In this issue of Blood, Khanam et al propose a descriptive integrated genome-wide analysis of the oncogenetic and epigenetic landscape of T-cell lymphoblastic lymphoma (T-LBL) and propose molecular candidates for relapse prediction.1
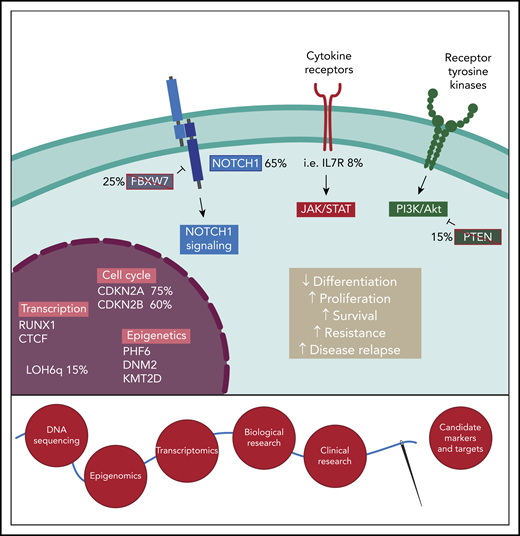
Exploring the oncogenetic landscape of T-LBL to identify candidate markers for disease progression and relapse. Frequent alterations found in T-LBL lead to uncontrolled activation of oncogenetic pathways, including NOTCH1, JAK-STAT, and PI3K/Akt. Additionally, deletion of cell-cycle repressors CDKN2A and CDKN2B or LOH6q elicit cell proliferation and suppress apoptosis. Mutations of transcription factors and epigenetic regulators reshape cell identity and sustain malignant cell expansion and disease progression. Alterations frequencies are indicated for the main events. Integrative approaches combining next-generation DNA sequencing, epigenomics, and transcriptomics have to be engaged. Such investigations are required to determine the oncogenetic drivers of T-LBL and candidate markers of clinical outcomes, notably the treatment response and relapse risk. LOH6q, loss of heterozygosity at chromosome 6q.
Exploring the oncogenetic landscape of T-LBL to identify candidate markers for disease progression and relapse. Frequent alterations found in T-LBL lead to uncontrolled activation of oncogenetic pathways, including NOTCH1, JAK-STAT, and PI3K/Akt. Additionally, deletion of cell-cycle repressors CDKN2A and CDKN2B or LOH6q elicit cell proliferation and suppress apoptosis. Mutations of transcription factors and epigenetic regulators reshape cell identity and sustain malignant cell expansion and disease progression. Alterations frequencies are indicated for the main events. Integrative approaches combining next-generation DNA sequencing, epigenomics, and transcriptomics have to be engaged. Such investigations are required to determine the oncogenetic drivers of T-LBL and candidate markers of clinical outcomes, notably the treatment response and relapse risk. LOH6q, loss of heterozygosity at chromosome 6q.
The World Health Organization classifies T-lymphoblastic leukemia/lymphoma as 2 immature T-cell malignancies sharing many phenotypic and clinical similarities: T-cell acute lymphoblastic leukemia (T-ALL) and T-LBL. Their distinction is essentially based, arbitrarily, on the level of bone marrow infiltration, with T-ALL and T-LBL potentially representing 2 distinct manifestations of a unique T-cell malignancy or arising from a common premalignant progenitor that diverges following acquisition of additional, unique mutations.2
Over the last 2 decades, extensive efforts have led to improved understanding of the biology of T-ALL. Cutting-edge advances in next-generation sequencing notably led to the precise classification of T-ALL into molecular subgroups, identifying driver mutations, and stratifying clinical outcome and relapse risk.3 Similar efforts still need to be engaged for T-LBL.
Khanam et al report for the first time a descriptive genome-wide analysis of 16 T-LBL patients and targeted whole-exon analysis of 76 to 80 genes on an extended cohort (see figure). They report frequent oncogenetic alterations identified in other T-cell malignancies and propose molecular markers of disease relapse. Since T-ALL and T-LBL share common roots, it is not surprising to find that the most frequent oncogenetic events in T-LBL also occur in T-ALL. The most frequent alterations reported result in abnormal activation of the Notch1 pathway, a well-described T-ALL oncogenic pathway.3 Additional T-ALL oncogenic drivers, including the JAK-STAT, phosphatidylinositol 3-kinase (PI3K)/Akt, Ras, and p53 signaling pathways, epigenetic factors, and critical hematopoietic transcription factors are frequently altered in T-LBL, with frequency rates close to those observed in T-ALL.3 Despite this shared oncogenetic landscape, genuine T-LBL–specific drivers have yet to be identified, leaving the distinct phylogeny of T-ALL and T-LBL obscure. This may, of course, be biased by the preferential analysis of T-ALL–associated mutations and hotspots in T-LBL. Nevertheless, this study uses an integrative approach to unravel for the first time the oncogenetic and epigenetic landscape in T-LBL in an extensive cohort of patients.
A major clinical challenge to overcome is the dismal prognosis of relapsed T-ALL/T-LBL cases. As such, the identification of molecular markers predictive of relapse is badly needed. Such a classifier exists for T-ALL, being determined by the mutational status of NOTCH1, FBXW7, RAS, and PTEN.4,5 In T-LBL, a similar classifier, including NOTCH1, FBXW7, RAS, and PTEN and loss of heterozygosity at chromosome 6q, has been evaluated by the authors’ group but considered inferior to one defining high-risk patients on the basis of PTEN mutation and/or LOH6q in NOTCH1 wild-type T-LBL.6 In this issue, Khanam et al propose mutations of KMT2D as an alternative predictor of T-LBL relapse. The authors report that KMT2D mutations combined with PTEN mutations define a group of patients with a high incidence of relapse, although this was restricted to the subgroup of patients without NOTCH1/FBXW7 mutations. Since there was significant overlap between KMT2D and PTEN mutations, it is difficult to determine their respective impact on relapse risk Importantly, KMT2D is not reported to be frequently altered in T-ALL, so it will be important to determine if KMT2D status is associated with an increased risk of relapse, even if rare. Alternatively, KMT2D may represent a T-LBL–specific marker of relapse risk.
This study nicely illustrates the importance of integrative approaches in T-LBL and other T-cell malignancies, benefiting from advances in DNA sequencing and epigenomics. These parameters should also be compared with assessment of minimal disseminated disease, reported to identify poor prognosis patients,7,8 although this is not confirmed on recent therapeutic regimens.9,10 Such studies can unveil the complex oncogenic events driving T-LBL and lead to the identification of potential therapeutic targets and molecular predictors of disease relapse and/or treatment response.
Conflict-of-interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal