In this issue of Blood, Watanabe-Kusunoki et al present new observations on the role of gasdermin D, demonstrating that it mediates neutrophil pyroptosis and contributes to a focal form of thrombotic microangiopathy (TMA) in the kidney in response to cholesterol crystal challenges.1 They suggest that gasdermin D is a potential therapeutic target for this disorder and potentially for other forms of TMA.
TMA, as suggested by its name, is a pathologic description of microvascular thrombosis. TMA is defined as a syndrome with heterogeneous causes characterized by the clinical features of microangiopathic hemolytic anemia, thrombocytopenia, and organ injury.2 The past 2 decades of basic and clinical research have provided a greater understanding of the molecular pathogenesis of many forms of TMA, exemplified by several primary TMAs, including hereditary or acquired ADAMTS13 deficiency-mediated TMA (alias thrombotic thrombocytopenic purpura) and complement-mediated TMA. These discoveries have led to groundbreaking targeted therapies that have revolutionized the clinical management of these potentially fatal disorders.
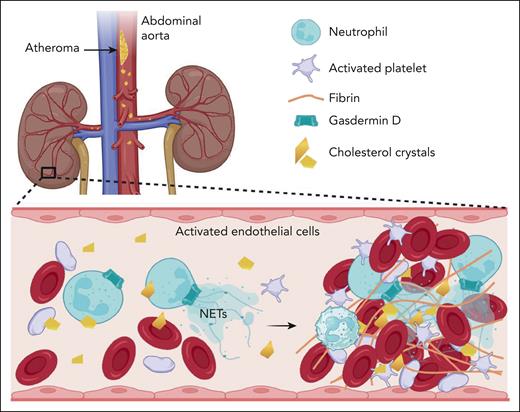
The study by Watanabe-Kusunoki et al describes the involvement of gasdermin D in a mouse kidney TMA model, which exhibits pathologic TMA induced by cholesterol crystal injection (termed “focal crystalline TMA”) (see figure). Gasdermin D is similar to complement, creating pores in cell membranes. When activated by inflammatory caspases, such as caspases 1, 4, 5, and 11, gasdermin D oligomerizes and forms pores in cellular membranes.3 Gasdermin D is recognized for facilitating interleukin-8β secretion and promoting neutrophil extracellular traps (NETs or suicidal NETosis) and pyroptosis triggered by intracellular infections. However, its significance in the molecular pathogenesis of sterile inflammation-related TMA lesions remains elusive. The authors found that gasdermin D, likely in neutrophils, is crucial for developing focal crystalline TMA and subsequent acute ischemic injury in the kidney. They discovered that gasdermin D was involved in neutrophil β2 integrin activation, pyroptosis-mediated NETosis, and thromboinflammation in response to cholesterol crystals. Therapeutic administration of disulfiram, an inhibitor of gasdermin D pore formation that does not affect other inflammasome components, protected mice from crystalline TMA and acute kidney ischemic injury.
Model depicting cholesterol emboli, originating from the atheromatous plaques of the abdominal aorta, activate gasdermin D on neutrophils, leading to pyroptosis-mediated neutrophil extracellular trap (NET)osis, thromboinflammation, and subsequent obstruction of microcirculation in the kidney. Figure created using bioRender.
Model depicting cholesterol emboli, originating from the atheromatous plaques of the abdominal aorta, activate gasdermin D on neutrophils, leading to pyroptosis-mediated neutrophil extracellular trap (NET)osis, thromboinflammation, and subsequent obstruction of microcirculation in the kidney. Figure created using bioRender.
Cholesterol crystal embolism is an acute and potentially fatal complication of advanced atherosclerosis.4 Cholesterol emboli originating from the rupture of atheromatous plaques of the aorta can affect almost every organ through microvascular obstructions and ischemic injury. The kidney is commonly affected by cholesterol emboli, causing acute inflammation and fibrin thrombi in small arteries, arterioles, and glomeruli, which are similar to disorders traditionally described as TMA.5
The diverse causes of TMA continue to expand.2,6 Primary TMA is typically accompanied by clinical features of microangiopathic hemolytic anemia, thrombocytopenia, and organ injury. However, renal-limited forms of TMA, such as those secondary to renal transplantation and as described in this study by Watanabe-Kusunoki et al, are not uncommon.5,7 The inducible mouse model of kidney TMA reported here enables the analysis of lesion progression in gasdermin D knockout mice and investigation of cholesterol crystals as a trigger for causing microvascular thrombosis. However, further studies are required to determine whether gasdermin D–mediated neutrophil pyroptosis is involved in the pathogenesis of other forms of TMA with different causes.
Conflict-of-interest disclosure: L.X. declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal