Key Points
Contemporary treatment approaches for AITL remain suboptimal.
A novel prognostic AITL score defined low-, intermediate-, and high-risk subgroups with differing outcomes.
Abstract
Angioimmunoblastic T-cell lymphoma (AITL) is a unique subtype of peripheral T-cell lymphoma (PTCL) with distinct clinicopathologic features and poor prognosis. We performed a subset analysis of 282 patients with AITL enrolled between 2006 and 2018 in the international prospective T-cell Project (NCT01142674). The primary and secondary end points were 5-year overall survival (OS) and progression-free survival (PFS), respectively. We analyzed the prognostic impact of clinical covariates and progression of disease within 24 months (POD24) and developed a novel prognostic score. The median age was 64 years, and 90% of patients had advanced-stage disease. Eighty-one percent received anthracycline-based regimens, and 13% underwent consolidative autologous stem cell transplant (ASCT) in first complete remission (CR1). Five-year OS and PFS estimates were 44% and 32%, respectively, with improved outcomes for patients who underwent ASCT in CR1. In multivariate analysis, age ≥60 years, Eastern Cooperative Oncology Group performance status >2, elevated C-reactive protein, and elevated β2 microglobulin were associated with inferior outcomes. A novel prognostic score (AITL score) combining these factors defined low-, intermediate-, and high-risk subgroups with 5-year OS estimates of 63%, 54%, and 21%, respectively, with greater discriminant power than established prognostic indices. Finally, POD24 was a powerful prognostic factor with 5-year OS of 63% for patients without POD24 compared with only 6% for patients with POD24 (P < .0001). These data will require validation in a prospective cohort of homogeneously treated patients. Optimal treatment of AITL continues to be an unmet need, and novel therapeutic approaches are required.
Introduction
Angioimmunoblastic T-cell lymphoma (AITL) is a unique subtype of peripheral T-cell lymphoma (PTCL) accounting for ∼2% of all non-Hodgkin lymphomas and ∼15% to 20% of PTCLs.1,2 AITL is generally a disease of older adults, with a median age at diagnosis of ∼65 years, and is typically characterized by an aggressive course, with progressive lymphadenopathy, hepatosplenomegaly, constitutional symptoms, anemia, and hypergammaglobulinemia.3,4 Histopathologically, AITL is characterized by a clonal T-cell infiltrate along with prominent neovascularization.5 The neoplastic cells express pan T-cell antigens (CD2, CD3, and CD5) and typically express CD4.6 The cell of origin of AITL has been identified as a T follicular helper (TFH) cell, and in the World Health Organization classification of lymphoid neoplasms, AITL now represents a subgroup of PTCLs with TFH phenotype.7 Neoplastic cells express ≥2 (preferably 3) TFH-associated markers, including CD10, BCL6, PD-1/CD279, ICOS, CXCR5, CXCL13, and CD154.7-9 Secondary B-cell proliferations are also commonly observed in AITL and are often positive for Epstein-Barr virus.10-13
In a large international retrospective study of patients treated between 1990 and 2002, outcomes for AITL were poor with 5-year overall survival (OS) and progression-free survival (PFS) estimates of 32% and 18%, respectively.13 In the latter study, there was no difference in outcomes in patients treated with or without anthracyclines. In contrast, the prospective COMPLETE study from the United States and a systematic review and meta-analysis suggested improved outcomes with anthracycline-containing regimens such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).14,15 Retrospective studies evaluating more intensive regimens have suggested improved PFS with the addition of etoposide to CHOP, particularly for younger patients under age 60 years.16,17 A retrospective study from the European Group for Blood and Marrow Transplantation suggested improved outcomes for AITL patients undergoing autologous stem cell transplantation (ASCT) in first complete remission (CR1).18
The present study evaluated outcomes of 282 patients with AITL registered in the T-cell Project (TCP), an international prospective cohort study in patients with mature T-cell and natural killer–cell lymphomas. A key objective of the TCP was to better define the clinical characteristics and survival outcomes of different PTCL subtypes. To our knowledge, this subset analysis represents the largest international prospective AITL cohort reported to date, allowing for a real-world assessment of treatment practices, outcomes, and prognostic factors for patients treated in the contemporary era.
Methods
Patients
We performed a subset analysis of patients with AITL enrolled between September 2006 and February 2018 in the TCP (registered at clinicaltrials.gov under NCT01142674). Seventy-four institutions in 13 countries (Argentina, Brazil, Chile, France, Israel, Italy, South Korea, Slovakia, Spain, Switzerland, England, United States, and Uruguay) served as enrollment sites. The study was conducted in compliance with the Helsinki Declaration, and approval was obtained from the institutional review board at the coordinating center (Modena Cancer Center, University of Modena, and Reggio Emilia, Modena, Italy) and at each participating center per institutional standards, with all patients signing informed consent prior to registration. Consecutive patients with mature T-cell or natural killer–cell lymphomas diagnosed according to the World Health Organization classification of tumors of hematopoietic and lymphoid tissues (editions 2001, 2008, or 2017) were registered into the TCP at initial diagnosis before initiation of treatment.19 Eligible patients were adults (age ≥18 years) with adequate tissue biopsy specimens for diagnosis and available clinical data, including baseline information on disease staging, laboratory parameters at diagnosis, treatment regimens received, and follow-up for at least 5 years. The choice of treatment regimen and consideration of ASCT after CR1 were at the discretion of the treating physician. Full inclusion and exclusion criteria are provided in the study protocol (supplemental Materials, available on the Blood Web site).
The TCP used a central dedicated database. Data were collected on baseline clinical and disease characteristics, first-line treatment, and response evaluation as assessed by the local investigators following standard institutional imaging protocols.20 Survival follow-up was updated until database lock on 30 March 2019. Data on radiotherapy dose and field and Epstein-Barr virus viral load were not routinely collected.
Study end points
The primary end point of the study was OS at 5 years, measured from the date of diagnosis until death from any cause or the date of the last known contact for living patients. The key secondary end point was PFS at 5 years, measured from the time of diagnosis to the date of progressive disease assessment or death from any cause. We also compared outcomes between patients with early progression of disease within 24 months (POD24) after diagnosis and those without POD24.21 Patients were not evaluable for POD24 if they were censored or had died within 24 months without POD. Other exploratory analyses included (1) comparison of outcomes of patients ≤65 years old in CR1 who underwent ASCT vs those who did not, and (2) outcomes by era (2006-2010 [prior to the US Food and Drug Administration (FDA) approval of romidepsin] vs 2011-2018 [reflecting increasing use of novel agents]).
Statistical analysis
Standard descriptive analyses were performed for clinical and demographic end points. Fisher’s exact tests were used to identify associations between categorical variables. Mann-Whitney tests were used to compare median age between groups. Two-tailed values of P < .05 were considered statistically significant. Survival estimates were calculated using the Kaplan-Meier method, and time-to-event distributions were compared using log-rank tests (univariate regression). Cox models were used to investigate the association between survival outcomes and covariates (age ≥60 years, advanced-stage disease, elevated lactic dehydrogenase [LDH], multiple extranodal sites, Eastern Cooperative Oncology Group [ECOG] performance status >2, bone marrow involvement, B symptoms, platelet count <150 000/μL, chemotherapy regimen, and response to therapy) with hazard ratios (HRs) used as a summary measure. Covariates identified to have an independent prognostic effect on PFS were used to create a novel prognostic score (AITL score). The performance of the AITL score was compared with previously published prognostic indices, including the International Prognostic Index (IPI),22 the Prognostic Index for T-cell lymphoma (PIT),23 and the Prognostic Index for AITL (PIAI),4 using a measure of global fit (Akaike’s information criteria [AIC]) and concordance index (Harrell C-statistic), with low AIC values indicating better fit and high Harrell C-statistic values indicating better discrimination.24,25 High-risk disease was defined as IPI ≥3, PIT ≥2, or PIAI ≥2, as previously reported.4,22,23 Statistical analyses were performed using Stata (version 14.2) and SPSS (version 20.0).
Results
Patient characteristics
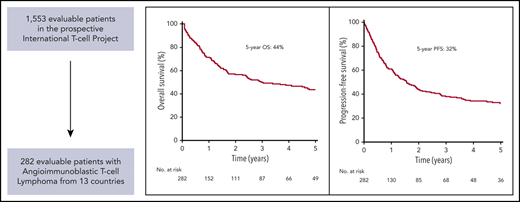
Of 1553 patients eligible for analysis in the TCP, 282 patients (18%) had a diagnosis of AITL (supplemental Figure 1). Biopsy specimens were centrally reviewed in 231 cases (82%), and pathology reports were centrally reviewed for all patients. AITL comprised 7% (22/299), 21% (80/384), 21% (147/689), and 18% (33/181) of all T-cell lymphoma cases registered in South America, North America, Europe, and Asia, respectively, with significantly fewer cases reported in South America compared with the other geographic regions (P = .002). The geographic distribution of patient enrollment is shown in supplemental Table 1. Additional demographic features and patient characteristics are summarized in Table 1. The median age at diagnosis was 64 years (range, 22-88 years), with a male predominance (60%). Ninety percent of patients had advanced-stage disease. Lymphadenopathy was present in 74% of patients, while splenomegaly and hepatomegaly were reported in 31% and 22%, respectively. Polyclonal hypergammaglobulinemia was present in 30% of patients. Skin rash, hemolytic anemia, and other autoimmune phenomena occurred in 14%, 12%, and 10% of patients, respectively.
Patient characteristics
| Parameters . | N . | n . | % . |
|---|---|---|---|
| Age ≥60 y | 282 | 177 | 63 |
| Age ≥70 y | 282 | 107 | 38 |
| Male sex | 282 | 170 | 60 |
| Stage III-IV | 282 | 254 | 90 |
| ECOG performance status >2 | 262 | 80 | 31 |
| B symptoms | 268 | 172 | 64 |
| Bulky disease >5 cm | 282 | 30 | 11 |
| Extranodal sites ≥2 | 268 | 88 | 33 |
| Bone marrow involvement | 268 | 36 | 13 |
| LDH > ULN | 240 | 139 | 58 |
| Hemoglobin <12 g/dL | 261 | 158 | 61 |
| Platelets <150 000/mm3 | 262 | 73 | 28 |
| Monocytes <800/mm3 | 237 | 179 | 76 |
| ANC >6500/mm3 | 251 | 88 | 35 |
| β2M > ULN | 125 | 99 | 79 |
| CRP > ULN | 151 | 108 | 82 |
| IPI ≥3 | 183 | 102 | 56 |
| PIT ≥2 | 183 | 113 | 62 |
| PIAI ≥2 | 183 | 115 | 63 |
| Parameters . | N . | n . | % . |
|---|---|---|---|
| Age ≥60 y | 282 | 177 | 63 |
| Age ≥70 y | 282 | 107 | 38 |
| Male sex | 282 | 170 | 60 |
| Stage III-IV | 282 | 254 | 90 |
| ECOG performance status >2 | 262 | 80 | 31 |
| B symptoms | 268 | 172 | 64 |
| Bulky disease >5 cm | 282 | 30 | 11 |
| Extranodal sites ≥2 | 268 | 88 | 33 |
| Bone marrow involvement | 268 | 36 | 13 |
| LDH > ULN | 240 | 139 | 58 |
| Hemoglobin <12 g/dL | 261 | 158 | 61 |
| Platelets <150 000/mm3 | 262 | 73 | 28 |
| Monocytes <800/mm3 | 237 | 179 | 76 |
| ANC >6500/mm3 | 251 | 88 | 35 |
| β2M > ULN | 125 | 99 | 79 |
| CRP > ULN | 151 | 108 | 82 |
| IPI ≥3 | 183 | 102 | 56 |
| PIT ≥2 | 183 | 113 | 62 |
| PIAI ≥2 | 183 | 115 | 63 |
ANC, absolute neutrophil count; CRP, C-reactive protein; ULN, upper limit of normal.
Treatment regimens and outcomes
Complete treatment details were available in 216 patients, the majority of whom (81%) received anthracycline-containing chemotherapy regimens with or without etoposide (16% and 65%, respectively). The remaining patients received other chemotherapy regimens without anthracyclines (11%) or supportive care (8%). A total of 106 patients treated with curative intent achieved a CR (51%), and 37 had a partial response (18%), for an overall response rate of 69%. Thirteen percent of patients (N = 27) underwent consolidative ASCT in CR1. The decision to undergo ASCT in CR1 was preplanned and varied according to institutional practice. Only 3% of patients received consolidative radiotherapy.
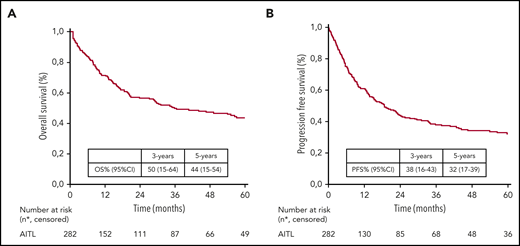
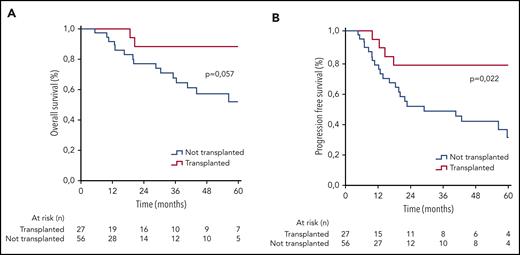
At a median follow-up of 58 months, the 5-year OS and PFS estimates for the entire patient cohort were 44% (95% confidence interval [CI], 15% to 54%) and 32% (95% CI, 17% to 39%), respectively (Figure 1). For patients receiving chemotherapy regimens with and without etoposide, the 5-year OS estimates were 50% (95% CI, 18% to 68%) and 43% (95% CI, 22% to 62%), respectively (P = .769). There was no difference in OS or PFS for patients treated in 2006-2010 (prior to the FDA approval of romidepsin) compared with 2011-2018 (reflecting increasing use of novel agents) (supplemental Figures 2 and 3). Patients who underwent consolidative ASCT in CR1 (n = 27) had superior outcomes compared with transplant-eligible patients (age ≤65 years) who did not undergo ASCT (n = 56) with 5-year OS estimates of 89% and 52%, respectively (P = .05), and 5-year PFS estimates of 79% and 31%, respectively (P = .022) (Figure 2). The characteristics of patients transplanted in CR1 vs those who were not had statistically significant differences in bulky disease (>5 cm), anemia (hemoglobin <12 g/dL), and elevated LDH (supplemental Table 2). In total, 128 deaths were recorded, with 48% of deaths occurring within 1 year from diagnosis and 84% occurring within 2 years from diagnosis. The most common cause of death was progressive disease (69%) followed by infection (16%), second malignancies (1%), and other treatment-related toxicities (3%).
OS and PFS. Kaplan-Meier curves show OS (A) and PFS (B) estimates for the entire study cohort. The 3- and 5-year OS and PFS estimates are listed with 95% CIs. The number of patients under follow-up is listed under the x-axis.
OS and PFS. Kaplan-Meier curves show OS (A) and PFS (B) estimates for the entire study cohort. The 3- and 5-year OS and PFS estimates are listed with 95% CIs. The number of patients under follow-up is listed under the x-axis.
OS and PFS stratified by transplant status in CR1. Kaplan-Meier curves show OS (A) and PFS (B) estimates for patients who underwent autologous stem cell transplantation in first complete remission (red line) vs transplant-eligible patients (age ≤65) who did not undergo transplantation (blue line). The number of patients under follow-up is listed under the x-axis.
OS and PFS stratified by transplant status in CR1. Kaplan-Meier curves show OS (A) and PFS (B) estimates for patients who underwent autologous stem cell transplantation in first complete remission (red line) vs transplant-eligible patients (age ≤65) who did not undergo transplantation (blue line). The number of patients under follow-up is listed under the x-axis.
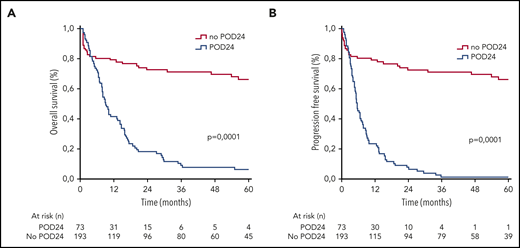
POD24
POD24 occurred in 73 patients (27%), while 193 patients were without disease progression within the first 24 months (73%). Of the 73 patients with POD24, 65 died within 24 months, while only 8 were alive at the last follow-up. POD24 was a powerful prognostic factor, with 5-year OS and PFS estimates of 63% and 48%, respectively for patients without POD24 vs only 6% and 2%, respectively, for patients with POD24 (P < .0001 for both comparisons; Figure 3).
OS and PFS stratified by POD24. Kaplan-Meier estimates of OS (A) and PFS (B) are shown for patients experiencing POD24 (blue line) or without POD24 (red line). The number of patients under follow-up is listed under the x-axis. Outcomes were superior for patients without POD24 (log-rank value of P < .0001 for both comparisons).
OS and PFS stratified by POD24. Kaplan-Meier estimates of OS (A) and PFS (B) are shown for patients experiencing POD24 (blue line) or without POD24 (red line). The number of patients under follow-up is listed under the x-axis. Outcomes were superior for patients without POD24 (log-rank value of P < .0001 for both comparisons).
Prognostic indices
Of the 282 patients in this study, 183 had complete laboratory data to calculate previously reported prognostic indices including the IPI, PIT, and PIAI (Table 2). All prognostic indices identified high-risk subgroups with inferior OS and PFS compared with low-risk patients (Table 3). Patients with high-risk IPI, PIT, and PIAI scores (56%, 62%, and 63% of patients, respectively) had 5-year PFS estimates of 25%, 27%, and 24%, respectively. Patients with low-risk IPI, PIT, and PIAI scores had 5-year PFS estimates of 40%, 37%, and 44%, respectively.
Adverse prognostic factors in AITL
| Adverse prognostic factor . | IPI22 . | PIT23 . | PIAI4 . | AITL score . |
|---|---|---|---|---|
| Age ≥60 y | + | + | + | + |
| ECOG >2 | + | + | + | + |
| LDH > ULN | + | + | ||
| Stage III-IV | + | + | ||
| Extranodal sites ≥2 | + | |||
| Bone marrow involvement | + | |||
| B symptoms | + | |||
| Lymphopenia (<1000/mm3) | + | |||
| Thrombocytopenia (<150 000/mm3) | + | |||
| CRP > ULN | + | |||
| β2M > ULN | + |
Comparison of AITL score with established prognostic indices
| Prognostic index . | IPI . | PIT . | PIAI . | AITL score . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Risk group (score) | Low (0-2) | High (3-5) | Low (0-1) | High (2-4) | Low (0-1) | High (2-5) | Low (0-1) | Intermediate (2) | High (3-4) |
| n (%) | 81/183 (44) | 102/183 (56) | 70/183 (38) | 113/183 (62) | 68/183 (37) | 115/183 (63) | 16/96 (17) | 22/96 (23) | 58/96 (60) |
| Median PFS (95% CI), mo | 34 (12-57) | 8 (5-11) | 29 (18-41) | 9 (4-14) | 46 (13-59) | 13 (7-19) | 31 (13-NR) | 12 (8-16) | 9 (4-15) |
| 5-y PFS (95% CI), % | 40 (21-65) | 25 (9-48) | 37 (17-52) | 27 (9-41) | 44 (14-66) | 24 (8-36) | 41 (17-62) | 37 (9-41) | 13 (7-26) |
| P value | .0006 | .03 | .0006 | .003 | |||||
| Median OS (95% CI), mo | NR | 16 | NR | 17 (4-31) | NR | 24 (1-48) | NR | 35 (14-44) | 20 (6-30) |
| 5-y OS (95% CI), % | 61 (23-79) | 32 (11-51) | 64 (21-81) | 29 (10-50) | 61 (14-72) | 36 (14-49) | 63 (20-68) | 54 (10-67) | 21 (11-32) |
| P | .0005 | .0002 | .001 | .0003 | |||||
| Harrell C-statistic | 0.697 | 0.648 | 0.711 | 0.785 | |||||
| AIC global fit | 566.4 | 575.3 | 543.4 | 524.0 | |||||
| Prognostic index . | IPI . | PIT . | PIAI . | AITL score . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Risk group (score) | Low (0-2) | High (3-5) | Low (0-1) | High (2-4) | Low (0-1) | High (2-5) | Low (0-1) | Intermediate (2) | High (3-4) |
| n (%) | 81/183 (44) | 102/183 (56) | 70/183 (38) | 113/183 (62) | 68/183 (37) | 115/183 (63) | 16/96 (17) | 22/96 (23) | 58/96 (60) |
| Median PFS (95% CI), mo | 34 (12-57) | 8 (5-11) | 29 (18-41) | 9 (4-14) | 46 (13-59) | 13 (7-19) | 31 (13-NR) | 12 (8-16) | 9 (4-15) |
| 5-y PFS (95% CI), % | 40 (21-65) | 25 (9-48) | 37 (17-52) | 27 (9-41) | 44 (14-66) | 24 (8-36) | 41 (17-62) | 37 (9-41) | 13 (7-26) |
| P value | .0006 | .03 | .0006 | .003 | |||||
| Median OS (95% CI), mo | NR | 16 | NR | 17 (4-31) | NR | 24 (1-48) | NR | 35 (14-44) | 20 (6-30) |
| 5-y OS (95% CI), % | 61 (23-79) | 32 (11-51) | 64 (21-81) | 29 (10-50) | 61 (14-72) | 36 (14-49) | 63 (20-68) | 54 (10-67) | 21 (11-32) |
| P | .0005 | .0002 | .001 | .0003 | |||||
| Harrell C-statistic | 0.697 | 0.648 | 0.711 | 0.785 | |||||
| AIC global fit | 566.4 | 575.3 | 543.4 | 524.0 | |||||
NR, not reached.
In 96 patients, additional laboratory data were available, including baseline β2 microglobulin (β2M) and CRP levels. In univariate analysis, factors associated with inferior OS and PFS included age ≥60 years, ECOG performance status >2, multiple extranodal sites, B symptoms, hemoglobin <12 g/dL, elevated β2M, and elevated CRP (Table 4). In multivariate analysis, only 4 factors retained an independent prognostic value for PFS: age ≥60 years, ECOG performance status >2, elevated β2M, and elevated CRP. Combining these 4 covariates, we developed a novel prognostic score (AITL score), which stratified patients into low- (17%), intermediate- (23%), or high-risk (60%) groups. Patients with low-, intermediate-, and high-risk AITL scores had 5-year PFS estimates of 41%, 37%, and 13%, respectively (P = .003) and 5-year OS estimates of 63%, 54%, and 21%, respectively (P = .0003). In comparison with the IPI, PIT, and PIAI, the AITL score demonstrated the greatest discriminant power with a lower AIC (524.0) and higher Harrell C-statistic (0.785) than the other prognostic indices (Table 3).
Univariate and multivariate analysis for PFS
| . | Univariate analysis . | Multivariate analysis . | ||
|---|---|---|---|---|
| P . | HR (95% CI) . | P . | HR (95% CI) . | |
| Age ≥60 y | .002 | 1.33 (1.1-1.6) | .003 | 2.98 (1.7-6.8) |
| Stage III-IV | .069 | 1.68 (0.88-3.2) | — | — |
| Extranodal sites ≥2 | .003 | 1.73 (1.2-2.6) | .082 | 3.2 (1.7-5.1) |
| ECOG >2 | .0003 | 1.9 (1.4-2.7) | .001 | 4.3 (2.1-6.8) |
| Bone marrow involvement | .223 | 1.3 (0.8-1.9) | — | — |
| B symptoms | .017 | 1.5 (1.0-2.1) | .092 | 2.31 (1.8-3.5) |
| LDH > ULN | .005 | 1.62 (1.1-2.2) | .071 | 1.73 (1.4-3.1) |
| Hemoglobin <12 g/dL | .018 | 1.48 (1-2) | .123 | 0.75 (0.2-2.4) |
| Platelets <150 000/mm3 | .438 | 1.1 (0.8-1.6) | — | — |
| Monocytes <800/mm3 | .033 | 1.5 (2.6) | .082 | 1.31 (0.9-3.3) |
| ANC >6500/mm3 | .173 | 1.26 (0.9-1.7) | — | — |
| β2M > ULN | .003 | 2.9 (1.4-5.8) | .002 | 3.21 (2.2-6.5) |
| CRP > ULN | .004 | 2.9 (1.4-6.1) | .003 | 1.9 (1.2-4.6) |
| . | Univariate analysis . | Multivariate analysis . | ||
|---|---|---|---|---|
| P . | HR (95% CI) . | P . | HR (95% CI) . | |
| Age ≥60 y | .002 | 1.33 (1.1-1.6) | .003 | 2.98 (1.7-6.8) |
| Stage III-IV | .069 | 1.68 (0.88-3.2) | — | — |
| Extranodal sites ≥2 | .003 | 1.73 (1.2-2.6) | .082 | 3.2 (1.7-5.1) |
| ECOG >2 | .0003 | 1.9 (1.4-2.7) | .001 | 4.3 (2.1-6.8) |
| Bone marrow involvement | .223 | 1.3 (0.8-1.9) | — | — |
| B symptoms | .017 | 1.5 (1.0-2.1) | .092 | 2.31 (1.8-3.5) |
| LDH > ULN | .005 | 1.62 (1.1-2.2) | .071 | 1.73 (1.4-3.1) |
| Hemoglobin <12 g/dL | .018 | 1.48 (1-2) | .123 | 0.75 (0.2-2.4) |
| Platelets <150 000/mm3 | .438 | 1.1 (0.8-1.6) | — | — |
| Monocytes <800/mm3 | .033 | 1.5 (2.6) | .082 | 1.31 (0.9-3.3) |
| ANC >6500/mm3 | .173 | 1.26 (0.9-1.7) | — | — |
| β2M > ULN | .003 | 2.9 (1.4-5.8) | .002 | 3.21 (2.2-6.5) |
| CRP > ULN | .004 | 2.9 (1.4-6.1) | .003 | 1.9 (1.2-4.6) |
Discussion
To our knowledge, this study represents the largest prospective international cohort of patients with AITL reported to date, allowing for an assessment of real-world treatment approaches, outcomes, and prognostic factors of patients treated in the contemporary era. Constituting 18% of patients in the TCP database, AITL represents the second most common subtype of PTCL globally, with a lower incidence in South America as previously published.26 Consistent with prior reports, AITL was more frequently diagnosed in older adults (median age, 64 years) and typically presented with advanced-stage disease, B symptoms, elevated LDH, and high-risk disease as defined by multiple prognostic indices, including the IPI, PIT, and PIAI.1-4
Most patients were treated with anthracycline-based regimens such as CHOP, and only a small proportion also received etoposide (16%), which may in part reflect the older age of our cohort (63% of patients ≥60 years old). There was no significant difference in outcomes with or without etoposide, although statistical power is limited due to the relatively small number of patients. An even smaller proportion of patients underwent consolidative ASCT in CR1 (13%). This may also reflect the older age of our cohort as well as geographic variations in practice patterns. Comparing outcomes between patients ≤65 years old who underwent ASCT in CR1 with those who did not suggested that ASCT in CR1 was associated with superior outcomes with favorable 5-year OS and PFS estimates of 89% and 79%, respectively. However, the intrinsic selection bias and lack of a randomized comparison are important limitations, particularly given the higher incidence of bulky disease, elevated LDH, and anemia in the nontransplanted group. Notably, the benefit of ASCT in CR1 observed in this cohort is consistent with prior studies, including a prospective study from the United States COMPLETE registry,27 a large population-based cohort from the Swedish Lymphoma Registry,28 and a recent systematic review and meta-analysis of 16 retrospective studies.29 Cumulatively, these data suggest that consolidative ASCT should be considered in CR1 for transplant-eligible patients with AITL.
Our study validated the prognostic value of the IPI, PIT, and PIAI in a large prospective AITL cohort and in a limited data set of 96 patients enabled identification of novel prognostic factors and a new prognostic score (AITL score). We identified β2M and CRP as independent prognostic factors associated with PFS, consistent with a prior retrospective study.30 The AITL score combining 4 covariates (age, performance status, β2M, and CRP) stratified patients into low-, intermediate-, and high-risk groups and demonstrated greater discriminant power than the IPI, PIT, and PIAI. Of note, patients with a high-risk AITL score had particularly dismal outcomes, with 5-year PFS of 13% compared with 24% to 27% for patients with a high-risk IPI, PIT, or PIAI. These findings require validation in a prospective cohort of homogeneously treated patients. We also identified POD24 as a powerful prognostic factor, consistent with a recent retrospective study in PTCL.31
Overall, treatment of AITL with standard chemotherapy regimens in the contemporary era was associated with disappointing outcomes with 5-year OS and PFS estimates of 44% and 32%, respectively. While these outcomes are marginally better than those reported in a large population-based study from the Swedish Lymphoma Registry (5-year OS and PFS estimates of 32% and 20%, respectively), the differences may in part reflect the older median age of 70, differences in patient selection (academic medical centers vs a broad population-based cohort), and the requirement of available biopsy material for review.28 We did not observe any difference in outcomes between patients treated in 2006-2010 (prior to the FDA approval of romidepsin for relapsed disease) compared with 2011-2018 (an era reflecting increasing use of novel agents).
Recently, several trials have attempted to improve upon standard CHOP-based therapy by using alternative chemotherapy backbones or incorporating novel agents such as brentuximab vedotin (BV) or romidepsin into frontline therapy. A randomized phase 2 trial in the United Kingdom compared CHOP with a non–anthracycline-based regimen (gemcitabine, cisplatin, and methylprednisolone) to mitigate multidrug resistance efflux pumps but was closed early for lack of efficacy.32 More recently, the international, randomized phase 3 ECHELON-2 trial demonstrated superior outcomes in patients with CD30+ PTCL (defined as ≥10% CD30 expression) receiving BV-CHP vs CHOP chemotherapy.33 However, only 12% of patients on the ECHELON-2 trial had AITL, and the benefit of BV-CHP in CD30+ AITL remains unclear (HR for PFS, 1.40; 95% CI, 0.64-3.07; HR for OS, 0.87; 95% CI, 0.29-2.58).33
Improvements in our understanding of AITL biology over the past decade, including the identification of recurrent somatic mutations in RHOA, TET2, DNMT3A, and IDH2, have led to novel therapeutic strategies such as epigenetic modifying therapies.34-37 Recent studies suggest that AITL and other TFH PTCLs may have higher response rates to histone deacetylase (HDAC) inhibitors, such as romidepsin and belinostat, compared with non-TFH PTCLs, which may reflect the higher frequency of mutations in TET2 and DNMT3A, which perturb epigenetic regulation.38,39 Azacitidine, a hypomethylating agent, has also demonstrated high response rates in AITL as a single agent and in combination with romidepsin, further supporting the role of epigenetic dysregulation in AITL.40,41 Despite encouraging results from a phase 1b/2 study combining romidepsin with CHOP as frontline therapy for PTCL, the randomized phase 3 Ro-CHOP (romidepsin-CHOP) trial failed to demonstrate a PFS benefit in the romidepsin + CHOP arm compared with CHOP alone.42,43
In summary, we demonstrate in this international prospective study that outcomes remain suboptimal for patients with AITL treated in the contemporary era, with particularly poor outcomes for high-risk patients and those experiencing POD24. Elevated β2M and CRP at initial diagnosis had an independent prognostic impact associated with inferior PFS. In transplant-eligible patients, superior outcomes were observed among patients consolidated with ASCT in CR1. These findings are hypothesis generating and lay the framework for future studies. Optimal treatment of AITL remains an unmet need. Novel therapeutic approaches and better understanding of disease biology are required to improve outcomes.
Requests for original data should be sent to the corresponding author (mcivallero@unimo.it).
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
There is a Blood Commentary on this article in this issue.
Acknowledgments
This work was funded by the Fondazione Cassa di Risparmio di Modena, the Associazione Angela Serra per la Ricerca sul Cancro, the Fondazione Italiana Linfomi, Allos Therapeutics, Spectrum Pharmaceuticals, Associazione Italiana per la Ricerca sul Cancro, National Institutes of Health, National Cancer Institute grant CCSG P30 CA008748 (S.M.H.), and Italian Association for Cancer Research grants 10007 and 20198 (S.P.).
Authorship
Contribution: R.H.A., M.A.S., T.S., and M.F. wrote the manuscript; M.C. and M.M. conducted statistical analyses and made the figures; I.D., J.V., S.A.P., and G.I. reviewed pathology specimens; R.H.A., W.S.K., A.R.S., S.M.H., F.H., M.E.C., I.D., U.V., J.R., S.M., and J.M.V. enrolled study patients; and all authors reviewed and approved the final manuscript.
Conflict-of-interest disclosure: S.M.H. has received research support from ADC Therapeutics, Affimed, Aileron, Celgene,Daiichi Sankyo, Forty Seven, Inc, Kyowa Hakko Kirin, Millennium/Takeda, Seattle Genetics, Trillium Therapeutics, and Verastem/SecuraBio; and has been a consultant for Acrotech Biopharma, ADC Therapeutics, Astex, C4 Therapeutics, Celgene, Janssen, Kura Oncology, Kyowa Hakko Kirin, Myeloid Therapeutics, ONO Pharmaceuticals, Seattle Genetics, SecuraBio, Shoreline Biosciences, Inc, Takeda, Trillium Therapeutics, Tubulis, Verastem, and Vividion Therapeutics. The remaining authors declare no competing financial interests.
Correspondence: Ranjana H. Advani, Stanford Cancer Institute, 875 Blake Wilbur Dr, Stanford, CA 94304; e-mail: radvani@stanford.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal