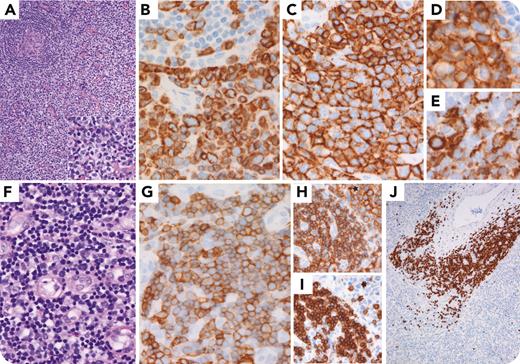
A 57-year-old man presented with fatigue. Imaging revealed massive splenomegaly and generalized lymphadenopathy. Inguinal node biopsy showed involvement by peripheral T-cell lymphoma with T-follicular helper phenotype (PTCL-TFH), comprising an interfollicular infiltrate of medium-sized lymphocytes with clear cytoplasm (panel A, hematoxylin and eosin [H&E] 4× and 10× objective, inset). These cells expressed CD3 (panel B, 40× objective), CD4, CD2, CD5, CD7, T-cell receptor β, and aberrant CD20 (panel C, 40× objective) with scattered Epstein-Barr virus and all TFH markers (viz, PD-1 [panel D, 40× objective], inducible T-cell costimulator [panel E, 40× objective], and CXCL13). A second, patchy blastoid lymphoid component was also seen interspersed (panel F, H&E 40× objective). This second component expressed CD3 (not shown), dim CD5 (panel G, 40× objective), dual CD4/CD8 (panels H and I, respectively, 10× objective; ∗angioimmunoblastic T-cell lymphoma-like areas), as well as terminal deoxynucleotidyltransferase (TdT) (panel J, 4× objective), supporting a concurrent minor indolent T-lymphoblastic proliferation (iT-LBP). Next-generation sequencing revealed a pathogenic frameshift mutation in exon 4 of the TP53 gene.
iT-LBP is defined by aggregates of nonclonal TdT+/CD3+ T-lymphoid blasts, most often coexpressing CD4 and CD8. In lymph nodes, iT-LBP occupies interfollicular regions and may be associated with Castleman disease, Castleman disease–like changes, follicular dendritic cell sarcoma, or AITL. Though recurrences have been observed, iT-LBP is clinically indolent, and treatment is not required. Awareness of this entity is important, as T-lymphoblastic lymphoma/leukemia overlaps immunophenotypically with iT-LBP.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal