Key Points
BV and Nivo with staggered or concurrent dosing were active and well tolerated when used as first salvage therapy in patients with r/r cHL.
The ORR and CR rate were 85% and 67%, with a 3-year PFS rate of 91% in patients who proceeded directly to transplant.
Abstract
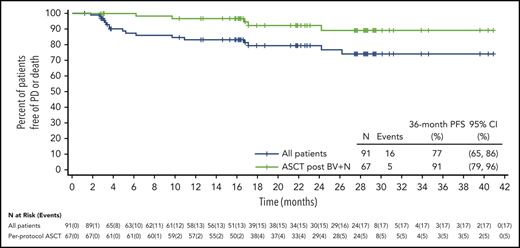
This phase 1-2 study evaluated brentuximab vedotin (BV) combined with nivolumab (Nivo) as first salvage therapy in patients with relapsed/refractory (r/r) classical Hodgkin lymphoma (cHL). In parts 1 and 2, patients received staggered dosing of BV and Nivo in cycle 1, followed by same-day dosing in cycles 2 to 4. In part 3, both study drugs were dosed, same day, for all 4 cycles. At end of study treatment, patients could undergo autologous stem cell transplantation (ASCT) per investigator discretion. The objective response rate (ORR; N = 91) was 85%, with 67% achieving a complete response (CR). At a median follow-up of 34.3 months, the estimated progression-free survival (PFS) rate at 3 years was 77% (95% confidence interval [CI], 65% to 86%) and 91% (95% CI, 79% to 96%) for patients undergoing ASCT directly after study treatment. Overall survival at 3 years was 93% (95% CI, 85% to 97%). The most common adverse events (AEs) prior to ASCT were nausea (52%) and infusion-related reactions (43%), all grade 1 or 2. A total of 16 patients (18%) had immune-related AEs that required systemic corticosteroid treatment. Peripheral blood immune signatures were consistent with an activated T-cell response. Median gene expression of CD30 in tumors was higher in patients who responded compared with those who did not. Longer-term follow-up of BV and Nivo as a first salvage regimen shows durable efficacy and impressive PFS, especially in patients who proceeded directly to transplant, without additional toxicity concerns. This trial was registered at www.clinicaltrials.gov as #NCT02572167.
Introduction
Approximately 10% to 30% of patients with classical Hodgkin lymphoma (cHL) are refractory to initial therapy or relapse after standard therapies.1-4 Standard of care for these patients is salvage chemotherapy followed by autologous stem cell transplantation (ASCT). Achieving a complete metabolic response (CMR) after salvage chemotherapy is associated with significantly higher long-term relapse-free survival post-ASCT; therefore, identifying well-tolerated regimens that achieve high complete response (CR) rates pre-ASCT is important.5
Brentuximab vedotin (BV) is an antibody-drug conjugate directed to CD30, expressed on Reed-Sternberg cells and a small population of normal activated T and B cells (supplemental Figure 1, available on the Blood Web site). In addition to direct cytotoxicity, BV may activate the innate immune system and initiate an antitumor immune response by induction of immunogenic cell death via endoplasmic reticulum stress.6,7 In a phase 2 study of single-agent BV in patients with relapsed/refractory (r/r) cHL, the objective response rate (ORR) and CR rate were 72% and 33%, respectively.8,9 In additional phase 2 studies, sequential BV followed by chemotherapy reserved for patients with residual disease, or BV combined with chemotherapy, are effective salvage approaches prior to ASCT.10-12
Nivolumab (Nivo) is a monoclonal antibody that targets programmed cell death protein 1 (PD-1), blocking the interaction with ligands overexpressed by Reed-Sternberg cells, to restore an effective antitumor immune response. In patients with r/r cHL treated with Nivo, the ORR and CR rate were 73% and 28%, respectively.13 Both BV and Nivo are well tolerated with distinct mechanisms and demonstrated single-agent activity in cHL, and it is plausible that a combination of both agents could achieve a higher CR rate and minimize chemotherapy exposure, while being administered in an outpatient setting.
This phase 1-2 study evaluated BV in combination with Nivo as first salvage therapy in patients with r/r cHL. In an interim analysis at a median follow-up of 7.8 months, the combination was found to be active and well tolerated, with an ORR and CR rate of 82% and 61%, respectively.14 This report presents safety and efficacy results in all treated patients, including patients treated with sequential or concurrent dosing of BV and Nivo, as well as the long-term follow-up (LTFU) results with a median follow-up of 34.3 months.
Methods
Patients
This multicenter, single-arm, phase 1-2 trial (NCT02572167) enrolled adults with biopsy-proven primary refractory (ie, not achieving a CR or progression <3 months after CR) or relapsed Hodgkin lymphoma (HL; progression ≥3 months after CR). The study consisted of parts 1/2 and part 3, which was initiated by an amendment to the protocol (supplemental Figure 2). Patients with prior salvage therapy (including radiotherapy), prior BV (parts 1/2 only) or immuno-oncology therapy, or prior autologous or allogeneic stem cell transplantation were excluded.15 In part 3, patients refractory to a BV-containing regimen or who discontinued BV due to unacceptable toxicity were ineligible. Written informed consent was obtained from the patient or legally authorized representative in accordance with institutional policies. The study protocol and amendments were approved by site institutional review boards and conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practices.
Procedures
Patients were staged with a positron emission tomography (PET) scan and a dedicated contrast-enhanced computed tomography (CT) scan, and received up to 4 cycles of BV 1.8 mg/kg every 3 weeks IV over 30 minutes followed by Nivo 3.0 mg/kg IV over 60 minutes. In parts 1/2 (staggered dosing), BV was administered on day 1 and Nivo on day 8 of cycle 1, with both agents administered on day 1 during cycles 2 to 4. During part 2, the protocol was amended to mandate prophylactic treatment with steroids (hydrocortisone 100 mg or equivalent) and antihistamines (diphenhydramine 25-50 mg or equivalent) at day 1 of each cycle beginning at cycle 2. Patients in part 3 (same-day dosing) received both BV and Nivo on day 1 of all cycles, based on the interim efficacy and safety results in parts 1 and 2 of this study and encouraging results with same-day dosing of both agents in the Eastern Cooperative Oncology Group and the American College of Radiology Imaging Network (ECOG-ACRIN) study E4412.16 Mandatory prophylactic treatment with steroids was not required in part 3. After the end of response assessment, patients could undergo per-protocol ASCT at physician discretion.
Antitumor activity was assessed according to the Lugano Classification Revised Staging System for malignant lymphoma,17 with the incorporation of the Lymphoma Response to Immunomodulatory Therapy Criteria (LYRIC)18 for part 3. Additional salvage therapy prior to ASCT or post-ASCT consolidative therapies (eg, additional BV or radiation) was performed at physician discretion according to institutional practices.
After cycle 2, a CT scan of diagnostic quality was performed. Patients in parts 1 and 2 with radiographic evidence of progressive disease (PD) and patients in part 3 with confirmed unequivocal PD were not eligible for further treatment on the study. At the end of planned treatment, response was evaluated by PET and CT scans (15-37 days after last dose), and for patients with a CMR (Deauville score ≤3), subsequent protocol assessments were conducted by CT scan only. For patients in part 3 with suspected tumor flare or pseudoprogression, response was scored as indeterminate per LYRIC criteria until a biopsy was performed to either confirm or refute PD or subsequent evaluation at 12 weeks was conducted.
Adverse events (AEs) and serious AEs, regardless of relationship to study drug, were recorded from study day 1 through 100 days after the last dose of Nivo and included the ASCT period, as applicable. Safety was monitored by a safety monitoring committee.
Outcome measures
The primary objectives were to assess the safety profile and antitumor activity of BV in combination with Nivo. Secondary objectives were to assess ORR, response duration, and progression-free survival (PFS) rate after ASCT. Additional objectives included assessment of overall survival (OS) and PFS, the proportion of patients able to mobilize adequate CD34+ stem cells after combination treatment, the effect of dosing schedule on biomarkers, and the effect of tumor microenvironment and peripheral immune status. The method used for stem cell mobilization was at the discretion of the investigator.
Statistical analysis
ORR and CR rate, with 2-sided 95% exact binomial confidence intervals (CIs),19 were determined based on overall best response prior to ASCT or initiation of subsequent antitumor treatment. Duration of response and PFS were estimated using Kaplan-Meier, and the 95% CI was calculated using log-log transformation.20 Duration of response was defined as the time from first documentation of objective response to the first documentation of PD or death due to any cause. PFS was defined as the time from enrollment to the first documentation of PD or death due to any cause.
AEs were classified using the Medical Dictionary for Regulatory Activities (MedDRA), version 23.0, with a standard MedDRA query performed to identify events of peripheral neuropathy (PN). Grade of severity was determined per National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.03. AEs that were (1) from a list of predefined preferred terms representing potential immune-related AEs (IrAEs) and (2) required treatment with systemic steroids were summarized as being potentially immune related.
Biomarker assessment
Multiple flow cytometry panels were performed by Q2 Solutions (Marietta, GA) on heparinized whole blood. Serum cytokines and chemokines were evaluated by enzyme-linked immunosorbent assay at Covance (Greenfield, IN) and the Luminex platform at Myriad RBM (Austin, TX); for a list of the serum cytokines and chemokines evaluated, see supplemental Methods. Peripheral blood mononuclear cells were sent to Adaptive Biotechnologies (Seattle, WA) for T-cell receptor β sequencing (immunoSEQ).
RNA sequencing (RNA-Seq) libraries were prepared from archived tumor tissue at relapse using the Illumina RNA-Seq Access protocol and sequenced to 30 million 100-bp paired-end reads. Sequences were aligned using STAR, and transcript abundance was quantified using RSEM. Samples with >60% uniquely aligned reads were analyzed. Expression levels were standardized by scaling to total library size.
Results
Patients
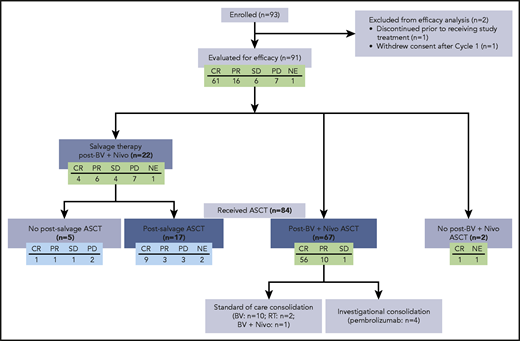
Ninety-three patients with r/r cHL were enrolled at 11 sites from 21 October 2015 to 11 September 2017. Median follow-up, as of the May 2020 data cutoff date, was 34.3 months (range, 1.8-49.9 months). Ninety-one patients received and completed study treatment and were observed through the 100-day safety reporting period. Two enrolled patients did not receive treatment due to consent withdrawal or reasons stated as “other.” Ninety patients entered LTFU for disease progression or death. At data cutoff, 77 patients continued in LTFU, 6 died, 5 were lost to follow-up, and 2 withdrew consent. For all treated patients, the median age was 34 years (range, 18-69 years) (Table 1). At study entry, 42% had primary refractory disease and 30% had relapsed within 1 year of completing frontline therapy, and none received prior BV. Eighty-six patients (92%) completed all 4 cycles of BV and Nivo. Early treatment discontinuations were due to AEs, patient decision (n = 2 each), PD, or investigator decision (n = 1 each). In total, 84 of 91 of all treated patients (92%) ultimately proceeded to ASCT after initiating study therapy (Figure 1). Two patients in a CR after therapy with BV and Nivo did not proceed to ASCT because of Guillain-Barré syndrome (n = 1, see “Safety”) and patient refusal (n = 1).
Baseline demographics and disease characteristics
| . | All treated patients, N = 91 . |
|---|---|
| Median age (range), y | 34 (18, 69) |
| Sex, n (%) | |
| Male | 40 (44) |
| Female | 51 (56) |
| Disease stage at initial diagnosis, n (%) | |
| I | 1 (1) |
| II | 52 (57) |
| III | 16 (18) |
| IV | 20 (22) |
| Unknown | 2 (2) |
| Prior systemic therapy regimens,* n (%) | |
| ABVD | 82 (90) |
| BEACOPP | 2 (2) |
| Radiation | 18 (20) |
| Stanford V | 3 (3) |
| Other | 8 (9) |
| Best response to prior line of therapy, n (%) | |
| CR | 52 (57) |
| PR | 11 (12) |
| SD | 3 (3) |
| PD | 24 (26) |
| Unknown | 1 (1) |
| No. of prior therapies, including radiation | |
| Mean (STD) | 1.2 (0.5) |
| Median | 1.0 |
| Minimum, maximum | 1, 3 |
| Disease status relative to frontline treatment, n (%) | |
| Primary refractory | 38 (42) |
| PR or SD to frontline therapy | 13 (14) |
| PD to frontline therapy | 24 (26) |
| Unknown response to frontline therapy | 1 (1) |
| Relapsed, remission duration ≤1 y | 27 (30) |
| Relapsed, remission duration >1 y | 26 (29) |
| ECOG performance status, n (%) | |
| Grade 0 | 58 (64) |
| Grade 1 | 32 (35) |
| Bulky disease at baseline, n (%) | 12 (13) |
| Extranodal disease at baseline, n (%) | 24 (26) |
| . | All treated patients, N = 91 . |
|---|---|
| Median age (range), y | 34 (18, 69) |
| Sex, n (%) | |
| Male | 40 (44) |
| Female | 51 (56) |
| Disease stage at initial diagnosis, n (%) | |
| I | 1 (1) |
| II | 52 (57) |
| III | 16 (18) |
| IV | 20 (22) |
| Unknown | 2 (2) |
| Prior systemic therapy regimens,* n (%) | |
| ABVD | 82 (90) |
| BEACOPP | 2 (2) |
| Radiation | 18 (20) |
| Stanford V | 3 (3) |
| Other | 8 (9) |
| Best response to prior line of therapy, n (%) | |
| CR | 52 (57) |
| PR | 11 (12) |
| SD | 3 (3) |
| PD | 24 (26) |
| Unknown | 1 (1) |
| No. of prior therapies, including radiation | |
| Mean (STD) | 1.2 (0.5) |
| Median | 1.0 |
| Minimum, maximum | 1, 3 |
| Disease status relative to frontline treatment, n (%) | |
| Primary refractory | 38 (42) |
| PR or SD to frontline therapy | 13 (14) |
| PD to frontline therapy | 24 (26) |
| Unknown response to frontline therapy | 1 (1) |
| Relapsed, remission duration ≤1 y | 27 (30) |
| Relapsed, remission duration >1 y | 26 (29) |
| ECOG performance status, n (%) | |
| Grade 0 | 58 (64) |
| Grade 1 | 32 (35) |
| Bulky disease at baseline, n (%) | 12 (13) |
| Extranodal disease at baseline, n (%) | 24 (26) |
ABVD, adriamycin bleomycin vinblastine dacarbazine; BEACOPP, bleomycin etoposide adriamycin cyclophosphamide oncovin procarbazine prednisone; ECOG, Eastern Cooperative Oncology Group; PD, progressive disease; PR, partial response; SD, stable disease; STD, standard deviation
Patients may have received >1 therapy.
Therapy following study treatment, including ASCT. Of 91 patients evaluated for efficacy, 84 patients underwent ASCT, including 67 patients who did so directly after treatment with BV and Nivo. Two patients did not undergo ASCT after treatment with BV and Nivo. A total of 22 patients received salvage therapy after treatment with BV and Nivo. NE, not evaluable; PR, partial response; RT, radiation therapy; SD, stable disease.
Therapy following study treatment, including ASCT. Of 91 patients evaluated for efficacy, 84 patients underwent ASCT, including 67 patients who did so directly after treatment with BV and Nivo. Two patients did not undergo ASCT after treatment with BV and Nivo. A total of 22 patients received salvage therapy after treatment with BV and Nivo. NE, not evaluable; PR, partial response; RT, radiation therapy; SD, stable disease.
Clinical activity
All treated patients
The ORR for all treated patients was 85%, with 67% CR (Table 2). A decrease in tumor volume and metabolic activity was observed in 97% and 93% of efficacy-evaluable patients, respectively (Figure 2, panels A and B, respectively). In part 1/2, a patient with a residual fluorodeoxyglucose (FDG)-avid lesion (Deauville score 5) following study treatment was considered as having a CR as biopsy results showed no evidence of HL. In part 3, 5 patients had an indeterminate response 2 (IR2) at end of therapy (Deauville score 4-5). Of these, 4 had no evidence of HL on biopsy and were considered to be in a CR. In the fifth case, there was no anatomic CT scan correlate to the FDG+ site, and this patient was also considered to have achieved a CR. Subgroup analyses, which include response rates according to response to frontline therapy, are summarized by disease status in supplemental Table 1 and disease stage in supplemental Table 2.
Best clinical response and Deauville 5-point scale
| . | All treated patients, N = 91 . | |
|---|---|---|
| n (%) . | 95% CI . | |
| Objective response rate (CR + PR) | 77 (85) | 75.5, 91.3 |
| CMR/CR | 61 (67) | 56.4, 76.5 |
| Deauville score = 1 | 23 (25) | |
| Deauville score = 2 | 20 (22) | |
| Deauville score = 3 | 12 (13) | |
| Deauville score = 4* | 2 (2) | |
| Deauville score = 5* | 4 (4) | |
| PMR/PR | 16 (18) | 10.4, 27 |
| Deauville score = 4 | 9 (10) | |
| Deauville score = 5 | 7 (8) | |
| NMR/SD | 5 (5) | 1.8, 12.4 |
| Deauville score = 4 | 1 (1) | |
| Deauville score = 5 | 4 (4) | |
| PMD/PD | 7 (8) | 3.1, 15.2 |
| Deauville score = 5 | 7 (8) | |
| Not evaluable | 1 (1) | |
| Not applicable† | 1 (1) | |
| . | All treated patients, N = 91 . | |
|---|---|---|
| n (%) . | 95% CI . | |
| Objective response rate (CR + PR) | 77 (85) | 75.5, 91.3 |
| CMR/CR | 61 (67) | 56.4, 76.5 |
| Deauville score = 1 | 23 (25) | |
| Deauville score = 2 | 20 (22) | |
| Deauville score = 3 | 12 (13) | |
| Deauville score = 4* | 2 (2) | |
| Deauville score = 5* | 4 (4) | |
| PMR/PR | 16 (18) | 10.4, 27 |
| Deauville score = 4 | 9 (10) | |
| Deauville score = 5 | 7 (8) | |
| NMR/SD | 5 (5) | 1.8, 12.4 |
| Deauville score = 4 | 1 (1) | |
| Deauville score = 5 | 4 (4) | |
| PMD/PD | 7 (8) | 3.1, 15.2 |
| Deauville score = 5 | 7 (8) | |
| Not evaluable | 1 (1) | |
| Not applicable† | 1 (1) | |
CMR/CR, PMR/PR, NMR/SD, and PMD/PD per Lugano classification 2014,17 with PET scan assessment required to determine response. CMR/CR, PMR/PR, NMR/SD, PMD/PD, CP, and not evaluable are mutually exclusive. Patients with both PMD/PD and clinical progression are counted as PMD/PD.
CMR, complete metabolic response; NMR, no metabolic response; PMD, progressive metabolic disease; PMR, partial metabolic response; PR, partial response; SD, stable disease.
Five patients in part 3 with CR met LYRIC criteria for IR-2 (4 with negative biopsies; 1 false positive with no corresponding lesion on CT scan). One patient in part 1/2 had a residual FDG-avid lesion (Deauville score of 5) following study treatment but was considered CR because a biopsy showed no evidence of HL.
No postbaseline assessment.
Percentage change in the sum of the product of diameters and maximum percent change in the standard uptake value in efficacy evaluable patients (n = 90). Sum of the product of diameters (SPD; A) and maximum standard uptake value (SUV; B) percentage changes are calculated from the baseline SPD/SUV to the minimum postbaseline SPD/SUV measured prior to initiation of subsequent chemotherapy or radiotherapy (including conditioning regimen for ASCT). Best response was determined per Lugano 2014,17,18 with PET scanning required until assessment of CMR or PD. Patients without postbaseline tumor assessment are excluded.
Percentage change in the sum of the product of diameters and maximum percent change in the standard uptake value in efficacy evaluable patients (n = 90). Sum of the product of diameters (SPD; A) and maximum standard uptake value (SUV; B) percentage changes are calculated from the baseline SPD/SUV to the minimum postbaseline SPD/SUV measured prior to initiation of subsequent chemotherapy or radiotherapy (including conditioning regimen for ASCT). Best response was determined per Lugano 2014,17,18 with PET scanning required until assessment of CMR or PD. Patients without postbaseline tumor assessment are excluded.
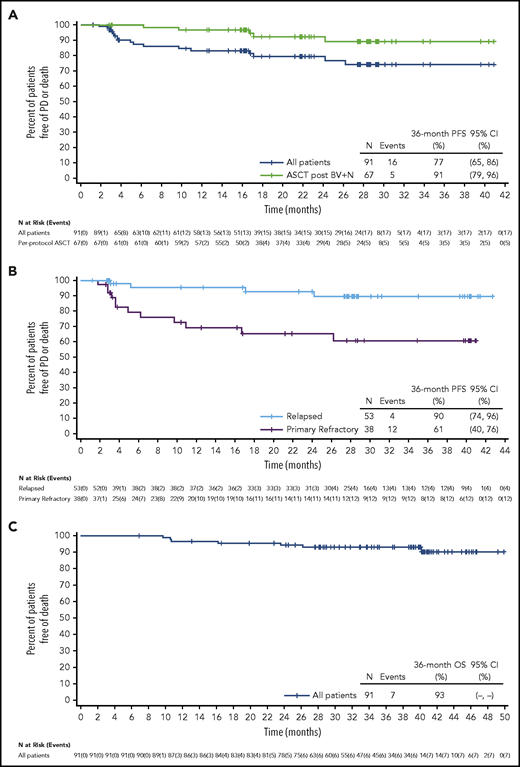
Overall, PD or death without prior PD occurred in 16 of 91 patients (18%). The estimated PFS rate at 3 years was 77% (95% CI, 65% to 86%), and median PFS was not reached (Figure 3A). The PFS rate at 3 years by response to frontline treatment was 90% (95% CI, 74% to 96%) for patients with relapsed disease (n = 53) vs 61% (95% CI, 40% to 76%) for patients with primary refractory disease (n = 38) (Figure 3B). The PFS rate at 3 years by response to study treatment CR (n = 61) vs non-CR (n = 30) was 90% (95% CI, 78% to 96%) vs 42% (95% CI, 19% to 64%), respectively. For patients with partial response (PR) (n = 16, 10 of whom proceeded directly to ASCT), the 3-year PFS rate was 67% (95% CI, 28% to 88%); lastly, the PFS rate at 3 years by remission duration (>1 year, n = 26 vs ≤1 year, n = 27) after frontline treatment was 88% (95% CI, 59% to 97%) vs 91% (95% CI, 68% to 98%).
PFS and OS in patients with r/r HL. (A) PFS in all treated patients (blue line) compared with the subset of patients who received per-protocol ASCT (without prior additional salvage; green line). Patients who started an antitumor therapy (excluding stem cell transplant or post-ASCT consolidative therapy) other than the study treatment prior to documentation of tumor progression were censored at the date of the most recent disease assessment prior to start of new therapy that was adequate to document progressive disease. (B) PFS in patients with relapse disease at study entry vs primary refractory patients. (C) OS in all treated patients.
PFS and OS in patients with r/r HL. (A) PFS in all treated patients (blue line) compared with the subset of patients who received per-protocol ASCT (without prior additional salvage; green line). Patients who started an antitumor therapy (excluding stem cell transplant or post-ASCT consolidative therapy) other than the study treatment prior to documentation of tumor progression were censored at the date of the most recent disease assessment prior to start of new therapy that was adequate to document progressive disease. (B) PFS in patients with relapse disease at study entry vs primary refractory patients. (C) OS in all treated patients.
Overall, there were 7 deaths among all treated patients in the study, none of which occurred during the safety reporting period. Four were disease related including 3 due to PD and 1 due to acute neutropenic colitis occurring >2 years after end of study treatment. One death was non–disease related due to organizing pneumonia and occurred >8 months after the end of study treatment. Two deaths were due to unknown causes with each occurring >15 months after the end of study treatment. The estimated OS rate at 3 years was 93% (95% CI, 85% to 97%) (Figure 3C), with the median not reached.
Patients with per-protocol ASCT
Sixty-seven patients (74%) underwent per-protocol ASCT (defined as ASCT directly after treatment with 4 cycles of BV and Nivo, without additional salvage) (Figure 1). Best responses to study treatment prior to ASCT in these patients included 56 patients with CR, 10 with PR, and 1 with stable disease (SD).
The median time from end of treatment to the start of stem cell mobilization was 9.5 days (range, −13 to 46 days). A median 5.5 × 106 CD34+ cells per kg were collected (range, 1 × 106 to 60 × 106 CD34+ cells per kg) in a median of 1 apheresis session (range, 1-5). Median times to neutrophil and platelet engraftment were 12 days (range, 8-29 days) and 16 days (range, 4-114 days), respectively.
Among 67 patients who proceeded directly to ASCT (56 CR, 10 PR, and 1 SD), the estimated PFS rate at 3 years was 91% (95% CI, 79% to 96%) (Figure 3A). This rate was 95% (95% CI, 83% to 99%) for patients in a CR and 67% (95% CI, 28% to 88%) for those in a PR. The median PFS rate was not reached. At the time of the data cutoff, 5 patients (7%) had an event (n = 4 PD; n = 1 death). The estimated PFS rate post-ASCT (defined as the time from stem cell infusion to first documentation of disease progression or death) at 3 years was 91% (95% CI, 79% to 96%), and median PFS rate was not reached.
Seventeen patients received additional consolidation therapy prior to ASCT. Before transplant, 10 patients were in a CR, 6 in a PR, and 1 had SD. Consolidation in the CR patients included BV (n = 5), pembrolizumab (n = 3), BV and Nivo (n = 1), and radiotherapy (n = 1). For this group, the estimated PFS rate at 3 years was 100% (95% CI, 100% to 100%). For the 7 patients not in a CR, consolidation consisted of BV (n = 5), pembrolizumab (n = 1), and radiotherapy (n = 1), with an estimated PFS at 3 years of 63% (95% CI, 14% to 89%). For the 46 patients in a CR who received ASCT without additional consolidation, the estimated PFS rate at 3 years was 95% (95% CI, 82% to 99%).
Outcomes of patients with additional salvage therapy
Twenty-two patients who did not undergo per-protocol ASCT received a median of 1 additional salvage therapy (range, 1-5) (supplemental Table 3). After BV and Nivo treatment, 4 of these patients were in a CR, 6 in a PR, 4 had SD, 7 had PD, and 1 was not evaluable. Three of 4 patients with a CR received additional salvage therapy due to delays in transplant. One patient had a partial metabolic response that was later revised to a CMR when it was determined that the FDG uptake was not due to lymphoma. Overall, 17 of 22 patients (77%) underwent ASCT after receiving additional salvage treatment, whereas 5 patients (23%) did not.
Safety
A total of 90 patients (99%) had treatment-emergent AEs prior to per-protocol ASCT. The most common treatment-emergent AEs were nausea in 47 patients (52%), infusion-related reactions (IRRs) in 39 patients (43%), and fatigue in 36 patients (40%), all grades 1 and 2, except 1 incidence of grade 3 fatigue. Two patients (2%) discontinued treatment due to AEs (1 each with grade 3 PN and increased γ-glutamyltransferase). Peripheral sensory neuropathy was reported by 16 patients (18%), all grade 1 except for 1 grade 3 (not specified) PN that led to treatment discontinuation. Other grade 3 or higher AEs occurred in 30 patients (33%) (supplemental Table 4), including neutropenia (n = 4 grade 3; n = 1 grade 4). IRRs in parts 1 and 2 and in part 3 occurred in 28 patients (46%) and 11 patients (37%), respectively, mostly at cycle 2 (34% and 23%, respectively).
Across all study parts, immunosuppressive treatment (systemic corticosteroids) was administered to 16 patients (18%) for potential IrAEs, excluding IRRs (supplemental Table 5). No patient discontinued study treatment due to an IrAE. Grade 3 or higher IrAEs included pneumonitis in 3 patients (3%), and maculopapular rash, increased aspartate aminotransferase, diarrhea, and Guillain-Barré syndrome each occurring in 1 patient (1%). All 3 patients with grade 3 or higher pneumonitis events were treated successfully with systemic corticosteroids. All events in the 3 patients with pneumonitis occurred ∼2 to 4 months after the last dose of study therapy. In 2 patients, pneumonitis developed ∼1 to 2 months after ASCT, and in 1 patient during subsequent therapy with ifosfamide, carboplatin, and etoposide before proceeding to ASCT. Of the 3 patients, 2 remain in LTFU whereas 1 patient died of PD >3 years after the last doses of BV and Nivo. The Guillain-Barré event occurred ∼4 weeks after the patient received the last doses of BV and Nivo. The patient was treated with IV immunoglobulin and plasma exchange with improvement. The patient had PD ∼3 months after the last doses of BV and Nivo, was treated with ifosfamide, carboplatin, and etoposide, but did not proceed to ASCT.
AEs leading to dose delay of BV or Nivo occurred in 10 patients (11%) and 11 patients (12%), respectively. Events leading to BV dose delay in >1 patient included neutropenia and hyperlipasemia (n = 2 each). Events leading to Nivo dose delay in >1 patient included neutropenia only (n = 2). All patients were able to receive another dose of the delayed drug, and all but 1 patient who experienced a dose delay received 4 cycles of treatment.
Biomarker analyses
Pharmacodynamic signatures of activity
Flow cytometric evaluation of peripheral blood from part 1/2 revealed a 20% decrease of T-regulatory cells at cycle 1, day 8 (C1D8), as well as reductions in activated and dividing T cells (Figure 4).15 Within 1 to 2 weeks after the first dose of Nivo, counts for these cell types increased up to 70% above baseline, consistent with an activated immune response. In part 3, the C1D8 reductions observed in part 1/2 were not statistically significant except for CD4+ T-cell counts, and by cycle 1, day 15/cycle 2, day 1 (C1D15/C2D1), the T-cell expansion observed in part 1/2 was amplified from 25% to 150% above baseline in the T-cell subpopulations analyzed (Figure 4A). Changes in CD8+ T-cell counts were greater in part 3, with dividing CD8+ T cells expanding by 133% compared with 31% in part 1/2.
T-cell response and cytokine changes over time in peripheral blood. (A) Median percentage change from baseline of patient peripheral circulating T-cell subtypes. Dividing T cells were identified by Ki-67+, activated T cells by HLA-DR+, regulatory T cells by CD4+/CD127−/CD25hi/CCR4+. Cell counts were derived from a dual platform method of no-wash absolute T-cell quantification and T-cell subtype percentages. Boxes indicate the interquartile range, horizontal white lines indicate the median values, and the bars extend to the upper and lower adjacent values. (B) Average fold change of cytokines over all patients compared with baseline. (C) Change from baseline in levels of IP-10, IL-18, and IFN-γ in 2 treatment parts over time. Boxes indicate the interquartile range, horizontal black lines indicate the median values, and the bars extend to the upper and lower adjacent values. P values for all panels were generated by Student t test. APRIL, a proliferation inducing ligand; BAFF, B-cell–activating factor; BDNF, brain-derived neurotrophic factor; BSLN, baseline; LAP, latency associated peptide; MCP, monocyte chemoattractant protein; MIG, monokine induced by IFN-γ; MIP, macrophage inflammatory protein; MMP, matrix metalloproteinase; MPIF, myeloid progenitor inhibitory factor; sCD30, soluble CD30; SCF, stem cell factor; SDF, stromal cell–derived factor; TGF, transforming growth factor; TNF, tumor necrosis factor.
T-cell response and cytokine changes over time in peripheral blood. (A) Median percentage change from baseline of patient peripheral circulating T-cell subtypes. Dividing T cells were identified by Ki-67+, activated T cells by HLA-DR+, regulatory T cells by CD4+/CD127−/CD25hi/CCR4+. Cell counts were derived from a dual platform method of no-wash absolute T-cell quantification and T-cell subtype percentages. Boxes indicate the interquartile range, horizontal white lines indicate the median values, and the bars extend to the upper and lower adjacent values. (B) Average fold change of cytokines over all patients compared with baseline. (C) Change from baseline in levels of IP-10, IL-18, and IFN-γ in 2 treatment parts over time. Boxes indicate the interquartile range, horizontal black lines indicate the median values, and the bars extend to the upper and lower adjacent values. P values for all panels were generated by Student t test. APRIL, a proliferation inducing ligand; BAFF, B-cell–activating factor; BDNF, brain-derived neurotrophic factor; BSLN, baseline; LAP, latency associated peptide; MCP, monocyte chemoattractant protein; MIG, monokine induced by IFN-γ; MIP, macrophage inflammatory protein; MMP, matrix metalloproteinase; MPIF, myeloid progenitor inhibitory factor; sCD30, soluble CD30; SCF, stem cell factor; SDF, stromal cell–derived factor; TGF, transforming growth factor; TNF, tumor necrosis factor.
T-cell receptor β sequencing revealed an initial clonal contraction at C1D8 followed by a durable expansion, peaking at C1D15/C2D1, and following a temporal course similar to T-cell activation markers (supplemental Figure 3). The contraction observed at C1D8 was less pronounced in part 3, mirroring the observed cellular differences.
Statistically significant changes to inflammatory-associated serum cytokine levels were also observed compared with pretreatment with corrected value of P < .05 relative to C1D15 in both treatment parts, including increases in interferon-γ (IFN-γ), interleukin 18 (IL-18), IFN-γ–induced protein 10 (IP-10), and IFN-inducible T-cell α chemoattractant (ITAC) and decreases in IL-2RA, IL-22, and thymus- and activation-regulated chemokine (TARC) (Figure 4B-C). Levels remained significantly altered at cycles 2 and 3. Although changes were observed in levels of IFN-γ, IP-10, and IL-18 in both part 1/2 and part 3, the relative increase in levels was more pronounced with same-day dosing (P = .002, .0001, .01, respectively) at C1D8 than with staggered dosing. The level of change was similar after cycle 2 with both dosing schedules.
Tumor transcript analysis
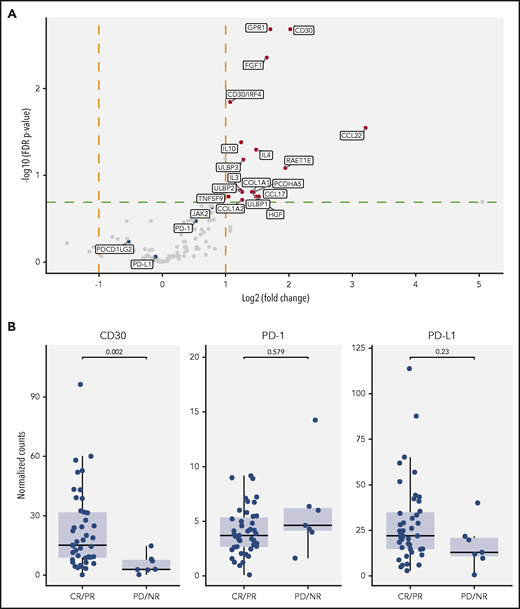
We performed RNA-Seq analysis of tumor biopsies collected at baseline from 50 patients. The panel included 132 markers of immune cells, inflammatory response, and the tumor microenvironment. The CD30 (TNFRSF8) gene was the highest gene (sorted by computed P values) differentially expressed in a comparison of patients who achieved CR/PR vs those with PD/SD (fourfold change) (Figure 5A). Expression of CCL22, IL-4, TARC, and IL-10 was also higher in CR/PR patients than PD/SD. No significant association between PD-1 or programmed death ligand 1 (PD-L1) gene expression and clinical activity was observed (Figure 5B).
Comparison of pretreatment tumor gene expression in patients with CR/PR and PD/NR. (A) Volcano plot showing the fold change and associated P values (Student t test) from a comparison of the expression of 132 selected genes in CR/PR vs PD/NR patients. The red dots represent genes found to be differentially expressed by predefined thresholds (log2 fold change >1 and false discovery rate (FDR)-corrected value of P < .2). (B) Baseline gene expression levels of CD30, PD-1, and PD-L1 among patients with different clinical activity. Gene expression is reported as counts per million sequenced reads. Boxes indicate the interquartile range, horizontal black lines indicate the median values, and the bars extend to the upper and lower adjacent values. FGF, fibroblast growth factor; GPR, G-protein–coupled receptor; HGF, hepatocyte growth factor; IRF, IFN-regulatory factor; NR, no response; ULBP, UL16-binding protein.
Comparison of pretreatment tumor gene expression in patients with CR/PR and PD/NR. (A) Volcano plot showing the fold change and associated P values (Student t test) from a comparison of the expression of 132 selected genes in CR/PR vs PD/NR patients. The red dots represent genes found to be differentially expressed by predefined thresholds (log2 fold change >1 and false discovery rate (FDR)-corrected value of P < .2). (B) Baseline gene expression levels of CD30, PD-1, and PD-L1 among patients with different clinical activity. Gene expression is reported as counts per million sequenced reads. Boxes indicate the interquartile range, horizontal black lines indicate the median values, and the bars extend to the upper and lower adjacent values. FGF, fibroblast growth factor; GPR, G-protein–coupled receptor; HGF, hepatocyte growth factor; IRF, IFN-regulatory factor; NR, no response; ULBP, UL16-binding protein.
Discussion
Among patients with r/r cHL, the combination of BV and Nivo as first salvage therapy, with staggered or concurrent dosing, was active and well tolerated. The ORR and CR rate were 85% and 67%, respectively, which are higher than either agent administered individually. Responses were durable and PFS was high, especially for those who underwent ASCT after study completion without additional salvage therapy. Although the study was not designed to compare same-day and staggered dosing, the results suggest that same-day dosing from the start of combination therapy is feasible. BV administered in combination with Nivo did not negatively impact stem cell mobilization, collection yields, or engraftment.
After a median of 34.3 months of follow-up, no new toxicities were observed with BV and Nivo, and the AE profile of the combination was similar to each agent administered individually.8,9,13 Eighteen percent of patients required treatment with systemic corticosteroids for potential IrAEs, excluding IRRs. The proportion of patients with IRRs was lower in part 3 (37%), which used same-day dosing and an alternative premedication strategy, compared with parts 1/2 (46%). The lack of control groups for the independent treatment components makes interpretation of the IRR incidence difficult. Overall, the combination of BV and Nivo as salvage therapy is associated with mild IRRs and characteristic irAEs in a minority of patients but less hematologic or gastrointestinal toxicity than conventional salvage regimens.
Antitumor activity in this study was assessed according to the Lugano Classification Revised Staging System for malignant lymphoma, with the incorporation of LYRIC criteria for part 3. Five patients in part 3 with a CR met LYRIC criteria for IR-2, including 4 with negative biopsies and 1 false positive with no corresponding lesion on CT scan. One patient in part 1/2 had a residual FDG-avid lesion (Deauville score of 5) following study treatment but was considered a CR as a biopsy showed no evidence of HL. Our findings underscore the importance of biopsy to determine whether a residual FDG-avid area after treatment represents disease or inflammation.
Our results compare favorably with results of other first-line salvage regimens that combine BV with chemotherapy, as well as traditional combination chemotherapy.11,21-23 Conventional salvage treatment with platinum- and gemcitabine-based chemotherapy regimens are associated with ORRs ranging from 70% to 89%,5,24,25 and CR rates from 54% to 73%.5,26,27 Studies of BV monotherapy as initial salvage therapy have reported CR rates of 27% to 43%,11,12,28 whereas sequential BV chemotherapy or BV combined with chemotherapy report CMR rates of 69% to 83%.10,29 In contrast to some chemotherapy-based regimens, BV and Nivo can be administered on an outpatient basis without routine growth factor use, and nearly all patients in the study were able to complete the 4 planned cycles. A limitation of our study was the heterogeneity in subsequent salvage or post-ASCT consolidation therapy received. Nineteen percent of study patients proceeded to ASCT after receiving additional consolidation and outcomes were comparable with those who did not get further consolidation, although the small numbers preclude definitive conclusions. Overall, the excellent PFS observed in patients who proceeded to ASCT directly after BV and Nivo, which represents about three-quarters of the cohort, was not impacted by the heterogeneity of patients receiving additional salvage therapy, as the latter were censored.
The regimen may be particularly useful as a chemotherapy-sparing option in the pre-ASCT salvage setting as evidenced by the 3-year PFS rate of 90% after BV and Nivo as first salvage therapy in the relapsed setting. Notably, the 3-year PFS rate with BV and Nivo was lower among patients with primary refractory disease (61%), highlighting the need for further refinement of treatment regimens for primary refractory HL. Other ongoing investigations of BV and Nivo include CheckMate 744 (NCT02927769), a phase 2 open-label trial of BV and Nivo in pediatric patients and young adults with r/r cHL after first-line treatment, with incomplete responders receiving treatment with BV plus bendamustine. Another study, ECOG-ACRIN E4412 (NCT01896999), has demonstrated that BV and Nivo results in a similar ORR/CR in adults with r/r cHL, including patients receiving 2 or more salvage regimens.30 Arms K and L of the latter study are ongoing, randomizing adult and pediatric patients with r/r cHL to receive BV and Nivo with or without ipilimumab in an effort to improve the CR rate with the regimen. Our study results warrant a randomized study of immunotherapy-based salvage therapy compared with chemotherapy-based salvage therapy.
Immunophenotyping and cytokine analysis in blood were consistent with an activated T-cell response. Some pharmacodynamic effects were affected by dose schedule. Decreases were observed in regulatory, activated, and dividing T-cell counts at C1D8 in all study parts, but the decreases were generally not statistically significant in part 3, presumably because Nivo counteracts the effect of BV on CD30+ T-cell counts with same-day dosing. By the start of the second cycle, decreases in regulatory, activated, and dividing T cells were reversed in all study parts, presumably by release of checkpoint blockade, with cell counts peaking 2 to 3 weeks after first dose. Serum levels of inflammatory-associated cytokines were also altered, with reductions in TARC concurrent with increases in proinflammatory cytokines and chemokines. Dose schedule–specific effects were observed for some cytokines and chemokines, including IFN-γ, IP-10, and IL-18. These observations suggest a more active immune signature with same-day dosing of BV and Nivo compared with staggered dosing.
The median gene expression of CD30 was fourfold higher in tumor samples from patients with CR/PR than from patients with PD/SD; however, responses were observed even among patients with low CD30 expression. No significant association was observed between PD-1 and PD-L1 gene expression and clinical activity.
In summary, BV and Nivo as initial salvage therapy, together with ASCT, was well tolerated and provided durable remissions in a high proportion of patients with r/r cHL. Among patients who proceeded directly to ASCT, the estimated PFS rate at 3 years was 91%. These data continue to support the promise of combining BV and Nivo as a salvage regimen that is highly active and well tolerated and may potentially offer an alternative to chemotherapy-based salvage in patients with r/r cHL.
Acknowledgments
The authors acknowledge Susan Cottrell (Next Medical and Science Writing, funded by Seagen Inc), Jennifer Burton (employee of Seagen Inc), and Gary Dorrell (employee of Seagen Inc) for assistance in manuscript preparation.
This work was supported by direct joint funding from Seagen Inc and Bristol-Myers Squibb. A.F.H. was supported by the Emmet and Toni Stephenson Leukemia & Lymphoma Society Scholar Award, and the Lymphoma Research Foundation Larry and Denise Mason Clinical Investigator Career Development Award.
Authorship
Contribution: R.H.A., A.J.M., N.L.B., J.M.V., R.R., T.A.F., A.S.L., B.A.C., S.M.A., C.H.M., L.B., D.T., S.A., M.S., and A.F.H. conceived and designed the study; R.H.A., A.J.M., N.L.B., J.M.V., R.R., T.A.F., A.S.L., B.A.C., S.M.A., C.H.M., L.B., C.Z., D.T., S.A., M.S., and A.F.H. collected and assembled data; and R.H.A., A.J.M., N.L.B., J.M.V., R.R., T.A.F., A.S.L., B.A.C., S.M.A., C.H.M., L.B., C.Z., D.T., S.A., M.S., L.H., and A.F.H. provided study materials or patients, analyzed and interpreted data, wrote and gave final approval of the manuscript, and are accountable for all aspects of the work.
Conflict-of-interest disclosure: R.H.A. reports research funding from Agensys, Celgene, Forty Seven, Genentech, Infinity Pharma, Janssen, Kura, Merck, Millennium Pharma, Pharmacyclics, Regeneron, and Seagen Inc; and serves as a consultant for AstraZeneca, Autolus, Mayer, Bristol-Myers Squibb, Celmed, Genentech, Gilead, Pharmacyclics, Seagen Inc, and Takeda. A.J.M. and M.S. report research funding from Seagen Inc. N.L.B. serves as an advisory board member and consultant for Kite Pharma, Pfizer, and Seagen Inc; and reports research funding from Affimed Thera, Bristol-Myers Squibb, Celgene, Dynavax, Forty Seven, Genentech, Gilead, Immune Design, Janssen, Kite Pharma, Medimmune, Merck, Millennium, Novartis, Pfizer, Pharmacyclics, and Seagen Inc. J.M.V. reports research funding from Acerta Pharma, Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Incyte Corp, Kite Pharma, Merck, Novartis, and Seagen Inc; and received honoraria from and serves as a consultant for AbbVie, Acerta, AstraZeneca, Epizyme, Janssen/Pharmacyclics, Kite Pharma, Kyopharm, Legend Pharma, Nordic Nanovector, Novartis, Roche, Sandoz, Vaniam Group, and Verastem. R.R. reports research funding from Genentech, Janssen, Merck, and Seagen Inc; and serves as an advisory board member and consultant for Bristol-Myers Squibb, Pharmacyclics, Sandoz-Novartis, and Seagen Inc. T.A.F. serves as an advisory board member and consultant for Bayer, Bristol-Myers Squibb, and Seagen Inc; reports research funding from Amgen, Bristol-Myers Squibb, Celgene, Cell Medica, Corvus, Eisai, Kyowa Hakko Kirin, Pfizer, Portola Pharma, Roche, Seagen Inc, Trillium, and Viracta; received honoraria from AbbVie, Bayer, Bristol-Myers Squibb, Kite Pharma, Pharmacyclics, Takeda, and Seagen Inc; and served on speaker’s bureaus for AbbVie, Celgene, Janssen, Kite Pharma, Pharmacyclics, and Seagen Inc. A.S.L. reports research funding from Seagen Inc; serves on a speaker’s bureau for Research to Practice; and serves as a consultant for Humanigen and Seagen Inc. B.A.C. serves as an advisory board member for Genentech; and reports research funding from Acerta, Bristol-Myers Squibb, Celgene, Genentech, Merck, and Seagen Inc. S.M.A. reports research funding from ADC Therapeutics, Affimed, Bristol-Myers Squibb, A1 Therapeutics, Pfizer, Regeneron, Seagen Inc, and Trillium. C.H.M. reports research funding from ADC Therapeutics, Merck, Pharmacyclics, and Seagen Inc; served as a consultant for Celgene, Genentech, Merck, and Seagen Inc; and received honoraria from Pharmacyclics. L.B., C.Z., D.T., S.A., and L.H. report equity ownership in Seagen Inc. A.F.H. reports research funding from AstraZeneca, Bristol-Myers Squibb, Genentech, Gilead Sciences, Immune Design, Kite Pharma, Merck & Co, Pharmacyclics, and Seagen Inc; and serves as a consultant for Adaptive Biotechnologies, Bristol-Myers Squibb, Gilead/Kite Pharma, and Seagen Inc.
The current affiliation for R.R. is Department of Medicine, University of Tennessee Graduate School of Medicine, Knoxville, TN.
The current affiliation for L.B. is Zymeworks Biopharmaceuticals, Vancouver, BC, Canada.
Correspondence: Ranjana H. Advani, Stanford University Medical Center, 875 Blake Wilbur Dr, Stanford, CA 94305; e-mail: radvani@stanford.edu.
Qualified researchers may request access to certain data and related study documents consistent with the Principles for Responsible Clinical Trial Data Sharing. Further details about data requests can be found at http://www.seattlegenetics.com/patients-healthcare-professionals/clinical-data-requests or by e-mailing ctdr@seagen.com.
Presented in part at the 61st annual meeting of the American Society of Hematology, Orlando, FL, 7-10 December 2019; the 60th annual meeting of the American Society of Hematology, San Diego, CA, 1-4 December 2018; and the 11th International Symposium on Hodgkin Lymphoma, Cologne, Germany, 27-29 October 2018.
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal