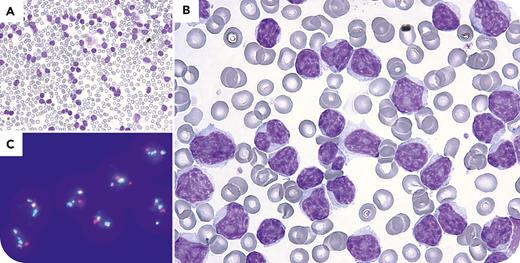
A 67-year-old man with no significant medical history presented with marked leukocytosis of 279.6 × 109/L identified on routine blood work. Peripheral blood smear revealed predominantly medium-sized lymphocytes with prolymphocytic morphology (relatively condensed but not clumped chromatin, regular nuclear outlines, and a single nucleolus) (panel A: 20× lens objective, original magnification ×200; panel B: 100× lens objective, original magnification ×1000; May-Grünwald stain for both panels). Scattered cells with chronic lymphocytic leukemia–like morphology were also noted. Imaging revealed a 21-cm splenomegaly without lymphadenopathy. Flow cytometry confirmed clonal B cells expressing CD19+, CD20++, CD5+, CD23−/+, CD22+dim, CD79b+, and a strong κ light chain. A definitive diagnosis of mantle cell lymphoma (MCL) was made through cytogenetic analysis, which demonstrated the hallmark t(11;14)(q13;q32) (panel C: metaphase fluorescence in situ hybridization dual-fusion probe [MetaSystems, Heidelberg, Germany]; 100× lens objective, original magnification ×1000: 1 green, 1 orange, and 2 green-orange fusion signals), along with del(13q14), monosomy 12 and del(17p). Next-generation sequencing identified a likely pathogenic variant in TP53. Bone marrow biopsy showed cyclin D1 positivity and SOX11 negativity.
This case highlights an atypical and aggressive presentation of leukemic nonnodal MCL with prolymphocytic morphology. The exclusion of B-prolymphocytic leukemia from the 5th edition of the World Health Organization Classification of Haematolymphoid Tumours and the redistribution of such cases into entities like MCL and other lymphoid variants underscore the importance of integrated diagnostic approaches.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal