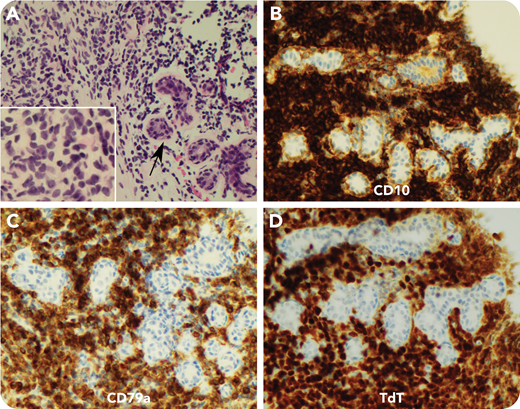
An 18-year-old woman presented with a gradually enlarging 9-cm breast mass that was firm but nontender without overlying skin changes. She was otherwise well without B symptoms or lymphadenopathy. A core biopsy was performed for clinical suspicion of giant fibroadenoma vs phyllodes tumor. Surprisingly, microscopy revealed a multifocal infiltrate of medium-sized apparent lymphoid cells with irregular nuclear contours, dispersed chromatin, and scant cytoplasm (panel A, hematoxylin and eosin stain; arrow, breast duct, with inset highlighting the infiltrating cell morphology; 60× objective/×780 total magnification for inset, 40× objective/×400 total magnification for main panel). Initial staining showed partial CD20 with strong CD10 expression, suspicious for precursor B cells (panel B, CD10 immunohistochemistry; 40× objective/×400 total magnification). This was confirmed by positive staining for CD19, PAX5, CD79a (panel C, CD79a immunohistochemistry; 40× objective/×400 total magnification), and TdT (panel D, TdT immunohistochemistry; 40× objective/×400 total magnification). Staging investigations ruled out blood or bone marrow involvement. The final diagnosis was therefore B-lymphoblastic lymphoma.
Breast masses are common, but they are not often caused by hematologic malignancies. Lymphocytic infiltrates in breast tissue are usually reactive; however, lymphomas including diffuse large B-cell lymphoma, follicular lymphoma, anaplastic large cell lymphoma, and rarely, lymphoblastic lymphoma (LBL) have been reported. As highlighted by this case, the clinical presentation of breast lymphoma can be subtle, and LBL is a critical diagnosis to consider, particularly in younger patients with suspicious morphology.
An 18-year-old woman presented with a gradually enlarging 9-cm breast mass that was firm but nontender without overlying skin changes. She was otherwise well without B symptoms or lymphadenopathy. A core biopsy was performed for clinical suspicion of giant fibroadenoma vs phyllodes tumor. Surprisingly, microscopy revealed a multifocal infiltrate of medium-sized apparent lymphoid cells with irregular nuclear contours, dispersed chromatin, and scant cytoplasm (panel A, hematoxylin and eosin stain; arrow, breast duct, with inset highlighting the infiltrating cell morphology; 60× objective/×780 total magnification for inset, 40× objective/×400 total magnification for main panel). Initial staining showed partial CD20 with strong CD10 expression, suspicious for precursor B cells (panel B, CD10 immunohistochemistry; 40× objective/×400 total magnification). This was confirmed by positive staining for CD19, PAX5, CD79a (panel C, CD79a immunohistochemistry; 40× objective/×400 total magnification), and TdT (panel D, TdT immunohistochemistry; 40× objective/×400 total magnification). Staging investigations ruled out blood or bone marrow involvement. The final diagnosis was therefore B-lymphoblastic lymphoma.
Breast masses are common, but they are not often caused by hematologic malignancies. Lymphocytic infiltrates in breast tissue are usually reactive; however, lymphomas including diffuse large B-cell lymphoma, follicular lymphoma, anaplastic large cell lymphoma, and rarely, lymphoblastic lymphoma (LBL) have been reported. As highlighted by this case, the clinical presentation of breast lymphoma can be subtle, and LBL is a critical diagnosis to consider, particularly in younger patients with suspicious morphology.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal