Abstract
Background
Rearrangements of lysine methyltransferase 2A (KMT2A) gene, previously known as the MLL gene, occur in 3 to 5% of adult patients with de novo AML and are enriched in therapy-related disease after treatment with topoisomerase II inhibitors (Bill, M et al. PNAS. 2020). KMT2A encodes a histone H3 lysine 4 methyltransferase and KMT2A rearrangements result in fusion proteins that induce aberrant Hox gene expression. (Armstrong, SA et al. Nature. 2002) Among patients with KMT2A rearranged AML (rAML) receiving intensive chemotherapy, the fusion partner impacts prognosis, and KMT2A-MLLT3 is associated with an intermediate risk while other KMT2A rearrangements are associated with adverse risk in the ELN classification. (Dohner, H et al. Blood. 2017) Here we evaluate the outcomes of patients with newly diagnosed and relapsed or refractory (R/R) AML with KMT2A rearrangements receiving venetoclax and hypomethylating agents (HMA).
Methods
Medical records of 333 patients with newly diagnosed or R/R AML receiving venetoclax in combination with HMAs at City of Hope National Medical Center between 11/1/2015 and 4/15/2020 were reviewed. Criteria for inclusion were a pathologically confirmed diagnosis of AML, age > 18 years, treatment with either decitabine or azacitidine in combination with venetoclax. KMT2A rearrangements were detected by karyotype and confirmed by FISH or RNA sequencing. Responses were evaluated per the ELN criteria (Dohner, H et al. Blood. 2017) Minimal residual disease flow cytometry was performed at the University of Washington. Patient characteristics were summarized by frequency and associations between overall response and patient and disease characteristics were tested by Fisher's exact test. OS was evaluated by the Kaplan-Meier method and the difference between groups was determined by log-rank test. All statistical analyses were performed using SPSS and Prism.
Results
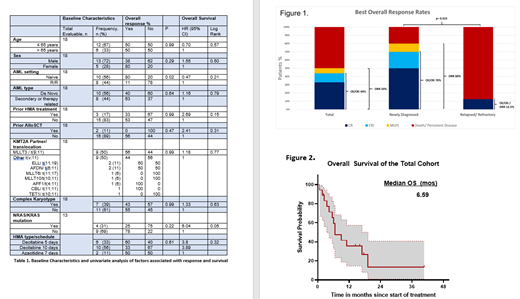
We identified 18 patients (5.4%) with KMT2A rAML who met criteria for inclusion. MLLT3 was the predominant fusion partner, occurring in nine patients followed by ELL (n=2), AFDN (n=2), MLLT6 (n=1), MLLT10 (n=1), AFF1 (n=1), CBL (n=1), and TET1 (n=1). The cohort included both newly diagnosed (n=10) and R/R (n=8) AML patients. 44% had therapy-related or secondary AML. NRAS or KRAS mutations occurred in 4 out of 13 patients (31%) with available sequencing prior to treatment. Decitabine was the predominant HMA used in combination with venetoclax and 56% of all patients received 10-day dosing during the first cycle. For the total cohort, 9 patients achieved an overall response (ORR 50%), including 8 patients with a complete remission (CR/CRi 44%) and 1 (6%) patient with a morphologic leukemia free state, Figure 1. All six of the responders who were tested for MRD were negative. For treatment naïve patients, we observed a CR/CRi rate of 70% and a median survival of 11 months. On univariate analysis, R/R disease was the only factor associated with a significant decrease in response (ORR 12.5% vs. 80%, p=0.015, Table 1). With a median follow-up of 14.4 months for responding patients, median OS for the cohort was 6.59 months and 19.15 months for responding patients (Figure 2). The presence of NRAS or KRAS mutations was the only factor significantly impacting survival (HR 6.04, log rank 0.05, Table 1). Notably, the KMT2A fusion partner type did not impact response or survival. Allogeneic stem cell transplant was performed in 4 out of 9 (44%) responding patients.
Conclusion
Here, we show that venetoclax in combination with HMA led to a high rate of response and prolonged survival in a high-risk KMT2A rAML population. The outcomes of newly diagnosed KMT2A rAML patients after treatment with venetoclax and HMA in this study are similar to chemotherapy outcomes in patients aged < 60 years (CR 68% and median OS 0.9 months; Bill, M et al. PNAS. 2020). Consistent with previous studies, we found that MLLT3 was the most common fusion partner, occurring in 50% of patients and that RAS mutations were also common (~30%). In contrast to what has been reported for chemotherapy outcomes and in the ELN classification, the KMT2A-MLLT3 translocation was not associated with improved outcomes when compared to other KMT2A translocations. While this study was limited in being retrospective and having a small and heterogeneous population, our findings suggest that venetoclax and HMA are effective in KMT2A rAML and warrant further investigation.
Koller: Novartis: Consultancy. Al Malki: Hansa Biopharma: Consultancy; Rigel Pharma: Consultancy; Neximmune: Consultancy; Jazz Pharmaceuticals, Inc.: Consultancy; CareDx: Consultancy. Aribi: Seagen: Consultancy. Ali: Incyte: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Speakers Bureau; CTI BioPharma: Membership on an entity's Board of Directors or advisory committees. Marcucci: Novartis: Other: Speaker and advisory scientific board meetings; Agios: Other: Speaker and advisory scientific board meetings; Abbvie: Other: Speaker and advisory scientific board meetings. Pullarkat: AbbVie, Amgen, Genentech, Jazz Pharmaceuticals, Novartis, Pfizer, and Servier: Membership on an entity's Board of Directors or advisory committees; Amgen, Dova, and Novartis: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal