stromal layers. M2-10B4 cells harvested from large-scale cultures in RPMI 1640 with 10% FCS were irradiated at 8,000 cGy and plated in 96-well plates at 15,000 cells/well in 100 μL long-term culture medium (LTCM). LTCM consisted of Myelocult (Stem Cell Technologies, Vancouver, British Columbia, Canada) containing 10−6 mmol/L hydrocortisone (Sigma). Within 1 week, human test cells were plated in limiting dilution at 24 wells/cell dose in another 100 μL LTCM and maintained at 37°C in 100% humidified atmosphere containing 5% CO2, with weekly half-medium change. After 5 to 6 weeks, 120 μL medium were removed from each well followed by the addition of 150 μL of a mixture consisting of 3 parts FCS and 4 parts 3.3% methylcellulose and containing at final concentration 5 × 10−2 mmol/L 2-mercaptoethanol, 100 ng/mL SCF, 25 ng/mL IL-3, 25 ng/mL IL-6, 25 ng/mL GM-CSF, and 2 U/mL EPO. After an additional 2 weeks, wells were scored for the presence or absence of hematopoietic colonies and the frequency of LTC-IC was calculated using the maximum likelihood estimator.23
Short-term culture.
CD34+ cells initially isolated in G0 were plated in a serum-free medium consisting of IMDM supplemented with 25 mmol/L HEPES (Biowhittaker), 10 μg/mL BSA, 10 μg/mL bovine insulin, 200 μg/mL transferrin (all from Stem Cell Technologies), 2 mmol/L alanyl-glutamine, 1% (vol/vol) lipids cholesterol-rich, 1 mmol/L sodium pyruvate (all from Sigma), 100 U/mL penicillin, 100 μg/mL streptomycin, and 5 × 10−2 mmol/L 2-mercaptoethanol. Cells were stimulated during 36 hours by a combination of 50 ng/mL IL-3, 100 ng/mL SCF, and 100 ng/mL flt-3 ligand (FL) or a combination of 50 ng/mL thrombopoietin (TPO), 100 ng/mL SCF, and 100 ng/mL FL. Viability of cultured cells was always greater than 98% as judged by trypan blue exclusion.
Transplantation of human cells into NOD/SCID mice.
Twelve- to 14-week-old NOD/SCID mice were sublethally irradiated with 300 cGy from a 137Cs source (GammaCell 40; Nordion International, Kanata, Ontario, Canada). Mice received 10 × 106 nonadherent CD34−cells irradiated with 2,000 cGy, as accessory cells, by intravenous tail injection. Two hours later, mice were transplanted with fresh or cultured CD34+ cells. Animals were not treated with cytokines during the experiments. After 6 to 7 weeks,14 24mice were killed by cervical dislocation and bone marrow cells were harvested from femurs and tibias by flushing the bones with HBSS-5% FCS. Nucleated cells were isolated by centrifugation over Ficoll-Paque (Pharmacia Fine Chemicals, Piscataway, NJ), washed, and resuspended in IMDM with 10% FCS for further analyses.
Flow cytometric analysis of engraftment.
Between 1.0 × 105 and 2.5 × 105NOD/SCID BM cells were pelletted, resuspended in 50 μL mouse serum (Sigma), and incubated with various mouse antihuman monoclonals for 20 minutes at 4°C. FITC-conjugated antibodies included anti-CD45, CD33, CD19, CD15 (BDIS), and CD38 (Immunotech). Phycoerythrin (PE)-conjugated anti-CD34 was obtained from BDIS and anti-CD45-PE was obtained from Pharmingen (San Diego, CA). Samples were analyzed on a FACScan (BDIS). Positive cells were identified by comparison with isotypic controls and with cells harvested from control (not transplanted) NOD/SCID mice stained with the same antibodies.
In the case of highly engrafted mice (>10% CD45+ cells), CD45+CD34+ cells were sorted on a FACStar Plus (BDIS) and assayed for their progenitor and LTC-IC frequencies.
PCR detection of human β-globin gene.
Briefly, individual colonies were plucked and transferred into Eppendorf tubes, lyzed with 500 μL water, and pelletted. DNA was extracted with InstaGene matrix (Bio-Rad, Hercules, CA) as per the manufacturer’s instructions. Positive controls consisted of individual colonies grown from purified human CD34+ cells and negative controls were samples of 103 and 10 × 103 murine BM cells harvested from a control animal. PCR was performed using a 20-bp 5′ primer GAA TCC AGA TGC TCA AGG CC and a 20-bp 3′ primer CAA TCC AGC TAC CAT TCT GCamplifying a 345-bp fragment of human β-globin gene. After an initial denaturation step of 5 minutes at 94°C, a hot start at 85°C was used, followed by 40 cycles consisting of 4 minutes at 94°C, 2 minutes at 56°C, and 1.5 minutes at 72°C. The final cycle had a 10-minute extension step. PCR products were analyzed on a 1.5% agarose gel after staining with ethidium bromide.
Growth factors.
Human recombinant IL-3, IL-6, SCF, TPO, and GM-CSF were kind gifts from Amgen (Thousand Oaks, CA). Human recombinant EPO was obtained from Amgen. Human recombinant FL was a kind gift from Immunex (Seattle, WA).
Statistical analysis.
Comparisons were made using the Student’s t-test. AllP values are two-sided.
RESULTS
Cell cycle fractionation of MPB CD34+ cells by staining with Hst and PY.
We17,25 and others26,27 have already reported the homogeneous G0/G1 cell cycle status of MPB CD34+ cells compared with their BM counterparts. When analyzed with a standard DNA histogram, up to 15% of BM CD34+ cells are in the S/G2+M phase, whereas less than 1% of MPB CD34+ cells are in the same actively cycling compartment (Fig 1A and B). Thus, the vast majority of MPB CD34+ cells cannot be ascribed to a precisely defined position in the cell cycle, because cells in G0 and in G1 have the same DNA content. Simultaneous DNA/RNA staining with Hst and PY, respectively, was used in the present study to discriminate the G0 phase from the G1 phase of the cell cycle (Fig 1C and D). Cells in G0 were identified by minimal RNA content, whereas cells traversing into G1were defined as cells with maximal RNA staining. The validity of this approach has been demonstrated in previous reports by kinetic and phenotypic data from this laboratory.16-18 Most notably, expression of Ki-67, a nuclear antigen specifically expressed by cycling cells,20 was restricted to PYhighcells, whereas PYlow cells were Ki-67 negative.
Differential cell cycle status of colony-forming cells (CFC) and LTC-IC in MPB CD34+cells.
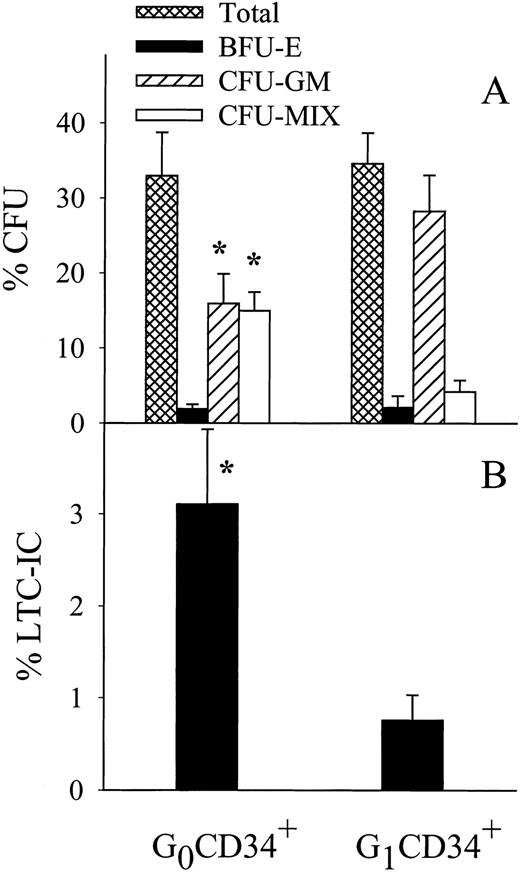
The frequency of late and primitive progenitor cells was determined in CD34+ cells isolated in G0 or in G1by standard CFC and LTC-IC assays, respectively. The overall clonogenic activity was very similar, approximately 30%, in G0 and G1CD34+ cells (P > .05; Fig 2A). However, as already reported for BM CD34+ cells,17 consistent differences were observed in the distribution of the different types of progenitors: the G0 compartment was relatively enriched in multipotential progenitors (colony-forming unit-mixed [CFU-Mix]; 15% in G0v 4% in G1; P < .05), whereas there were more committed myeloid progenitors in G1(colony-forming unit–granulocyte-macrophage [CFU-GM]; 16% in G0v 28% in G1; P < .05).
In vitro functional assays of MPB CD34+cells isolated in G0 or in G1 phase of the cell cycle. (A) Progenitor cell assay. Numbers of hematopoietic colonies are given per 100 cells plated. Data shown are the mean ± SEM of four experiments performed in duplicate. Total indicates total number of hematopoietic colonies; BFU-E, burst-forming unit-erythroid; CFU-GM, colony-forming unit-granulocyte/macrophage; CFU-MIX, CFU-Mixed. (B) Frequencies of LTC-IC among G0 and G1CD34+ cells. Frequencies per 100 cells are reported as the mean ± SEM, n = 4. *P < .05 versus G1CD34+ cells, paired t-tests.
In vitro functional assays of MPB CD34+cells isolated in G0 or in G1 phase of the cell cycle. (A) Progenitor cell assay. Numbers of hematopoietic colonies are given per 100 cells plated. Data shown are the mean ± SEM of four experiments performed in duplicate. Total indicates total number of hematopoietic colonies; BFU-E, burst-forming unit-erythroid; CFU-GM, colony-forming unit-granulocyte/macrophage; CFU-MIX, CFU-Mixed. (B) Frequencies of LTC-IC among G0 and G1CD34+ cells. Frequencies per 100 cells are reported as the mean ± SEM, n = 4. *P < .05 versus G1CD34+ cells, paired t-tests.
As for more primitive cells (Fig 2B), the G0 compartment was significantly enriched in LTC-ICs compared with the G1compartment (3.1% for G0CD34+ cells v0.8% for G1CD34+ cells; P < .05).
NOD/SCID repopulating ability of MPB CD34+cells isolated in G0 or in G1.
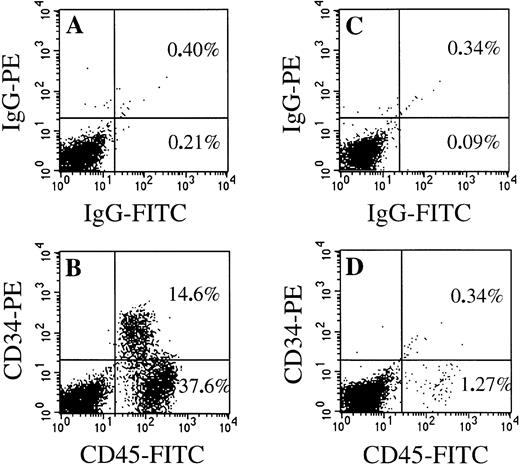
Comparison of the repopulating ability of G0CD34+ and G1CD34+cell populations was assessed by transplanting equal numbers of either cell fraction sorted from single-donor MPB samples. After 6 to 7 weeks,14 24 the extent of human cell engraftment was evaluated by flow cytometric determination of human CD45+and/or CD34+ cells in suspensions of BM cells harvested from recipient mice. High numbers of human CD45+cells (up to 75% after injection of 2 × 106 cells) were detected in the BM of animals transplanted with G0CD34+ cells. Of interest is the fact that a large fraction of chimeric human CD45+ cells was also CD34+ (Fig 3B). In sharp contrast, low numbers of CD45+ cells were demonstrated after transplantation of G1CD34+ cells and chimeric CD34+ cells were mostly undetectable (Fig 3D). In four separate experiments in which MPB CD34+ cells sorted in either G0 or G1 were transplanted at cell doses ranging from 2 × 106 to 0.7 × 106, the repopulating activity of G0CD34+ cells was consistently severalfold higher than that of G1CD34+ cells. The percentage of human CD45+ cells in mice receiving G0CD34+ cells was on average 16-fold higher (range, 12.3- to 19.1-fold; P < .05, pairedt-test) than in mice injected with G1CD34+ cells (Fig4A). In one additional experiment in which fractions of BM CD34+ cells instead of MPB CD34+ cells were used as grafts, similar results were obtained: at a cell dose of 0.8 × 106 cells transplanted, the average percentage of chimeric human CD45+ cells was 3.6% in mice transplanted with G0CD34+ cells (n = 2 mice) and only 0.2% in animals receiving G1CD34+ cells (n = 3 mice).
Comparison of FACScan analysis of BM cells harvested from NOD/SCID mice transplanted 6 weeks previously with 1.0 × 106 MPB CD34+ cells isolated in G0 or in G1 phase of the cell cycle. Cells were stained either with isotypic control antibodies (upper panels) or with antihuman CD45-FITC and antihuman CD34-PE (lower panels). (A and B) Mouse transplanted with G0CD34+ cells; (C and D) mouse transplanted with G1CD34+ cells.
Comparison of FACScan analysis of BM cells harvested from NOD/SCID mice transplanted 6 weeks previously with 1.0 × 106 MPB CD34+ cells isolated in G0 or in G1 phase of the cell cycle. Cells were stained either with isotypic control antibodies (upper panels) or with antihuman CD45-FITC and antihuman CD34-PE (lower panels). (A and B) Mouse transplanted with G0CD34+ cells; (C and D) mouse transplanted with G1CD34+ cells.
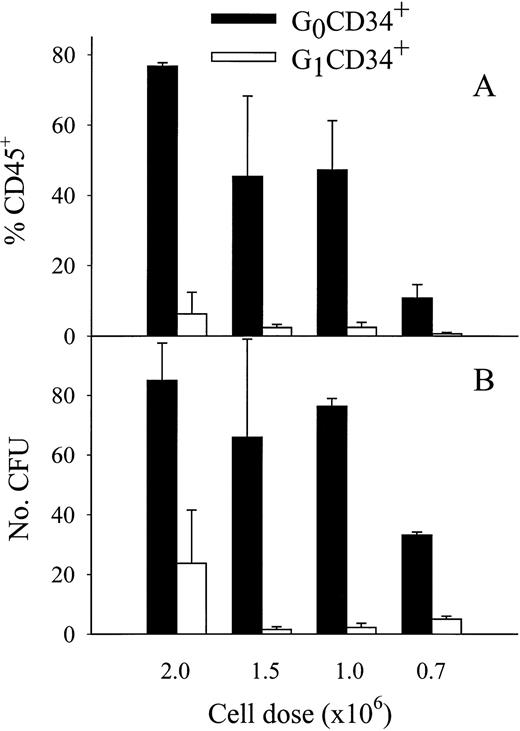
Comparison of engraftment capacity of MPB CD34+ cells isolated in G0 or in G1 phase of the cell cycle. Data from four experiments are reported as the mean ± SEM. Each experiment was performed with MPB CD34+ cells isolated from a different donor (n = 2 to 4 animals per experiment). (A) Percentages of chimeric human CD45+ cells in the BM of mice transplanted 6 weeks previously with indicated numbers of G0 or G1CD34+ cells. Average chimerism was statistically higher after transplantation of G0CD34+ cells than after transplantation of G1CD34+ cells (P < .05, pairedt-test). (B) Numbers of human progenitor cells per 50 × 103 BM cells 6 weeks posttransplantation in the same recipient mice. Average human progenitor output was statistically higher in G0- versus G1-transplanted mice (P < .05, paired t-test).
Comparison of engraftment capacity of MPB CD34+ cells isolated in G0 or in G1 phase of the cell cycle. Data from four experiments are reported as the mean ± SEM. Each experiment was performed with MPB CD34+ cells isolated from a different donor (n = 2 to 4 animals per experiment). (A) Percentages of chimeric human CD45+ cells in the BM of mice transplanted 6 weeks previously with indicated numbers of G0 or G1CD34+ cells. Average chimerism was statistically higher after transplantation of G0CD34+ cells than after transplantation of G1CD34+ cells (P < .05, pairedt-test). (B) Numbers of human progenitor cells per 50 × 103 BM cells 6 weeks posttransplantation in the same recipient mice. Average human progenitor output was statistically higher in G0- versus G1-transplanted mice (P < .05, paired t-test).
The presence of human clonogenic cells in BM low-density cells harvested from recipient mice was also determined by a progenitor cell assay selective for human cells.14 21 The numbers of engrafted human progenitors were in good correlation with those of CD45+ cells (Fig 4B), indicating that functional human hematopoietic cells were present in chimeric mice. Human progenitors in the marrow were on average 22-fold more numerous in mice transplanted with G0CD34+ cells than in those receiving G1CD34+ cells (P < .05, pairedt-test). The selectivity of the assay for human clonogenic cells was confirmed by PCR amplification of the human β-globin gene in DNA extracts prepared from individual colonies. In two experiments in which DNA from individual colonies derived from the BM of 2 to 4 mice was analyzed by PCR, human sequences were detected in 23 of 24 progenitors.
Differentiative capacity of repopulating cells present in MPB G0CD34+ cells.
The phenotypic profile of engrafted CD45+ cells in G0-transplanted mice was determined by two-color staining (Table 1). A mean of 19.9% of CD45+ cells were also CD34+ 6 to 7 weeks after transplantation. Expression of CD19 and CD33 antigens on 55.7% and 34.2%, respectively, of human CD45+ cells demonstrated the presence of repopulating cells with lympho-myeloid potential. The same phenotyping method was used to characterize the differentiation of engrafted human CD34+ detected in G0-transplanted mice (Table 1). Small but detectable numbers of CD34+ cells had low or no expression of the CD38 antigen, suggesting that primitive cells were maintained. In accordance with the study of Pflumio et al,15 the majority of engrafted CD34+ cells (64.6%) coexpressed CD19, whereas only 18.2% were CD33+, showing the predominant differentiation of human MPB CD34+ cells towards the B-lymphoid lineage in the NOD/SCID model.
Phenotype of Chimeric Human Cells Harvested From NOD/SCID Mice Transplanted With G0CD34+Cells
| . | % Engrafted Human Cells With Indicated Phenotype . | ||||||
|---|---|---|---|---|---|---|---|
| % CD45+Cells . | % CD34+ . | ||||||
| CD34+ . | CD19+ . | CD33+ . | CD15+ . | CD38− . | CD19+ . | CD33+ . | |
| Mean ± SEM | 19.9 ± 3.1 | 55.7 ± 5.1 | 34.2 ± 5.1 | 35.0 ± 5.2 | 2.1 ± 0.6 | 64.6 ± 2.3 | 18.2 ± 2.4 |
| Range | 11.7-29.5 | 34.3-75.9 | 17.2-54.6 | 16.7-53.1 | 0.5-4.8 | 54.1-74.0 | 12.1-27.9 |
| . | % Engrafted Human Cells With Indicated Phenotype . | ||||||
|---|---|---|---|---|---|---|---|
| % CD45+Cells . | % CD34+ . | ||||||
| CD34+ . | CD19+ . | CD33+ . | CD15+ . | CD38− . | CD19+ . | CD33+ . | |
| Mean ± SEM | 19.9 ± 3.1 | 55.7 ± 5.1 | 34.2 ± 5.1 | 35.0 ± 5.2 | 2.1 ± 0.6 | 64.6 ± 2.3 | 18.2 ± 2.4 |
| Range | 11.7-29.5 | 34.3-75.9 | 17.2-54.6 | 16.7-53.1 | 0.5-4.8 | 54.1-74.0 | 12.1-27.9 |
The phenotypic profile of BM cells harvested from NOD/SCID mice transplanted 6 weeks previously with G0CD34+cells was determined by FACScan analysis. Cells were stained with antihuman CD45-FITC or antihuman CD34-FITC and PE-conjugated antihuman MoAbs of indicated specificity. Data shown are from three experiments (n = 2 or 3 animals per experiment).
CD34+ cells were reisolated from the BM of highly positive animals and assayed in vitro. Both granulo-monocytic (CFU-GM) and erythroid progenitors (burst-forming unit-erythroid [BFU-E]) were demonstrated in progenitor cell assays at frequencies of 1.36% ± 0.1% and 0.1% ± 0.02%, respectively. Primitive hematopoietic progenitor cells assayed as LTC-ICs were also present, although at a lower frequency than in the original graft (0.1% ± 0.02% v 3.1% ± 0.8%).
Effect of G0-G1 progression in vitro on the repopulating ability of MPB CD34+ cells.
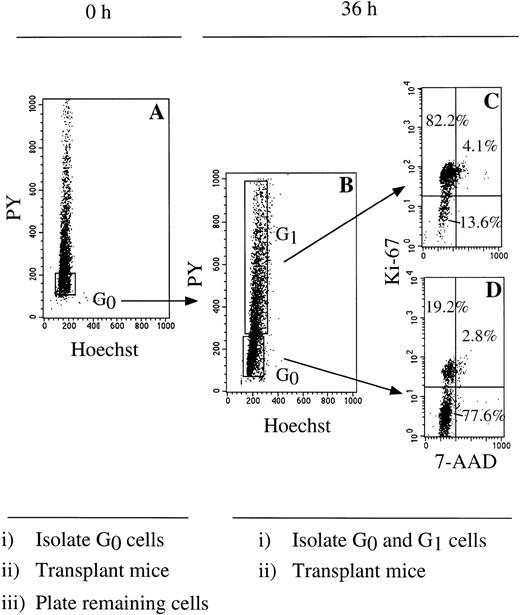
Given the marked difference of repopulating activity between MPB CD34+ cells residing in vivo (ie, in a fresh MPB sample) in G0 or in G1, we were interested in examining whether the same relationship existed for cells progressing from G0 to G1 under in vitro cytokine stimulation. The experimental design is shown in Fig 5. A first Hst/PY fractionation was used to isolate CD34+cells in G0 or in G1 (Fig 5A), and defined cell doses were used for mice transplantation on the original day of cell isolation. The remaining cells isolated in G0 were plated in serum-free conditions and stimulated with a combination of 100 ng/mL FL, 100 ng/mL SCF, and 50 ng/mL IL-3, a cytokine mixture previously shown to promote the expansion of primitive cells detected as LTC-ICs.28 After 36 hours in culture, a second cell cycle fractionation step was used to separate cells remaining in G0 from those traversing into G1 under these conditions (Fig 5B). A short culture period was chosen to minimize cell proliferation such that only the effect of progression to an activated state was investigated and not the result of maturational cell divisions potentially leading to stem cell exhaustion. At this time point, the mean increase in total cells was 1.18- ± 0.17-fold (n = 3). Viability of cultured cells always exceeded 98%, as judged by trypan blue exclusion. To assess the fidelity of the cell cycle fractionation at 36 hours, aliquots of sorted cells were reanalyzed with 7-AAD and Ki-67 (Fig 5C and D). In the representative experiment shown in Fig 5, approximately 75% of PYlow cells were still in G0 as defined by the absence of Ki-67 expression, whereas more than 80% of PYhigh cells were mitotically activated, Ki-67–positive cells. Cells reisolated in these two fractions were used in transplantation experiments at the same dose as those used 36 hours before. All recipient mice were analyzed for the presence of chimeric human CD45+ cells 6 weeks posttransplantation (Table 2).
Cell sorting strategy to isolate CD34+cells during ex vivo G0-G1 progression. (A) MPB CD34+ cells in G0 were isolated in a first Hst/PY sort and either directly injected into recipient animals or plated in ex vivo conditions. (B) After 36 hours, a second Hst/PY sort was used to separate cultured cells transiting to G1 from those remaining in G0. Both cell subsets were then assayed in NOD/SCID mice. Cell-cycle status of cells isolated in G1(C) or G0 (D) after culture was confirmed by restaining samples of sorted cells with 7-AAD and Ki-67. Percentages of cells detected in each quadrant are indicated.
Cell sorting strategy to isolate CD34+cells during ex vivo G0-G1 progression. (A) MPB CD34+ cells in G0 were isolated in a first Hst/PY sort and either directly injected into recipient animals or plated in ex vivo conditions. (B) After 36 hours, a second Hst/PY sort was used to separate cultured cells transiting to G1 from those remaining in G0. Both cell subsets were then assayed in NOD/SCID mice. Cell-cycle status of cells isolated in G1(C) or G0 (D) after culture was confirmed by restaining samples of sorted cells with 7-AAD and Ki-67. Percentages of cells detected in each quadrant are indicated.
Effect of Cell Cycle Progression Under IL-3-SCF-FL Stimulation on the Repopulating Activity of CD34+ Cells Initially Isolated in G0
| Experiment . | Time in Culture . | Cell Cycle Status . | Cell Dose/Mouse (×106) . | % Chimerism (%CD45+)* . |
|---|---|---|---|---|
| 1 | 0 h | G0 | 1.0 | 52.2; 20.8; 68.7 |
| 36 h | G0 | 1.0 | 35.2; 38.1 | |
| G1 | 1.0 | 1.6; 0.2 | ||
| 2 | 0 h | G0 | 0.7 | 12.0; 18.0 |
| 36 h | G0 | 0.7 | 5.2; 9.15 | |
| G1 | 0.7 | <0.1; <0.1 | ||
| Total | 0.7 | <0.1; 0.4 | ||
| 3 | 0 h | G0 | 0.7 | 12.9 |
| 36 h | Total | 0.7 | 1.5; 3.4 |
| Experiment . | Time in Culture . | Cell Cycle Status . | Cell Dose/Mouse (×106) . | % Chimerism (%CD45+)* . |
|---|---|---|---|---|
| 1 | 0 h | G0 | 1.0 | 52.2; 20.8; 68.7 |
| 36 h | G0 | 1.0 | 35.2; 38.1 | |
| G1 | 1.0 | 1.6; 0.2 | ||
| 2 | 0 h | G0 | 0.7 | 12.0; 18.0 |
| 36 h | G0 | 0.7 | 5.2; 9.15 | |
| G1 | 0.7 | <0.1; <0.1 | ||
| Total | 0.7 | <0.1; 0.4 | ||
| 3 | 0 h | G0 | 0.7 | 12.9 |
| 36 h | Total | 0.7 | 1.5; 3.4 |
NOD/SCID mice were transplanted with indicated cell doses of freshly isolated (0 h) G0CD34+ cells or with CD34+ cells initially isolated in G0 and either remaining in G0 or progressing into G1 after 36 hours of ex vivo culture under IL-3-SCF-FL stimulation, as shown in Fig5. In experiments 2 and 3, the total represents CD34+ cells isolated in G0, cultured for 36 hours, and directly assayed for NOD/SCID repopulating capacity without restaining with Hst/PY and cell cycle fractionation.
Percentage of CD45+ cells are indicated for each recipient mouse 6 weeks posttransplantation.
As already shown, freshly isolated CD34+ cells residing in G0 were able to produce a high level of engraftment. As for cells remaining in G0 after 36 hours of cytokine stimulation, the level of repopulating activity was comparable or slightly reduced compared with that observed in noncultured G0 cells (experiments 1 and 2, Table 2). Most strikingly, CD34+ cells initially isolated in G0 and traversing from G0 into G1 during in vitro culture had virtually no repopulating ability.
This differential engraftment potential of cultured cells could be explained by the presence of two different subsets of G0CD34+ cells: a subset enriched in repopulating cells, which responded poorly to mitogenic stimulation in vitro and remained sequestrated in the G0 compartment after 36 hours in culture, and a highly responsive subset, transiting quickly into G1, but initially devoid of repopulating activity. Alternatively, these observations could be the result of a loss of repopulating capacity resulting directly from the progression to an active state in the cell cycle. To distinguish between these two options, we performed two experiments in which fresh G0CD34+ cells were cultured for 36 hours under the same conditions as those described above, then directly transplanted into NOD/SCID recipients without restaining with Hst/PY and separation into quiescent and activated fractions (experiments 2 and 3, Table 2). In both experiments, the engraftment efficiency of unfractionated cultured cells was massively reduced compared with that of fresh G0CD34+ cells indicating that repopulating activity was compromised after ex vivo culture, most likely by progression into G1. Because no adjustment to the number of cells remaining in G0 among total cells used as a graft was made, it is difficult to estimate the magnitude of chimerism lost due to decreased numbers of G0 cells in the graft.
A negative effect of IL-3 on the in vitro maintenance of primitive hematopoietic cells has now been highly suspected,29,30whereas TPO has emerged as a potent stimulator of putative stem cells.28 31 To ensure that our observations on the effect of G0-G1 progression were not dependent on a suboptimal combination of cytokines, we substituted IL-3 with TPO in an additional experiment. MPB CD34+ cells initially isolated in G0 were exposed to the combination of TPO-SCF-FL for 36 hours and then fractionated into G0 and G1subcompartments (Fig 5). The same relationship between cell cycle progression and SRC activity as that determined after IL-3-SCF-FL stimulation was observed such that CD34+ cells traversing into G1 were largely devoid of reconstituting ability compared with cells remaining in G0(Table 3). This finding suggests that in vitro mitotic activation is intrinsically detrimental to the maintenance of SRC activity, independently of the type of cytokines used during ex vivo culture.
Effect of Cell Cycle Progression Under TPO-SCF-FL Stimulation on the Repopulating Activity of CD34+ Cells Initially Isolated in G0
| Time in Culture . | Cell Cycle Status . | % Chimerism (%CD45+)* . |
|---|---|---|
| 0 h | G0 | 12.9 |
| 36 h | G0 | 7.2 |
| G1 | 0.5; 0.9 |
| Time in Culture . | Cell Cycle Status . | % Chimerism (%CD45+)* . |
|---|---|---|
| 0 h | G0 | 12.9 |
| 36 h | G0 | 7.2 |
| G1 | 0.5; 0.9 |
NOD/SCID mice were transplanted with 0.7 × 106freshly isolated (0 h) G0CD34+ cells or CD34+ cells initially isolated in G0 and either remaining in G0 or progressing into G1 after 36 hours of ex vivo culture under TPO-SCF-FL stimulation, as shown in Fig.5.
Percentage of CD45+ cells are indicated for each recipient mouse 6 weeks posttransplantation.
DISCUSSION
The present report describes for the first time a strong relationship between cell cycle status and BM repopulating potential, based on a direct cell cycle fractionation method originally described by our group.16-18 Using simultaneous DNA/RNA staining and various in vitro assays, we previously demonstrated that primitive hematopoietic cells were mainly found in the G0 phase of the cell cycle. We show herein that this relationship also applies to NOD/SCID repopulating cells contained within freshly isolated human MPB CD34+ cells. Although we did not use limiting dilution analysis to determine the frequency of SRC in mitotically quiescent and activated subsets of MPB CD34+ cells,13 we show a significantly large difference in the readout of these two cell populations in the NOD/SCID mouse model. This suggests that SRC are highly enriched in the G0 compartment, that SRC present in the G1 phase have a reduced proliferative capacity in the murine microenvironment, or a combination of both phenomena. This is further evidence of the ability of our cell cycle fractionation method to isolate functionally defined populations of human hematopoietic progenitor/stem cells based on their cycling status. Although the endpoint analysis of engraftment at 6 to 7 weeks posttransplantation is in agreement with other investigators,14 24 the exact nature and position of these cells in the hierarchy of the pool of engrafting hematopoietic progenitor cells remain to be fully elucidated.
Few studies have examined the outcome of ex vivo culture of putative stem cells in the NOD/SCID model. Differences were pointed out in the behavior of SRC compared with that of in vitro assayable human hematopoietic cells, ie, CFC and LTC-IC. Gan et al32 showed that incubation of hematopoietic cells on stromal cells maintained or even expanded CFC and LTC-IC, whereas SRC declined over the same period of time. In gene marking experiments, after prestimulation over the C-terminal fragment of fibronectin,33 high levels of transduction were observed in CFC and LTC-IC, but no transduced cells were detected in the BM of recipient mice. Finally, using CB CD34+CD38− cells, Bhatia et al34 were able to demonstrate a twofold increase of SRC in short-term culture, although in a similar study, Conneally et al24 showed that ex vivo expanded SRC had a reduced proliferative capacity compared with that of freshly isolated SRC. It appears therefore that expansion of SRC is at best limited and achieved at the expense of a decrease in the generative capacity of individual repopulating cells.
The ability of the DNA/RNA staining method to sort cells in precise phases of the cell cycle was used in the present study to determine the effect of in vitro cell cycle activation on the repopulating ability of putative stem cells, in the absence of cell division. A short cytokine stimulation period of 36 hours was used to induce a fraction of CD34+ cells initially isolated in G0 to progress into G1 without executing a complete cell cycle, while allowing almost an equal number of cells to remain in G0. Thus, the only variable tested in these experiments was the movement along the G0/G1 phase of the cell cycle and not the effect of cellular divisions. This was confirmed by the absence of an increase in cell numbers during ex vivo culture. Our data show that engagement in G1 after cytokine stimulation is associated with a decrease in repopulating capacity. Two mutually nonexclusive mechanisms may underlie these observations. It is possible that SRC are sequestrated in the G0 compartment during culture, whereas more differentiated cells quickly traverse into G1. This is most likely, because we previously demonstrated that CD34+ cells isolated in G0 by the Hst/PY method were still heterogeneous in their ability to respond to cytokine stimulation,16 18 with the most quiescent cells being the most primitive. Another possible explanation is that ex vivo G0-G1 transition may directly affect the capacity of pre-existing SRC to repopulate the BM of the recipient animal. The decline in repopulating capacity of unfractionated stimulated cells demonstrates that G1 progression, under culture conditions used in this study, does indeed reduce SRC activity.
This study provides evidence that ex vivo culture can modify primitive hematopoietic functions of putative stem cells before any cellular division actually occurs. This is compatible with at least two hypotheses. First, commitment and/or differentiation may take place during the G0-G1 transition. Second, homing of primitive progenitor cells to the BM microenvironment is possibly impaired after cell cycle activation. The latter hypothesis is also suggested by studies that have now established a direct relationship between cytokine stimulation and affinity and/or expression of integrins at the surface of human hematopoietic progenitors35-38 or between cell cycle status, expression of adhesion molecules, and engraftment of murine progenitor cells.39 Because the BM microenvironment is thought to comprise multiple loci supporting hematopoietic progenitors at different levels of differentiation,40 ex vivo modulation of adhesive properties by cycle activation may impair the ability for stimulated primitive cells to home to adequate sites and express their full generative and differentiative capacity. Further studies will be needed to elucidate cell cycle-related changes in adhesion molecules affinity and/or expression, potentially leading to impaired engraftment.
ACKNOWLEDGMENT
The authors thank Dr David A. Williams (Herman B Wells Center for Pediatric Research, Indiana University School of Medicine) for the use of the NOD/SCID mice facility, Susan Rice and Jon McMahel for technical assistance in flow cytometric cell sorting, and Ryan Cooper for help in immunomagnetic CD34+ cell selection. We are also grateful to Amgen and Immunex for generous gifts of recombinant human cytokines.
Supported by National Institutes of Health Grant No. R01 HL55716 and a research award from the Phi Beta Psi Sorority to E.F.S. Herman B Wells Center for Pediatric Research is a Center of Excellence in Molecular Hematology (NIDDK P50 DK 49218). A.G. is supported by a fellowship from the Fonds National de la Recherche Scientifique (FNRS, Brussels, Belgium) and by a travel grant from the Centre Anticancéreux près l’ULg (University of Liège, Liège, Belgium).
Address reprint requests to Edward F. Srour, PhD, Indiana University School of Medicine, 1044 W Walnut St, R4-202, Indianapolis, IN 46202.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal