In this issue of Blood, Sardo et al expand our understanding of the interplay between erythropoiesis and iron metabolism.1 They have identified fibrinogen-like protein 1 (FGL1) as a novel erythroid regulator produced by hepatocytes in response to hypoxia that suppresses hepcidin, the master regulator of systemic iron homeostasis.
Because hemoglobin synthesis and red blood cell (RBC) production are strongly dependent on the availability of iron, erythropoiesis must be finely coordinated with iron metabolism. Accordingly, anemia is the main consequence of iron deficiency.
Systemic iron homeostasis is regulated by hepcidin, a liver-derived hormone that controls dietary iron absorption and iron recycling by blocking the activity of the iron exporter ferroportin.2 The expression of hepcidin is controlled by the bone morphogenetic protein–son of mother against decapentaplegic (BMP-SMAD) homolog pathway, activated by the ligands BMP2 and BMP6, and downregulated by transmembrane serine protease 6 (TMPRSS6).3
During increased erythropoietic activity, both physiological and pathological, the iron consumption by erythroid cells, already highly elevated in steady state, may rise by up to 5- to 10-fold. To cope with this enormous iron demand, hepcidin expression must be fully suppressed to favor the influx of iron into the bloodstream, a process that requires inhibition of the BMP-SMAD pathway. Supporting this logic, when the pathway is constitutively active, as in the case of TMPRSS6 mutations in patients with iron-refractory iron-deficiency anemia (Online Mendelian Inheritance in Man entry #206200), or in mice with genetic deletion of Tmprss6, hepcidin levels remain high despite expanded erythropoiesis,4 suggesting that the long-sought “erythroid regulator,” postulated by Clement Finch 50 years ago, should be a BMP-SMAD inhibitor. However, it remained elusive until 2014, when erythroferrone (ERFE) was identified by Kautz and colleagues.5
ERFE is an erythropoietin (EPO) target gene, secreted by the erythroid precursors in response to physiological (hemorrhage) and pathological (ineffective erythropoiesis) conditions, which downregulates hepcidin expression by sequestering BMP ligands, mainly BMP6 (see figure).6 Although ERFE is essential for hepcidin downregulation in the first hours after erythropoietic stress, it appears dispensable thereafter, as Erfe-deficient mice treated long term with EPO efficiently repress hepcidin,7 and ablation of Erfe in β-thalassemic mice does not correct hepcidin levels that remain inappropriately low relative to liver iron.8 Therefore, an ERFE-independent mechanism of hepcidin suppression likely acts in expanded erythropoiesis.
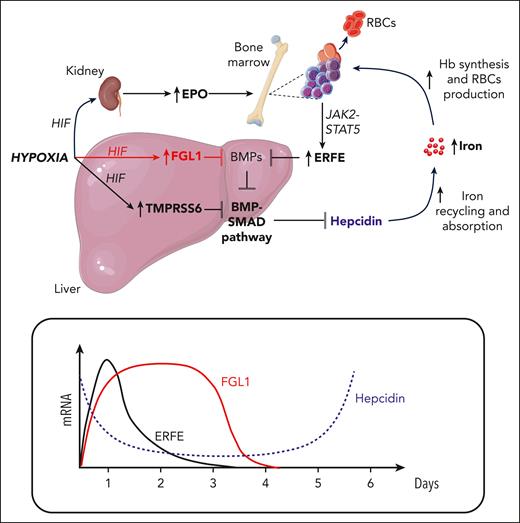
Under hypoxia (experimentally induced by controlled bleeding), the kidney increases production of EPO, a growth factor that stimulates proliferation of erythroid precursors and their differentiation into mature RBCs, whereas the liver upregulates the serine protease TMPRSS6 to decrease the BMP-SMAD pathway and hepcidin expression. In erythroid precursors, activation of the EPO-dependent signaling pathway, mediated by JAK2-STAT5, increases the production of ERFE, a secreted protein that inhibits the BMP-SMAD pathway and hepcidin by sequestering the BMP ligand BMP6. ERFE reaches its maximum concentration within 24 hours (lower panel) after bleeding. The liver plays a crucial role in the hypoxia-mediated inhibition of the BMP-SMAD pathway and hepcidin through the upregulation of the newly identified “erythroid regulator” FGL1. Like ERFE, FGL1 acts upstream of the BMP-SMAD signaling by sequestering BMP6. However, the timing of FGL1 expression is delayed compared with ERFE and reaches its maximum level 1 to 3 days after bleeding. Reduced production of hepcidin promotes iron recycling and uptake of dietary iron by stabilizing the sole iron exporter ferroportin at the cell membrane of macrophages and enterocytes, respectively, thereby increasing iron entry into the bloodstream. The coordinated activity of ERFE and FGL1, which ensures efficient hepcidin downregulation (lower panel), provides all the iron required by erythroid cells for hemoglobin synthesis and RBC production. HIF, hypoxia-inducible factor.
Under hypoxia (experimentally induced by controlled bleeding), the kidney increases production of EPO, a growth factor that stimulates proliferation of erythroid precursors and their differentiation into mature RBCs, whereas the liver upregulates the serine protease TMPRSS6 to decrease the BMP-SMAD pathway and hepcidin expression. In erythroid precursors, activation of the EPO-dependent signaling pathway, mediated by JAK2-STAT5, increases the production of ERFE, a secreted protein that inhibits the BMP-SMAD pathway and hepcidin by sequestering the BMP ligand BMP6. ERFE reaches its maximum concentration within 24 hours (lower panel) after bleeding. The liver plays a crucial role in the hypoxia-mediated inhibition of the BMP-SMAD pathway and hepcidin through the upregulation of the newly identified “erythroid regulator” FGL1. Like ERFE, FGL1 acts upstream of the BMP-SMAD signaling by sequestering BMP6. However, the timing of FGL1 expression is delayed compared with ERFE and reaches its maximum level 1 to 3 days after bleeding. Reduced production of hepcidin promotes iron recycling and uptake of dietary iron by stabilizing the sole iron exporter ferroportin at the cell membrane of macrophages and enterocytes, respectively, thereby increasing iron entry into the bloodstream. The coordinated activity of ERFE and FGL1, which ensures efficient hepcidin downregulation (lower panel), provides all the iron required by erythroid cells for hemoglobin synthesis and RBC production. HIF, hypoxia-inducible factor.
To identify this hypothetical player, Sardo and colleagues performed a microarray analysis of liver and bone marrow to pick out transcripts encoding secreted proteins, whose expression was induced in Erfe-deficient mice between 1 and 2 days after phlebotomy. Interestingly, the only transcript that came up in both liver and bone marrow was Fgl1 (see figure). FGL1, or hepassocin, is a member of the fibrinogen superfamily, mainly expressed by hepatocytes. It has been described as an acute-phase protein upregulated in patients with metabolic disorders and involved in the development and progression of cancer. In contrast to the BMP agonist property of fibrinogen, FGL1 acts as a BMP antagonist that, by binding BMP6 with its globular domain, suppresses hepcidin expression both in vitro and in vivo in male mice. The response to FGL1 is sexually dimorphic because female mice, which express more liver Fgl1 than males, are resistant to FGL1-mediated hepcidin downregulation. However, the physiological significance of these differences remains unclear.
Fgl1-deficient mice are viable, with no obvious phenotype other than increased body weight and glucose intolerance.9 Interestingly, although iron and hematological parameters are comparable with those of wild-type mice, hepcidin is higher in Flg1 knockout animals, and its downregulation by phlebotomy is attenuated, although Erfe is elevated as in wild-type mice. Interestingly, unlike ERFE, Fgl1 is not an EPO-target gene, but is induced by hypoxia through 2 hypoxia-inducible factor binding sites in its promoter region. In anemia, hypoxia caused by the reduction of RBCs and hemoglobin triggers a physiological response, which targets both EPO activity and iron homeostasis to replenish the number of RBCs in the circulation. This response involves increased EPO production by the kidney, an ERFE increase by bone marrow (and spleen), and upregulation of FGL1 and TMPRSS610 by hepatocytes, on one hand stimulating erythroid cell proliferation and differentiation and, on the other, ensuring iron supply by inhibiting hepcidin expression (see figure).
Unbalanced activation of these signaling pathways has deleterious effects, as in the case of β-thalassemia, where long-term suppression of hepcidin by expanded ineffective erythropoiesis and hypoxia causes systemic iron overload and organ failure.
Although the involvement of FGL1 in the pathophysiology of the disease remains to be clarified, blocking or interfering with its activity may represent a novel therapeutic approach for iron-loading anemias, characterized by increased Fgl1 expression in the liver. That hepatocytes are the main source of FGL1 is particularly attractive from a therapeutic viewpoint. Indeed, this cell type is easily accessible for the administration of short interfering RNA or antisense oligonucleotides conjugated with N-acetylgalactosamine, which leads to rapid endocytosis of nucleic acids and selective degradation of target RNAs by binding to the asialoglycoprotein receptor highly expressed on hepatocytes.
Future studies and novel tools are required to prove the relevance of FGL1 in human physiology and disease. However, the evidence that FGL1 shares 82% identity between human and mouse suggests that its function is also conserved.
With the identification of FGL1, Sardo and colleagues add another piece to the complex regulation of hepcidin; suggest a further link between hypoxia, iron regulation, and metabolism; and offer another potential target to be explored in the treatment of diseases characterized by a dysregulated cross talk between erythropoiesis and iron metabolism.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal