Abstract
In this study we sought to extend the plasma half-life while maintaining the potent antithrombin activity of hirudin. We hypothesized that gene fusion of hirudin to albumin would result in the expression of a slowly cleared hirudin molecule. A hirudin variant 3 (HV3) cDNA was obtained by gene synthesis, while a 1,996-bp full-length rabbit serum albumin (RSA) cDNA was selected from a rabbit liver cDNA library. Expression of the former in COS-1 cells conferred antithrombin activity on media conditioned by the cells, while expression of the latter resulted in the secretion of a 67-kD protein that reacted with mono-specific anti-RSA antibodies. Having shown independent expression of the two proteins, we next expressed two fusion proteins: HV3 linked via its C-terminus to albumin (HLA), and HV3 linked via its N-terminus to albumin (ALH). The former, but not the latter, inhibited both the amidolytic and fibrinogenolytic activities of thrombin. HLA also retained the dye-binding characteristics of RSA, as judged by Affi-Gel Blue chromatography. Highly similar concentrations of either commercial HV1 (40 nmol/L) or HLA (30 nmol/L) were required to halve the initial rate of thrombin reaction with chromogenic substrate S2238, suggesting the retention of high-affinity inhibition of thrombin by the fusion protein. An His-tagged form of HLA was purified by Ni2+-chelate affinity and heparin-Sepharose chromatography. The purified, radioiodinated protein was injected into rabbits, and demonstrated a catabolic half-life of 4.60 ± 0.16 days. This represents an extension of hirudin half-life in vivo of greater than two orders of magnitude; gel analysis of HLA(H)6 recovered from rabbits showed that it circulated in intact form. Our results provide a rationale for future testing of the biological effects of HLA, and support our initial hypothesis.
HEMATOPHAGOUS organisms rely for sustenance on the blood of their prey. They must, of necessity, use strategies that counteract, or limit coagulation, frequently via the secretion of proteinaceous clotting inhibitors. These polypeptides have attracted considerable scientific attention in that they may provide both novel tools for the study of coagulation and new anticlotting agents of potential therapeutic utility. Examples from this potential pharmacopoeia include leech proteins that inhibit thrombin or factor Xa (hirudin1 and antistasin2 ), the factor Xa inhibitor tick anticoagulant peptide (TAP3), the vampire bat factor IXa and Xa inhibitor draculin,4 and the snake antiplatelet factor barbourin.5 Of these, hirudin has arguably been the most extensively studied.
The hirudins are a family of closely related proteins secreted from the salivary gland of the medicinal leech, comprised of 65 or 66 amino acids.6 They are among the most potent known inhibitors of thrombin, with Ki values in the sub-picomolar range.7 X-ray crystallographic studies of hirudin-thrombin complexes have confirmed that hirudin contains a globular N-terminal domain, and an extended, negatively charged C-terminal domain.8 The interaction of the latter with the fibrinogen-binding exosite of thrombin and of portions of the former with the catalytic site contribute to the many close contacts between hirudin and thrombin.8 The availability of large quantities of recombinant hirudin produced in yeast9 has renewed interest in this potent and specific10 thrombin inhibitor.
Hirudin is rapidly cleared from the mammalian circulation, exhibiting a catabolic half-life of 1 hour or less in all laboratory animals tested.11 Indeed, hirudin is excreted intact and in active form from dogs, largely through renal clearance.12 The resulting short duration of action of hirudin necessitates the use of doses higher than would otherwise be necessary, and may thus contribute to the recent finding that the clinical window of safety for hirudin may be relatively narrow.13 This property has prompted previous efforts to extend the half-life of hirudin in vivo, including the chemical coupling of dextran14 or polyethylene glycol15 to the inhibitor. The rationale behind such strategies is that increasing the time that hirudin remains in the circulation should allow the use of lower doses and/or less frequent administration of the agent; current administration protocols for recombinant hirudin include continuous infusions.16
Given the well-known carrier protein properties of serum albumin,17 we hypothesized that it might be possible to retard the clearance of a rapidly cleared anticoagulant protein (hirudin) via fusion to this slowly cleared plasma protein. Accordingly, in this study, we obtained cDNAs for hirudin by gene synthesis, and cloned rabbit serum albumin (RSA) because we wished to test the resulting protein in as homologous an in vivo setting as possible. We show that in-frame fusion of hirudin and albumin cDNAs leads to the production of a hirudin-albumin fusion protein that retains the potent antithrombin activity of unfused hirudin and acquires the extremely slow clearance from the circulation characteristic of unfused albumin.
MATERIALS AND METHODS
Materials
A plasmid encoding human serum albumin, designated p(Alb)3, was generously provided by Dr James Wilson (University of Michigan Medical Center, Ann Arbor). Recombinant desulfato-hirudin HV1 (CGP 39393), hereafter referred to as commercial HV1, was kindly provided by Dr R.B. Wallis (Ciba-Geigy Pharmaceuticals, Horsham, UK). Human α-thrombin (>3,300 NIH U/mg; >93% active) was the generous gift of Dr John Fenton (New York State Division of Biologicals, Albany). Oligonucleotides were synthesized at the Institute for Molecular Biology and Biotechnology, McMaster University (Hamilton, Ontario, Canada). All enzymes for the modification of DNA were purchased from Promega (Madison, WI), with the exception of Pfu polymerase (Stratagene, La Jolla, CA) and Taq polymerase (Perkin-Elmer, Mississauga, Ontario, Canada). T7 sequencing kits, Sephaglas DNA purification kits, and deoxyribonucleotides were from Pharmacia LKB Biotechnology (Baie d'Urfe, Quebec, Canada). Canadian Life Technologies (Burlington, Ontario, Canada) was the supplier of competent Escherichia coli DH5α cells, Lipofectin reagent, penicillin/streptomycin, and dye-free Dulbecco's minimal essential medium (DMEM) for cell culture. COS-1 cells were obtained from the American type Culture Collection (Rockville, MD). The radioactive products (35S)-methionine and (35S)-cysteine (Tran35Slabel) were bought from ICN (Mississauga, Ontario, Canada), as were methionine and cysteine-deficient DMEM; 35S-dATP and Na125I were from Mandel (Toronto, Ontario, Canada). Affi-Gel Blue (50-100 mesh), and nitrocellulose blotting membranes were purchased from BioRad (Mississauga, Ontario, Canada). Rabbit serum albumin and bovine serum albumin (RSA and BSA) were from Sigma (St Louis, MO). Alkaline phosphatase-conjugated rabbit-antichicken IgG was from Jackson Labs (Bar Harbor, ME). A commercial rabbit liver cDNA library (5′-STRETCH; Clontech, Palo Alto, CA) was also purchased. Qiagen (Chatsworth, CA) was the source of plasmid DNA isolation kits and Ni2+-chelate affinity resin. Chromogenic substrate S2238 (H-D-Phenylalanyl-L-pipecolyl-L-arginine-p-nitroaniline dihydrochloride) for quantitation of thrombin activity was purchased from Helena Laboratories (Guelph, Ontario, Canada). Immulon 2 microtiter plates were from Amicon (Beverly, MA). All other chemicals and reagents not specifically listed above were of the highest quality available.
Methods
Gene synthesis of HV3.Four mutually priming oligonucleotides were used to synthesize a hirudin variant 3 (HV3) cDNA [modified from ref 18]: primers A (5′-GGCCTCTGGG GCCGTGTGGC TTGTATCACC TACACAGACT GCACAGAGTC TGGCCAGAAC CTGTGC-3′) and C (5′-GTATACTGGG CTCCCAGGGC AAGGACAACC AGTGTGTGAC AGGAGAGGGA ACTCCTAAGC CTCAGAGCCA CA-3′) on the sense strand, and primers B (5′-GTATACACTT GTTGCCCTTG CCACACACAT TGGAGCCCTC ACACAGGCAC AGGTTCTGGC C-3′) and D (5′-GGATCCTACT CATCATAGGC ATCCTCAGGG ATAGGCTCAA AGTCTCCCTG GTTGTGGCTC TGAGGCT-3′) on the antisense. Primers A and B, and C and D, were combined in separate polymerase chain reactions (PCRs) at a final concentration of 1.0 μmol/L, and amplified using Taq polymerase for 30 cycles under otherwise standard conditions.19 The resulting PCR products, AB (112 bp) and CD (124 bp) were gel-purified, made blunt-ended using the Klenow fragment of DNA polymerase I, and introduced into the EcoRV site of pGEM5zf(+) (Promega) using standard manipulations.20 DNA sequencing showed that all resulting subclones contained some errors, but these misincorporations were fully corrected by additional PCR reactions (eg, a near-perfect match CD subclone was used as the template in a standard PCR reaction primed by an SP6 primer and primer D). Misincorporations at both 5′ and 3′ ends of AB were corrected by similar PCR manipulations involving primers encoding the first 27 bp of primers A and B. A 150-bp Acc I digestion product of the resulting AB clone [in pGEM5zf(+)] was inserted into the Acc I–linearized CD clone [in pGEM7zf(+)]. This final HV3 plasmid was found to be without misincorporations by DNA sequencing, and designated plasmid pABCD. This final construct contained nucleotides 124-138 of a rabbit antithrombin cDNA21 (encoding a portion of the signal sequence) joined in frame to the 66 codons of HV3 and a termination codon.
Molecular cloning of rabbit serum albumin.A λgt-11 rabbit liver cDNA library was screened by hybridization as previously described21,22 using a 2,200-bp BamHI fragment of p(Alb)323 containing the entire human albumin cDNA to generate random-primer 32P-labeled probes. The phage clone giving the most intense hybridization signal on a preliminary screen of 2 × 105 plaques was transferred to the EcoRI site of pGEM3zf(+) p(alb)72. The 1,600-bp cDNA insert of p(alb)72 was used to rescreen the library, and yielded a clone with a 1,996-bp insert that was transferred to the EcoRI site of pUC19 and the resulting plasmid designated p(alb)192. This full-length RSA cDNA was sequenced on both strands using the dideoxy method, a process facilitated by the use of p(alb)192 derivatives with nested deletions.24 The sequence of the RSA cDNA was deposited in Genbank (accession number U18344).
Construction of expression plasmids.Five expression plasmids were constructed, as described below. (1) A 216-bp Sfi I-EcoRI restriction fragment of pABCD (see above) and a 132-bp fragment of pGEM7zf(+)-rAT-III−32-433 were gel-purified and inserted into the EcoRI site of the eukaryotic expression vector pSG5,25 in a three-part ligation. The resulting plasmid, pSG5-HV3, encoded the 32–amino acid secretory signal sequence of rabbit antithrombin, fused to the 66 codon HV3 cDNA assembled by gene synthesis. (2) For expression of recombinant RSA, the 1,996-bp cDNA was released from p(alb)192 by EcoRI digestion and inserted into the corresponding site of pSG5. Analysis of candidate subclone miniprep DNA was used to identify a plasmid containing the RSA cDNA in the sense (pSG5-RSA) and antisense (pSG5-ASR) orientations with respect to the SV40 promoter of pSG5. (3) To fuse the mature form of RSA to HV3, pSG5-HV3 was used as a template in a standard PCR reaction primed by employing a pSG5-specific primer that bound upstream of the insert (primer 3952, 5′-GTAATACGAC TCACTATAGG-3′) and primer 4115 (5′-AACCATGGAG CCACCTCCGC CACCTCCCTC ATGATAGGCA TCCTCAG-3′). The latter replaces the termination codon of pSG5-HV3 with (Gly)6 -Ser-Met. The RSA cDNA was similarly modified, in a reaction primed by the SP6 primer and primer 3951 (5′-CTCCATGGAA GCACATAAAA GTGAGAT-3′). The latter replaces the secretory signal sequence of RSA with an Nco I restriction site. EcoRI-Nco I–digested HV3 PCR product and the Nco I-EcoRI–digested RSA PCR product were ligated into EcoRI-digested pSG5, in a three-part ligation reaction, that yielded pSG5-HLA (for hirudin linked to albumin). (4) A similar procedure was used to fuse mature HV3 to the C-terminus of RSA, with the exception that the EcoRI and BamHI sites of pSG5 were employed, the manipulations resulted in a Met-Val-(Gly)6 spacer separating Ala581 of RSA and Ile1 of HV23, and the resulting plasmid was designated pSG5-ALH (for albumin linked to hirudin). (5) Expression plasmid pSG5-HLA was modified by PCR, using a similar protocol to those described above, using primers 3952 and primer 6932 (5′-CCCGGGATCC TTAATGGTGA TGGTGATGGT GGCCTAAGGT AGCTTTACTT GATTCAACAA G-3′). The resulting PCR product was restricted with EcoRI and BamHI and inserted between these sites in pSG5 to yield pSG5-HLA(H)6 , in which six His codons had been introduced between Gly 584 and the termination codon. All PCR reactions used to produce the fusion proteins employed high-fidelity Pfu polymerase to eliminate misincorporations, and the hirudin moieties, fusion, and insertion points were verified by DNA sequencing.
Antibodies and enzyme-linked immunosorbent assays (ELISAs).RSA was injected subcutaneously into a laying hen and IgG partially purified from yolks obtained from the eggs as described previously.26 Affinity-purified, monospecific antibodies were obtained following negative selection on immobilized BSA, and positive selection on immobilized RSA, and used to develop an ELISA for recombinant products containing RSA. Briefly, affinity-purified chicken anti-RSA antibodies were used as the trapping antibody, and a biotinylated preparation of the same antibody was used to detect bound antigen, in conjunction with streptavidin conjugated to alkaline phosphatase. This ELISA could detect RSA at a concentration of 10 ng/mL, but showed no reactivity to 1 μg/mL BSA. For recombinant HV3, commercial HV1 was used to immunize laying hens, and the resulting IgG partially purified. For ELISAs, HV3-containing samples were bound to microtiter plate wells, and detected using this antibody and affinity-purified rabbit-antichicken IgG conjugated to alkaline phosphatase.
Measurement of thrombin activity.The amidolytic activity of thrombin was assayed using chromogenic substrate S2238. Conditioned media containing known concentrations of COS-derived material or commercial HV1 was incubated in the assay buffer (66.7 mmol/L Tris-Cl, pH 8.0, containing 133 mmol/L NaCl and 0.27% [wt/vol] polyethylene glycol, Mr 8,000), and 50 μmol/L of S2238 at 37°C for 2 minutes. Thrombin (diluted in ice-cold assay buffer) was added, and the reaction was allowed to proceed for 5 minutes at 37°C. Amidolysis of S2238 was stopped with the addition of 20% acetic acid, and the absorbance at 405 nm determined on a spectrophotometer. The ability of fused or unfused hirudin to influence the reaction of thrombin with fibrinogen was assayed using a variation of the thrombin clotting time (TCT) assay. In this assay, factor II–depleted human plasma was diluted threefold into imidazole buffer containing 0.5 nmol/L hirudin-related inhibitor; the reaction was initiated by the addition of human α-thrombin to 2.14 nmol/L final concentration. Time to clot formation was measured on an automated fibrometer.
Binding assays.The binding of 125I-α-thrombin to either HV1 or HLA immobilized on wells of microtiter plates was investigated. Conditioned media containing HLA or HV1 was diluted in 0.01 mol/L phosphate buffer (pH 8.5) and coated onto the wells for a minimum of 8 hours at 4°C. Wells were rinsed with Tris-buffered saline, pH 7.4, containing 0.01% Tween-20 (TBST), incubated with 5% skim milk powder in TBST for 1 hour, and washed once in TBST before addition of ligand (125I-labeled thrombin, specific activity 1.6 × 104 dpm/ng). The time to reach the steady state and the range of concentration of hirudin-related protein in which the specific ligand binding was linear were determined in preliminary experiments using 1.9 nmol/L 125I-thrombin. A 100-fold molar excess of unlabeled thrombin was used to determine residual, nonspecific binding in all assays. Time of binding was fixed at 70 minutes or 40 minutes for HV1 and HLA, respectively. At the end of the binding incubations, wells were rinsed with TBST, the wash was aspirated, the wells were separated and the total bound radioactivity was determined directly in a gamma counter. HLA or HV1 in solution were used to compete for binding of 125I-thrombin to HV1 or HLA, respectively, bound to the wells of microtiter plates. The specific binding of 0.4 nmol/L 125I-thrombin in 70 minutes to 0.29 pmol of HV1 in the presence of 0 to 10 nmol/L HLA or HV1 was determined, and IC50 values were established from the inhibition plots by regression.
Kinetic experiments.The kinetics of the reaction of thrombin with its chromogenic substrate S2238 was followed essentially as described27 using a Cary 3E UV-visible spectrophotometer and allied software (Varion Canada, Inc, Mississauga, Ontario). The change in absorbance at 405 nm was followed for at least 10 minutes, and initial rates of reaction were obtained from the resulting progress curves. Final inhibitor concentrations were from 2 × 10−8 mol/L to 1.2 × 10−7 mol/L, with a substrate concentration of 50 μmol/L, and a thrombin concentration of 4.5 × 10−11 mol/L.
Purification of HLA(H)6 . Conditioned media from 30 100-mm plates lipofected with pSG5-HLA(H)6 under transfection conditions previously described28 were pooled and passed over a 2.5-mL Ni2+-chelate (Ni-NTA-agarose; Qiagen) affinity column. The column was washed with 20 column volumes of TBS, and eluted with a linear gradient of 0 to 2.0 mol/L imidazole pH 6.5. Fractions containing HLA(H)6 were identified by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), pooled, and dialyzed against 4.0 L of TBS, and batch-adsorbed to a 2.0-mL vol of Affi-Gel Blue. The resin was washed 5× with TBS and eluted with 2 mol/L NaCl. After dialysis against TBS, the preparation (14 mL) was batch-adsorbed to 2.0 mL of heparin-Sepharose, and the unbound fraction concentrated by ultrafiltration and dialyzed against phosphate-buffered saline. This final preparation contained 12 μg of HLA(H)6 (as judged by BioRad protein assays standardized with BSA) and was free of contaminating protein as judged by SDS-PAGE.
In vivo experiments.Male New Zealand White rabbits (2.8 to 3.2 kg) were injected with 2 × 107 dpm/kg each of 125I-labeled HLA(H)6 purified as described above. At various times after injection, blood samples were drawn from the marginal vein of the other ear into 1/10 volume of acid-citrate-dextrose (ACD) anticoagulant. Plasma samples (0.3 mL) were precipitated by addition of an equal volume of 20% trichloroacetic acid (TCA) and the radioactivity in the resulting pellets was quantified using a gamma counter.
Pharmacokinetic analysis.The clearance data were analyzed using the technique of curve peeling, as described,29 using Lotus 1,2,3 software (Lotus Development Corp, Cambridge, MA). Briefly, the logarithm of the residual radioactivity was plotted against the time after injection in decimal days. The terminal exponential phase of the clearance was curve-fit using linear regression. Subtraction of the equation describing this line from the remaining data yielded a biphasic curve. The curve-peeling process was repeated; after the second curve-peeling, a single linear component remained on the semi-log plot, indicating the need for three terms in the equation, indicative of a three-compartment model.29 Fusion protein clearance, then, is described by the following equation:
where Cn are coefficients, and a(n ) are rate constants. Fractional catabolic rates, half-lives, and distributions were calculated from Cn and a(n) values derived from the curve peeling as described by Carlson et al.30 31
General.Previous publications from this laboratory have described routine protocols for SDS-PAGE, fluorography, and autoradiography; concentration of conditioned cell media; transient transfection and metabolic labeling of COS cells; iodination of α-thrombin; and double-stranded DNA sequencing. Sequence management and alignments were performed using GENEPRO (Riverside Scientific, Seattle, WA) software. All protein samples analyzed by SDS-PAGE in this study were reduced with 2-mercaptoethanol before electrophoresis.
RESULTS
Gene Synthesis of HV3 and Expression in COS Cells
To test the concept that clearance of anticoagulant proteins could be modulated via gene fusion to albumin, it was first necessary to obtain independent recombinant expression of each moiety of the future fusion protein. Because any hirudin-albumin fusion protein would be expected to contain 20 disulphide bonds (and an unpaired Cys residue), we chose to express the proteins in COS cells, taking advantage of the optimal folding and disulphide bond formation afforded by passage through the mammalian cell secretory pathway. Accordingly, the hirudin cDNA was obtained via gene synthesis, with codon choices being made on the basis of frequency of use in rabbit antithrombin, a protein successfully expressed in COS cells in our laboratory previously,28 and whose cleavable signal sequence was attached to the hirudin codons to direct secretion from COS cells. Hirudin variant 3 (HV3) was selected for use, as it seemed reasonable to employ the most active known hirudin variant,32 given that some diminution of activity could arise when hirudin became part of a larger polypeptide.
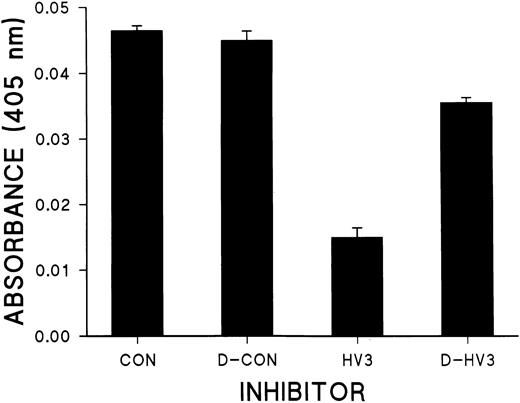
Use of mutually priming, 60- to 70-nucleotide long primers resulted in the gene synthesis of HV3 in two parts. As has been previously noted, the method is relatively error-prone; nevertheless, because in our hands the few misincorporations that were noted clustered at the termini of the products, they were easily repaired in an additional round of PCR. Transfection of COS cells with the resulting expression plasmid, pSG5-HV3, resulted in the appearance in the conditioned media of thrombin inhibitory activity. Addition of this conditioned media, but not that of mock-transfected cells, reduced amidolysis of the chromogenic substrate by thrombin (Fig 1). The bulk of this inhibitory activity was lost after dialysis through 12- to 14-kD molecular weight cut-off (MWCO) membranes (Fig 1), but was retained following dialysis against 6- to 8-kD MWCO dialysis tubing (not shown). In addition, clotting times determined in the presence of HV3 were prolonged from 43 ± 1 seconds to 52 ± 1 seconds (see Fig 4B). These results are consistent with the successful production of recombinant HV3 in COS cells and its secretion from the cells in a form capable of inhibiting both thrombin-mediated amidolysis and fibrinogenolysis.
Thrombin amidolytic activity assays. The amidolytic activity of thrombin in the presence of equal amounts of conditioned media from mock-transfected Cos cells (CON) or those transfected with pSG5-HV3 (HV3) was determined as described in Materials and Methods using chromogenic substrate S2238 (n = 3, ±mean), with a thrombin concentration of 0.1 nmol/L. D-CON and D-HV3 are the same as CON and HV3, except that the conditioned media were dialyzed before use overnight at 4° using dialysis tubing with MWCO of 12 to 14 kD.
Thrombin amidolytic activity assays. The amidolytic activity of thrombin in the presence of equal amounts of conditioned media from mock-transfected Cos cells (CON) or those transfected with pSG5-HV3 (HV3) was determined as described in Materials and Methods using chromogenic substrate S2238 (n = 3, ±mean), with a thrombin concentration of 0.1 nmol/L. D-CON and D-HV3 are the same as CON and HV3, except that the conditioned media were dialyzed before use overnight at 4° using dialysis tubing with MWCO of 12 to 14 kD.
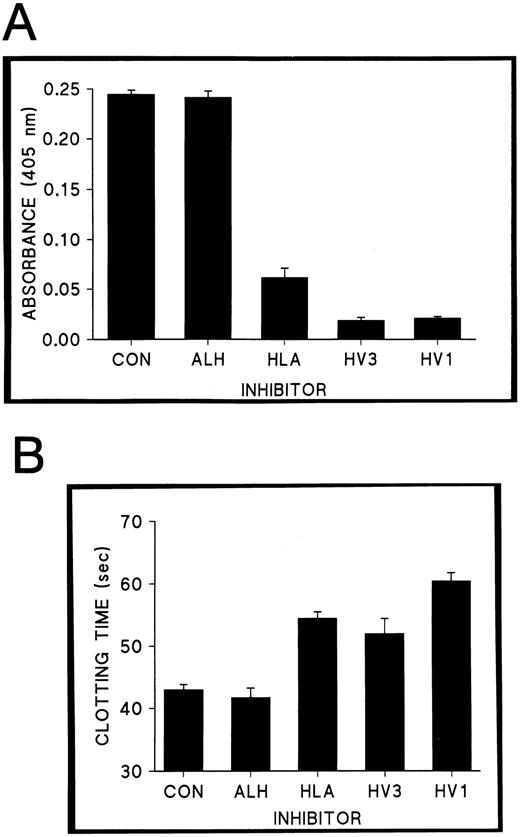
Thrombin inhibitory activity of fused and unfused hirudins. (A) Results of amidolytic assays of thrombin activity to which conditioned media containing 1.0 nmol/L Cos-derived recombinant protein (ALH, HLA, or HV3) was added. Conditioned media from nontransfected cells served as a negative control for inhibition (CON), while commercial HV1 was diluted in this media to 1.0 nmol/L (HV1). (B) Thrombin clotting times in the presence of 0.5 nmol/L Cos-derived recombinant protein, equivalent amounts of control conditioned media (CON), or of control conditioned media combined with HV1 (HV1). Error bars correspond to the standard deviation (n = 4) in both panels.
Thrombin inhibitory activity of fused and unfused hirudins. (A) Results of amidolytic assays of thrombin activity to which conditioned media containing 1.0 nmol/L Cos-derived recombinant protein (ALH, HLA, or HV3) was added. Conditioned media from nontransfected cells served as a negative control for inhibition (CON), while commercial HV1 was diluted in this media to 1.0 nmol/L (HV1). (B) Thrombin clotting times in the presence of 0.5 nmol/L Cos-derived recombinant protein, equivalent amounts of control conditioned media (CON), or of control conditioned media combined with HV1 (HV1). Error bars correspond to the standard deviation (n = 4) in both panels.
Molecular Cloning and Expression of Rabbit Serum Albumin
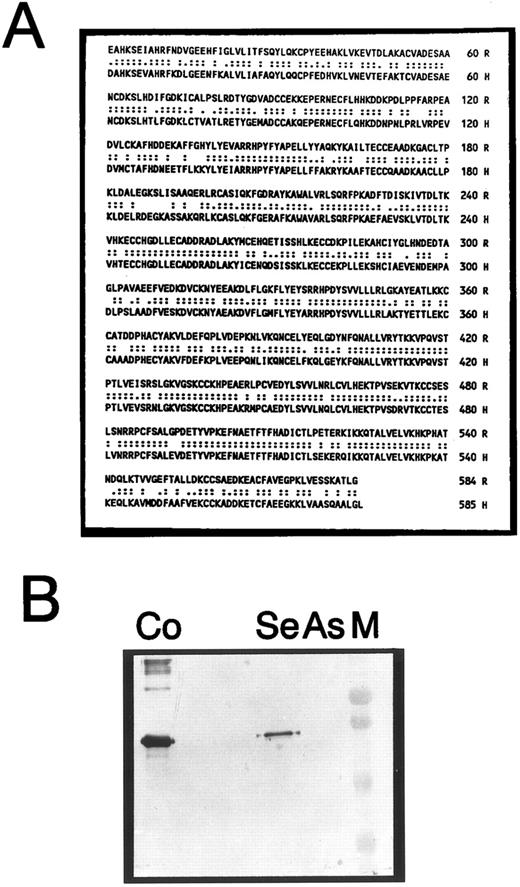
Because we planned to investigate the clearance, and eventually the anticoagulant and antithrombotic properties of the hirudin-albumin fusion proteins in rabbit experimental models, we elected to use RSA as the albumin moiety. Because no RSA cDNA had been described, RSA was cloned by screening a rabbit liver cDNA library in λgt-11, using hybridization to a human serum albumin (HSA) cDNA. The longest clone that was obtained is 1,996 nucleotides long, and is comprised of a 1,824-bp open reading frame, preceded by 51 nucleotides of 5′ untranslated region, and followed by 111 bp of 3′ untranslated sequence that terminates in a polyadenylation signal (TATAAA). Based on the complete identity of the first 24 codons to the HSA pre-pro sequence, the next residue was designated Glu 1. As shown in Fig 2A, the mature HSA33 and RSA proteins share 73% amino acid identity. Like other animal albumins,34 RSA is one residue smaller than its human counterpart, and comprises 584 amino acids to give a predicted molecular weight of 66,019. All of its 35 cysteine residues are conserved, as is its single tryptophan.
Characterization of the RSA cDNA. The protein sequence corresponding to the mature, circulating RSA, deduced from the DNA sequence of p(alb)192, is shown in (A), aligned to its human counterpart. R, RSA; H, HSA. Double dots indicate identical, and single dots, similar residues; amino acid numbering is shown at the right. (B) An immunoblot stained with mono-specific anti-RSA antibodies. Lane Se, conditioned media from Cos cells transfected with pSG5-RSA (sense orientation); lane As, equivalent amount of conditioned media from cells transfected with pSG5-ASR (antisense orientation). M, prestained low-molecular-weight range markers (BioRad); Co, positive control (250 ng purified plasma-derived RSA).
Characterization of the RSA cDNA. The protein sequence corresponding to the mature, circulating RSA, deduced from the DNA sequence of p(alb)192, is shown in (A), aligned to its human counterpart. R, RSA; H, HSA. Double dots indicate identical, and single dots, similar residues; amino acid numbering is shown at the right. (B) An immunoblot stained with mono-specific anti-RSA antibodies. Lane Se, conditioned media from Cos cells transfected with pSG5-RSA (sense orientation); lane As, equivalent amount of conditioned media from cells transfected with pSG5-ASR (antisense orientation). M, prestained low-molecular-weight range markers (BioRad); Co, positive control (250 ng purified plasma-derived RSA).
Insertion of the RSA cDNA into the pSG5 eukaryotic cell expression vector in the sense orientation, followed by transfection of COS cells, resulted in the appearance in the conditioned media of a 67-kD polypeptide that was detected on immunoblots using a monospecific, affinity-purified chicken anti-RSA IgG (Fig 2B, lane Se). This protein comigrated with plasma-derived RSA, and was absent from media conditioned by cells transfected with pSG5 containing RSA in the antisense orientation (Fig 2B, lane As). These results confirm the successful cloning and expression of RSA in COS cells.
Production of Fusion Proteins ALH and HLA
As the generation of hirudin fusion proteins had not been previously reported, it was not known a priori whether N-terminal or C-terminal fusion would be more desirable. Accordingly, two fusion proteins were generated: HLA (HV3 linked to albumin), in which RSA was attached to the C-terminus of hirudin; and ALH (albumin linked to HV3), in which RSA was attached to the N-terminus of hirudin. In both cases, a hexaglycine spacer was incorporated into the design of the fusion protein to promote independence of folding of the two parental proteins; in the case of HLA, Gly6 -Met-Ser separate Glu 66 of HV3 and Glu 1 of RSA (Fig 3A, L1), while in the case of ALH, Met-Val-Gly6 separate Ala 581 of RSA and Ile 1 of HV3 (Fig 3A, L2). As shown in Fig 3B, transfection of COS cells with expression plasmids encoding these chimeric proteins resulted in the appearance of anti-RSA immunoreactive products with decreased mobility compared with recombinant COS-derived RSA; the mobility of ALH was slightly greater than that of the 74-kD HLA. In repeated transfection experiments, the concentration of ALH secreted into the medium never exceeded 20% of the levels achieved with HLA; moreover, whereas HLA inhibited both the amidolytic and fibrinogenolytic activity of thrombin to an extent similar to that obtained with unfused hirudins (Fig 4), ALH was without detectable effects. Importantly, neither activity of HLA was diminished by dialysis of HLA-containing conditioned media (using 12-kD MWCO), a finding that supports the integrity of the fusion protein in the conditioned media (Fig 3B). Accordingly, ALH was not further investigated, whereas characterization of HLA continued.
Expression of HV3, RSA, and fusion proteins. (A) Schematic, linear representations of the recombinant proteins produced in this study. Hatched areas represent HV3 segment, while solid areas correspond to RSA segments. L1, linker 1 [(G)6SM]; L2, linker 2 [MV(G)6 ]. Size of proteins, in amino acids (aa), is given at right. (B) An anti-RSA immunoblot showing immunoreactive components of conditioned media from Cos cells transfected with the following plasmids: pSG5-RSA (RSA), pSG5-HLA (HLA), pSG5-ASR (ASR), pSG5-ALH (ALH), and pSG5 lacking any insert (CON). Horizontal marks, at left, indicate the positions of the 94-, 67-, 43-, and 30-kD molecular-weight markers.
Expression of HV3, RSA, and fusion proteins. (A) Schematic, linear representations of the recombinant proteins produced in this study. Hatched areas represent HV3 segment, while solid areas correspond to RSA segments. L1, linker 1 [(G)6SM]; L2, linker 2 [MV(G)6 ]. Size of proteins, in amino acids (aa), is given at right. (B) An anti-RSA immunoblot showing immunoreactive components of conditioned media from Cos cells transfected with the following plasmids: pSG5-RSA (RSA), pSG5-HLA (HLA), pSG5-ASR (ASR), pSG5-ALH (ALH), and pSG5 lacking any insert (CON). Horizontal marks, at left, indicate the positions of the 94-, 67-, 43-, and 30-kD molecular-weight markers.
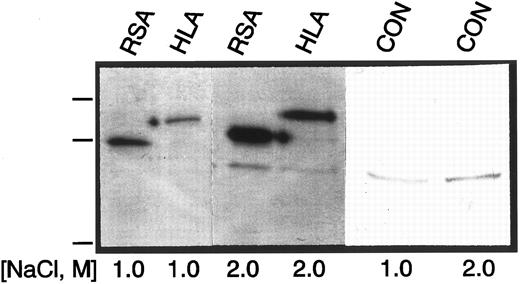
Retention of Parent Protein Characteristics by HLA
Having shown the retention of thrombin inhibitory characteristics similar to that of unfused hirudin by HLA, we wished to characterize the albumin moiety of the fusion protein in a similar way. Because albumin lacks known enzymatic or enzyme inhibitory activities, we chose to assess the binding of HLA to immobilized Cibacron blue dye (Affi-Gel Blue; BioRad), a well-known property of the serum albumins.35 The 35S-labeled products of metabolic labeling of COS cells transfected with pSG5, pSG5-RSA, and pSG5-HLA were passed over Affi-Gel Blue mini-columns, washed with TBS, and eluted with either 1.0 or 2.0 mol/L NaCl. Equivalent amounts of each eluate were TCA-precipitated, and detected by SDS-PAGE and autoradiography. As shown in Fig 5, highly similar elution patterns for both proteins were observed; moreover, no ELISA-detectable material was found in either the flow-through or the wash in either case. These results are consistent with the retention of at least some albumin-like properties in the fusion protein HLA.
Gel analysis of eluates from Affi-Gel Blue columns. Equivalent amounts of media transfected with pSG5-RSA (RSA), pSG5-HLA (HLA), or pSG5 (CON), and metabolically labeled with 35S-Met and -Cys were chromatographed on separate Affi-Gel Blue minicolumns. Bound material was eluted with the salt concentrations shown below the lanes, and resolved by SDS-PAGE followed by fluorography and autoradiography. Molecular-weight markers (94, 67, 43 kD) are shown at left.
Gel analysis of eluates from Affi-Gel Blue columns. Equivalent amounts of media transfected with pSG5-RSA (RSA), pSG5-HLA (HLA), or pSG5 (CON), and metabolically labeled with 35S-Met and -Cys were chromatographed on separate Affi-Gel Blue minicolumns. Bound material was eluted with the salt concentrations shown below the lanes, and resolved by SDS-PAGE followed by fluorography and autoradiography. Molecular-weight markers (94, 67, 43 kD) are shown at left.
Analysis of Thrombin Inhibition and Binding by Fused and Unfused Hirudins
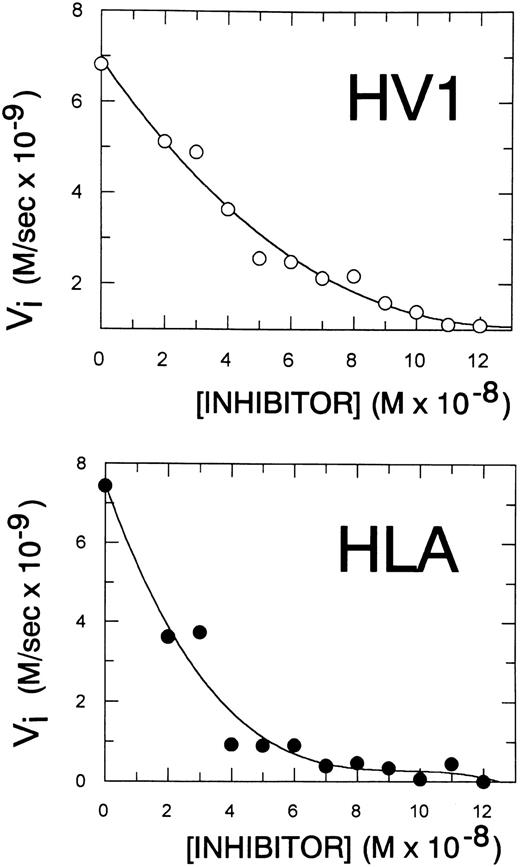
To compare the ability of HLA and HV1 to inhibit thrombin in a more quantitative manner, kinetic titration experiments were performed. No decrease in the affinity of interaction of the fusion protein with thrombin was detected in experiments in which the concentration of HLA or unfused commercial HV1 required to halve the initial rate of thrombin-mediated S2238 was determined (Fig 6). It was found that 40 nmol/L HV1 or 30 nmol/L HLA was required to reduce the initial rate of 1.9 nmol/L thrombin-mediated amidolysis of S2238 by 50% (to 3.5 × 10−9 mol/L/s). Similar results were obtained in an independent series of experiments in which fused or unfused hirudin was the immobilized “receptor,” and the specific binding of 125I-thrombin, serving as the radioligand, was determined in the presence of increasing amounts of competitor HLA or HV1; here, the IC50 for HLA as an inhibitor of the HV1-thrombin binding was 72 ± 5 pmol/L, versus 97 ± 3 pmol/L for HV1 as an inhibitor of the HLA-thrombin binding (data not shown, n = 3, ±SEM). Taken together, the results of both kinetic and binding experiments suggest that fusion of hirudin to albumin did not significantly reduce its potency as a thrombin-binding inhibitor.
Kinetic titration of fused and unfused hirudin as an inhibitor of thrombin-mediated amidolysis. The initial velocity of the reaction of thrombin with chromogenic substrate S2238 was determined in the presence of increasing concentrations of either unfused (HV1, top graph) or fused hirudin (HLA, bottom graph). Results shown are from one paired experiment that is representative of a total of three.
Kinetic titration of fused and unfused hirudin as an inhibitor of thrombin-mediated amidolysis. The initial velocity of the reaction of thrombin with chromogenic substrate S2238 was determined in the presence of increasing concentrations of either unfused (HV1, top graph) or fused hirudin (HLA, bottom graph). Results shown are from one paired experiment that is representative of a total of three.
Purification of His-Tagged HLA
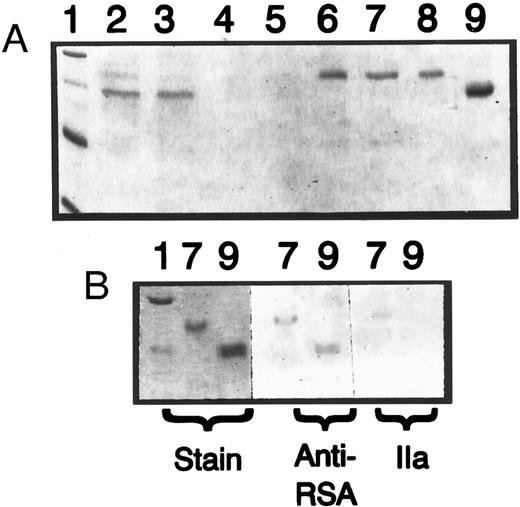
The retention of albumin-like dye-binding characteristics by fusion protein HLA suggested that it might also have acquired the property of slow plasma clearance; its retention of high-affinity thrombin-binding capacity made investigating its clearance worthwhile. To facilitate HLA purification, given the relatively small amounts of protein produced by COS cells (1 to 4 μg/100-mm plate of cells), pSG5-HLA was altered to encode a protein identical to HLA, but with an His6 tag on the C-terminus. After determining that the product of the resulting plasmid, pSG5-HLA(H)6 , inhibited thrombin in an indistinguishable manner from HLA lacking the His tag, 30 plates of cells were transfected with the pSG5-HLA(H)6 . Their conditioned media was pooled, and HLA(H)6 was purified by Ni2+-chelate affinity chromatography. Examination of material eluted from the nickel column showed that it contained a polypeptide of the expected size (75 kD) and minor quantities of a contaminating protein of 45 kD (Fig 7A, lane 6). This contaminant copurified with the major product on Affi-Gel Blue but, unlike the 75-kD protein, could be removed through its binding to heparin-Sepharose to yield a homogenous preparation (Fig 7A, lanes 6 through 8). The 75-kD species was identified as HLA(H)6 , as it reacted both with anti-RSA antibodies and with thrombin, in a blot overlay assay (Fig 7B). Moreover, the purified material inhibited thrombin amidolytic activity in a manner indistinguishable from nontagged HLA. Iodination of this material using the Iodogen method (Fig 8, inset A, HH6) supported the assertion that the material was purified, because no other bands were visible on the autoradiogram.
Purification and characterization of HLA(H)6 . (A) A 10% SDS gel stained with Coomassie Blue, on which aliquots of fractions containing HLA(H)6 were electrophoresed at different stages of its preparation. Lane 2, conditioned media from Cos cells transfected with pSG5-HLA(H)6 ; lane 3, flow-through from Ni-NTA-agarose column; lanes 4 and 5, wash fractions with and without Tween 20; lane 6, peak of eluate from Ni-NTA-agarose column; lane 7, eluate from Affi-Gel Blue; lane 8, flow-through from heparin-Sepharose. Lane 9 contains 1.0 μg of plasma-derived RSA, and lane 1 shows molecular weight markers (same as Fig 3). (B) Additional electrophoresis of aliquots of samples shown in lanes 7 and 9 in (A); the gel was cut in three, and portions stained with Coomassie Blue (Stain), immunoblotted with anti-RSA as in Fig 3, or blot-overlaid with thrombin (IIa).
Purification and characterization of HLA(H)6 . (A) A 10% SDS gel stained with Coomassie Blue, on which aliquots of fractions containing HLA(H)6 were electrophoresed at different stages of its preparation. Lane 2, conditioned media from Cos cells transfected with pSG5-HLA(H)6 ; lane 3, flow-through from Ni-NTA-agarose column; lanes 4 and 5, wash fractions with and without Tween 20; lane 6, peak of eluate from Ni-NTA-agarose column; lane 7, eluate from Affi-Gel Blue; lane 8, flow-through from heparin-Sepharose. Lane 9 contains 1.0 μg of plasma-derived RSA, and lane 1 shows molecular weight markers (same as Fig 3). (B) Additional electrophoresis of aliquots of samples shown in lanes 7 and 9 in (A); the gel was cut in three, and portions stained with Coomassie Blue (Stain), immunoblotted with anti-RSA as in Fig 3, or blot-overlaid with thrombin (IIa).
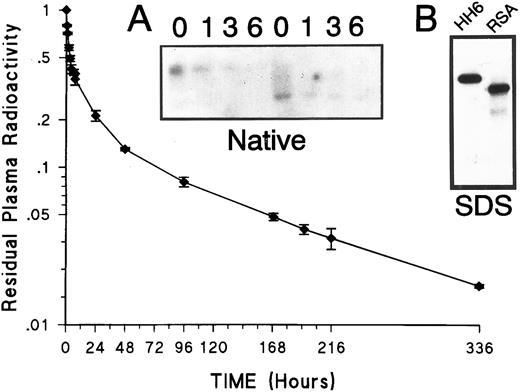
Clearance of HLA(H)6 from the rabbit circulation. Rabbits were injected with 125I-HLA(H)6 , and the fraction of the protein-bound radioactivity remaining in the circulation was determined over time (n = 3, ±SD). (Inset A) An autoradiogram of a 10% polyacrylamide nondenaturing gel (Native), on which 5 μL of plasma from rabbits injected with HLA (first four lanes) and RSA (last four lanes) have been electrophoresed. (Inset B) An autoradiogram of a 10% SDS gel (SDS) on which aliquots of radioiodinated purified HLA(H)6 (HH6), and purified plasma-derived RSA (RSA) have been electrophoresed.
Clearance of HLA(H)6 from the rabbit circulation. Rabbits were injected with 125I-HLA(H)6 , and the fraction of the protein-bound radioactivity remaining in the circulation was determined over time (n = 3, ±SD). (Inset A) An autoradiogram of a 10% polyacrylamide nondenaturing gel (Native), on which 5 μL of plasma from rabbits injected with HLA (first four lanes) and RSA (last four lanes) have been electrophoresed. (Inset B) An autoradiogram of a 10% SDS gel (SDS) on which aliquots of radioiodinated purified HLA(H)6 (HH6), and purified plasma-derived RSA (RSA) have been electrophoresed.
In Vivo Clearance of Radiolabeled, His-Tagged HLA
The clearance of HLA(H)6 was quantified following injection of three rabbits (weight 2.2 to 2.4 kg) with tracer levels of 125I-labeled HLA(H)6 (32 million cpm protein bound radioactivity each, corresponding to 1.6 μg). The protein-bound radioactivity in blood samples taken over the next 2 weeks was determined, and the residual radioactivity was plotted against time (Fig 8). Even after 2 weeks (336 hours), greater than 2% of the injected material remained in the circulation. Computer-assisted curve peeling revealed three terms in the equation required to describe the clearance curve (see Materials and Methods), suggesting that a three-compartment model was most accurate. The results showed a catabolic half-life of 4.60 ± 0.16 days, a noncirculating vascular wall half-life of 0.48 ± 0.03 days, and a circulatory half-life of 0.029 ± 0.006 days. Fractional catabolic rates and distributions from these experiments are presented in Table 1, compared with those reported for RSA. Compared with RSA, HLA(H)6 exhibits similar pharmacokinetic behavior, with a somewhat larger distribution into the extravascular space, and a somewhat increased rate of catabolism in the plasma compartment. Compared with catabolic half-life estimates (t1/2 β values) and fractional catabolic rates for whole-body elimination of hirudin on the order of hours,36 these results suggest that fusion protein HLA acquires the long in vivo residency time of serum albumin.
Pharmacokinetic Properties of Fused Hirudin and RSA
| . | HLAH6 . | RSA . |
|---|---|---|
| jT | .151 ± .009 | .125 ± .002 |
| j3 | .792 ± .019 | .314 ± .001 |
| j3.5 | .436 ± .055 | .248 ± .018 |
| Ap | .191 ± .008 | .399 ± .007 |
| Aw | .160 ± .053 | .109 ± .035 |
| Ae | .649 ± .061 | .532 ± .024 |
| . | HLAH6 . | RSA . |
|---|---|---|
| jT | .151 ± .009 | .125 ± .002 |
| j3 | .792 ± .019 | .314 ± .001 |
| j3.5 | .436 ± .055 | .248 ± .018 |
| Ap | .191 ± .008 | .399 ± .007 |
| Aw | .160 ± .053 | .109 ± .035 |
| Ae | .649 ± .061 | .532 ± .024 |
Comparison of fractional catabolic rates and compartmental distributions of HLA(H)6 (this study, see Fig 8) and of RSA.36 Symbols: jT , j3 , and j3.5 , fractions of fusion protein or RSA in total body, plasma compartment, and plasma compartment plus noncirculating vessel wall catabolized per day; Ap , Aw , and Ae , fractions of total body fusion protein or RSA in plasma, noncirculating vessel wall, and extravascular compartments, respectively. Data were calculated from individual plasma curves as described in Materials and Methods.
Two additional experiments were also performed. In the first, an identical dose of 125I-labeled HLA(H)6 as in the full clearance study was used in one rabbit, while another received an equivalent dose of 125I-labeled plasma-derived RSA. Plasma samples were collected over time from both animals, and analyzed on nondenaturing gels (Fig 8, inset A). This mode of electrophoresis allowed separation of the HLA(H)6 from the large, unlabeled albumin band, and showed a clear difference in mobility between labeled fusion protein and labeled RSA in plasma, one that persisted for at least 6 hours. No breakdown products were detected, suggesting that the fusion protein remains intact in vivo. Secondly, we injected the same tracer dose of labeled HLA(H)6 into each of two rabbits, and compared the residual plasma radioactivity after 4 hours with two rabbits injected with an equivalent dose of 125I-labeled commercial HV1; 45% ± 3% of the former, but only 10% ± 4% of the latter remained in the plasma. Urine from both sets of animals was collected, and after 24 hours 76% ± 6% of the HV1-, but only 12% ± 1% of the HLA(H)6 -derived radioactivity was found in the urine. These results are consistent with both our more extensive clearance study (Fig 8) and previously published results,36 and also support the contention that fusion protein HLA(H)6 clears less rapidly than unfused hirudin.
DISCUSSION
The purpose of this investigation was to determine if a genetic fusion of hirudin and albumin could be performed in a way that would yield a novel polypeptide which retained the potent antithrombin activity of hirudin and the slow clearance of serum albumin. COS cell expression was selected over systems in which higher yields are possible, to avoid complicating the characterization of candidate proteins with the necessity to consider de-aggregation or solubilization and refolding protocols. The first priority of this project was to establish functional and separate expression of the two parental proteins to be fused. As shown in Figs 1 and 4, transfection of the synthetic HV3 cDNA into COS cells resulted in the appearance of an antithrombin activity in the conditioned media of comparable affinity to that of commercial HV1 produced in yeast. Similarly, transfection of the full-length RSA cDNA into COS cells resulted in the appearance of recombinant RSA with electrophoretic (Fig 2) and chromogenic (Fig 5) properties indistinguishable from its plasma-derived counterpart.
To maximize the probability of independent folding and independence of action of the two portions of the fusion proteins, a hexaglycine spacer was engineered into both candidate fusion proteins, HLA and ALH. Similar strategies have been successfully used in the generation of heavy- and light-chain Ig fusion proteins.37 HLA, but not ALH, inhibited thrombin-mediated cleavage of both chromogenic and natural substrates (Fig 4). Although it has been reported that even minor perturbations of the amino-terminal region of hirudin interfered with antithrombin activity,38 our results do not preclude nonspecific explanations of the lack of function of ALH. Examination of the fusion proteins coelectrophoresed on an immunoblot (Fig 3B) suggests that ALH exhibits a faster mobility, indicative either of degradation or misfolding (such as that exhibited by antithrombin Utah in ref 31). The latter explanation is supported by the finding of consistently reduced secretion or synthesis of ALH compared to HLA (not shown). Irrespective of the mechanism(s) involved in the lack of activity of ALH, these results suggested that further characterization of HLA, but not ALH, was warranted.
Both quantitative binding and kinetic experiments showed no large differences in reactivity when the inhibition of thrombin by the fusion protein was compared with its inhibition by unfused hirudin. Kinetic titration experiments (Fig 6) showed near equivalence in terms of the concentration of inhibitor required to reduce the initial rate of thrombin inhibition by twofold (40 nmol/L HV1 v 30 nmol/L HLA). Similarly, in a binding assay in which 125I-labeled thrombin could bind to either immobilized HV1, or soluble HLA, or vice versa, highly similar IC50 values (73 pmol/L for HLA v 95 pmol/L for HV1) were obtained. The observation that HLA was slightly more inhibitory in both sets of experiments than unfused HV1 may derive from the incorporation of HV3 rather than HV1 into the fusion protein, because this hirudin variant exhibits a threefold to fourfold increase in affinity for thrombin compared with HV1.32 These quantitative results confirm the retention of potent antithrombin activity characterized by fusion protein HLA.
These findings, together with the retention of albumin-like dye-binding characteristics by HLA (Fig 5), prompted us to investigate the clearance of HLA in vivo. This experiment was made feasible by the generation of an His-tagged HLA that could be purified in the microgram quantities necessary for radiolabeling. In previous investigations of the clearance of radiolabeled HV1 in rabbits, 2 hours after injection only 2% of the HV1 remained in the circulation36; in the case of HLA, this level of injected protein was still present in the circulation after 2 weeks. This represents an increase in catabolic half-life from 0.7 hours36 to 4.60 ± 0.16 days. This value is much closer to that obtained for the clearance of radiolabeled RSA in rabbits (5.55 ± 0.11 days)39 and suggests that via incorporation into HLA, the clearance of HV3 has been made much more like that of RSA than HV1. Gel analysis of HLA recovered from rabbit blood after injection, compared with RSA treated in an identical fashion, renders unlikely the possibility of separation of the hirudin and albumin domains in HLA (Fig 8, inset A). Reduced clearance is also supported by our finding of decreased levels of radioactivity derived from injected labeled proteins in the urine of rabbits treated with HLA, as opposed to unfused hirudin.
Previous efforts to increase the half-life of hirudin in the circulation have included addition of dextran particles and polyethylene glycol chains to the inhibitor, resulting in an increase in t1/2β of approximately one order of magnitude14,15; we have demonstrated in this study that gene fusion increases the t1/2β of hirudin by greater than two orders of magnitude (160-fold). In addition, coupling procedures that use reactive amino groups will, at least in part, modify the N-terminus of hirudin, a region where even minor modifications can have negative effects on function.38 Such heterogeneity is also expected to occur in approaches that use chemical cross-linking to form adducts of hirudin with other proteins, eg, streptokinase40 and albumin.41 In neither instance was the fate of these adducts determined in vivo.
Clinical trials comparing hirudin to heparin and other conventional therapies have had mixed results, suggesting potential advantages of hirudin in the prevention of deep-vein thrombosis.42 However, unexpectedly high rates of bleeding complications in the setting of coronary thrombolysis suggest a relatively narrow window of safety.43 44 The availability of hirudins with longer durations of action could be relevant to this problem, in that the ability to use lower, but longer-acting, doses could conceivably expand this window. Irrespective of the future uses of hirudin per se, our results suggest that gene fusion to long-lived plasma proteins is a feasible means to extend the availability of anticoagulant peptides, and provide the impetus to scale-up production of HLA to study its biologic effects in vivo. With respect to this last point, it would clearly have been informative to have shown prolonged effects of HLA, rather than simply its prolonged presence in vivo; however, the minimum dose required for such an effect exceeded our capacity to generate HLA protein in COS-1 cells. We are in the process of full characterization of HLA produced in yeast and anticipate that this expression system will allow us to determine the effectiveness of HLA as an antithrombotic agent in future experiments.
ACKNOWLEDGMENT
The authors thank Dr Gerard Wright (Department of Biochemistry, McMaster University) for helpful discussions and the loan of equipment, and Drs Morris Blajchman, Mark Hatton, and Fred Ofosu (Department of Pathology and Medicine, McMaster University) for helpful discussions, enthusiastic support, and review of the manuscript.
Supported by a Grant-In-Aid from the Heart and Stroke Foundation of Ontario. W.P.S. is a Bayer/Canadian Red Cross Society/Medical Research Council of Canada Scholar.
Preliminary reports describing some of this work have appeared in abstract form (Thromb Haemost 73:145, 1995; and Blood 86:358a, 1995).
Address reprint requests to William P. Sheffield, PhD, Department of Pathology, HSC 3N10, McMaster University, 1200 Main St W, Hamilton, Ontario, Canada L8N 3Z5.

![Fig. 3. Expression of HV3, RSA, and fusion proteins. (A) Schematic, linear representations of the recombinant proteins produced in this study. Hatched areas represent HV3 segment, while solid areas correspond to RSA segments. L1, linker 1 [(G)6SM]; L2, linker 2 [MV(G)6 ]. Size of proteins, in amino acids (aa), is given at right. (B) An anti-RSA immunoblot showing immunoreactive components of conditioned media from Cos cells transfected with the following plasmids: pSG5-RSA (RSA), pSG5-HLA (HLA), pSG5-ASR (ASR), pSG5-ALH (ALH), and pSG5 lacking any insert (CON). Horizontal marks, at left, indicate the positions of the 94-, 67-, 43-, and 30-kD molecular-weight markers.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/89/9/10.1182_blood.v89.9.3243/3/m_bl_0055f3.jpeg?Expires=1767924031&Signature=qsVlyuSSFFLOp7xq0CtP7ahTb9dOFEm1lXSA24DLj3S2tK~kynTzALhkPj8q1uIjaVNoI2T8ibqiwS7CLHwT599XJJlr~VwiDLGMj-uYDIM4ItwTa7M5U6LqEYI8g4Rkjb0H0TwxqO730Ym4kCAbiJqRgNEPif~edxWJTG3vvhZYJHDUt4luHXPTY8TDF1O8R2x3GtD2TfuMqYpgTbM9brHOphEL4DJ3HwGJPThmpwvGKNuHMSKx8~GJ2kCw4IiXtqzbQhxn31goh7IpddU3gP0HSNgB~zZVcM36UW3ByjMPs698UEDISONm4rNPS0qiLCIikhILjsQCiK~sJFASZg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal