Abstract
Allogeneic hematopoietic stem cell transplantation (alloHSCT) is a potentially curative treatment for patients with high-risk acute leukemias, but unfortunately disease recurrence remains the major cause of death in these patients. Infusion of donor lymphocytes (DLI) has the potential to restore graft-versus-leukemia immunologic surveillance; however, efficacy varies across different hematologic entities. Although relapsed chronic myeloid leukemia, transplanted in chronic phase, has proven remarkably susceptible to DLI, response rates are more modest for relapsed acute myeloid leukemia and acute lymphoblastic leukemia. To prevent impending relapse, a number of groups have explored administering DLI preemptively on detection of measurable residual disease (MRD) or mixed chimerism. Evidence for the effectiveness of this strategy, although encouraging, comes from only a few, mostly single-center retrospective, nonrandomized studies. This article seeks to (1) discuss the available evidence supporting this approach while highlighting some of the inherent challenges of MRD-triggered treatment decisions post-transplant, (2) portray other forms of postremission cellular therapies, including the role of next-generation target-specific immunotherapies, and (3) provide a practical framework to support clinicians in their decision-making process when considering preemptive cellular therapy for this difficult-to-treat patient population.
Introduction
Allogeneic hematopoietic stem cell transplantation (alloHSCT) is a potentially curative treatment for acute leukemias. However, relapse is the major cause of death in this patient population. Second alloHSCT and infusion of donor lymphocytes (DLI) represent the only established treatment options with the potential for cure. Unfortunately, both measures convey equally disappointing results with long-term survival of 5% to 20%1-5.
The concept of DLI was introduced in the early 1990s6,7 to enhance the immunological graft-versus-leukemia (GvL) effect, driven in part by restoration of T-cell immunity and reversal of T-cell exhaustion in resident CD8+ T cells.8 Response to DLI, however, varies dramatically depending on the underlying disease. Relapsed chronic myeloid leukemia (CML), when transplanted in chronic phase, proved particularly susceptible to DLI, with response rates of 70% to 80%.7,9 For patients transplanted in the accelerated phase, response rates dropped to ∼40%, and those transplanted in blast crisis were resistant to DLI in an early seminal study.7 Relapsed acute myeloid leukemia (AML), similarly, is disproportionally more resistant than chronic-phase CML, with response rates of 30% to 40%.7,10 DLI performs even worse in the context of relapsed acute lymphoblastic leukemia (ALL), with remissions of less than 15%.7,11
In this article, we will discuss the available clinical evidence on the different cellular strategies pursued to treat and prevent relapse of high-risk AML after alloHSCT. Although others have comprehensively reviewed the evolution of cell therapy,12,13 this article will place an emphasis on how these strategies have been applied in the posttransplant setting. We will conclude with our institutional perspective on how to manage this hard-to-treat patient population. Although the primary focus of this article will be on AML, we will introduce seminal work conducted in the context of CD19+ lymphoid malignancies when it has been instrumental in driving forward innovations for the treatment of AML.
What is the role of preemptive cellular therapy after allogeneic transplant?
Given the limited efficacy of DLI at overt relapse, several groups have explored administering DLI earlier when disease burden is lower. Prophylactic and preemptive DLI both aim to augment the GvL effect before overt hematologic relapse. Figure 1 provides an overview of the different strategies pursued to refine DLI treatment.
Overview of different strategies to administer DLI. (1) Prophylactic DLI is administered after a defined interval posttransplant to reduce the risk of relapse. (2) Preemptive DLI serves to restore GvL on impending relapse as detected by persisting MRD or LOC. (3) Therapeutic DLI is administered to treat overt hematologic relapse. Abbreviations: DLI, donor lymphocyte infusion; GvL, graft-versus-leukemia effect; LOC, loss of complete donor chimerism; MRD, measurable residual disease. Image created in BioRender.
Overview of different strategies to administer DLI. (1) Prophylactic DLI is administered after a defined interval posttransplant to reduce the risk of relapse. (2) Preemptive DLI serves to restore GvL on impending relapse as detected by persisting MRD or LOC. (3) Therapeutic DLI is administered to treat overt hematologic relapse. Abbreviations: DLI, donor lymphocyte infusion; GvL, graft-versus-leukemia effect; LOC, loss of complete donor chimerism; MRD, measurable residual disease. Image created in BioRender.
Prophylactic DLI is administered to patients at high risk for relapse at a defined interval posttransplant to prevent disease recurrence. Identification of high-risk patients is based on pretransplant clinical features (unfavorable cytogenetics, chemo-refractory disease, remission status including measurable residual disease [MRD] at time of transplant), transplant-associated factors (use of anti-T-cell antibodies, T cell-depleted grafts, reduced-intensity conditioning [RIC] regimens, recipients of bone marrow grafts) and posttransplant considerations (graft-versus-host disease [GvHD], uncontrolled infections).14-19
Preemptive DLI aims to combat impending relapse triggered either by detection of MRD or loss of complete donor chimerism (LOC).20-31,34,35
Both strategies need to be carefully weighed against potential toxicity, especially acute and chronic GvHD, which may occur in up to 12% and 31%, respectively.32-34
What is the clinical evidence to support preemptive DLI?
The evidence for preemptive DLI comes from a handful of mostly single-center, nonrandomized studies20-31,34,35 (Table 1) that encompass a broad range of different disease entities including AML but also spanning aggressive lymphatic malignancies, making interpretation of their results challenging. In 2007, Dominietto et al investigated preemptive DLI on detection of MRD after alloHSCT in patients with AML and ALL. The risk of relapse was reduced (6% vs 63%) and 3-year overall survival (OS) improved (80% vs 26%) compared with no intervention.20 Of note, this was a retrospective study and the non-DLI arm was composed only of patients ineligible for DLI because of uncontrolled GvHD, absence of a potential donor, or evidence of overt relapse, thus limiting any definitive conclusions. In a follow-up study, improved response rates (45% vs 33%) and prolonged 2-year survival (43% vs 19%) were reported when DLI was administered at the time of molecular relapse instead of overt relapse.26 Moreover, patients with relapsed/refractory (R/R) AML positive for Wilms’ tumor protein (WT1-MRD+) who received DLI at a lower cutoff threshold (100 WT1 copies/104ABL) fared significantly better than those with a higher threshold of 180 WT1 copies/104ABL (cumulative incidence of relapse [CIR]: 29% vs 76%; leukemia-free survival at 4 years: 74% vs 23%), underscoring the notion that DLI may be more effective at a time of lower disease burden.35
Overview of studies evaluating preemptive DLI
| Reference . | Study design . | Disease . | Graft type, conditioning regimen, donor source, GvHD prophylaxis . | Trigger . | Cell dose . | Study arms compared . | Efficacy outcomes . | Grade III/IV GvHD . |
|---|---|---|---|---|---|---|---|---|
| 20 | Prospective, nonrandomized | AML (n = 36), ALL (n = 44) | NR | MRD | Starting CD3 dose Matched related: 1 × 106/kg MUD/MMUD: 1 × 105/kg | Preemptive DLI vs no DLI | CIR: 6% 3-y OS: 80% —— CIR: 63% 3-y OS: 26% | NR |
| 21 | Case report | AML (n = 1) | NR | MRD, MC | Not reported | Single case report | Conversion to MRD negativity | NR |
| 22 | Prospective, nonrandomized | AML (n = 61) ALL (n = 38) MDS (n = 6) Total n = 105 | T cell-replete MAC-BM/PBSC-alloHSCT Conditioning regimens/donor source: matched related (n = 40): Bu/Cy or Cy/TBI Haplo (n = 53) and MUD (n = 12): Bu/Cy + ATG or Cy/TBI + ATG GvHD prophylaxis: CSA, MMF, MTX (± ATG) | MRD | Median CD3 dose: 3.8 × 107/kg | Preemptive DLI (n = 56) vs IL-2 (n = 49) | CIR: 28% 3-y OS: 58% 3-y DFS: 56% —— CIR: 64% 3-y OS: 28% 3-y DFS: 24% | 8% (P = .471) —— 4% |
| 30 | Retrospective | AML (n = 14) ALL (n = 11) CML (n = 2) | T cell-replete MAC-PBSC-alloHSCT Conditioning regimens/donor source: matched related (n = 14): Bu/Cy Haplo (n = 2) and MUD (n = 11): Bu/Cy + ATG + cytarabine GvHD prophylaxis: CSA, MMF, MTX (± ATG) | MRD | Median CD3 dose: 5.51 × 107/kg | Preemptive DLI vs Therapeutic DLI | 1-y OS: 94% —— 1-y OS: 27% | 6% —— 9% |
| 24 | Prospective, nonrandomized phase 2 trial | AML (n = 14) MDS (n = 4) MPN (n = 2) Others (n = 16) | T cell-replete low-dose alemtuzumab RIC-PBSC-alloHSCT Conditioning regimens: Myeloid: Flu/Bu Lymphoid: Flu/Cy (± rituximab) Donor source: MUD: 33 MMUD: 3 GvHD prophylaxis: Tacrolimus, MTX, alemtuzumab | MC (<50% at d+60) | Starting CD3 dose: 0.5–1.0 × 107/kg | Preemptive DLI | 2-y OS: 57%; 2-y DFS: 38%; 1-y NRM: 14% | 0% |
| 25 | Retrospective | AML (n = 16) NHL (n = 6) HL (n = 5) MM (n = 4) ALL (n = 3) Others (n = 6) | T cell-replete HLA-haplo-BM-alloHSCT Conditioning regimens: MAC (n = 6): Bu/Cy RIC (n = 34): Flu/Cy/TBI Donor source: Haplo (n = 40) GvHD prophylaxis: Tacrolimus, MMF, PTCy | MRD, LOC | Starting CD3 dose 1 × 105/kg-1 × 106/kg | Preemptive DLI (n = 5) vs Therapeutic DLI (n = 35) | ORR: 60% —— ORR: 26% | NR |
| 23 | Prospective, nonrandomized | AML (n = 17) | T cell-replete BM/PBSC-MAC-alloHSCT Conditioning regimens/donor source: matched related (n = 43): Bu/Cy or Cy/TBI Haplo (n = 44) and MUD (n = 5): Bu/Cy + ATG or Cy/TBI + ATG GvHD prophylaxis: CSA, MMF, MTX (± ATG) | MRD | NR | Preemptive DLI vs No DLI | 2-y CIR: 24% 2-y OS: 64% —— 2-y CIR: 84% 2-y OS: 0% | NR |
| 26 | Retrospective | AML (n = 22) ALL (n = 9) MM (n = 1) | T cell-replete HLA-haplo-MAC-BM-alloHSCT Conditioning regimens: Flu/Bu/TT Flu/TBI Donor source: Haplo (n = 32) GvHD prophylaxis: CSA, MMF, PTCy | MRD | Starting CD3 dose 1 × 104/kg-1 × 105/kg | Preemptive DLI vs Therapeutic DLI | ORR: 45% 2-y OS: 43% —— ORR: 33% 2-y OS: 19% | 5% —— 8% |
| 35 | Retrospective | AML (n = 207) | T cell-replete MAC-BM/PBSC/CB-alloHSCT Conditioning regimens: Bu/Flu (+TT), Bu/Cy, Cy/Mel/TT Cy/TT, Cy/TBI Donor source: Matched related (n = 82) MUD (n = 66) Haplo (n = 59) GvHD prophylaxis: CSA, MTX | MRD | Starting CD3 dose: Matched-sibling: 1 × 106/kg MUD: 1 × 105/kg; HaploDLI: 1 × 104/kg | WT1 100 copies/104 ABL vs WT1 180 copies/104 ABL | CIR: 29% 4-y LFS 74% —— CIR: 76% 4-y LFS: 23% | 0% 0% |
| 31 | Retrospective | AML (n = 31) NHL (n = 19) MDS (n = 8) Others (n = 28) | T cell-replete BM/PBSC-MAC/RIC-alloHSCT Conditioning regimens: RIC (n = 60): Flu, Mel, Alemtuzumab MAC (n = 26): Bu/Cy, Bu/Flu, TBI/Cy, TBI/Cy/VP Donor sources: Matched related (n = 53) MUD (n = 25) MMUD (n = 8) GvHD prophylaxis: Not reported for MAC; alemtuzumab for RIC | MC | Starting CD3 dose: Matched-sibling: 3 × 106-1 × 107/kg MUD: 1-3 × 106/kg | Preemptive DLI vs Therapeutic DLI | 5-y OS: 69% 5-y PFS: 71% —— 5-y OS: 28% 5-y PFS: 18% | 26% —— 31% |
| 28 | Retrospective | AML (n = 14) MDS (n = 20 ALL/NHL (n = 5) CML (n = 2) | T-cell replete PB-haploHCT Conditioning regimens: MAC (n = 8) RIC (n = 13) Donor source: Haplo (n = 21) GvHD prophylaxis: tacrolimus, MMF/ sirolimus, MMF, PTCy | MC | Most common starting CD3 dose: 1 × 106/kg | Preemptive DLI (n = 2) vs Therapeutic DLI (n = 12) | 120-d OS: 100% —— 120-d OS: 29% | NR |
| 27 | Retrospective, matched-pair analysis | AML, MDS, ALL (n = 20) | T cell-replete BM/PBSC-MAC-alloHSCT Conditioning regimens/donor source: matched related (n = 8): Bu/Cy Haplo (n = 12): Bu/Cy + cytarabine + ATG GvHD prophylaxis: CSA, MMF, MTX | MRD | Median CD3 dose: 2.5 × 107/kg | No control | MRD conversion: 75%; 2-y CIR 31%; 2-y OS 69% | Grade II-IV aGvHD: 4 (20%) |
| 29 | Retrospective single-center landmark analysis | AML (n = 42) | T cell-replete PBSC-MAC/RIC-alloHSCT Conditioning regimens: MAC (n = 12): Bu/Cy, TT/Bu/Flu RIC (n = 30): Flu/BCNU/Mel, Flu/TT Donor source: matched related (n = 11) MUD (n = 23) MMUD (n = 7) Haplo (n = 1) GvHD prophylaxis: CSA/Alemtuzumab, CSA/MMF, MTX ± ATG | MRD (n = 18) MC (n = 24) | Median starting CD3 dose: 0.69 × 106/kg | Preemptive DLI vs Therapeutic DLI | 5-y OS: 43% —— 5-y OS: 10% | 7% —— 6% |
| 34 | Retrospective registry study | AML (n = 153) ALL (n = 39) | BM/PBSC-MAC /RIC-alloHSCT with (n = 149) and without (n = 42) T-cell depletion Conditioning regimens: MAC (n = 74) RIC (n = 107) Donor source: Matched related (n = 129) MUD (n = 63) GvHD prophylaxis: No IST regimens reported | MRD (n = 23) MC (n = 169) | Median starting CD3 dose: 1 × 106/kg | Preemptive DLI for MRD (n = 23) Preemptive DLI for MC (n = 169) | Decreasing MRD/improving peripheral blood counts: 71% (16/21); 5-y NRM: 9% 5-y CIR: 44% 5-y LFS: 47% 5-y OS: 51% —— Improving MC: 70% (110/158); 5-y NRM: 15% 5-y CIR: 28% 5-y LFS: 57% 5-y OS: 63% | 7% (18/248 patients from entire cohort including preemptive DLI for MRD/MC and prophylactic DLI) |
| Reference . | Study design . | Disease . | Graft type, conditioning regimen, donor source, GvHD prophylaxis . | Trigger . | Cell dose . | Study arms compared . | Efficacy outcomes . | Grade III/IV GvHD . |
|---|---|---|---|---|---|---|---|---|
| 20 | Prospective, nonrandomized | AML (n = 36), ALL (n = 44) | NR | MRD | Starting CD3 dose Matched related: 1 × 106/kg MUD/MMUD: 1 × 105/kg | Preemptive DLI vs no DLI | CIR: 6% 3-y OS: 80% —— CIR: 63% 3-y OS: 26% | NR |
| 21 | Case report | AML (n = 1) | NR | MRD, MC | Not reported | Single case report | Conversion to MRD negativity | NR |
| 22 | Prospective, nonrandomized | AML (n = 61) ALL (n = 38) MDS (n = 6) Total n = 105 | T cell-replete MAC-BM/PBSC-alloHSCT Conditioning regimens/donor source: matched related (n = 40): Bu/Cy or Cy/TBI Haplo (n = 53) and MUD (n = 12): Bu/Cy + ATG or Cy/TBI + ATG GvHD prophylaxis: CSA, MMF, MTX (± ATG) | MRD | Median CD3 dose: 3.8 × 107/kg | Preemptive DLI (n = 56) vs IL-2 (n = 49) | CIR: 28% 3-y OS: 58% 3-y DFS: 56% —— CIR: 64% 3-y OS: 28% 3-y DFS: 24% | 8% (P = .471) —— 4% |
| 30 | Retrospective | AML (n = 14) ALL (n = 11) CML (n = 2) | T cell-replete MAC-PBSC-alloHSCT Conditioning regimens/donor source: matched related (n = 14): Bu/Cy Haplo (n = 2) and MUD (n = 11): Bu/Cy + ATG + cytarabine GvHD prophylaxis: CSA, MMF, MTX (± ATG) | MRD | Median CD3 dose: 5.51 × 107/kg | Preemptive DLI vs Therapeutic DLI | 1-y OS: 94% —— 1-y OS: 27% | 6% —— 9% |
| 24 | Prospective, nonrandomized phase 2 trial | AML (n = 14) MDS (n = 4) MPN (n = 2) Others (n = 16) | T cell-replete low-dose alemtuzumab RIC-PBSC-alloHSCT Conditioning regimens: Myeloid: Flu/Bu Lymphoid: Flu/Cy (± rituximab) Donor source: MUD: 33 MMUD: 3 GvHD prophylaxis: Tacrolimus, MTX, alemtuzumab | MC (<50% at d+60) | Starting CD3 dose: 0.5–1.0 × 107/kg | Preemptive DLI | 2-y OS: 57%; 2-y DFS: 38%; 1-y NRM: 14% | 0% |
| 25 | Retrospective | AML (n = 16) NHL (n = 6) HL (n = 5) MM (n = 4) ALL (n = 3) Others (n = 6) | T cell-replete HLA-haplo-BM-alloHSCT Conditioning regimens: MAC (n = 6): Bu/Cy RIC (n = 34): Flu/Cy/TBI Donor source: Haplo (n = 40) GvHD prophylaxis: Tacrolimus, MMF, PTCy | MRD, LOC | Starting CD3 dose 1 × 105/kg-1 × 106/kg | Preemptive DLI (n = 5) vs Therapeutic DLI (n = 35) | ORR: 60% —— ORR: 26% | NR |
| 23 | Prospective, nonrandomized | AML (n = 17) | T cell-replete BM/PBSC-MAC-alloHSCT Conditioning regimens/donor source: matched related (n = 43): Bu/Cy or Cy/TBI Haplo (n = 44) and MUD (n = 5): Bu/Cy + ATG or Cy/TBI + ATG GvHD prophylaxis: CSA, MMF, MTX (± ATG) | MRD | NR | Preemptive DLI vs No DLI | 2-y CIR: 24% 2-y OS: 64% —— 2-y CIR: 84% 2-y OS: 0% | NR |
| 26 | Retrospective | AML (n = 22) ALL (n = 9) MM (n = 1) | T cell-replete HLA-haplo-MAC-BM-alloHSCT Conditioning regimens: Flu/Bu/TT Flu/TBI Donor source: Haplo (n = 32) GvHD prophylaxis: CSA, MMF, PTCy | MRD | Starting CD3 dose 1 × 104/kg-1 × 105/kg | Preemptive DLI vs Therapeutic DLI | ORR: 45% 2-y OS: 43% —— ORR: 33% 2-y OS: 19% | 5% —— 8% |
| 35 | Retrospective | AML (n = 207) | T cell-replete MAC-BM/PBSC/CB-alloHSCT Conditioning regimens: Bu/Flu (+TT), Bu/Cy, Cy/Mel/TT Cy/TT, Cy/TBI Donor source: Matched related (n = 82) MUD (n = 66) Haplo (n = 59) GvHD prophylaxis: CSA, MTX | MRD | Starting CD3 dose: Matched-sibling: 1 × 106/kg MUD: 1 × 105/kg; HaploDLI: 1 × 104/kg | WT1 100 copies/104 ABL vs WT1 180 copies/104 ABL | CIR: 29% 4-y LFS 74% —— CIR: 76% 4-y LFS: 23% | 0% 0% |
| 31 | Retrospective | AML (n = 31) NHL (n = 19) MDS (n = 8) Others (n = 28) | T cell-replete BM/PBSC-MAC/RIC-alloHSCT Conditioning regimens: RIC (n = 60): Flu, Mel, Alemtuzumab MAC (n = 26): Bu/Cy, Bu/Flu, TBI/Cy, TBI/Cy/VP Donor sources: Matched related (n = 53) MUD (n = 25) MMUD (n = 8) GvHD prophylaxis: Not reported for MAC; alemtuzumab for RIC | MC | Starting CD3 dose: Matched-sibling: 3 × 106-1 × 107/kg MUD: 1-3 × 106/kg | Preemptive DLI vs Therapeutic DLI | 5-y OS: 69% 5-y PFS: 71% —— 5-y OS: 28% 5-y PFS: 18% | 26% —— 31% |
| 28 | Retrospective | AML (n = 14) MDS (n = 20 ALL/NHL (n = 5) CML (n = 2) | T-cell replete PB-haploHCT Conditioning regimens: MAC (n = 8) RIC (n = 13) Donor source: Haplo (n = 21) GvHD prophylaxis: tacrolimus, MMF/ sirolimus, MMF, PTCy | MC | Most common starting CD3 dose: 1 × 106/kg | Preemptive DLI (n = 2) vs Therapeutic DLI (n = 12) | 120-d OS: 100% —— 120-d OS: 29% | NR |
| 27 | Retrospective, matched-pair analysis | AML, MDS, ALL (n = 20) | T cell-replete BM/PBSC-MAC-alloHSCT Conditioning regimens/donor source: matched related (n = 8): Bu/Cy Haplo (n = 12): Bu/Cy + cytarabine + ATG GvHD prophylaxis: CSA, MMF, MTX | MRD | Median CD3 dose: 2.5 × 107/kg | No control | MRD conversion: 75%; 2-y CIR 31%; 2-y OS 69% | Grade II-IV aGvHD: 4 (20%) |
| 29 | Retrospective single-center landmark analysis | AML (n = 42) | T cell-replete PBSC-MAC/RIC-alloHSCT Conditioning regimens: MAC (n = 12): Bu/Cy, TT/Bu/Flu RIC (n = 30): Flu/BCNU/Mel, Flu/TT Donor source: matched related (n = 11) MUD (n = 23) MMUD (n = 7) Haplo (n = 1) GvHD prophylaxis: CSA/Alemtuzumab, CSA/MMF, MTX ± ATG | MRD (n = 18) MC (n = 24) | Median starting CD3 dose: 0.69 × 106/kg | Preemptive DLI vs Therapeutic DLI | 5-y OS: 43% —— 5-y OS: 10% | 7% —— 6% |
| 34 | Retrospective registry study | AML (n = 153) ALL (n = 39) | BM/PBSC-MAC /RIC-alloHSCT with (n = 149) and without (n = 42) T-cell depletion Conditioning regimens: MAC (n = 74) RIC (n = 107) Donor source: Matched related (n = 129) MUD (n = 63) GvHD prophylaxis: No IST regimens reported | MRD (n = 23) MC (n = 169) | Median starting CD3 dose: 1 × 106/kg | Preemptive DLI for MRD (n = 23) Preemptive DLI for MC (n = 169) | Decreasing MRD/improving peripheral blood counts: 71% (16/21); 5-y NRM: 9% 5-y CIR: 44% 5-y LFS: 47% 5-y OS: 51% —— Improving MC: 70% (110/158); 5-y NRM: 15% 5-y CIR: 28% 5-y LFS: 57% 5-y OS: 63% | 7% (18/248 patients from entire cohort including preemptive DLI for MRD/MC and prophylactic DLI) |
aGvHD, acute graft-versus-host disease; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; ATG, antithymocyte globulin; BCNU, carmustine; Bu, busulfan; CIR, cumulative incidence of relapse; CSA, cyclosporine A; Cy, cyclophosphamide; DFS, disease-free survival; DLI, donor lymphocyte infusion; Flu, fludarabine; Haplo, HLA-haploidentical donor; LFS, leukemia-free survival; MAC, myeloablative conditioning; MC, mixed chimerism; MDS, myelodysplastic syndrome; Mel, melphalan; MMUD, mismatched unrelated donor; MMF, mycophenolate mofetil; MRD, measurable residual disease; MTX, methotrexate; MUD, matched unrelated donor; NR, not reported; NRM, nonrelapse mortality; ORR, overall response rate; OS, overall survival; PTCy, posttransplant cyclophosphamide; RIC, reduced-intensity conditioning; TBI, total body irradiation; TT, thiotepa; VP, etoposide.
A large prospective trial evaluated preemptive DLI for MRD after alloHSCT across a spectrum of hematologic entities including AML. Preemptive DLI significantly reduced CIR at 3 years (28% vs 64%) without increasing the incidence of ≥grade 3 GvHD compared with interleukin-2 (IL-2).22 Two follow-up studies found similar results in AML and myelodysplastic syndrome (MDS).23,27 Interestingly, the addition of chemotherapy before DLI did not add any benefit.27 Another group tested preemptive DLI triggered by the detection of <50% donor T-cell chimerism at day d+60 in 25 patients receiving alemtuzumab-containing RIC-unrelated transplant for hematologic malignancies including AML. This approach was safe with no cases of high-grade GvHD and led to a promising 2-year OS of 57%.24
In 2021, Rettig et al studied preemptive DLI as triggered by either MRD or mixed chimerism (MC) vs therapeutic DLI in patients with AML.29 Preemptive DLI improved 5-year OS (43% vs 10%) with minimal incidence of high-grade GvHD. Patients with MC fared significantly better than those treated for MRD, possibly signifying a more favorable biological trajectory. Surprisingly, there was no significant difference regarding the time to first DLI between the 2 cohorts calling into question the traditional “early-warning” concept and potentially pointing to inherent differences in the underlying disease characteristics.29 On the contrary, timing has been suggested as a crucial determinant for both DLI efficacy and safety with unacceptable toxicity when administered before d+100 and potentially lost efficacy for prophylactic DLI administered beyond 6 months posttransplant.36
Although the available data support a role for preemptive DLI to treat impending relapse posttransplant, reliably establishing an MRD marker in the context of the heterogeneous genomic landscape of AML is challenging.29,37 Using MC to trigger preemptive DLI is even more troublesome because recrudescent recipient cells do not necessarily point toward relapse.1 Hence, it remains elusive when, and if at all, preemptively treated patients would have relapsed, had they not been given DLI infusions, leading to both lead time and selection biases.
What are the consensus guidelines regarding administration of preemptive DLI?
Based on the available evidence, the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT) outlined in their 2016 Guidelines an individualized and risk-adapted approach to identify patients with AML at high risk for relapse for which preemptive DLI should be considered. Although acknowledging that their recommendations lie outside the current standard of care, they advocate for aggressive weaning and discontinuation of all immunosuppression upon detection of MRD and/or increasing MC and starting DLI as early as d+100 in suitable high-risk patients while closely monitoring for GvHD.1 The EBMT Handbook similarly describes the use of preemptive DLI for persisting or reemergent MRD/MC. According to the authors, DLI should only be initiated in the absence of GvHD and uncontrolled infections with a recommended starting cell dose of 1 × 105/kg to 1 × 106/kg for both related and unrelated matched donors, and 1 × 104/kg for HLA-haploidentical donors because of toxicity concerns arising from higher HLA disparity and risk of GvHD. DLI may be repeated 3 to 4 times at 4- to 12-week intervals with incremental dose increases of 0.5 to 1 log steps until achieving MRD negativity or complete donor chimerism.38 In their 2020 Consensus Recommendations on the Clinical Use of Haploidentical DLI, the Acute Leukemia Working Party notes the potential benefits of preemptive DLI and proposes repeated administration of DLI for persistent MRD or LOC starting at a dose of 1 × 105 CD3 cells/kg. The authors recommend tapering all immunosuppression before initiating DLI and excluding patients whose donor chimerism has fallen below 50% for concerns of marrow aplasia.39
What other strategies have been pursued to restore GvL using DLI?
Manipulated DLI
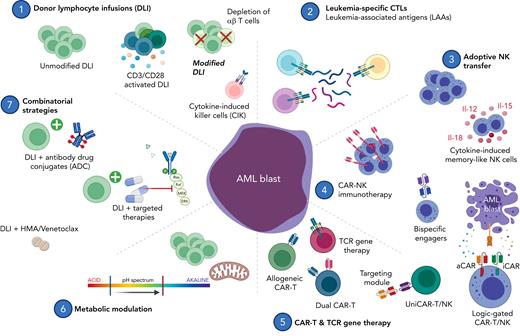
To discriminate GvL from GvHD, several groups have manipulated donor T cells ex vivo with the goal of favoring T-cell subsets that can kill leukemic cells while sparing healthy tissue. Figure 2 provides an overview of the various postremission strategies being pursued.
Postremission adoptive cellular therapy for high-risk acute leukemia. (1) Donor lymphocyte infusions aim to restore GvL and have been applied clinically to treat overt relapse posttransplant, prevent relapse in high-risk patients (prophylactic intent), and to restore GvL on impending relapse as defined by detection of MRD or LOC (preemptive intent). Several groups have refined this strategy with depletion and enrichment of specific T-cell subsets. Cytokine-induced killer cells (CIK) mimic an NK-like phenotype and are capable of HLA-unrestricted killing mediated through NKG2D and DAP10. (2) CTLs are primed ex vivo with leukemia-associated antigen (LAA) peptide mixes to redirect specificity. (3) Adoptive transfer of NK cells supports immune reconstitution early posttransplant. Ex vivo cytokine induction using interleukins-12, -15, -18 primes memory-like NK cells for enhanced killing. (4) CAR-modified NK cells are redirected for specific target engagement using a genetically engineered synthetic receptor. Logic-gated CAR-NK cells can discriminate between leukemic blasts and healthy progenitor cells by recognition of both activating and inhibitory stimuli. (5) CAR-T cells are genetically engineered to specifically recognize and kill targets in an HLA-unrestricted manner. Universal allogeneic CAR-T candidates are genetically edited for safe clinical use despite being derived from third-party donors. Dual-CAR-T constructs target multiple antigens simultaneously to circumvent immune escape arising from antigen-negative disease. TCR-engineered T cells recognize leukemia-associated antigens such as WT1 in an HLA-dependent manner. (6, 7) DLI combination therapy promises both synergistic antileukemic activity and immune modulation to augment GvL. Abbreviations: aCAR, activating chimeric antigen receptor; ADC, antibody-drug conjugate; Bcl-2, B-cell lymphoma-2; BiTE, bispecific T-cell engager; CAR, chimeric antigen receptor; CIK, cytokine-induced killer cells; CTL, cytotoxic T lymphocytes; DLI, donor lymphocyte infusion; HDACi, histone deacetylase inhibitor; HMA, hypomethylating agent; iCAR, inhibitory chimeric antigen receptor; LAA, leukemia-associated antigen; LOC, loss of complete donor chimerism; TCR, T-cell receptor; WT1, Wilms’ tumor protein. Image created in BioRender.
Postremission adoptive cellular therapy for high-risk acute leukemia. (1) Donor lymphocyte infusions aim to restore GvL and have been applied clinically to treat overt relapse posttransplant, prevent relapse in high-risk patients (prophylactic intent), and to restore GvL on impending relapse as defined by detection of MRD or LOC (preemptive intent). Several groups have refined this strategy with depletion and enrichment of specific T-cell subsets. Cytokine-induced killer cells (CIK) mimic an NK-like phenotype and are capable of HLA-unrestricted killing mediated through NKG2D and DAP10. (2) CTLs are primed ex vivo with leukemia-associated antigen (LAA) peptide mixes to redirect specificity. (3) Adoptive transfer of NK cells supports immune reconstitution early posttransplant. Ex vivo cytokine induction using interleukins-12, -15, -18 primes memory-like NK cells for enhanced killing. (4) CAR-modified NK cells are redirected for specific target engagement using a genetically engineered synthetic receptor. Logic-gated CAR-NK cells can discriminate between leukemic blasts and healthy progenitor cells by recognition of both activating and inhibitory stimuli. (5) CAR-T cells are genetically engineered to specifically recognize and kill targets in an HLA-unrestricted manner. Universal allogeneic CAR-T candidates are genetically edited for safe clinical use despite being derived from third-party donors. Dual-CAR-T constructs target multiple antigens simultaneously to circumvent immune escape arising from antigen-negative disease. TCR-engineered T cells recognize leukemia-associated antigens such as WT1 in an HLA-dependent manner. (6, 7) DLI combination therapy promises both synergistic antileukemic activity and immune modulation to augment GvL. Abbreviations: aCAR, activating chimeric antigen receptor; ADC, antibody-drug conjugate; Bcl-2, B-cell lymphoma-2; BiTE, bispecific T-cell engager; CAR, chimeric antigen receptor; CIK, cytokine-induced killer cells; CTL, cytotoxic T lymphocytes; DLI, donor lymphocyte infusion; HDACi, histone deacetylase inhibitor; HMA, hypomethylating agent; iCAR, inhibitory chimeric antigen receptor; LAA, leukemia-associated antigen; LOC, loss of complete donor chimerism; TCR, T-cell receptor; WT1, Wilms’ tumor protein. Image created in BioRender.
Donor lymphocyte subsets
Early attempts to differentiate GvL from GvHD originated in the mid-1990s when groups sought to selectively deplete DLI of T-cell subsets that had been implicated in mediating GvHD.40-43 Seeking to reduce relapse rates for recipients of T cell-depleted allografts, groups in the mid-2000s tested the prophylactic administration of CD8-depleted DLI to accelerate immune reconstitution early posttransplant. One study investigated infusion of CD8-depleted DLI on days +60 and +120 after T cell-depleted HLA-identical RIC alloHSCT and demonstrated it to be safe and capable of restoring full donor chimerism in 4 trial subjects with declining chimerism.44 For T cell-depleted HLA-haploidentical grafts, this approach was shown to promote T-cell recovery without increasing the risk of nonrelapse mortality (NRM; 1-year NRM: 15%).45
With time, research focus shifted to removing regulatory T-cell subsets (Treg) with the aim of unleashing alloreactivity and enhancing GvL. As hypothesized, Treg depletion resulted in enhanced response rates and improved event-free survival in patients with relapsed hematologic malignancies, without excess GvHD.46-48 Another approach, shown in preclinical studies to enhance GvL without increasing GvHD, is to enrich for memory T cells. This subset was believed to have a lower ability to induce GvHD because of a skewed T-cell receptor (TCR) repertoire secondary to prior antigen exposure.49,50 However, results from a phase 1 trial in patients with relapsed hematologic malignancies, including AML, yielded disappointing long-term disease control with only 3 of 15 patients (20%) in complete remission (CR) and a median disease-free survival of 4.9 months.51
Adopted from the field of pediatric haploidentical allo-transplant, DLI depleted of alloreactive αβ T cells52-55 aim to skew the immune cell composition toward gamma-delta (γδ) T cells and natural killer (NK) cells that kill leukemic blasts in a non-major histocompatibility complex (MHC)-restricted manner without inducing GvHD. Evidence for this strategy remains scarce, with only 1 case report documenting the course of a patient with AML relapse after transplant. After sorafenib reinduction, the patient received a total of eight αβ T cell-depleted DLI infusions that helped induce and transiently maintain an MRD-negative remission before a second fulminant relapse, unresponsive to DLI.56 A phase 1 trial is under way to further explore this concept in the posttransplant setting (NCT03939585).57 A related effort aims to eradicate alloreactive T cells using photodepletion. In recipients of TCD-haploHSCT, this approach was shown to reduce NRM and prolong survival.58
Activated DLI and cytokine-induced killer cells
Carl June’s group explored in a phase 1 trial ex vivo activated DLI using CD3/CD28 stimulation and reported complete remissions in a subset of patients with relapsed leukemia after HSCT without causing excessive GvHD.59 In a follow-up study, they tested prophylactic administration of activated DLI on days +120 and +180 in patients with high risk for relapse following alloHSCT. This approach, although safe, had a limited effect in preventing relapse60 potentially because of delayed administration or intrinsically inferior potency compared with unstimulated DLI. In support of their expansion protocol, the authors report no phenotypic signs of T-cell exhaustion and point to previous studies of genetically modified T cells expanded up to >1000-fold using the same approach with evidence of in vivo persistence for up to a decade.
CIK cells are CD8+ T lymphocytes cultured ex vivo with interferon-γ, IL-2, and anti-CD3 to induce an NK-like phenotype with non-HLA-restricted cytotoxicity mediated through NKG2D and DAP10.61,62 Infusion of CIK cells has been explored in patients with relapsed hematologic malignancies posttransplant including AML and has been shown to induce clinically meaningful responses in 30% to 50% of patients without inducing high-grade GvHD.63,64
G-CSF mobilized DLI
Granulocyte colony-stimulating factor (G-CSF)-mobilized donor lymphocytes, derived from the initial stem cell product, have been explored in a small number of retrospective studies.65-72 The cellular composition of the G-CSF DLI product has been reported to be different from that of steady-state DLI, with increased frequencies of immunoregulatory myeloid-derived suppressor cells, which might constrain severe forms of GvHD and favorably affect clinical outcomes. Furthermore, higher numbers of CD34+ progenitor cells might accelerate engraftment after myeloablative conditioning.72 Although one retrospective study reported improved conversion to full donor chimerism and lower CIR for G-CSF-primed DLI,67 most studies found both approaches to be equally effective and safe.
Leukemia-specific CTLs
In contrast to the previously mentioned forms of cellular immunotherapy, antigen-specific cytotoxic T cells (CTLs) aim to selectively target leukemia-associated antigens (LAAs) by priming donor-derived T cells with peptide mixes ex vivo in combination with cytokines.73-75 In AML, the adoptive transfer of donor-derived WT1-specific T cells was pioneered by Greenberg’s group and found to exert antileukemic activity, including induction of a prolonged MRD-negative remission in 1 patient.76 Extending the scope of CTLs beyond a single antigen, infusion of multispecific CTLs against PRAME, WT1, Survivin, and NY-ESO-1, is currently under investigation both with therapeutic and prophylactic intent in patients with AML after alloHSCT in a trial run by the Baylor group, with very promising early reports.77
How to combine DLI with other agents
DLI combination strategies build on the molecular rationale to modulate the T cell-driven antileukemic response and favorably impact GvL while mitigating GvHD. Epigenetic modulators, for instance, have been shown to augment GvL by upregulating previously silenced LAAs,78 minor histocompatibility antigens,79 and MHC class I/II molecules80-82 and may prevent GvHD by activating Tregs.83-85 The available clinical evidence both to combat overt relapse86-88 and with prophylactic intent,89-92 however, is disappointing, with limited long-term success for most patients. More promising, a retrospective study found a survival benefit for patients with Flt3-ITD-mutant AML who received DLI and sorafenib as salvage treatment for relapse after alloHSCT.93 Venetoclax with DLI has also been explored but larger studies are needed to assess potential synergies.94 DLI has similarly been tested alongside novel leukemia-directed bispecific T cell engagers95-98 and antibody-drug conjugates,99 such as gemtuzumab ozogamicin in the case of R/R AML (NCT03374332).
Other groups have examined ways to restore GvL, circumventing the direct transfer of immune cells by leveraging the power of immune checkpoint blockade. For example, CTLA-4 blockade after alloHSCT has been shown to induce remissions without causing significant GvHD,100 emulating some of the immunological effects observed with DLI.8 In a recent study, metabolic reprograming of infused lymphocytes restored GvL in patients with relapsed AML and augmented T-cell metabolic fitness as assessed by elevated levels of oxidative phosphorylation.101
How can NK cells prevent relapse posttransplant?
DLIs exert their antileukemic potency through HLA-restricted killing which is hampered by genomic HLA class I loss or downregulation of HLA II molecules, in effect rendering leukemic blasts invisible to donor T cells.102
In AML, especially in the HLA-haploidentical and mismatched setting, the selective pressure arising from HLA disparity has been shown to result in relapse associated with genomic loss of the mismatched HLA class I/II.103-106 Seminal studies have shown epigenetic silencing of HLA class II molecules in up to 50% of patients with R/R AML after alloHSCT, including those transplanted from matched donors.107,108 Adoptive NK immunotherapy promises to overcome this mechanism of immune escape by relying on a set of germline-encoded endogenous killer-cell immunoglobulin-like receptors that prime NK cells for HLA-unrestricted killing.
Early evidence for NK-driven alloreactivity was observed in patients undergoing T cell-depleted haploHSCT, in which NK cells provided the dominant force of antileukemic immunity early after transplant.109-111 Evidence supporting the safe clinical use of NK adoptive cell therapy emerged in the early 2000s from the group in Minnesota and later by multiple other investigators that tested unmodified NK cells and ex vivo expanded NK cells to treat and prevent relapse after alloHSCT.112-121 More recently, adoptive transfer of cytokine-induced memory-like NK cells, which are stimulated ex vivo with IL-12/15/18, has been shown to reduce the frequency of pathogenic variant alleles including WT1, TP53, TET2, ASXL1, in the first 3 patients with relapsed AML after alloHSCT in an ongoing phase 1 trial.122-124
Prophylactic NK immunotherapy has been explored to provide recipients of HLA-haploidentical grafts with an early line of immunologic defense to mitigate some of the morbidity and mortality secondary to delayed T-cell reconstitution.125,126 In a trial reported in 2021, infusion of up to 1 × 108 NK cells peritransplant led to early NK-dominant immune reconstitution and significantly reduced CIR compared with historical controls (4% vs 38%) with minimal incidence of high-grade GvHD.126 With the increasing adoption of posttransplant cyclophosphamide as GvHD prophylaxis both in the HLA-mismatched and matched transplantation setting, the benefits of early immune reconstitution afforded by adoptive transfer of ex vivo expanded NK cells are likely to become more relevant even beyond haploHSCT.
Cellular immunotherapy using engineered lymphocytes
The advent of genetically engineered lymphocytes has opened novel avenues to treat and prevent AML relapse posttransplant. The first clinical application to leverage these tools was to engineer T cells to express suicide genes including inducible Caspase9127,128 or thymidine kinase129 as safety switches, which allow their elimination in vivo in the event of GvHD.
CAR-redirected cellular therapy
The next leap in genetic engineering came with CD19-chimeric antigen receptor (CAR)-modified T lymphocytes, and some early studies focused on how these could be exploited to treat relapsed ALL after alloHSCT.130,131 In AML, there is a relative paucity of suitable antigens, and most efforts have focused on targeting CD33132-136 and CD123.135,137,138 Aside from the quest to identify viable targets, research efforts have also focused on engineering more sophisticated CAR constructs. Today’s CAR molecules build on optimized intracellular costimulatory domains and may include molecular payloads for enhanced functionality including transgenic expression of cytokines or immunomodulatory agents (ie, fourth-generation CAR-T cells, sometimes referred to as TRUCKs).139 Efforts are also ongoing to increase immune cell trafficking, extend in vivo persistence, and overcome functional suppression from the tumor microenvironment leveraging multiplexed genetic editing approaches.140-143 Dual targeting has been proposed to overcome tumor immune evasion from antigen loss144-147 and logic-gated CAR circuits now allow the selective targeting of cancerous cells while sparing healthy tissues with shared antigen expression.148-150 In AML, logic-gated CARs, which are activated by specific leukemic antigens but inhibited by concurrent recognition of surface molecules expressed on healthy HSCs, have been reported.151-154 Another approach to target shared antigens while avoiding excessive toxicity builds on short-lived adaptor molecules that cross-link universal CAR molecules expressed on either T or NK cells with their respective targets.155-159 Recent first-in-human data demonstrated that this strategy can yield responses including CRs in relapsed AML160 (NCT04230265).
Despite these advancements, the cumbersome manufacturing process of autologous CAR-T products continues to restrict the scope of eligible patients, and several groups are exploring universal allogeneic CAR-T cells to overcome these logistical hurdles as well as immunologic anergy of autologous lymphocytes.161-163 In AML, allogeneic CAR-T cells targeting CD123 (NCT03190278, NCT02159495, NCT03114670, NCT03556982) and CD33 (NCT02799680) are being investigated in the clinic and could present an option for patients relapsing after alloHSCT.
CAR-NK immunotherapy offers a highly scalable, allogeneic cell product.164 Current NK cell therapy programs rely on different sources of NK cells including cord blood,164-166 peripheral blood,123,124,167 induced pluripotent stem cells (iPSCs)168-170 and cell lines,171,172 with each platform presenting its unique advantages and limitations, as has been reviewed previously.173,174 Clinically, CAR-NK therapy has demonstrated highly encouraging responses in patients with CD19+ malignancies.175,176 Current trial protocols have excluded patients who had previously undergone alloHSCT. Given its favorable safety record, CAR-NK immunotherapy may, however, be an attractive treatment strategy after transplant for future studies to explore. Next-generation CAR-NK therapies are already on the horizon, with many efforts ongoing to enhance NK cell fitness including through metabolic modulation.170,177
TCR gene therapy
Targeting AML is difficult because shared surface antigen expression across leukemic blasts and healthy stem cells. TCR gene therapy allows the reprogramming of T cells to recognize LAAs, presented through HLA molecules and promises to selectively target transformed cells.186 Greenberg and his group pioneered this approach by prophylactically infusing 12 patients after alloHSCT with genetically modified T cells targeting WT1.187-189 Compared with matched controls, they found an encouraging relapse-free survival rate of 100% vs 54% at a median follow-up of 44 months. Very recently, HLA-independent T cells have emerged and leverage a modified TCR-CD3 complex to target extracellular antigens. By design, HLA-independent T cells have dramatically increased antigen sensitivity and allow the targeting of antigens expressed at very low densities, another strategy to overcome antigen-low immune escape.190
How do we manage imminent relapse after alloHSCT using preemptive cell therapy?
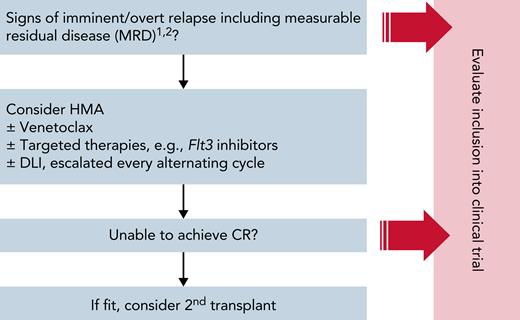
As evidence for the preemptive use of DLI remains scarce and available studies may be confounded by nonrandom selection bias, the decision for preemptive administration of DLI must be meticulously weighed against the risk of inducing GvHD. Although we cannot recommend a definitive guideline because of the lack of unequivocal data, we provide our institutional algorithm (Figure 3) to guide clinicians in their decision-making process to identify patients who might benefit from preemptive cellular therapy.
MD Anderson Cancer Center institutional algorithm to manage patients with high-risk AML after alloHSCT outside of a clinical trial. The presented algorithm is adopted from MDACC’s institutional guidelines to help identify patients who may be candidates for cell therapy post-alloHSCT and to structure the clinical decision-making process that feeds into the management of this hard-to-treat patient population. As a general rule, we propose an individualized risk-stratified approach that takes into account both pretransplant clinical features (eg, remission status, molecular and cytogenetic risk profile, comorbidities, chemorefractory disease), transplant-associated aspects (eg, graft type, donor source, conditioning regimen, degree of HLA disparity, type of GvHD prophylaxis), and posttransplant parameters including the emergence and severity of aGvHD, MRD markers, and chimerism studies. Whenever possible, patients should be evaluated for inclusion into a clinical trial to benefit from novel innovative treatment strategies. Outside of clinical trials, patients should be treated on protocols whenever possible. Candidates for DLI should be discussed at a patient management conference. (1) MRD studies should be performed in accordance with Food and Drug Administration guidance and based on either multiparameter flow cytometry, reverse transcriptase-quantitative polymerase chain reaction (PCR), allele-specific oligonucleotide PCR (ASO-PCR), or targeted NGS. Assessment of MRD levels should be performed longitudinally (ie, both pre- and posttransplant) to provide the highest degree of sensitivity and specificity in detecting clinically relevant leukemia-driving clones taking into account the manufacturer’s guidance for the specific diagnostic test used. Results should be carefully interpreted in light of the test’s inherent sensitivity and specificity as well as diagnostic limitations arising from clonal evolution and clonal heterogeneity. (2) Chimerism assessment is done on peripheral blood or bone marrow. Due to the lack of unequivocal data and the concern of inducing GvHD, our institutional guidelines preclude any conclusions regarding the use of preemptive cell therapy based on mixed T-cell chimerism studies only.
MD Anderson Cancer Center institutional algorithm to manage patients with high-risk AML after alloHSCT outside of a clinical trial. The presented algorithm is adopted from MDACC’s institutional guidelines to help identify patients who may be candidates for cell therapy post-alloHSCT and to structure the clinical decision-making process that feeds into the management of this hard-to-treat patient population. As a general rule, we propose an individualized risk-stratified approach that takes into account both pretransplant clinical features (eg, remission status, molecular and cytogenetic risk profile, comorbidities, chemorefractory disease), transplant-associated aspects (eg, graft type, donor source, conditioning regimen, degree of HLA disparity, type of GvHD prophylaxis), and posttransplant parameters including the emergence and severity of aGvHD, MRD markers, and chimerism studies. Whenever possible, patients should be evaluated for inclusion into a clinical trial to benefit from novel innovative treatment strategies. Outside of clinical trials, patients should be treated on protocols whenever possible. Candidates for DLI should be discussed at a patient management conference. (1) MRD studies should be performed in accordance with Food and Drug Administration guidance and based on either multiparameter flow cytometry, reverse transcriptase-quantitative polymerase chain reaction (PCR), allele-specific oligonucleotide PCR (ASO-PCR), or targeted NGS. Assessment of MRD levels should be performed longitudinally (ie, both pre- and posttransplant) to provide the highest degree of sensitivity and specificity in detecting clinically relevant leukemia-driving clones taking into account the manufacturer’s guidance for the specific diagnostic test used. Results should be carefully interpreted in light of the test’s inherent sensitivity and specificity as well as diagnostic limitations arising from clonal evolution and clonal heterogeneity. (2) Chimerism assessment is done on peripheral blood or bone marrow. Due to the lack of unequivocal data and the concern of inducing GvHD, our institutional guidelines preclude any conclusions regarding the use of preemptive cell therapy based on mixed T-cell chimerism studies only.
Our institutional guidelines recommend performing T and myeloid chimerism studies on peripheral blood and if available also on bone marrow samples. For MRD studies, bone marrow samples would be preferred when available. Within our institution, MRD is routinely assessed by multiparameter flow cytometry but may be complemented with polymerase chain reaction or next-generation sequencing-based detection methods, bearing in mind the inherent limitations of MRD assessment in the posttransplant setting.37 Our institution regards mixed myeloid chimerism, as defined by the CD33+ fraction, a particular concern reflecting imminent relapse. Mixed T-cell chimerism, as defined by the CD3+ fraction, on the other hand, is frequently observed with busulfan/fludarabine conditioning regimens and should, by itself, not entail DLI infusions.
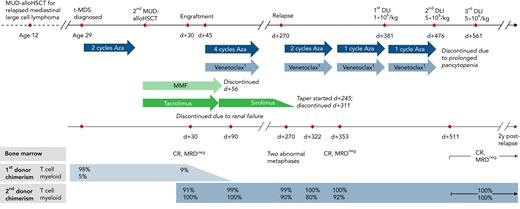
For patients with molecular relapse and/or mixed chimerism, we suggest evaluation for inclusion into a clinical trial. If no suitable trials are available, preemptive DLI may be considered in an individualized risk-stratified approach. Cell doses should be adjusted according to the donor source with starting doses of 1 × 106-7/kg in the matched-sibling/matched unrelated donor setting and 1 × 104-6/kg for haplo-DLI depending on patient and transplant-related factors including graft type and GvHD prophylaxis (Figure 4). Epigenetic modulators, venetoclax, and targeted therapies may also be considered. If DLI fails to convert MRD, HLA loss should be ruled out, preferably using polymerase chain reaction-based assays.191 Second alloHSCT should be reserved for overt hematologic relapse, in which chemotherapy-based reinduction should similarly be evaluated. For documented HLA loss, a different donor may be considered for the patient to benefit from renewed GvL.192,193 To illustrate our institutional management, we have included a case vignette of a patient with relapsed t-MDS after alloHSCT who received DLI with azacitidine and venetoclax to restore complete donor chimerism (Figure 5).
MD Anderson Cancer Center institutional guidelines for DLI starting dose. DLI starting dose should be selected based on donor and graft type. If DLI is administered earlier than 6 months after transplant, the starting cell dose should be adjusted on a case-by-case basis to minimize the risk of GvHD. DLI is repeated every alternating cycle of HMA therapy, escalating cell doses incrementally in 0.5 log steps. q, every; w, weeks.
MD Anderson Cancer Center institutional guidelines for DLI starting dose. DLI starting dose should be selected based on donor and graft type. If DLI is administered earlier than 6 months after transplant, the starting cell dose should be adjusted on a case-by-case basis to minimize the risk of GvHD. DLI is repeated every alternating cycle of HMA therapy, escalating cell doses incrementally in 0.5 log steps. q, every; w, weeks.
Case vignette. A 32-year-old man with a history of MUD-alloHSCT for relapsed mediastinal large cell lymphoma underwent second MUD-alloHSCT for therapy-related MDS (t-MDS) with complex karyotype and del7q. He relapsed at day (d) +270 with chimerism studies revealing 99% donor T cells and 90% donor myeloid cells. Chimerism studies on day +322 indicated further decrease of donor myeloid chimerism to 80%. Immunosuppression with sirolimus was tapered and ended by day +311. Administration of azacitidine in combination with dose-adjusted venetoclax due to anti-fungal prophylaxis led to MRDneg complete remission (CR) by day +353 with concomitant increase in donor myeloid chimerism to 92%. Three courses of DLI were administered from d+381 through d+561 at escalating dose levels of 1 × 106 to 5 × 106/kg. Donor myeloid chimerism was fully restored 30 days after the second course of DLI. The patient continues to be in MRDneg CR with complete donor chimerism at 2 years after relapse. 1Dose adjusted to 100 mg daily because of concomitant antifungal prophylaxis.
Case vignette. A 32-year-old man with a history of MUD-alloHSCT for relapsed mediastinal large cell lymphoma underwent second MUD-alloHSCT for therapy-related MDS (t-MDS) with complex karyotype and del7q. He relapsed at day (d) +270 with chimerism studies revealing 99% donor T cells and 90% donor myeloid cells. Chimerism studies on day +322 indicated further decrease of donor myeloid chimerism to 80%. Immunosuppression with sirolimus was tapered and ended by day +311. Administration of azacitidine in combination with dose-adjusted venetoclax due to anti-fungal prophylaxis led to MRDneg complete remission (CR) by day +353 with concomitant increase in donor myeloid chimerism to 92%. Three courses of DLI were administered from d+381 through d+561 at escalating dose levels of 1 × 106 to 5 × 106/kg. Donor myeloid chimerism was fully restored 30 days after the second course of DLI. The patient continues to be in MRDneg CR with complete donor chimerism at 2 years after relapse. 1Dose adjusted to 100 mg daily because of concomitant antifungal prophylaxis.
Conclusions and future directions
The quest to provide patients with high-risk AML with effective and tolerable treatment options has come a long way. However, despite the many strategies tested to improve outcomes for this patient group, the rate of relapse remains high, and long-term survival is unacceptably low.
On a more optimistic note, the available studies have linked preemptive DLI to reduced CIR and improved survival without excessive toxicity. Nevertheless, future prospective studies are needed to better delineate the role of preemptive DLI in preventing relapse. Although randomized, controlled trials are desirable, the complexity of studying patients in the posttransplant setting makes these studies challenging. Future research initiatives should embrace collaborative international efforts while fostering harmonization of standards to detect MRD to arrive at a meaningfully large sample size of real-world evidence.
The advent of genetically engineered lymphocytes has opened novel treatment avenues and laid the groundwork for further innovations.12,143,173 Going forward, we project that DLI will continue to play an important role in the management of patients with high-risk AML after alloHSCT. Aside from unmodified DLI, we anticipate multi-LAA-specific T cells and CAR/TCR-engineered cell therapies will gain considerable momentum and expand the current treatment armamentarium. Whether antigen-specific cell therapies will evolve to serve as preemptive measures to eradicate MRD/MC after alloHSCT remains to be seen. Notwithstanding, the powerful tools of genetic engineering promise an exciting new era of next-generation cell therapies, with novel concepts to modulate the immune response being explored to overcome some of the most notorious hurdles of AML therapy.
Acknowledgments
The authors thank Judy Moyes for critical review and edit of the manuscript.
This work was supported by the German Research Foundation (A.B., as Walter Benjamin Postdoctoral Fellow) (464778766); by grants from CPRIT (RP160693), by a Stand Up To Cancer Dream Team Research Grant (grant number: SU2C-AACR-DT-29-19), by grants from the National Institutes of Health (NIH) National Cancer Institute (1 R01 CA211044-01, 5 P01CA148600-03, and P50CA100632-16), the Specialized Program of Research Excellence (SPORE) in Leukemia grant (P50CA100632), by a grant (CA016672) to the MD Anderson Cancer Center from the NIH, and the generous support of The University of Texas Anderson Cancer Center Moon Shots Program. The SU2C research grant is administered by the American Association for Cancer Research, the scientific partner of SU2C.
Authorship
Contribution: A.B. and K.R. wrote and approved the article.
Conflict-of-interest disclosure: K.R. and The University of Texas MD Anderson Cancer Center have an institutional financial conflict of interest with Takeda Pharmaceutical and Affimed GmbH. K.R. participates on the Scientific Advisory Board for GemoAb, AvengeBio, Virogin Biotech, GSK, Caribou Biosciences, Navan Technologies, and Bayer. A.B. declares no competing financial interests.
Correspondence: Katayoun Rezvani, Department of Stem Cell Transplantation and Cellular Therapy, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 423, Houston, TX 77030; e-mail: krezvani@mdanderson.org.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal