Key Points
In the population with SCA, for whom most deaths are attributable to sudden cardiac death, VA are common and mostly affect men.
Left ventricular GLS using speckle tracking echocardiography appears to be a valuable parameter for improving rhythmic risk stratification.
Abstract
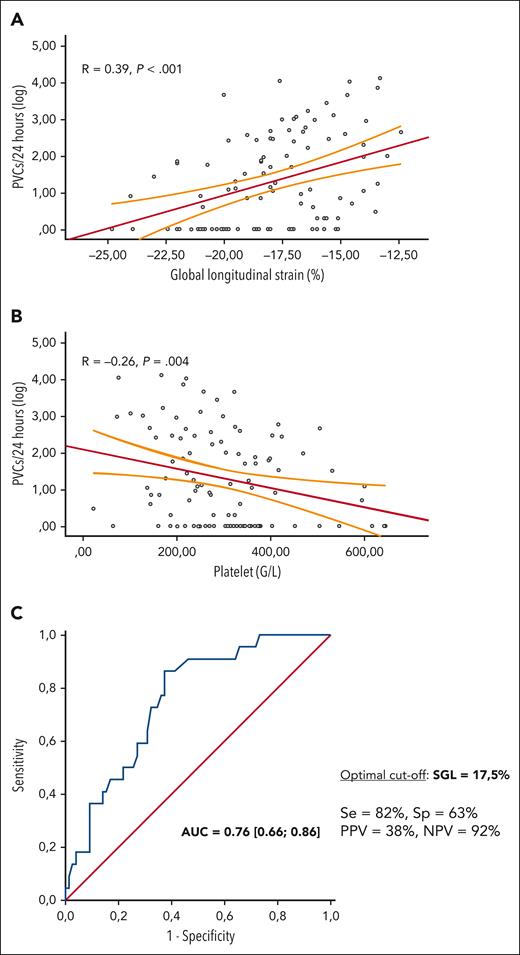
Sudden death is 1 of the leading causes of death in adults with sickle cell anemia (SCA) but its etiology remains mostly unknown. Ventricular arrhythmia (VA) carries an increased risk of sudden death; however, its prevalence and determinants in SCA are poorly studied. This study aimed to identify the prevalence and predictors of VA in patients with SCA. From 2019 to 2022, 100 patients with SCA were referred to the physiology department to specifically analyze cardiac function and prospectively included in the DREPACOEUR registry. They underwent a 24-hour electrocardiogram monitoring (24h-Holter), transthoracic echocardiography, and laboratory tests on the same day. The primary end point was the occurrence of VA, defined as sustained or nonsustained ventricular tachycardia (VT), >500 premature ventricular contractions (PVCs) on 24h-Holter, or a recent history of VT ablation. The mean patient age was 46 ± 13 years, and 48% of the patients were male. Overall, VA was observed in 22 (22%) patients. Male sex (81% vs 34%; P = .02), impaired global longitudinal strain (GLS): –16% ± 1.9% vs –18.3% ± 2.7%; P = .02), and decreased platelet count (226 ± 96 giga per liter [G/L] vs 316 ± 130 G/L) were independently associated with VA. GLS correlated with PVC load every 24 hours (r = 0.39; P < .001) and a cutoff of –17.5% could predict VA with a sensitivity of 82% and a specificity of 63%. VAs are common in patients with SCA, especially in men. This pilot study uncovered GLS as a valuable parameter for improving rhythmic risk stratification.
Introduction
Sickle cell disease (SCD) is the most common inherited blood disorder in the world.1 Major medical advances, such as antibiotic prophylaxis, vaccination, hydroxyurea, and red blood cell exchange, have considerably improved the prognosis of homozygous patients with SCD—also called sickle cell anemia (SCA)—but unmasked chronic disease complications, among which cardiovascular impairment and sudden death are the leading causes of mortality.2-9 Although the exact cause of sudden death is often unknown and may include cardiovascular, thromboembolic, or cerebral etiologies, it is likely that a significant proportion might be attributable to ventricular rhythm disorders, such as in the general population.10-13
Cardiac involvement in SCA is complex and not fully understood but leads to diffuse myocardial fibrosis, a well-known substrate of VA, especially in the context of arrhythmogenic triggers such as hypoxemia, acidosis, or hydroelectricity disorders, which are frequently observed in this population.14-20 Previous case studies and health care database analyses reported electrocardiographic abnormalities such as increased QT prolongation and a higher prevalence of arrhythmias in patients with SCA, which increases the risk of developing fatal arrhythmias.21-23 This proarrhythmogenic environment has recently been observed in an SCA murine model, in which mice exhibited an increased susceptibility to ventricular tachycardia (VT).24 Despite accumulating evidence supporting the existence of ventricular arrhythmia (VA) in patients with SCA, there is currently no data thoroughly assessing its prevalence, determinants, and impact on prognosis.
Here, we propose to shed new light on VA in patients with SCA through a comprehensive evaluation that integrates electrocardiographic monitoring along with the patient’s phenotype, cardiac imaging, and biological analysis.
Method
Study population
From November 2018 to March 2022, adult patients with SCD followed at the Sickle Cell Referral Center of Henri Mondor teaching hospital (Créteil, France) and referred to the ambulatory cardiology department for documented or suspected cardiac involvement (refer to the criteria below) were included in the DREPACOEUR, a multicentric prospective registry. Inclusion criteria included patients with SCD who were >15 years and 3 months (with parental consent between 15 and 18 years old), at steady state (at least 1 month following acute complication) with 1 of the following features:
Chest pain suggestive of angina
Aggravation of dyspnea without argument for hematological etiology, justifying cardiopulmonary assessment
Recent hospitalization for an episode of decompensated heart failure
Abnormalities documented on echocardiography including left ventricular ejection fraction (LVEF) <50%, tricuspid regurgitation velocity (TRV) ≥2.5 meters per second (m/s),25,26 or E/A ratio <14
Abnormalities documented on cardiac magnetic resonance imaging (MRI) including: LVEF <50% or presence of iron overload (T2∗ < 20 milliseconds [ms])
Elevation of cardiac biomarkers (N-terminal probrain natriuretic peptide [NT pro-BNP]/BNP/troponin) according to laboratory standards
Frequent or consistent palpitations or electrocardiographic abnormalities such as ST-segment changes, rhythm, or conduction disorders
History of stroke with a suspicion of cardioembolic etiology after ruling out a vascular etiology
Surgery or hematopoietic stem cell transplantation justifying a previous cardiothoracic assessment
During the 1-day hospitalization, these patients underwent a physical examination, electrocardiogram (ECG), transthoracic echocardiography associated with speckle tracking imaging to assess systolic deformation, a 6-minute walking test, and a biology workup. Ambulatory pressure monitoring, 24-hour electrocardiogram monitoring (24h-Holter), computerized tomography (CT) coronary angiogram, and noninvasive testing for myocardial ischemia were also performed, pending the clinical presentation and decision of the cardiologist and SCD experts. Cardiac CT and noninvasive testing for myocardial ischemia were the only investigations that were not necessarily performed on the day of the visit.
For this analysis, only patients with SCA (SS or Sβ0) who underwent 24-hour ECG-Holter were included. Written informed consent was collected from all participating patients, and the database was declared to the Commission Nationale de l'Informatique et des Libertés (CNIL n°7830264) and approved by the ethics committee (protocol number 2013/NICB).
Data collection
All patients were interviewed, had their medical records examined, and underwent a physical examination. Height (cm) and weight (kg) were measured to calculate the body mass index. Blood pressure was measured as recommended.27 A resting ECG was performed to calculate the duration of the PR interval, QRS complex, and corrected QT. The presence of electrical left ventricular hypertrophy was investigated using the Sokolow-Lyon index.28 A history of cardiovascular risk factors was documented, including systemic hypertension, dyslipidemia, diabetes mellitus, active smoking, and sleep apnea obstructive syndrome. Routine laboratory tests (complete blood count, serum chemistry profile, lactate dehydrogenase, and NT pro-BNP) were performed at a 1-day hospital. The percentage of fetal hemoglobin in patients treated with hydroxyurea was obtained from a recent hemoglobin electrophoresis (<3 months) in the medical file.
24h-Holter
Simultaneous 3-channel 24h-Holter monitoring (NOVACOR, Rueil-Malmaison, France) was performed the day before hospitalization. The data were analyzed by a cardiologist who was blinded to the medical records. Premature atrial and ventricular contractions (premature atrial contractions [PAC] and premature ventricular contractions [PVC]) were quantified. Nonsustained VT was defined as 3 or more consecutive ventricular beats at a rate >100 beats per minute with a duration of <30 seconds and sustained VT was beyond 30 seconds. VA was defined according to European guidelines as the occurrence of sustained or nonsustained VT, >500 PVCs on 24h-Holter, or history of VT ablation.29 Moderate and high PVC burden were, respectively, set as 1000 to 10 000 per day and above 10 000 per day.30 The distribution of PVCs during nychthemeron and their morphology (polymorphic in the presence of 2 or more families of PVCs) were also collected.
Echocardiography evaluation
All patients underwent comprehensive 2-dimensional, M-mode, Doppler, and tissue Doppler echocardiography performed on the same ultrasound system (VIVID E95, General Electric, Boston, MA) according to contemporary guidelines by experienced sonographers blinded to the medical records.31,32 All studies were interpreted offline and in a blinded manner by a single cardiologist. Cardiac output, left ventricular (LV) end-diastolic volume, mass, and left atrial volume were indexed to the body surface area (cardiac index, LVEDVind [left ventricular end-diastolic volume indexed to body surface area], LVMind [left ventricular mass indexed to body surface area], and LAVind, respectively). The LV ejection fraction was calculated using Simpson biplane method. The LV global longitudinal strain (GLS) was acquired using automated functional imaging (using speckle tracking echocardiography) of 3 clips to perfectly track all myocardial segments in the apical 4-chamber, 2-chamber, and 3-chamber views. The mitral inflow velocity pattern, peak velocities of the early (E) and late (A) waves, and the E wave deceleration time were recorded. Tissue Doppler echocardiography was performed to measure early (e′) diastolic tissue velocities at the lateral mitral annulus. The lateral E/e′ ratio was used as a surrogate for LV filling pressure.33 Right ventricular (RV) function was assessed using tricuspid annular plane systolic excursion and the S' wave. Tricuspid regurgitation velocity was recorded to assess the pulmonary arterial pressure.34
Study end point
The objective of this study was to describe the prevalence and determinants of VA in patients with SCA with documented or suspected cardiac involvement in the DREPACOEUR registry.
Statistical analysis
All analyses were performed using SPSS 26 (IBM, Armonk, NY). Data are presented as percentages for categorical data and as mean ± standard deviation or median (interquartile range) for continuous variables, depending on the normality of their distribution. Comparisons between groups for continuous variables were performed using 1-way analysis of variance. The χ2 test was used to compare dichotomous variables. Multivariate analysis was then performed using binary logistic regression on the parameters available for all patients and was significantly associated with VA occurrence (P < .05). Notably the 6-minutes walking test data were not included in the multivariate analysis, given the large proportion of missing data. One-tailed Pearson’s correlation analyses were conducted on independent parameters associated with the end point. Odds ratios (ORs) are presented with a 95% confidence interval (CI). The area under the receiver operating characteristic curve (curve) was used to determine the accuracy of the LV GLS for identifying the VA. A P value <.05 indicated statistical significance.
Results
Population characteristics
Between July 2018 and March 2022, 200 patients with SCD were included in the DREPACOEUR registry based on arguments for cardiovascular disease. Among them, 173 (87%) had SS or Sβ0 (SCA), 6 (2%) had S/β-thalassemia, and 21 (11%) had the SC genotype. This study specifically included 100 patients with SCA who underwent a 24h-Holter before their hospitalization in the ambulatory cardiology department. The baseline clinical and laboratory characteristics are summarized in Table 1. Briefly, the mean age was 46 ± 13 years, 48% were male, and they were mostly referred for dyspnea (47%), chest pain (22%), palpitation, or ECG changes (11%), Table 1. Notably, none of the patients were included for myocardial iron overload on MRI. Patients had frequent disease complications (systemic hypertension, thromboembolic disease, and chronic kidney disease), Table 1. Most were treated with hydroxyurea (82%) and/or included in an erythrocytapheresis program (27%). Despite an overall preserved left ventricular ejection fraction in most of the patients (LVEF = 58% ± 6%), 6 (6%) had left ventricular dysfunction (40% < LVEF < 50%), and GLS was slightly reduced (–17.9% ± 2.7%, for a normal value ≤ –18%), with 51 (51%) > –18%, Table 2. The left cardiac cavities were dilated (LVEDVind = 81 ± 25 mL/m2 and LAVind = 57 ± 20 mL/m2). The RV function was preserved (tricuspid annular plane systolic excursion = 26 ± 5 mm). The tricuspid regurgitation velocity was 2.6 ± 0.3 m/s with 18 (19%) patients above 3 m/s. Forty-seven (47%) patients underwent coronary CT scan without any reported coronary artery disease. Twenty-four (24%) ischemic stress tests were performed and 6 patients exhibited electrical subendocardial ischemia with a normal coronary angiogram. Overall, epicardial coronary artery disease was ruled out in 60 (60%) patients and was unknown in the remaining cohort.
Clinical and biological characteristics of the studied population
| Characteristics . | Patients (n = 100) . |
|---|---|
| Demographic and clinical | |
| Age (y) | 46.0 ± 12.5 |
| Male, n (%) | 48 (48) |
| Body mass index (kg/m2) | 24.1 ± 4.3 |
| Systolic blood pressure (mmHg) | 131 ± 17.8 |
| Diastolic blood pressure (mmHg) | 76 ± 11.0 |
| Heart rate (beats per minute) | 72 ± 12 |
| Oxygen saturation (%) (n = 89) | 95 (93-97) |
| Referred for, n (%) | |
| Worsening of dyspnea | 47 (47) |
| Chest pain | 22 (22) |
| Palpitations or ECG changes | 11 (11) |
| Elevation of a cardiac biomarker | 5 (5) |
| Cardiac imaging abnormalities | 4 (4) |
| Episode of decompensated heart failure | 4 (4) |
| Recent stroke | 4 (4) |
| Pretransplant assessment (kidney/HSCs) | 3 (3) |
| Cardiovascular risk factors, n (%) | |
| Arterial hypertension | 67 (67) |
| Diabetes | 4 (4) |
| Dyslipidemia | 1 (1) |
| Obesity | 7 (7) |
| Obstructive sleep apnea syndrome | 11 (11) |
| Chronic kidney disease∗ | 35 (35) |
| Active smoking | 12 (12) |
| Thromboembolic history (PE/DVT) | 28 (28) |
| Treatment of SCD, n (%) | |
| None | 12 (12) |
| Hydroxyurea | 61 (61) |
| Erythrocytapheresis | 6 (6) |
| Hydroxyurea + erythrocytapheresis | 21 (21) |
| Bloodletting | 1 (1) |
| Biology | |
| Hemoglobin (g/dL) | 8.7 ± 1.5 |
| Leukocytes (G/L) | 7.8 ± 2.5 |
| Platelets (G/L) | 298 ± 128 |
| Potassium (mmol/L) | 4.3 ± 0.5 |
| Creatinine (μmol/L) | 63 (52-104) |
| GFR (based on CKD-EPI formula in mL/min per 1.73 m2) | 102 (86-118) |
| ASAT (IU/L) | 45 (32-60) |
| ALAT (IU/L) | 24 (20-34) |
| LDH (IU/L) | 446 (353-600) |
| Total bilirubin (μmol/L) | 29 (18-47) |
| Free bilirubin (μmol/L) | 20 (12-34) |
| Nt Pro-BNP (ng/L) | 155 (74-452) |
| Troponin T (Hs) (ng/L) | 5 (3-10) |
| Characteristics . | Patients (n = 100) . |
|---|---|
| Demographic and clinical | |
| Age (y) | 46.0 ± 12.5 |
| Male, n (%) | 48 (48) |
| Body mass index (kg/m2) | 24.1 ± 4.3 |
| Systolic blood pressure (mmHg) | 131 ± 17.8 |
| Diastolic blood pressure (mmHg) | 76 ± 11.0 |
| Heart rate (beats per minute) | 72 ± 12 |
| Oxygen saturation (%) (n = 89) | 95 (93-97) |
| Referred for, n (%) | |
| Worsening of dyspnea | 47 (47) |
| Chest pain | 22 (22) |
| Palpitations or ECG changes | 11 (11) |
| Elevation of a cardiac biomarker | 5 (5) |
| Cardiac imaging abnormalities | 4 (4) |
| Episode of decompensated heart failure | 4 (4) |
| Recent stroke | 4 (4) |
| Pretransplant assessment (kidney/HSCs) | 3 (3) |
| Cardiovascular risk factors, n (%) | |
| Arterial hypertension | 67 (67) |
| Diabetes | 4 (4) |
| Dyslipidemia | 1 (1) |
| Obesity | 7 (7) |
| Obstructive sleep apnea syndrome | 11 (11) |
| Chronic kidney disease∗ | 35 (35) |
| Active smoking | 12 (12) |
| Thromboembolic history (PE/DVT) | 28 (28) |
| Treatment of SCD, n (%) | |
| None | 12 (12) |
| Hydroxyurea | 61 (61) |
| Erythrocytapheresis | 6 (6) |
| Hydroxyurea + erythrocytapheresis | 21 (21) |
| Bloodletting | 1 (1) |
| Biology | |
| Hemoglobin (g/dL) | 8.7 ± 1.5 |
| Leukocytes (G/L) | 7.8 ± 2.5 |
| Platelets (G/L) | 298 ± 128 |
| Potassium (mmol/L) | 4.3 ± 0.5 |
| Creatinine (μmol/L) | 63 (52-104) |
| GFR (based on CKD-EPI formula in mL/min per 1.73 m2) | 102 (86-118) |
| ASAT (IU/L) | 45 (32-60) |
| ALAT (IU/L) | 24 (20-34) |
| LDH (IU/L) | 446 (353-600) |
| Total bilirubin (μmol/L) | 29 (18-47) |
| Free bilirubin (μmol/L) | 20 (12-34) |
| Nt Pro-BNP (ng/L) | 155 (74-452) |
| Troponin T (Hs) (ng/L) | 5 (3-10) |
Ordinal data are reported as mean ± standard deviation when they have a normal distribution, or as median (Q1-Q3) when they do not have a normal distribution, and nominal data as absolute value and percentage.
ALAT, alanine aminotransferase; ASAT, aspartate aminotransferase; CKD-Epi, Chronic Kidney Disease Epidemiology Collaboration; DVT, deep veinous thrombosis; GFR, glomerular filtration rate; HSCs, hematopoietic stem cells; LDH, lactate dehydrogenase; PE, pulmonary embolism.
GFR < 90 mL/min per 1.73 m2 according to CKD-EPI.
Echocardiographic variables in the study population
| Echocardiography data . | Patients . |
|---|---|
| LV function and remodeling | |
| LVEF in Simpson biplane (%) | 57.7 ± 5.8 |
| LVEF < 50%, n (%) | 6 (6) |
| GLS (%) | –17.9 ± 2.7 |
| GLS > –18% | 51 (51) |
| Cardiac output (L/min) | 6.2 ± 1.7 |
| End-diastolic ventricular diameter (mm) | 55.7 ± 6.7 |
| Indexed LV volume (mL/m2) | 80.6 ± 24.8 |
| Indexed LV mass (g/m2) | 110.2 ± 37.7 |
| Diastolic function | |
| E (cm/s) | 87 ± 21 |
| EDT (ms) | 192 ± 46 |
| A (cm/s) | 64 ± 20 |
| E/A | 1.5 ± 0.6 |
| E' lateral (cm/s) | 12.7 ± 3.7 |
| E/E' lateral | 7.8 ± 2.9 |
| Indexed LA volume (mL/m2) | 57.2 ± 19.8 |
| RV function and right pressures | |
| TAPSE (mm) | 25.6 ± 5.4 |
| S-wave (cm/s) | 14.6 ± 2.5 |
| TRV (m/s), n = 97 | 2.6 ± 0.3 |
| TRV ≥ 3 m/s, n (%) | 18 (19) |
| Pulmonary acceleration time (ms) | 133.4 ± 31.4 |
| Indexed tricuspid ring (mm/m2) | 19.4 ± 3.2 |
| RV end-diastolic area (cm2) | 20.9 ± 5.0 |
| Telesystolic area of the right atrium (cm2) | 20.1 ± 5.4 |
| Systolic pulmonary arterial pressure (mmHg) | 32.4 ± 8.6 |
| Right atrium pressure (mmHg) | 4.2 ± 2.7 |
| Valve disease | |
| Severe valve disease (grade 4), n (%) | 0 (0) |
| Mild to moderate valve disease (grade 2 and 3), n (%) | 10 (10) |
| Echocardiography data . | Patients . |
|---|---|
| LV function and remodeling | |
| LVEF in Simpson biplane (%) | 57.7 ± 5.8 |
| LVEF < 50%, n (%) | 6 (6) |
| GLS (%) | –17.9 ± 2.7 |
| GLS > –18% | 51 (51) |
| Cardiac output (L/min) | 6.2 ± 1.7 |
| End-diastolic ventricular diameter (mm) | 55.7 ± 6.7 |
| Indexed LV volume (mL/m2) | 80.6 ± 24.8 |
| Indexed LV mass (g/m2) | 110.2 ± 37.7 |
| Diastolic function | |
| E (cm/s) | 87 ± 21 |
| EDT (ms) | 192 ± 46 |
| A (cm/s) | 64 ± 20 |
| E/A | 1.5 ± 0.6 |
| E' lateral (cm/s) | 12.7 ± 3.7 |
| E/E' lateral | 7.8 ± 2.9 |
| Indexed LA volume (mL/m2) | 57.2 ± 19.8 |
| RV function and right pressures | |
| TAPSE (mm) | 25.6 ± 5.4 |
| S-wave (cm/s) | 14.6 ± 2.5 |
| TRV (m/s), n = 97 | 2.6 ± 0.3 |
| TRV ≥ 3 m/s, n (%) | 18 (19) |
| Pulmonary acceleration time (ms) | 133.4 ± 31.4 |
| Indexed tricuspid ring (mm/m2) | 19.4 ± 3.2 |
| RV end-diastolic area (cm2) | 20.9 ± 5.0 |
| Telesystolic area of the right atrium (cm2) | 20.1 ± 5.4 |
| Systolic pulmonary arterial pressure (mmHg) | 32.4 ± 8.6 |
| Right atrium pressure (mmHg) | 4.2 ± 2.7 |
| Valve disease | |
| Severe valve disease (grade 4), n (%) | 0 (0) |
| Mild to moderate valve disease (grade 2 and 3), n (%) | 10 (10) |
Ordinal data are reported as mean ± standard deviation and nominal data as absolute value and percentage.
A, mitral end-diastolic velocity; ASE, American Society of Echocardiography; E, mitral protodiastolic velocity; E', mitral protodiastolic annular velocity; EDT, E wave deceleration time; LA left atrium; LV, left ventricle; S, tricuspid annular mesosystolic velocity; TAPSE, tricuspid annular plane systolic excursion.
Seventy-eight patients (78%) underwent the 6-minute walking test, with a median distance of 490 m (415-559) (78% of the predicted value [67-88]) and frequent oxygen desaturation, with 49 (63%) patients falling below 88% during the test (supplemental Table 1, available on the Blood website).
Rhythmic data
Thirty-eight percent of the patients were already treated with antiarrhythmic compounds (mainly beta-blockers) for various overlapping indications, such as atrial hyperexcitability (58%) or dilated heart disease (31%) (Table 3). The QT interval on 12-lead surface ECG was normal in most of the patients (419 ± 26 ms) but was above 440 ms in 16 (16%) and at 480 ms in only 1 patient. VA was observed in 22 (22%) patients, 15 of whom had >500 PVCs every 24 hours (range, 500-13 000), 9 had episodes of nonsustained VT (range, 4-121 consecutive PVCs), and 1 patient had a recent history of VT ablation (Table 2). In addition, ECG-Holter uncovered atrial fibrillation in 3 (3%) patients and >500 PAC every 24 hours in 17 (17%) patients.
Rhythmic data and 24h-Holter monitoring results
| Characteristics . | Patients . |
|---|---|
| Corrected QT on surface ECG (ms) | 416 ± 26 |
| Corrected QT > 440 ms, n (%) | 16 (16) |
| LVH criteria, n (%) | 19 (19) |
| Heart rate (bpm) | 72 ± 12 |
| Antiarrhythmic medication, n (%) | 38 (38) |
| Beta-blockers | 35 (35) |
| Cordarone | 5 (5) |
| Flecaine | 2 (2) |
| Indication for beta-blockers, n = 35, n (%) | |
| Antianginal | 4 (11) |
| Atrial hyperexcitability or AF | 21 (58) |
| Ventricular hyperexcitability | 5 (14) |
| Dilated heart disease | 11 (31) |
| LV obstruction | 3 (8) |
| Arterial hypertension | 2 (5) |
| 24h-Holter results | |
| Ventricular data | |
| Total PVCs | 11 (0-259), (min 0; max 12 809) |
| PVCs > 500/24 h, n (%) | 15 (15) |
| NSVT (<30 sec), n (%) | 9 (9); range, 4-121 PVCs |
| SVT (≥30 sec), n (%) | 0 (0) |
| Patients with VA, n (%) | 22 (22) |
| Total PVCs (n = 22) | 984 (452-4035) |
| PVC > 1000 (n = 22), n (%) | 11 (50) |
| PVC > 10 000 (n = 22), n (%) | 3 (13) |
| Polymorphic trait (≥2 families) (n = 22) | 18 (82) |
| Daytime predominance (n = 22) | 20 (91) |
| Ventricular hyperexcitability under beta-blocker (n = 22) | 8 (36) |
| Atrial data | |
| Total PACs | 35 (5-254), (min 0; max 24 270) |
| PACs > 500/24 h, n (%) | 17 (17) |
| Atrial fibrillation, n (%) | 3 (3) |
| Characteristics . | Patients . |
|---|---|
| Corrected QT on surface ECG (ms) | 416 ± 26 |
| Corrected QT > 440 ms, n (%) | 16 (16) |
| LVH criteria, n (%) | 19 (19) |
| Heart rate (bpm) | 72 ± 12 |
| Antiarrhythmic medication, n (%) | 38 (38) |
| Beta-blockers | 35 (35) |
| Cordarone | 5 (5) |
| Flecaine | 2 (2) |
| Indication for beta-blockers, n = 35, n (%) | |
| Antianginal | 4 (11) |
| Atrial hyperexcitability or AF | 21 (58) |
| Ventricular hyperexcitability | 5 (14) |
| Dilated heart disease | 11 (31) |
| LV obstruction | 3 (8) |
| Arterial hypertension | 2 (5) |
| 24h-Holter results | |
| Ventricular data | |
| Total PVCs | 11 (0-259), (min 0; max 12 809) |
| PVCs > 500/24 h, n (%) | 15 (15) |
| NSVT (<30 sec), n (%) | 9 (9); range, 4-121 PVCs |
| SVT (≥30 sec), n (%) | 0 (0) |
| Patients with VA, n (%) | 22 (22) |
| Total PVCs (n = 22) | 984 (452-4035) |
| PVC > 1000 (n = 22), n (%) | 11 (50) |
| PVC > 10 000 (n = 22), n (%) | 3 (13) |
| Polymorphic trait (≥2 families) (n = 22) | 18 (82) |
| Daytime predominance (n = 22) | 20 (91) |
| Ventricular hyperexcitability under beta-blocker (n = 22) | 8 (36) |
| Atrial data | |
| Total PACs | 35 (5-254), (min 0; max 24 270) |
| PACs > 500/24 h, n (%) | 17 (17) |
| Atrial fibrillation, n (%) | 3 (3) |
Ordinal data are reported as mean ± standard deviation when they have a normal distribution, or as median (Q1-Q3) when they do not have a normal distribution, and nominal data as absolute value and percentage.
AF, atrial fibrillation; LVH, left ventricular hypertrophy; NSVT, nonsustained ventricular tachycardia; SVT, sustained ventricular tachycardia.
Among patients with VA, the median PVCs every 24 hours was 984 (452-4035), with 11 (50%) patients with a moderate PVC burden (>1000 every 24 hours) and 3 (13%) with a high PVC rate (>10 000 every 24 hours). PVCs were predominant during the day in most patients (91%) and mainly polymorphic (82%) (Table 2).
Determinants of VA in SCA—univariate analysis
Demographic characteristics of the patients with SCA with or without VA (n = 22 vs 78) are compared in Table 4. Patients with SCA exhibiting VA were predominantly male (81% vs 34%; P < .001), with a similar age. They had a higher diastolic blood pressure (81 ± 14 vs 75 ± 10 mmHg; P = .02) but no difference in terms of cardiovascular risk factors (Table 4). Regarding treatments, the 2 groups were highly comparable in terms of both antiarrhythmic medication and SCD management (hydroxyurea and erythrocytapheresis program). Notably, the corrected QT interval on the surface ECG was similar between the 2 groups (412 ± 29 ms vs 418 ± 26 ms; P = .35). Patients with VA had lower plasmatic platelet concentration (226 ± 96 vs 310 ± 130 giga per liter (G/L); P = .003) with no difference in hemoglobin or hemolysis markers. The proportion of patients with an NT pro-BNP ≥ 160 ng/L was higher in the group with VA (68% vs 44%; P = .047).
Univariate and multivariate analyses on primary end point
| Characteristics . | Ventricular hyperexcitability (n = 22) . | No ventricular hyperexcitability (n = 78) . | P in univariate . | P in multivariate . | OR (95% CI) . |
|---|---|---|---|---|---|
| Demographic and clinical | |||||
| Men | 18 (81) | 30 (34) | <.001 | .02 | 4.3(1.1-18.2) |
| Age (y) | 46.2 ± 11.6 | 46.1± 12.8 | .9 | ||
| Body mass index (kg/m2) | 22.6 ± 3.8 | 24.6 ± 4.4 | .053 | ||
| Systolic blood pressure (mmHg) | 134.6 ± 22.8 | 129.9 ± 16.1 | .3 | ||
| Diastolic blood pressure (mmHg) | 80.7 ± 13.7 | 74.5 ± 9.7 | .018 | .8 | |
| Heart rate (bpm) | 72 ± 14 | 72 ± 12 | .8 | ||
| Oxygen saturation (%) (n = 89) | 95 (93-97) | 95 (93-97) | .7 | ||
| Recurrent chest pain, n (%) | 5 (23) | 16 (21) | .8 | ||
| Dyspnea, n (%) | 9 (41) | 22 (28) | .1 | ||
| Daily palpitations, n (%) | 12 (54) | 27 (35) | .09 | ||
| Cardiovascular risk factors, n (%) | |||||
| Arterial hypertension | 14 (64) | 53 (60.2) | .7 | ||
| Diabetes | 0 | 4 (4.5) | .3 | ||
| Dyslipidemia | 1 | 0 | — | ||
| Obesity | 1 (4.5) | 6 (6.8) | .6 | ||
| Obstructive sleep apnea syndrome | 1 (4.5) | 10 (11.3) | .3 | ||
| Chronic kidney disease∗ | 10 (45) | 25 (32) | .2 | ||
| Active smoking | 3 (13.6) | 9 (10.2) | .8 | ||
| Thromboembolic history (PE/DVT) | 6 (27.2) | 22 (25) | .9 | ||
| Treatment of SCD, n (%) | |||||
| Hydroxyurea | 12 (54.5) | 49 (55.7) | .5 | ||
| Erythrocytapheresis | 0 (0) | 6 (6.8) | .2 | ||
| Hydroxyurea + erythrocytapheresis | 4 (18.2) | 17 (19.3) | .7 | ||
| Bloodletting | 0 (0) | 1 (1.1) | — | ||
| Biological characteristics | |||||
| Hemoglobin (g/dL) | 8.8 ± 1.7 | 8.6 ± 1.4 | .5 | ||
| Hemoglobin F under HU, % (n = 82) | 11.9 ± 9.3 | 13.4 ± 10.1 | .6 | ||
| Leukocytes (G/L) | 7.7 ± 2.5 | 7.8 ± 2.6 | .9 | ||
| Platelets (G/L) | 226 ± 96 | 316 ± 130 | .003 | .02 | 0.99(0.986-0.998) |
| Potassium (mmol/L) | 4.1 ± 0.5 | 4.3 ± 0.5 | .12 | ||
| Creatinine (μmol/L) | 84 (53-127) | 63 (52-88) | .9 | ||
| GFR (CKD-EPI, mL/min per 1.73 m2) | 94 (82-119) | 103 (86-119) | .6 | ||
| ASAT (IU/L) | 43 (34-59) | 45 (33-60) | .9 | ||
| ALAT (IU/L) | 23 (21-33) | 23 (18-37) | .8 | ||
| LDH (IU/L) | 433 (357-598) | 490 (367-600) | .8 | ||
| Total bilirubin (μmol/L) | 32 (22-33) | 29 (18-37) | .6 | ||
| Free bilirubin (μmol/L) | 25 (14-39) | 20 (18-46) | .8 | ||
| Nt Pro-BNP (ng/L) | 387 (85-626) | 142 (70-284) | .14 | ||
| Nt Pro-BNP ≥ 160 ng/L, n (%) | 15 (68) | 34 (44) | .047 | .08 | |
| Troponin T (Hs) (ng/L) | 7 (4-9) | 5 (3-10) | .9 | ||
| Echocardiography data | |||||
| LV function and remodeling | |||||
| LVEF in Simpson Biplane (%) | 56 ± 6.3 | 58.1 ± 5.6 | .13 | ||
| GLS (%) | −16.0 ± 1.9 | −18.3 ± 2.7 | <.001 | .02 | 1.4(1.02-1.9) |
| Cardiac output (L/min) | 6.4 ± 1.6 | 6.5 ± 1.7 | .8 | ||
| Indexed LV volume (mL/m2) | 94.7 ± 29.3 | 79.5 ± 19.3 | .01 | .5 | |
| Indexed LV mass (g/m2) | 128.4 ± 51.7 | 105.1 ± 31.3 | .02 | .8 | |
| Diastolic function | |||||
| E (cm/s) | 92 ± 23 | 85 ± 19 | .16 | ||
| EDT (ms) | 181 ± 36 | 195 ± 49 | .2 | ||
| A (cm/s) | 60 ± 20 | 64 ± 19 | .4 | ||
| E/A | 1.4 ± 0.5 | 1.7 ± 0.9 | .03 | .07 | |
| E' lateral (cm/s) | 12.5 ± 3.9 | 12.8 ± 3.7 | .8 | ||
| E/E' lateral | 8.4 ± 3.7 | 7.6 ± 2.6 | .3 | ||
| Indexed LA volume (mL/m2) | 60.3 ±25.9 | 56.4 ± 17.7 | .4 | ||
| RV function and right pressures | |||||
| TAPSE (mm) | 24 ± 5 | 26 ± 5 | .2 | ||
| S-wave (cm/s) | 14.7 ± 2.6 | 14.2 ± 1.8 | .4 | ||
| TRV (m/s) | 2.7 ± 0.3 | 2.6 ± 0.3 | .2 | ||
| TRV ≥ 3 m/s | 5 (23) | 13 (17) | .6 | ||
| Pulmonary acceleration time (ms) | 130 ± 33 | 134 ± 31 | .6 | ||
| Indexed tricuspid ring diameter (mm/m2) | 20.3 ± 2.5 | 19.1 ± 3.4 | .2 | ||
| RV end-diastolic area (cm2) | 22.2 ± 6.5 | 20.6 ±4.6 | .2 | ||
| Telesystolic area of the right atrium (cm2) | 21.5 ± 6.2 | 19.7 ± 5.1 | .2 | ||
| Systolic pulmonary arterial pressure (mmHg) | 35 ± 9.8 | 32 ± 8.2 | .12 | ||
| Right atrium pressure (mmHg) | 4.2 ± 2.8 | 4.3 ± 2.3 | .3 | ||
| Rhythmological characteristics | |||||
| Corrected QT on surface ECG (ms) | 412 ± 29 | 418 ± 26 | .4 | ||
| Corrected QT > 440 ms, n (%) | 3 (14) | 13 (17) | .7 | ||
| PR duration (ms) | 164 ± 22 | 168 ± 24 | .5 | ||
| QRS complex (ms) | 93 ± 18 | 91 ± 15 | .5 | ||
| LVH criteria, n (%) | 6 (27) | 13 (17) | .2 | ||
| Heart rate (bpm) | 71 ± 14 | 72 ± 12 | .8 | ||
| Antiarrhythmic treatment, n (%) | 8 (36) | 30 (34) | 0.8 | ||
| Beta-blockers | 8 (36) | 28 (32) | 0.9 | ||
| Cordarone | 0 | 1 | — | ||
| Flecaine | 0 | 1 | — | ||
| 24h-Holter results | |||||
| Atrial data | |||||
| Total PACs | 103 (19-542) | 31.5 (5-174) | .9 | ||
| Walking test data (n = 78) | |||||
| Test performed, n (%) | 18 (82) | 60 (68) | — | ||
| Walking distance (m) | 515 (415-560) | 475 (415-555) | .9 | ||
| Percentage of predicted distance (%) | 79 (66-84) | 77 (68-89) | .9 | ||
| Baseline saturation | 95 (93-97) | 95 (93-97) | .7 | ||
| Average saturation | 89 (84-92) | 91 (87-95) | .3 | ||
| Minimum saturation | 82 (69-87) | 86 (80-91) | .004 | ||
| Percentage of time spent <88% (%) | 23 (2-57) | 2 (0-58) | .09 |
| Characteristics . | Ventricular hyperexcitability (n = 22) . | No ventricular hyperexcitability (n = 78) . | P in univariate . | P in multivariate . | OR (95% CI) . |
|---|---|---|---|---|---|
| Demographic and clinical | |||||
| Men | 18 (81) | 30 (34) | <.001 | .02 | 4.3(1.1-18.2) |
| Age (y) | 46.2 ± 11.6 | 46.1± 12.8 | .9 | ||
| Body mass index (kg/m2) | 22.6 ± 3.8 | 24.6 ± 4.4 | .053 | ||
| Systolic blood pressure (mmHg) | 134.6 ± 22.8 | 129.9 ± 16.1 | .3 | ||
| Diastolic blood pressure (mmHg) | 80.7 ± 13.7 | 74.5 ± 9.7 | .018 | .8 | |
| Heart rate (bpm) | 72 ± 14 | 72 ± 12 | .8 | ||
| Oxygen saturation (%) (n = 89) | 95 (93-97) | 95 (93-97) | .7 | ||
| Recurrent chest pain, n (%) | 5 (23) | 16 (21) | .8 | ||
| Dyspnea, n (%) | 9 (41) | 22 (28) | .1 | ||
| Daily palpitations, n (%) | 12 (54) | 27 (35) | .09 | ||
| Cardiovascular risk factors, n (%) | |||||
| Arterial hypertension | 14 (64) | 53 (60.2) | .7 | ||
| Diabetes | 0 | 4 (4.5) | .3 | ||
| Dyslipidemia | 1 | 0 | — | ||
| Obesity | 1 (4.5) | 6 (6.8) | .6 | ||
| Obstructive sleep apnea syndrome | 1 (4.5) | 10 (11.3) | .3 | ||
| Chronic kidney disease∗ | 10 (45) | 25 (32) | .2 | ||
| Active smoking | 3 (13.6) | 9 (10.2) | .8 | ||
| Thromboembolic history (PE/DVT) | 6 (27.2) | 22 (25) | .9 | ||
| Treatment of SCD, n (%) | |||||
| Hydroxyurea | 12 (54.5) | 49 (55.7) | .5 | ||
| Erythrocytapheresis | 0 (0) | 6 (6.8) | .2 | ||
| Hydroxyurea + erythrocytapheresis | 4 (18.2) | 17 (19.3) | .7 | ||
| Bloodletting | 0 (0) | 1 (1.1) | — | ||
| Biological characteristics | |||||
| Hemoglobin (g/dL) | 8.8 ± 1.7 | 8.6 ± 1.4 | .5 | ||
| Hemoglobin F under HU, % (n = 82) | 11.9 ± 9.3 | 13.4 ± 10.1 | .6 | ||
| Leukocytes (G/L) | 7.7 ± 2.5 | 7.8 ± 2.6 | .9 | ||
| Platelets (G/L) | 226 ± 96 | 316 ± 130 | .003 | .02 | 0.99(0.986-0.998) |
| Potassium (mmol/L) | 4.1 ± 0.5 | 4.3 ± 0.5 | .12 | ||
| Creatinine (μmol/L) | 84 (53-127) | 63 (52-88) | .9 | ||
| GFR (CKD-EPI, mL/min per 1.73 m2) | 94 (82-119) | 103 (86-119) | .6 | ||
| ASAT (IU/L) | 43 (34-59) | 45 (33-60) | .9 | ||
| ALAT (IU/L) | 23 (21-33) | 23 (18-37) | .8 | ||
| LDH (IU/L) | 433 (357-598) | 490 (367-600) | .8 | ||
| Total bilirubin (μmol/L) | 32 (22-33) | 29 (18-37) | .6 | ||
| Free bilirubin (μmol/L) | 25 (14-39) | 20 (18-46) | .8 | ||
| Nt Pro-BNP (ng/L) | 387 (85-626) | 142 (70-284) | .14 | ||
| Nt Pro-BNP ≥ 160 ng/L, n (%) | 15 (68) | 34 (44) | .047 | .08 | |
| Troponin T (Hs) (ng/L) | 7 (4-9) | 5 (3-10) | .9 | ||
| Echocardiography data | |||||
| LV function and remodeling | |||||
| LVEF in Simpson Biplane (%) | 56 ± 6.3 | 58.1 ± 5.6 | .13 | ||
| GLS (%) | −16.0 ± 1.9 | −18.3 ± 2.7 | <.001 | .02 | 1.4(1.02-1.9) |
| Cardiac output (L/min) | 6.4 ± 1.6 | 6.5 ± 1.7 | .8 | ||
| Indexed LV volume (mL/m2) | 94.7 ± 29.3 | 79.5 ± 19.3 | .01 | .5 | |
| Indexed LV mass (g/m2) | 128.4 ± 51.7 | 105.1 ± 31.3 | .02 | .8 | |
| Diastolic function | |||||
| E (cm/s) | 92 ± 23 | 85 ± 19 | .16 | ||
| EDT (ms) | 181 ± 36 | 195 ± 49 | .2 | ||
| A (cm/s) | 60 ± 20 | 64 ± 19 | .4 | ||
| E/A | 1.4 ± 0.5 | 1.7 ± 0.9 | .03 | .07 | |
| E' lateral (cm/s) | 12.5 ± 3.9 | 12.8 ± 3.7 | .8 | ||
| E/E' lateral | 8.4 ± 3.7 | 7.6 ± 2.6 | .3 | ||
| Indexed LA volume (mL/m2) | 60.3 ±25.9 | 56.4 ± 17.7 | .4 | ||
| RV function and right pressures | |||||
| TAPSE (mm) | 24 ± 5 | 26 ± 5 | .2 | ||
| S-wave (cm/s) | 14.7 ± 2.6 | 14.2 ± 1.8 | .4 | ||
| TRV (m/s) | 2.7 ± 0.3 | 2.6 ± 0.3 | .2 | ||
| TRV ≥ 3 m/s | 5 (23) | 13 (17) | .6 | ||
| Pulmonary acceleration time (ms) | 130 ± 33 | 134 ± 31 | .6 | ||
| Indexed tricuspid ring diameter (mm/m2) | 20.3 ± 2.5 | 19.1 ± 3.4 | .2 | ||
| RV end-diastolic area (cm2) | 22.2 ± 6.5 | 20.6 ±4.6 | .2 | ||
| Telesystolic area of the right atrium (cm2) | 21.5 ± 6.2 | 19.7 ± 5.1 | .2 | ||
| Systolic pulmonary arterial pressure (mmHg) | 35 ± 9.8 | 32 ± 8.2 | .12 | ||
| Right atrium pressure (mmHg) | 4.2 ± 2.8 | 4.3 ± 2.3 | .3 | ||
| Rhythmological characteristics | |||||
| Corrected QT on surface ECG (ms) | 412 ± 29 | 418 ± 26 | .4 | ||
| Corrected QT > 440 ms, n (%) | 3 (14) | 13 (17) | .7 | ||
| PR duration (ms) | 164 ± 22 | 168 ± 24 | .5 | ||
| QRS complex (ms) | 93 ± 18 | 91 ± 15 | .5 | ||
| LVH criteria, n (%) | 6 (27) | 13 (17) | .2 | ||
| Heart rate (bpm) | 71 ± 14 | 72 ± 12 | .8 | ||
| Antiarrhythmic treatment, n (%) | 8 (36) | 30 (34) | 0.8 | ||
| Beta-blockers | 8 (36) | 28 (32) | 0.9 | ||
| Cordarone | 0 | 1 | — | ||
| Flecaine | 0 | 1 | — | ||
| 24h-Holter results | |||||
| Atrial data | |||||
| Total PACs | 103 (19-542) | 31.5 (5-174) | .9 | ||
| Walking test data (n = 78) | |||||
| Test performed, n (%) | 18 (82) | 60 (68) | — | ||
| Walking distance (m) | 515 (415-560) | 475 (415-555) | .9 | ||
| Percentage of predicted distance (%) | 79 (66-84) | 77 (68-89) | .9 | ||
| Baseline saturation | 95 (93-97) | 95 (93-97) | .7 | ||
| Average saturation | 89 (84-92) | 91 (87-95) | .3 | ||
| Minimum saturation | 82 (69-87) | 86 (80-91) | .004 | ||
| Percentage of time spent <88% (%) | 23 (2-57) | 2 (0-58) | .09 |
Univariate analyses used the analysis of variance test for quantitative variables and the χ2 test for qualitative variables. A significance level P ≤ .05 was considered statistically significant. Multivariate analysis was performed using binary logistic regression on univariate significant values (in bold): they appear in red when statistically significant (P < .05) and the OR is then indicated with the 95% CI. Values in boldface denote significant P values in univariate analysis.
GFR < 90 mL/min per 1.73m2 according to CKD-EPI.
Interestingly, despite normal LVEF and no argument for a major increase in LV filling pressures, echocardiography showed reduced GLS (–16.0% ± 1.9% vs –18.3% ± 2.7%; P < .001), higher LVEDVind (95 ± 29 vs 80 ± 19 mL/m2; P = .01), and LVMind (128 ± 52 vs 105 ± 31 g/m2; P = .02) in patients with VA (Table 4). Regarding diastolic function, only E/A ratio was slightly lower in patients with VA (1.4 ± 0.5 vs 1.7 ± 0.9; P = .03). TRV was similar in the 2 groups (2.78 ± 0.3 vs 2.68 ± 0.3; P = .2). Notably, among the 6 patients who had subendocardial ischemia during the stress test, only 1 exhibited VA.
Among patients who could perform the 6-minute walking test (n = 78), a lower minimal oxygen saturation (82 [69-87] vs 86% [80-91]; P = .004) and a trend of spending more time below 88% saturation during the test (23 [2-57] vs 2% [0-58]; P = .09) were found in patients with VA.
Furthermore, to assess whether a higher PVC burden was associated with clinical, biological, and echocardiographic parameters, we performed the same analysis comparing patients with more than 1000 PVCs every 24 hours (n = 11) with the others. Platelet count, male sex, GLS value, and E/A ratio were identified using univariate analysis (data not shown).
Determinants of VA in SCA—multivariate analysis
Gender, diastolic blood pressure, platelet count, NT pro-BNP ≥160 ng/L, GLS, LVEDVind, LVMind, and E/A ratio were entered into multivariate analysis (Table 3). Male sex (OR, 4.3 [95% CI, 1.1-18.2]; P = .02), alteration of GLS (OR, 1.4 [95% CI, 1.02-1.9]; P = .02) and decreased platelet count (OR, 0.99 [95% CI, 0.986-0.998]; P = .02) were independently associated with VA. The PVC load every 24 hours was correlated with GLS (correlation coefficient [R] = 0.39; P < .001) and platelet count (R = –0.26; P = .004), Figure 1. GLS showed good accuracy in identifying patients with VA (AUC = 0.76 [0.66-086]), with an optimal cutoff of −17.5% (sensitivity = 82%, specificity = 63%, positive predictive value = 38%, negative predictive value = 92%) (Figure 1).
Predictors of ventricular arrhythmia in SCA patients. Correlation between PVCs (logarithmic scale) and GLS (A) and platelet count (B). Receiver operating characteristic curves of GLS for identifying VA and determination of the optimal threshold (with the best sensitivity and specificity) (C). NPV, negative predictive value; PPV, positive predictive value; Se, sensitivity; Sp, specificity.
Predictors of ventricular arrhythmia in SCA patients. Correlation between PVCs (logarithmic scale) and GLS (A) and platelet count (B). Receiver operating characteristic curves of GLS for identifying VA and determination of the optimal threshold (with the best sensitivity and specificity) (C). NPV, negative predictive value; PPV, positive predictive value; Se, sensitivity; Sp, specificity.
Differences related to sex in the study population
Given the gender distribution of VAs in our study population, demographic differences by sex are reported in supplemental Table 2. Briefly, men were younger (43 ± 12 years vs 49 ± 12 years; P = .03) and had higher blood pressure. Men had a higher hemoglobin level (9.1 ± 1.3 vs 8.3 ± 1.3 g/dL; P = .005) and more impaired systolic function parameters on echocardiography (LVEF and GLS). Notably, men and women were comparable in terms of corrected QT on surface ECG, cardiovascular risk factors, antiarrhythmic medications, and specific SCA therapies.
Discussion
In this pilot study, we explored for the first time ventricular rhythmic abnormalities in patients with SCA in an integrative way, combining clinical, biological, and echocardiographic evaluation concomitantly with 24h-Holter. Our results underline the high prevalence of VA in SCA and its association with male gender, reduced GLS on echocardiography, and lower platelet count. These preliminary data are important because they shed new light on a crucial and dramatic complication in patients with SCA and open new avenues for larger observational studies before randomized clinical trials.
A high prevalence of VA in patients with SCA
The first main finding of this study was the high prevalence of VA (22%) in this population with SCA, of which 64% had at least a moderate PVC load and 41% exhibited nonsustained VT. These results are in line with recent preclinical data on SCD mice developing cardiomyopathy, which results in a predisposition to inducible VT. This electrical phenotype is associated with increased interleukin-18 and myocardial fibrosis, increasing the propensity for VAs.24 In contrast to previous studies, QT interval duration was not associated with VA, a discrepancy that may be explained by the use of antiarrhythmic drugs in the study population, which are known to interfere with QT interval.7,35 To our knowledge, we are the first to report and document such arrhythmia in clinical practice in a well-phenotyped cohort of patients with SCA, unmasking the fact that VAs are probably largely underestimated in this population.
The presence of frequent PVCs has been associated with the risk of sudden death and cardiovascular mortality in the population with non-SCD.30,36 This risk is greatly magnified by the PVC load per 24 hours and the presence of a structural heart disease, such as ischemic or hypertrophic cardiomyopathy.37,38 In addition, polymorphic morphology, suggesting multiple abnormal foci or multiple exit points from a reentrant circuit, and the occurrence of nonsustained VT have also been linked to higher mortality and heart failure rate in the population with non-SCD.39,40 With “sudden death” characterized as one of the top causes of death in SCA (about 20%8), it is likely that a significant portion is attributable to severe ventricular rhythm disorders.22,24 In line with this, it is of particular interest that more patients with VA had an NT pro-BNP ≥ 160 ng/L (68% vs 44%; P = .047), a previously reported mortality risk factor in SCD.41,42 One could hypothesize that myocardial ischemia, hypoxemia, acidosis, or hydroelectricity disorders along with diffuse myocardial fibrosis could act as arrhythmogenic triggers in patients with SCA.14,17,24,43 Consistent with this, it is interesting to observe that patients with VA mainly had electrical abnormalities during the day (possibly related to physical activities of daily living) and had deeper and sustained oxygen desaturations during the walking test.44 Notably, we ruled out the presence of myocardial ischemia due to epicardial coronary artery disease in all patients undergoing coronary testing (60% of the cohort and 59% of the patients with VA).29
Patients with SCA presenting with VA did not demonstrate the usual combination of factors suggesting poor cardiovascular prognosis typically described in SCD (ie, age, elevated TRV, pulmonary hypertension, or systemic hypertension), apart from the elevation of NT pro-BNP.45,46 We have described a new cluster of cardiac parameters that may predict cardiac risk. Our current data advocate for a broader screening of ventricular arrhythmias in patients with SCA for the early detection of patients at risk and may suggest preventive therapies.
LV global longitudinal strain as a good tool for rhythmic risk stratification
We then focused on potential cardiac remodeling and LV dysfunction because we did not find any argument for underlying coronary artery disease. By combining advanced echocardiography including speckle tracking imaging on the same day as 24h-Holter, our study identified GLS as a promising tool to optimize the stratification of the risk of VA in patients with SCA. Indeed, a cutoff value of GLS at –17.5% had an interesting negative and positive predictive values of 92% and 38%, respectively. Notably, GLS was slightly impaired in the whole population (–17.9%), a value similar to previous reports on SCA, providing some external validity to our results.47 Evidence gathered over the last decade has shown that GLS is more sensitive to left ventricular dysfunction than LVEF and our group has identified GLS to provide additional prognostic information in various cardiomyopathy etiologies, including incipiens diabetic cardiomyopathy.48,49 This technology is now standardized, well validated, reproducible, and widely available.50 Such a GLS alteration in patients with SCA might reflect the onset of myocardial fibrosis, which has already been associated with VAs in other structural heart diseases.51-53 Previous studies have demonstrated that GLS correlates with myocardial fibrosis on histology,54 MRI,55 and myocardial fibrosis biomarkers in different pathological settings.48,56,57 In line with this, in patients with VA, we uncovered worse LV remodeling and a slightly lower E/A ratio, hallmarks of myocardial fibrosis, and diastolic dysfunction that have previously been associated with early mortality in SCA.4,5,14 Nevertheless, these findings must be interpreted cautiously, because a high load of PVCs alone may per se contribute to LV systolic dysfunction.58 However, we are alerted by preliminary observations from the follow-up of a few patients in whom a sharp decrease in GLS values over time was associated with the onset of VA and even more with sudden cardiac death (unpublished data). This emphasizes that the follow-up of patients with SCA with any cardiac disorder is crucial to refine the prognostic role of the deterioration of GLS in predicting VA and sudden cardiac death. Furthermore, our data advocate for a tight collaboration between the hematologists in charge of patients with SCA and well-trained cardiologists aware of the specificity of cardiac function in this setting.
VA is associated with lower platelet count
In our study, a decrease in plasma platelet count was independently associated with VA. Little data exist on this topic, but in severe sickle cell crisis, thrombocytopenia is more common than thrombocytosis, and platelet counts correlate inversely with prognosis.59 The pathogenesis of thrombocytopenia may be linked to compromised marrow function or platelet consumption; however, these data cannot be extrapolated to our stable study population. Moreover, it is interesting to note that activation of platelets is known to be associated with the secretion of potential arrhythmic factors such as serotonin, histamine, purines, pyrimidines, calcium, and magnesium.60 However, given the high prevalence of treatment interfering with thrombocytopoiesis (such as hydroxyurea or blood exchange) in our study, these results should be interpreted cautiously and explored in dedicated analyses.
Gender distribution of VA
A striking finding of this study was the gender distribution of the VAs in patients with SCA. This disorder affected men 4.3 times more than women, despite a younger age, a higher hemoglobin level, and no differences in terms of antiarrhythmic treatments or SCA specific therapies. There is increasing evidence that men and women have different cardiac remodeling in chronic conditions, particularly in terms of myocardial fibrosis.61 This observation was already shared by our team in the context of SCA, as men showed greater myocardial remodeling on echocardiography.5 In our study, men had more remodeled hearts and poorer systolic function parameters, notably GLS, which could indicate greater fibrosis.51 In the general population, this differential susceptibility to ventricular hyperexcitability and the incidence of sudden cardiac death between men and women has been well described and observed in different structural heart diseases.62 For example, numerous observational studies have shown that women with coronary artery disease have less frequent VAs than men, suggesting a gender-related protective effect.63 The relative protection of women is probably related to the cardioprotective effects of estrogen, especially in young nonmenopausal women with SCA, and is essentially mediated by the estrogen receptor beta, which has known antiinflammatory and antifibrotic effect on cardiomyocytes and endothelial cells.64 To date, preclinical studies that investigated VAs in murine SCD models have been conducted exclusively in male animals. Future studies should consider this gender difference to better understand the underlying mechanisms of innate protection in SCA.
Limitations
We are aware that this was a pilot study and thus underpowered, with ventricular arrhythmia occurring in only 22 patients. Nevertheless, this is the largest prospective cohort of patients with SCA who underwent deep cardiac phenotyping combining systematic arrhythmia monitoring and cardiac imaging. This population study is biased because patients were selected based on clinical criteria indicative of underlying cardiovascular abnormalities and therefore do not reflect patients with SCA in general. In addition, the population was relatively old for SCA (46 years), heterogeneous in terms of antiarrhythmic therapies, and overall, at an advanced stage of the disease, with frequent organ complications. Although the age and severity of these patients might overestimate the incidence of ventricular arrhythmias, the use of antiarrhythmic treatment could also blunt it. Thus, we are cautious in extending our data to all patients with SCA and are convinced that future studies should include younger patients at lower risk. Meanwhile, because medical advances have considerably improved the prognosis of homozygous SCA, physicians will increasingly encounter this type of patients, who are older with more comorbidities. Therefore, physicians must be familiar with their high rhythmic risk. Finally, >80% of the study population receiving specific SCA therapies, which are known to have major and heterogeneous consequences on hematological laboratory data. This renders the interpretation of hematological data difficult and could mask differences between the 2 groups.
Perspectives
This pilot study highlights the need to improve the detection of patients with SCA at risk of ventricular arrhythmia, a population for which most deaths are attributable to sudden cardiac death. Our results emphasize the need to study these patients more broadly using longer duration ECG monitoring, including implantable loop recorders to evaluate its impact on prognosis. The use of other tools, such as signal-averaged ECG or cardiac MRI, with the quantification of fibrosis using multiparametric mapping could have an additional interest in the identification of patients at risk and will require dedicated investigations.14,65 The objective would be to refine the stratification of a population at high rhythmic risk to early initiate and evaluate preventive antiarrhythmic strategies (medication, ablation procedure, or implantable defibrillator) or targeted therapy (ie, interleukin-18 inhibitors) in a manner similar to that for hypertrophic heart disease,24,66 ultimately leading to better prevention of sudden cardiac death.
Conclusion
Ventricular arrhythmias are very common in patients with SCA, particularly in men, and the measurement of LV GLS using echocardiography appears to be a promising tool for risk stratification. This pilot study paves the way for a new era in the screening of rhythmic disorders in patients with SCA and highlights the crucial need to refine the risk stratification and develop appropriate antiarrhythmic strategies.
Acknowledgment
This work was supported by a grant from the FHU-SENEC (allocation number RSE20003DDA).
Authorship
Contribution: T.d’H., J.S., L.S., and M.D. designed and wrote the manuscript; L.B., H.G., L.A., G.d.L., S.I., A.L.P.H.d’A.d’O., Y.Z., N.B., Y.P., and L.M. performed the research and reviewed the manuscript; E.A. and T.d’H. analyzed the data; H.D., A.H., N.L., and G.D. performed the research, contributed to the design plan, and reviewed the manuscript; and P.B. designed the research and wrote the manuscript.
Conflict-of-interest disclosure: P.B. received grants from addmedica, Fabre Foundation, Novartis, and bluebird bio in the past 36 months; consulting fees from addmedica, Novartis, Roche, GBT Pharma, bluebird bio, Emmaus, Hemanext, Agios; and honoraria for lectures from Novartis, addmedica, and Jazz Pharma; and is a member of the Novartis steering committee and a cofounder of Innovhem. The remaining authors declare no competing financial interests.
Correspondence: Thomas d’Humières, Department of Physiology, Henri Mondor University Hospital, Assistance Publique Hôpitaux de Paris, 51 Ave du Maréchal de Lattre de Tassigny, 94010 Créteil, France; e-mail: thomas.dhumieres@aphp.fr.
References
Author notes
∗T.d’H., J.S., G.D., and P.B. contributed equally to this study.
Data are available on request from the corresponding author, Thomas d’Humières (thomas.dhumieres@aphp.fr).
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal